Abstract
Objective
The rising health care costs and increasing older adult population in the United States make preventive medicine for this age group especially crucial. Regular physical activity and fruit and vegetable consumption may prevent or delay the onset of many chronic conditions that are common among older adults. The decisional balance sheet is a promotional tool targeting the perceived pros and cons of behavior adoption. The current study tested the efficiency and effectiveness of a single-day decisional balance sheet program, targeting increased physical activity and fruit and vegetable intake among older adults.
Design and Sample
Participating adults (N = 21, age = 72.2) who represented a diverse population in Hawaii (Japanese = 5, Filipino = 4, Caucasian = 4, Native American = 1, Native Hawaiian = 1, Hispanic = 1, and Others = 5) were recruited from housing communities and randomized to a decisional balance sheet program adapted for physical activity or fruit and vegetable consumption.
Measures
Physical activity was assessed using the International Physical Activity Questionnaire (IPAQ) short form, and daily fruit and vegetable intake with the National Health and Nutrition Examination Survey single item instrument. Baseline and follow-up data were collected.
Results
Both programs were implemented efficiently, and participants in both groups improved their daily physical activity. The decisional balance sheet for fruit and vegetable consumption appeared less effective.
Conclusions
Specific suggestions for similar programs are reported.
Keywords: community living, geriatric nursing, nutrition, physical activity
By the year 2030, one of five Americans will be at least 65 years old (Balfour et al., 2009). Reports indicate that approximately 78% of U.S. health care dollars are spent on chronic disease, and these expenses rise dramatically as people develop multiple conditions (Anderson & Horvath, 2004). Given that 85% of older adults have at least one chronic condition and 62% have multiple chronic conditions (Anderson & Horvath, 2004), the increasing older adult population could add considerable strain to the U.S. health care system. To avert these future costs, it will be critical for all health stakeholders to engage in proactive approaches to prevent these conditions.
Two behaviors associated with the decreased risk of chronic disease are regular physical activity and daily fruit and vegetable consumption. Regular physical activity among older adults is associated with reduced risk of cardiovascular disease, thromboembolic stroke, hypertension, type 2 diabetes mellitus, osteoporosis, obesity, colon cancer, breast cancer, anxiety, and depression (Haskell et al., 2007). Furthermore, an epidemiological review reported fruit and vegetable consumption protective against numerous cancers, coronary heart disease, stroke, and cataract formation (Van Duyn & Pivonka, 2000). Although older adults commonly suffer from hypertension, heart disease, arthritis, eye disorders, and diabetes (Anderson & Horvath, 2004), they are the least physically active of all age groups (CDC, 2003) and many believe there is no point in improving their diet (Resnick & Daly, 1998).
From the years 2000 to 2030, the demand for older adult living communities is projected to double (Bernstein & Edwards, 2008). Despite the convenience of these localized settings, previous promotional efforts report difficulty in motivating older adults (Mihalko & Wickley, 2003). Less success among older adults may result from their passive approach to health care (Bastiaens, Van Royen, Pavlic, Raposo, & Baker, 2007), their multiple medical needs (Haber, 1994), and/or limited physician time devoted to preventive health (Fried & Guralnik, 1997; Langford, 2004; Thorpe & Howard, 2006). Previous reports suggest simple and minimally intense health promotion programs that aim to inform and empower older adult participants, rather than overwhelm them (Fox, Breuer, & Wright, 1997; Hochhalter, Song, Rush, Sklar, & Stevens, 2010; Tennstedt, 2000). One theory-based health promotional tool fitting this description is the decisional balance sheet.
