Abstract
Using data from the 2004 wave of the National Long-Term Care Survey, we examined how negative and positive caregiving experiences differ by caregivers’ gender and relationship to care recipients. We further considered how their caregiving experiences are affected by caregivers’ demographic characteristics, care recipients’ problem behavior and dependency, caregivers’ involvement, reciprocal help from care recipients, and social support available for caregivers. We found that female and adult-child caregivers, in general, reported having had more negative experiences than male and spouse caregivers, respectively. Wife caregivers were least likely to report positive experiences. We also found different risk factors for negative and positive caregiving experiences, and these factors varied depending on caregivers’ gender and relationship to the care recipient. The findings underscore the heterogeneity of caregiving experiences. To sustain informal care, state and local agencies need to tailor services to wife, husband, daughter, and son caregivers’ unique needs.
Keywords: Family caregivers, Interference, Strain, Burnout, Personal gratification
Family caregivers play a central role in caring for frail older adults. It is estimated that 36 million adults provide unpaid care to a family member who is age 65 or older (National Alliance for Caregiving, 2009). Nearly 80% of these family caregivers are spouses or adult children (Wolff & Kasper, 2006). Family caregivers, on average, provide more than 20 hours of care per week to older adults with limitations in daily activities (Johnson & Wiener, 2006). The estimated economic value of the care provided by family caregivers is approximately $450 billion a year, which exceeds total Medicaid spending and approaches 90% of the entire expenditure on Medicare (Feinberg, Reinhard, Houser, & Choula, 2011). As 76 million baby boomers gradually enter late life, most will eventually develop some form of functional limitations and rely on their spouses or adult children for care (Manton, Gu, & Lamb, 2006). Sustaining family caregivers’ capacity to help maintain older adults’ daily functioning, therefore, becomes an important policy issue.
Researchers have extensively examined risk factors associated with caregiving and have suggested ways to enhance caregivers’ well-being (Pinquart & Sörensen, 2003). Two issues, however, have not yet been adequately addressed. First, most prior studies have focused on caregivers’ negative experiences and overlooked the positive experiences associated with caregiving (Walker, Pratt, & Eddy, 1995), probably based on the assumption that by reducing negative experiences, caregivers can continue providing care. This line of thought ignores the fact that caregiving also brings about positive experiences, which may propel caregivers to continue their support. Caregivers may receive personal gratification when they feel useful by caring for frail older adults (Raschick & Ingersoll-Dayton, 2004), or they may view caregiving as a way to pay back for the help they received from the care recipients in the past (Henretta, Hill, Li, Soldo, & Wolf, 1997). Moreover, family members are expected to take care of each other. Providing care to family members confirms social norms and generates social approval (Lee, Netzer, & Coward, 1994). Because the decision to stay in the caregiver role is likely to be affected by negative as well as positive caregiving experiences, it is imperative to examine risk factors related to both types of experiences simultaneously.
The second issue is that previous research has not yet carefully examined whether risk factors associated with caregiving experiences vary by caregivers’ gender and their relationship to care recipients. When older adults need help, their spouses usually are the first to provide care. Adult children generally step in when spouses are not available. In either type of relationship, women are more likely than men to be caregivers. Past studies have examined whether risk factors related to caregiving experiences differ either by gender (Pinquart & Sörensen, 2006; Yee & Schulz, 2000) or by relationship (Lawton, Moss, Kleban, Glicksman, & Rovine, 1991; Li, Seltzer, & Greenberg, 1997). Few have fully explored the difference by gender as well as by relationship.
This study used the 2004 wave of the National Long-Term Care Survey to examine both negative and positive caregiving experiences. In particular, we examined how negative and positive caregiving experiences differ by four groups of caregivers: wives, husbands, daughters, and sons. We further considered how their caregiving experiences are affected by caregivers’ demographic characteristics, care recipients’ problem behavior and dependency, caregivers’ involvement, reciprocal help from care recipients, and social support available for caregivers of different genders and in different relationships.
