Abstract
When incorporating the values of a hemodynamic parameter into the care of patients, the precision of the measurement method should always be considered. A prospective analysis in the previous issue of Critical Care showed that the precision of transpulmonary thermodilution (TPTD) allows for reliable mean values if a standardised procedure is used. The present finding has a physiological basis, as TPTD requires a more prolonged transit time, which in turn reduces the effects that airway pressure and arrhythmia have on venous return-cardiac output steady states. Moreover, this result suggests that the current accepted threshold value of a 15% increase in cardiac output to identify a positive response to a fluid challenge could be reduced in the future. Indeed, this value is mainly related to the precision of the pulmonary artery catheter.
The first principle is that you must not fool yourself - and you are the easiest person to fool.
Richard Feynman (1918 to 1988)
When using a monitoring device for critically ill patients, inadequate precision of the technique can result in serious misinformation. Indeed, the definition of precision is the variability of values due to random errors of measurement. Semantically, it refers to how closely individual measurements agree with each other - that is, the minimum number of measurements necessary to reach a reliable mean value. In this regard, some questions have remained unresolved concerning the measurement of cardiac output (CO) by transpulmonary thermodilution (TPTD) and derived parameters such as global end-diastolic volume (GEDV) and extra-vascular lung water (EVLW). Indeed, TPTD precision has never been prospectively investigated in situations characterized by (1) constant conditions of measurements, (2) the same instrument and operator, and (3) repeated measurements during a short time period.
In the present issue of this journal, Monnet and colleagues [1] illustrated the precision of the TPTD technique and the number of cold boluses needed to achieve an acceptable level of precision when measuring CO, GEDV and EVLW in 91 critically ill patients. In this elegant study, the authors performed a series of five successive thermodilution measurements and then analyzed the precision of each sequence to demonstrate that a precision of less than 10% for CO, GEDV and EVLW could be reached with only three cold bolus injections of 15 ml each [1]. In addition, the least significance change (LSC) associated with three boluses was less than 12% for these three parameters, even if the patients underwent arrhythmia, were spontaneously breathing and/or were having continuous haemodialysis.
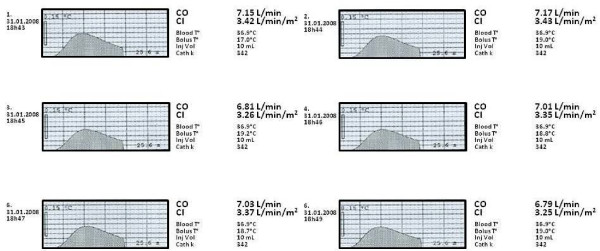
So, what does this mean for clinical practice? Firstly, the present study has finally determined the number of boluses needed to obtain a precise value of CO, GEDV and EVLW by TPTD. Indeed, measuring a change in CO does not necessarily mean that the physiological status of the patient has changed as the error of the measuring technique is directly related to the magnitude of the LSC [2]. This is what is confirmed by the present study by Monnet and colleagues: it takes three boluses to reach a precision below 10% and a LSC of 12% when determining an average value of CO, GEDV and EVLW. Surprisingly, besides the manufacturer's recommendations (Pulsion Medical System™, Munich, Germany), very few studies have focused on this relevant issue [3]. Moreover, the most recent study investigating this question showed conflicting results, with only two boluses needed to determine a reliable average value of cardiac index and GEDV in the stable patients [4]. Secondly, in their study on the precision of the pulmonary artery thermodilution technique, Stetz and colleagues [5] found that three boluses were sufficient to distinguish a real change of 15% in CO compared to the error of reproducibility. In the present study, Monnet and colleagues demonstrate that the TPTD technique allows a precision of less than 10% when measuring CO. The present finding would seem physiologically rational as CO measured using the TPTD curve has a longer circulatory transit time and thus covers more heart beats, which may in turn decrease the influence that arrhythmia and/or changes in pleural pressure has on the measurement (Figure 1). Moreover, the demonstration that the TPTD method is more precise than the classical thermodilution technique [5] could have a huge impact on the definition of a positive response to a fluid challenge since the presently accepted value of a 15% increase in CO is mainly related to the precision of the pulmonary artery catheter [5].