Decisional balance is a measure of attitude that captures how individuals weigh the consequences of a specific behavior in terms of pros and cons (Prochaska, Redding, & Evers, 1996). The decisional balance sheet program provides basic health knowledge and empowers individuals to take personal control over their own health (Janis & Mann, 1977). Specifically, participants discuss and record their perceived gains and losses associated with behavior adoption. This approach has been successful in the promotion of cancer screening among Chinese women (≥50 years) (Strong & Liang, 2009) and diabetes screening among middle-aged adults (40–69 years) (Kellar et al., 2008); however, there is minimal to no report on programs designed to promote older adults’ physical activity and/or fruit and vegetable consumption. The current study tested the implementation of a decisional balance sheet physical activity program and fruit and vegetable program; specifically describing the efficiency and effectiveness of programs adapted for older adults residing in community living homes.
Methods
Design and sample
Older adults were recruited from two community housing sites in Hawaii. Following informed consent, participants completed a 10-min health behavior survey and were randomly assigned to either the physical activity program or the fruit and vegetable program. Approximately 2 weeks later, participants completed a follow-up health behavior survey, and received a $10 grocery store gift card for their participation. All procedures were approved by the University Institutional Review Board.
Intervention
Decisional balance sheet program
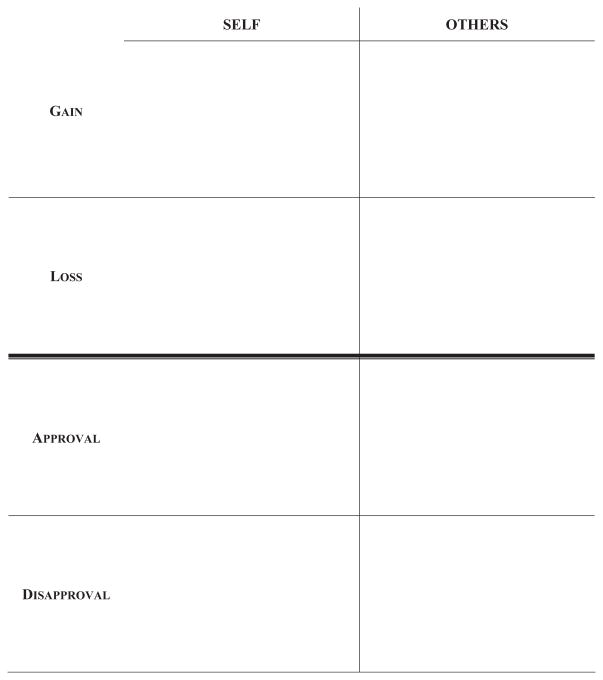
Apart from targeting different health behaviors, the physical activity and fruit and vegetable decisional balance programs were identical. The single-day program began with introductions, which was followed by a group discussion on the gains and losses associated with behavior adoption; participants were encouraged to share personal expectations throughout. Participants were then guided through completion of their own decisional balance sheet (see Fig. 1), recording the consequences of adopting the targeted behavior in terms of gains, losses, approvals, and disapprovals. As observed, the sheet includes a column labeled self and others; thus, participants were asked to consider both the personal and social consequences of increasing their physical activity or fruit and vegetable intake.
Figure 1.
Decisional Balance Sheet (Adapted from Janis & Mann, 1977)
Measures
Participants self-reported their gender, age, race/ethnicity, marital status, and height/weight. Physical activity was assessed using the International Physical Activity Questionnaire (IPAQ) short form, which has been validated across diverse populations and settings (Craig et al., 2003). Daily fruit and vegetable intake was assessed with the National Health and Nutrition Examination Survey single item instrument (NCHS, 2007), which has been validated extensively (Prochaska & Sallis, 2004; Resnicow et al., 2000).
Analytic strategy
Due to the small sample size and preliminary nature of this program evaluation, results are presented descriptively. The within and between group pre- to postintervention, change in average daily physical activity minutes, and fruit and vegetable servings are presented by intervention group.
Results
Participant demographics
Participants with complete assessment data at pre-and postintervention (N = 21) had a mean age of 72.24 years (standard deviation [SD] = 11.84) and a mean body mass index (BMI; weight/height2 × 703) of 26.14 (SD = 6.57). Seventy-six percent of participants were women, 80% were high school graduates, 95% were either single or widowed, and 71% self-reported their health as good to excellent. Participants represented an ethnically diverse population in Hawaii (Japanese = 5, Filipino = 4, Caucasian = 4, Native American = 1, Native Hawaiian = 1, Hispanic = 1, and Others = 5).