Negative versus positive caregiving experiences
Caregivers typically experience both negative and positive feelings simultaneously (Kramer, 1997; Walker et al., 1995). On the one hand, caregiving activities may interfere with caregivers’ daily routines; cause physical, emotional, and financial strain; and eventually exhaust their energy (Pinquart & Sörensen, 2003). On the other hand, caregivers can acquire satisfaction from helping their family members (Marks, Lambert, & Choi, 2002). Thus, to sustain family caregiving, policy makers need to know not only how to decrease caregivers’ negative experiences, but also how to increase their positive experiences.
Risk factors associated with caregiving experiences
Negative caregiving experience is likely to be affected by caregivers’ characteristics. Caregivers who are White (Pinquart & Sörensen, 2005), who complete fewer years of schooling, who are working (Li et al., 1997), and who have poor health (Miller et al., 2001) tend to report more distress than do their respective counterparts. Negative caregiving experiences may also be influenced by the interaction between caregivers and care recipients. Caregivers are likely to experience a higher level of distress when care recipients exhibit more problem behaviors or show greater dependency (Ingersoll-Dayton & Raschick, 2004; Schulz, O’Brien, Bookwala, & Fleissner, 1995), when caregivers spend long hours helping with activities of daily living (ADL) or instrumental activities of daily living (IADL) (Ingersoll-Dayton & Raschick, 2004; Kang, 2006; Neal, Ingersoll-Dayton, & Starrels, 1997), or when they do not receive reciprocal help or positive feedback from care recipients (Dwyer, Lee, & Jankowski, 1994; Raschick & Ingersoll-Dayton, 2004). In addition, caregivers’ social connections may have an impact on their negative caregiving experiences. Past studies have shown that lack of someone to take over caregiving tasks (Mui, 1995), lack of support from friends or relatives (Li et al., 1997; Miller et al., 2001), or family conflict (Kang, 2006; Strawbridge & Wallhagen, 1991) are positively related to caregivers’ depression. Fewer studies have examined factors that may contribute to positive caregiving experience. Among those that do, care recipients’ problem behavior has been found to be negatively but caregiver’s involvement and social support have been found to be positively associated with positive feelings (Lawton et al., 1991; Raschick & Ingersoll-Dayton, 2004).
Caregivers’ gender and relationship to care recipients
Caregiving experience is likely to vary by caregivers’ gender and relationship to care recipients because men and women are socialized differently and the roles of spouse and adult-child delineate different kinship obligations. Because women are socialized to nurture, they provide more help with hands-on tasks and longer hours of care than men (Neal et al., 1997; Pinquart & Sörensen, 2006). Men are also likely to use different strategies than women when dealing with problems that arise during caregiving, for example, by focusing on tasks and blocking emotions (Calasanti & King, 2007). Therefore, we anticipate that female caregivers report more negative experiences than male caregivers do. Moreover, many adult children, particularly daughters, are working or have their own families to take care of while providing help to their frail parents (Brody, 2004; Stephens, Townsend, Martire, & Druley, 2001). Because of competing commitments, we expect that adult-child caregivers report more negative experiences than spouse caregivers do.
With regard to positive caregiving experiences, we conjecture that male and adult-child caregivers are more likely than female and spouse caregivers, respectively, to acquire positive meaning from caregiving. This occurs because men are less expected to engage in the caregiver role than women. When men carry out caregiving tasks, they are more likely than women to be praised for their care provision (Harris, 2002). Unlike spouses, adult children are at a distinctly different life stage than their care recipients. The opportunity to care for their parents may increase appreciation of life for adult children more than spouses caring for their partner, as the latter is a normative expectation (Raschick & Ingersoll-Dayton, 2004).
Risk factors related to caregiving experiences are likely to differ depending on caregivers’ gender. Because women internalize and identify with their caregiver role and have more experiences of caring for others than men (Walker et al., 1995), we hypothesize that care recipients’ problem behaviors and dependency and long hours of care provision are more stressful for male caregivers than for female caregivers. Furthermore, women are socialized to be relationship-oriented whereas men are task-oriented (Lutzky & Knight, 1994). Thus, we anticipate that reciprocal help from care recipients and social support have a stronger effect on alleviating women’s caregiving burden and increasing their positive feelings than men’s. Because individuals with more years of schooling are less likely to hold traditional gender roles than individuals with fewer years of schooling (Brewster & Padavic, 2000), we suspect that more educated women experience more caregiving stress than less educated women.