Figure 1.
Example of measurement of cardiac output by transpulmonary thermodilution. Six boluses of 10 ml each (with an average room temperature of 18.62°C) administered at 1 minute intervals reveal an average cardiac output (CO) of 6.99 L/minute; standard deviation = 0.16, precision = 1.90%. BloodT°, temperature of blood; BolusT°, temperature of the cold bolus; Cath k, constant of the PiCCO™ arterial catheter; CI, cardiac index; CO, cardiac output; InjVol, volume of the cold bolus.
One cannot, however, extrapolate these findings to patients with hemodynamic instability and low CO, patho-physiological conditions where the assessment of the precision of a method is unachievable. Moreover, it is essential to acknowledge that the precision of TPTD may be related to the experience of the practitioner and of course may be compromised in extreme situations, such as high volume haemofiltration, therapeutic hypothermia [6], and the presence of an intra-cardiac shunt [7]. Finally, the impact of an increase in cold bolus volume (for example 20 ml) on the precision of the TPTD technique has not yet been determined. Therefore, until further evidence arises, three cold boluses of 15 ml each are mandatory in order to ensure precision of values when measuring CO in the critically ill patient.
Abbreviations
CO: cardiac output; EVLW: extravascular lung water; GEDV: global end-diastolic volume; LSC: least significance change; TPTD: transpulmonary thermodilution.
Competing interests
KB received reimbursements and consultant fees from Edwards LifeSciences. RG and NS have no potential conflicts of interest to declare.
See related research by Monnet et al., http://ccforum.com/content/15/4/R204
Contributor Information
Raphaël Giraud, Email: raphael.giraud@hcuge.ch.
Nils Siegenthaler, Email: nils.siegenthaler@hcuge.ch.
Karim Bendjelid, Email: karim.bendjelid@hcuge.ch.
References
- Monnet X, Persichini R, Ktari M, Jozwiak M, Richard C, Teboul JL. Precision of the transpulmonary thermodilution measurements. Crit Care. 2011;15:R204. doi: 10.1186/cc10421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cecconi M, Rhodes A, Poloniecki J, Della Rocca G, Grounds RM. Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies--with specific reference to the measurement of cardiac output. Crit Care. 2009;13:201. doi: 10.1186/cc7129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendjelid K, Giraud R, Siegenthaler N, Michard F. Validation of a new transpulmonary thermodilution system to assess global end-diastolic volume and extravascular lung water. Crit Care. 2010;14:R209. doi: 10.1186/cc9332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gondos T, Marjanek Z, Kisvarga Z, Halasz G. Precision of transpulmonary thermodilution: how many measurements are necessary? Eur J Anaesthesiol. 2009;26:508–512. doi: 10.1097/EJA.0b013e32832a2d23. [DOI] [PubMed] [Google Scholar]
- Stetz CW, Miller RG, Kelly GE, Raffin TA. Reliability of the thermodilution method in the determination of cardiac output in clinical practice. Am Rev Respir Dis. 1982;126:1001–1004. doi: 10.1164/arrd.1982.126.6.1001. [DOI] [PubMed] [Google Scholar]
- Bendjelid K, Schutz N, Suter PM, Romand JA. Continuous cardiac output monitoring after cardiopulmonary bypass: a comparison with bolus thermodilution measurement. Intensive Care Med. 2006;32:919–922. doi: 10.1007/s00134-006-0161-2. [DOI] [PubMed] [Google Scholar]
- Giraud R, Siegenthaler N, Park C, Beutler S, Bendjelid K. Transpulmonary thermodilution curves for detection of shunt. Intensive Care Med. 2010;36:1083–1086. doi: 10.1007/s00134-010-1876-7. [DOI] [PubMed] [Google Scholar]