Program efficiency
The brief decisional balance sheet program demonstrated high feasibility and efficiency. The localized population and organized structure of the environment provided easy implementation of the single-day program. Although there was some dropout, 71% of physical activity group participants, and 53% of fruit and vegetable participants attended both the baseline and follow-up meetings. The program required minimal staff involvement (≈30–40 min) and included minimal paper costs ($0.05 [one decisional balance sheet] × 21 participants = $1.05).
Program effectiveness
The average daily physical activity and fruit and vegetable servings at pre- and postintervention and mean change (i.e., postintervention-baseline) are presented in Table 1 by the decisional balance sheet program received. Both groups improved their moderate physical activity minutes, with the fruit and vegetable program participants demonstrating a greater mean increase (15.19 more minutes). Alternatively, compared with their counterparts, physical activity program participants reported a greater increase in their daily fruit and vegetable intake (1.01 more servings). However, the higher servings consumed by fruit and vegetable participants relative to physical activity participants at both assessment points is noteworthy.
TABLE 1.
Daily Moderate Physical Activity and Fruit and Vegetable Consumption
| Program | N | Behavior | Baseline mean (SD) | Follow-up mean (SD) | Mean changea |
|---|---|---|---|---|---|
| Physical activity | 12 | PA minutes | 18.76 (22.62) | 50.95 (54.51) | +32.19 |
| FV servings | 3.52 (3.42) | 3.79 (1.93) | +0.27 | ||
| Fruit and vegetable | 9 | PA minutes | 3.33 (10.00) | 50.38 (84.30) | +47.38 |
| FV servings | 5.63 (3.25) | 4.89 (1.83) | 30.74 |
PA = physical activity; FV = fruit and vegetable; SD = standard deviation.
Mean change = (follow-up mean – baseline mean).
Discussion
Within the next 20 years, the U.S. population will become much older, and projections estimate a dramatic rise in chronic conditions. Although aging is inevitable, the onset of chronic disease among older adults can be prevented. The current study evaluated two decisional balance sheet programs that targeted the health behavior of older adults residing in a community housing environment. Implementation procedures and results indicated that the brief program is an efficient and effective tool for promoting healthy behavior among older adults. Study outcomes are discussed below with suggestions for future application.
Relative to efficiency, the single-day decisional balance sheet program to promote physical activity and fruit and vegetable intake was implemented successfully. Being inclusive to older adults, the community-living setting proved highly functional for program implementation. The decisional balance sheet program was characteristically ideal, providing individually tailored motivation with minimal staff training and low participant demand. Housing communities for older adults are under increasing demand, generating increased opportunities for health promotion programs with excellent reach and simplified dissemination. Similar health promotion programs and evaluations within these type of settings are encouraged.
The decisional balance sheet program appeared effective for physical activity promotion, but potentially less applicable for increasing older adults’ fruit and vegetable intake. It may be that the perceived benefits of fruit and vegetables are not substantial enough to motivate increased intake among older adults, which would parallel previous evidence (Resnick & Daly, 1998). It is also important to recognize the high fruit and vegetable consumption at baseline, which left little room for improvement among fruit and vegetable participants. Finally, certain environmental factors are likely to impact program effectiveness (e.g., accessibility to physical activity/nutrition opportunities). Research identifying the specific characteristics of adult housing communities that are most salient to program success is warranted.