Risk factors associated with caregiving experiences also tend to vary by caregivers’ relationship to care recipients. Many spouses view care provision as a normative expectation of marriage and are more committed than adult-child caregivers (Harris, 2002; Lawton et al., 1991). As a result, we expect that care recipients’ problem behaviors and dependency and long hours of care provision are associated with greater strain for adult-child caregivers than for spouse caregivers. In addition, adult children often face competing demands of being a caregiver, a spouse, a parent, and an employee at the same time. Therefore, we conjecture that help from care recipients and other family members lessens adult-child caregivers’ stress and increases their positive feeling more than it does for spouse caregivers.
Present study
Caring for frail older adults is often a long-term commitment. In order to sustain informal care, policy makers need to not only reduce caregivers’ negative experiences, but also enhance their positive ones. Prior studies have extensively examined risk factors associated with negative caregiving experiences, but little is known about factors related to positive experiences. This study advances prior research by examining negative and positive caregiving experiences and taking into account the intersection of caregivers’ gender and relationship to care recipients. In particular, the study addresses three aims. First, we examine whether negative and positive caregiving experiences differ by caregivers’ gender and relationship. Second, we differentiate the relative importance of risk factors for negative and positive caregiving experiences among wife, husband, daughter, and son caregivers, respectively. Last, we identify common and unique risk factors for caregivers of different genders and in different relationships. By distinguishing the risk factors that are associated with the caregiving experiences of wives, husbands, daughters, and sons, the study is expected to shed light on interventions needed to better match their common and unique needs.
Methods
Data used in the analysis come from the 2004 wave of the National Long-Term Care Survey (NLTCS), a longitudinal study of Medicare beneficiaries age 65 or older that has been conducted since 1982. The interviews were repeated in 1984, 1989, 1994, 1999, and 2004. To offset high sample attrition because of mortality within this population, the data were refreshed in each wave with a sample of persons who turned 65 after the previous survey. Respondents with one or more limitations (ADL or IADL) that had lasted or were expected to last at least three months were screened to receive a detailed interview. Primary informal caregivers, identified by the disabled community-dwelling respondents, were subsequently interviewed in a supplemental survey. The caregiver survey provides rich information on caregivers’ demographic background, health, and employment; the amounts and types of help provided to elderly respondents; and caregiving experiences. Several studies have used earlier waves of the NLTCS data to examine caregiving experience (e.g., Ingersoll-Dayton & Raschick, 2004; Kang, 2006; Mui, 1995). The current study adds to this line of literature by considering both negative and positive caregiving experiences simultaneously and identifying common and unique risk factors for caregivers of different genders and in different relationships to the recipients.
In 2004, 20,474 older adults were randomly selected from Medicare beneficiary enrollment files. Of them, 5,201 community-dwelling older adults were screened to receive detailed interviews, 2,300 of which reported receiving unpaid help and identified a primary caregiver. In the end, 1,923 caregivers completed the caregiver survey. Because the current investigation focuses on spouse and adult-child caregivers, 371 caregivers who were other relatives or unrelated individuals were excluded (19.29% of the completed caregiver interviews). In total, the analysis consisted of 1,552 caregivers, including 357 wives, 265 husbands, 649 daughters, and 281 sons. One advantage of the NLTCS is that it recruited caregivers of older adults with at least one functional limitation, regardless of whether or not they had an illness. This is in contrast with the samples used in most prior studies, which have concentrated on caregivers whose care recipients had dementia or specific health problems (e.g., Lawton et al., 1991; Lutzky & Knight, 1994). Thus, relative to other studies, the NLTCS sample better represents the caregiver population in general.
Measures
Negative caregiving experience was measured by 12 items. Five items measure interference by asking caregivers whether they experienced loss of privacy; limits on social life or free time; giving constant attention to the care recipient; having less time for other family members; and giving up vacations, hobbies, or own activities as a result of caregiving (0 = no, 1 = yes). Three items focus on strain by asking caregivers to what extent they experienced physical, emotional, and financial strains because of caregiving (on a scale from 1 = not a strain at all to 5 = very much of a strain). Four items assess burnout by asking caregivers the extent to which they agreed with the following statements: (a) you are exhausted when you go to bed at night, (b) you have more things to do than you can handle, (c) you don’t have time just for yourself, and (d) you work hard as a caregiver but never seem to make any progress. Response categories ranged from not at all (1) to completely (4). We used all of these 12 items as indicators of the latent factor of caregivers’ negative experiences. These items have been used by prior researchers to measure negative caregiving experiences (interference: Kang, 2006; strain: Scharlach, Li, & Dalvi, 2006; and burnout: Ingersoll-Dayton & Raschick, 2004) and have a high reliability (α = .90).
Positive caregiving experience was gauged by two questions asking caregivers to what degree caregiving made them feel good about themselves and appreciate life more (on a scale from 1 = disagree a lot to 5 = agree a lot). We used these two items as indicators of the latent factor of caregivers’ positive experience. These two items are highly correlated (α = .78) and have been used by past studies to assess positive caregiving experience (Kang, 2006; Rashchick & Ingersoll-Dayton, 2004).
Care recipient’s problem behavior was measured by 15 items, including behaviors that occurred during the week prior to the interview, such as repeating questions or stories, hiding or forgetting about belongings, acting depressed or downhearted, becoming irritable or angry, and swearing or using foul language. Response categories varied from no day (1) to five or more days (4). We combined these items to create a scale (α = .82) ranging from 15 to 60, with a higher score representing a greater frequency of problem behaviors. Care recipient’s dependency was assessed by asking caregivers how many hours (0-24) at a time the care recipient could be left alone at home. We reversed the answers so that longer hours indicate a greater degree of dependency. Caregiver’s involvement was appraised by the number of hours that caregivers spent in a typical week helping the care recipient with ADLs or IADLs. These questions have been used by previous researchers to measure care recipients’ problem behavior (Kang, 2006; Ingersoll-Dayton & Raschick, 2004; Rashchick & Ingersoll-Dayton, 2004), dependency (Kasper, Steinbach, & Andrews, 1994), and caregivers’ involvement (Ingersoll-Dayton & Raschick, 2004; Rashchick & Ingersoll-Dayton, 2004).
Reciprocal help from care recipient was assessed by asking caregivers whether or not the care recipient had done the following for them: helped with household chores, babysat, gave money, provided company, or made caregivers feel useful or needed (0 = no, 1 = yes). Responses were summed such that higher scores indicate higher perceived reciprocal help (ranging from 0 to 5, α = .69). Availability of other caregivers was appraised by asking caregivers whether there was anyone else who could step in when they were unavailable to take care of the care recipient (0 = no, 1 = yes). Family conflict was evaluated by asking caregivers how much disagreement they had with their family members because they did not visit or call enough, did not give enough help, did not show enough appreciation, or gave unwanted advice. The response categories ranged from no disagreement (1) to quite a bit of disagreement (4). We combined these items to create a scale (α = .89) ranging from 4 to 16, with higher scores representing greater family conflict. Support from friends or relatives was examined by asking caregivers to what extent they had friends or relatives who cared and helped them, who made them feel good about themselves, and in whom they could confide and whom they wanted to be with when feeling down (on a scale from 1 = strongly disagree to 4 = strongly agree). We added these items to create a scale (α = .96) ranging from 7 to 28, with higher scores showing more perceived support. These measures have been adopted by prior researchers to capture reciprocal help (Dwyer et al., 1994; Kasper et al., 1994), availability of other caregivers (Mui, 1995), family conflict (Kang, 2006), and support from friends or relatives (Pearlin, Mullan, Semple, & Skaff, 1990).
Caregiver’s demographic characteristics
Race was classified as White (reference group), Black, Hispanic, and others. Education consisted of four categories: less than high school, high-school graduate (reference group), post high school, and bachelor’s degree or higher. Employment was determined by the number of hours working per week. Self-reported health was assessed by asking caregivers to rate their physical health (on a scale from 1 = poor to 4 = excellent). Each spouse caregiver was married to a care recipient and had no minor children living in the same household. Thus, these two variables (marital status and number of minor children) cannot predict negative and positive caregiving experiences for spouse caregivers. Because we conducted a multiple-group analysis (explained in the following section) that requires using the same covariates across different types of caregivers, these two variables were excluded from the analysis. In addition, age was highly correlated with generation (i.e., spouse versus adult-child caregivers), so it was also excluded. In this sample, the average ages of wife, husband, daughter, and son caregivers were 74, 77, 57, and 56 years old, respectively. Finally, a preliminary analysis suggested that income, coresidence status, and duration of caregiving are uncorrelated with caregivers’ caregiving experience. They were, therefore, excluded from the analysis.