Noteworthy is the untargeted increase in physical activity among fruit and vegetable participants, which is a phenomenon that has been well documented in previous intervention research (Berrigan, Dodd, Troiano, Krebs-Smith, & Barbash, 2003; Fine, Philogene, Grambling, Coups, & Sinha, 2004; Johnson et al., 2008). For example, a recent randomized controlled trial found that individuals who adopted one healthy behavior were up to five-times more likely to adopt an additional healthy behavior (Johnson et al., 2008). Prospective studies report considerable benefits of multiple health behavior adoption, estimating an approximate 70% reduction in chronic disease (Ford et al., 2009) and significantly improved quality of life (Harrington et al., 2010). Given such potential and older adults’ exaggerated concern for their personal health (Cox, Miller, & Mull, 1987; Fox et al., 1997), the success of multiple health behavior promotion among older adult populations is a valuable avenue for future research.
The prevalence of older adult housing communities is expected to rise dramatically over the next 20 years, generating excellent reach to the older adult population. Given this rising opportunity, evidence to inform efficient and effective promotional strategies that tailor to these contexts is warranted. The current decisional balance sheet program successfully promoted physical activity at low cost and with minimal staff involvement; hence, current practitioners are encouraged to implement the decisional balance sheet in similar settings. The current small and highly diverse sample did not allow examination of potential factors moderating the impact of the intervention (e.g., ethnicity, age); however, the large ethnic representation provides groundwork for future studies to build on, as well as practical information for nurse practitioners working among similar populations.
Acknowledgments
The authors disclosed receipt of the following financial support for the research and/or authorship of this article. Funded by the National Cancer R25 CA90956 and CURE supplement P30 CA071789.
References
- Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Reports. 2004;119(3):263–270. doi: 10.1016/j.phr.2004.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balfour DC, Evans S, Januska J, Lee HY, Lewis SJ, Nolan SR, et al. The future of Medicare Part D drug plans–results from a roundtable discussion. Journal of Managed Care Pharmacy. 2009;15(1 Suppl A):18–21. doi: 10.18553/jmcp.2009.15.s1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastiaens H, Van Royen P, Pavlic DR, Raposo V, Baker R. Older people’s preferences for involvement in their own care: A qualitative study in primary health care in 11 European countries. Patient Education and Counseling. 2007;68(1):33–42. doi: 10.1016/j.pec.2007.03.025. [DOI] [PubMed] [Google Scholar]
- Bernstein R, Edwards T. An older and more diverse nation by mid-century. U.S. Census Bureau News; 2008. Retrieved from http://www.census.gov/newsroom/releases/archives/population/cb08-123.html. [Google Scholar]
- Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behavior in U.S. adults. Preventive Medicine. 2003;36(5):615–623. doi: 10.1016/s0091-7435(02)00067-1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Prevalence of physical activity, including lifestyle activities among adults–United States, 2000–2001. Morbidity and Mortality Weekly Report. 2003;52(32):764–769. [PubMed] [Google Scholar]
- Cox CL, Miller EH, Mull CS. Motivation in health behavior: Measurement, antecedents, and correlates. Advances in Nursing Science. 1987;9(4):1–15. doi: 10.1097/00012272-198707000-00004. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Fine LJ, Philogene GS, Grambling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors. 2001 National Health Interview Survey. American Journal of Preventive Medicine. 2004;27(2 Suppl):18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Ford ES, Bergmann MM, Kroger J, Schien-kiewitz A, Weikert C, Boeing H. Healthy living is the best revenge. Archives of Internal Medicine. 2009;24:1355–1362. doi: 10.1001/archinternmed.2009.237. [DOI] [PubMed] [Google Scholar]
- Fox PJ, Breuer W, Wright JA. Effects of a health promotion program on sustaining health behaviors in older adults. American Journal of Preventive Medicine. 1997;13(4):257–264. [PubMed] [Google Scholar]