Analytic strategy
Two analyses were conducted. The first analysis addressed whether caregivers’ negative and positive experiences differed by their gender and relationship to care recipients. Proportions or means of the items measuring negative or positive caregiving experiences were computed separately for wife, husband, daughter, and son caregivers. Chi-squared and t tests were conducted to examine the differences in proportions and means, respectively, between wives and husbands, daughters and sons, wives and daughters, and husbands and sons. Comparing proportions or means between wife and husband caregivers and between daughter and son caregivers tells us whether there is a gender difference. Similarly, comparing proportions or means between wife and daughter caregivers and between husband and son caregivers informs us whether there is a relationship difference. Moreover, we examined the patterns of the correlations between the 12 items about negative caregiving experience and the two items about positive caregiving experience to justify that negative and positive caregiving experiences are two separate constructs.
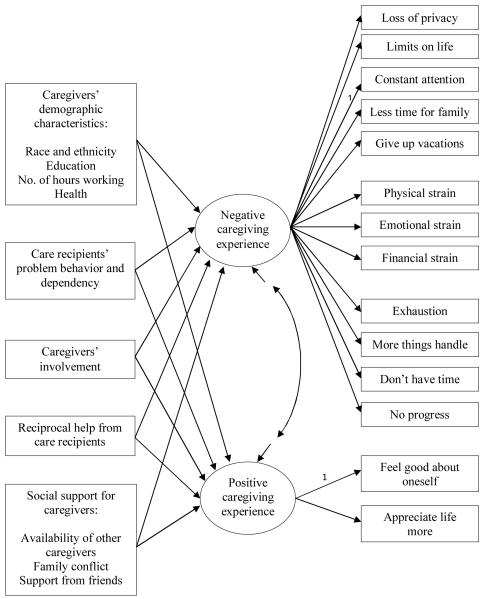
The second analysis addressed how care recipients’ problem behavior and dependency, caregivers’ involvement, reciprocal help from care recipients, and social support affected caregivers’ negative and positive experiences separately for wife, husband, daughter, and son caregivers. We estimated a multiple indicators and multiple causes model (MIMIC model, see Bollen, 1989). As shown in Figure 1, caregivers’ negative experience has direct effects on 12 items measuring negative caregiving experience; whereas caregivers’ positive experience has direct effects on two items: feeling good about oneself and appreciating life more. Both negative and positive caregiving experiences are affected by caregivers’ demographic characteristics, care recipients’ problem behavior and dependency, caregivers’ involvement, reciprocal help from care recipients, and social support available for caregivers. The model takes into account negative and positive caregiving experiences simultaneously and allows us to examine whether risk factors have the same effects on negative and positive caregiving experiences. All of the risk factors are allowed to be correlated in the model, as are all items within each subscale of negative experience, but these correlations are not shown in the figure to simplify the presentation.
Figure 1.
Conceptual Model
Note. To simplify the presentation, correlations among exogenous variables and residual correlations among five items measuring perceived interference, among three items measuring strain, and among four items measuring burnout are not shown. Factor loading from negative caregiving experience to the indicator, constant attention, and factor loading from positive caregiving experience to the indictor, feel good about oneself, are set to equal 1 in order to identify the model (Bollen, 1989).