- Fried LP, Guralnik JM. Disability in older adults: Evidence regarding significance, etiology, and risk. Journal of American Geriatrics Society. 1997;45(1):92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- Haber D. Health promotion and aging. New York, NY, U.S: Springer Publishing Co, Inc; 1994. [Google Scholar]
- Harrington J, Perry IJ, Lutomski J, Fitzgerald AP, McGee H, Barry MM, et al. Living longer and feeling better: Healthy lifestyle, self-rated health, obesity and depression in Ireland. European Journal of Public Health. 2010;20(1):91–95. doi: 10.1093/eurpub/ckp102. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Lee I, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Medicine and Science in Sports and Exercise. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- Hochhalter AK, Song J, Rush J, Sklar L, Stevens A. Making the most of your healthcare intervention for older adults with multiple chronic illness. Patient Education and Counseling. 2010;81(2):207–213. doi: 10.1016/j.pec.2010.01.018.. [DOI] [PubMed] [Google Scholar]
- Janis IL, Mann L. Decision making: A psychological analysis of conflict, choice, and commitment. New York: Free Press; 1977. [Google Scholar]
- Johnson SS, Paiva AL, Cummins CO, Johnson JL, Dyment SJ, Wright JA, et al. Transtheoretical model-based multiple behavior intervention for weight management: Effectiveness on a population basis. Preventive Medicine. 2008;46(3):238–246. doi: 10.1016/j.ypmed.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellar I, Sutton S, Griffin S, Prevost AT, Kin-month AL, Marteau TM. Evaluation of an informed choice invitation for type 2 diabetes screening. Patient Education and Counseling. 2008;72(2):232–238. doi: 10.1016/j.pec.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Langford MC. Type 2 diabetes and chronic systolic heart failure: Clinical implications. Journal of Cardiovascular Nursing. 2004;19(6 Suppl):S35–S44. doi: 10.1097/00005082-200411001-00005. [DOI] [PubMed] [Google Scholar]
- Mihalko SL, Wickley KL. Active living for assisted living: Promoting partnerships within a systems framework. American Journal of Preventive Medicine. 2003;25(3 Suppl 2):193–203. doi: 10.1016/s0749-3797(03)00184-3. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey Questionnaire. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. Retrieved from http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/nhanes07_08.htm. [Google Scholar]
- Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz F, Lewis MF, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA: Mossy-Bass; 1996. pp. 60–84. [Google Scholar]
- Prochaska JJ, Sallis JF. Reliability and validity of a fruit and vegetable screening measure for adolescents. Journal of Adolescent Health. 2004;34(3):163–165. doi: 10.1016/j.jadohealth.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Resnick B, Daly MP. Predictors of functional ability in geriatric rehabilitation patients. Rehabilitation Nursing. 1998;23(1):21–29. doi: 10.1002/j.2048-7940.1998.tb01752.x. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Odom E, Wang T, Dudley WN, Mitchell D, Vaughan R, et al. Validation of three food frequency questionnaires and 24-hour recalls with serum carotenoid levels in a sample of African-American adults. American Journal of Epidemiology. 2000;152(11):1072–1080. doi: 10.1093/aje/152.11.1072. [DOI] [PubMed] [Google Scholar]
- Strong C, Liang W. Relationships between decisional balance and stage of adopting mammography and Pap testing among Chinese American women. Cancer Epidemiology. 2009;33(5):374–380. doi: 10.1016/j.canep.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennstedt SL. Empowering older patients to communicate more effectively in the medical encounter. Clinics in Geriatric Medicine. 2000;16(1):61–70. doi: 10.1016/s0749-0690(05)70008-2. [DOI] [PubMed] [Google Scholar]
- Thorpe KE, Howard DH. The rise in spending among Medicare beneficiaries: The role of chronic disease prevalence and changes in treatment intensity. Health Affairs (Millwood) 2006;25(5):w378–w388. doi: 10.1377/hlthaff.25.w378.. [DOI] [PubMed] [Google Scholar]
- Van Duyn MA, Pivonka E. Overview of the health benefits of fruit and vegetable consumption for the dietetics professional: Selected literature. Journal of American Dietetic Association. 2000;100(12):1511–1521. doi: 10.1016/S0002-8223(00)00420-X. [DOI] [PubMed] [Google Scholar]