Because wives, husbands, daughters, and sons may have different caregiving experiences and there may be different risk factors associated with their experiences, the MIMIC model was combined with a multiple-group analysis (Bollen, 1989). One advantage of this analytic strategy is that equality constraints can be placed on regression coefficients within and between groups. Thus, comparing regression coefficients within each type of caregivers tells us the relative importance of each risk factor. Comparing regression coefficients across caregivers of different genders and in different relationships helps us identify the common and unique factors that are associated with caregiving experiences. The analysis was conducted using the statistical package Mplus Version 6.1 (Muthén & Muthén, 2010). Information was missing in some respondents’ reports, ranging from .3% (caregiver’s race) to 4.5% (number of hours that caregivers spent helping care recipients). The missing value for a single variable was imputed as a function of other covariates in the analysis (Acock, 2005; Royston, 2004, 2005). To preserve the randomness of the imputed variables, the results described next are based on 10 random, multiple-imputed replicates. We first fitted the model that allows all regression coefficients, factor loadings, and residual correlations to be freely estimated and then constrained nonsignificant coefficients to be zero after determining that such a constraint would not worsen the model fit. Because the study uses a large sample size, a model is considered to fit the data well when a comparative fit index is greater than .95, a Tucker-Lewis index is greater than .95, and a root mean square error of approximation is less than .06 (Hu & Bentler, 1999).
Results
Table 1 shows the correlation matrices and proportions or means of items measuring negative and positive caregiving experiences for wife, husband, daughter, and son caregivers, respectively. Items 1 through 12 measure negative experience, and items 13 and 14 measure positive experience. The upper and lower off-diagonal elements represent item correlations for wife and husband caregivers, respectively, in the first panel; whereas the upper and lower off-diagonal elements represent item correlations for daughter and son caregivers, respectively, in the second panel. Positive correlations were found among items measuring negative experience and among items measuring positive experience, whereas negative correlations were found between items measuring negative experience and items measuring positive experience. In addition, the small magnitudes of these negative correlations suggest that negative caregiving experience is not just the reverse of positive caregiving experience, and both negative and positive experiences are two related but separate constructs.
Table 1.
Proportions or Means of Respondents Who Reported Caregiving Experiences and Correlations among These Experiences
| Wife | Husband | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Loss of privacybcd | .17 | .12 | .85 | .62 | .56 | .52 | .59 | .62 | .46 | .56 | .61 | .68 | .66 | −.08 | −.05 | |
| 2. Limits on social lifeacd | .32 | .20 | .78 | .67 | .72 | .78 | .74 | .75 | .53 | .64 | .66 | .76 | .69 | −.12 | −.26 | |
| 3. Giving constant attention | .25 | .22 | .61 | .78 | .56 | .68 | .68 | .58 | .41 | .52 | .51 | .59 | .59 | .00 | −.10 | |
| 4. Less time for family membersabcd | .28 | .17 | .53 | .76 | .61 | .85 | .57 | .64 | .43 | .62 | .57 | .64 | .61 | −.13 | −.07 | |
| 5. Giving up vacations or hobbiesabcd | .37 | .24 | .53 | .79 | .59 | .77 | .67 | .70 | .56 | .64 | .61 | .67 | .64 | −.11 | −.13 | |
| 6. Physical strainab | 2.06 | 1.78 | .63 | .58 | .61 | .48 | .42 | .79 | .61 | .61 | .66 | .74 | .69 | −.04 | −.15 | |
| 7. Emotional strainab | 2.25 | 1.85 | .68 | .68 | .72 | .53 | .54 | .82 | .63 | .69 | .72 | .75 | .78 | −.13 | −.16 | |
| 8. Financial strain | 1.72 | 1.72 | .45 | .67 | .58 | .60 | .58 | .72 | .66 | .54 | .63 | .60 | .58 | .01 | −.09 | |
| 9. Exhaustionabc | 2.10 | 1.70 | .46 | .61 | .61 | .52 | .55 | .57 | .61 | .58 | .79 | .73 | .70 | −.11 | −.13 | |
| 10. More things than one can handleabc | 1.77 | 1.51 | .45 | .53 | .43 | .50 | .48 | .52 | .54 | .51 | .68 | .79 | .79 | −.17 | −.15 | |
| 11. Don’t have time for oneselfabc | 1.78 | 1.49 | .63 | .79 | .75 | .60 | .64 | .59 | .72 | .58 | .72 | .70 | .81 | −.17 | −.17 | |
| 12. Working hard but no progressab | 1.63 | 1.37 | .59 | .73 | .65 | .62 | .57 | .58 | .63 | .60 | .66 | .69 | .79 | −.19 | −.22 | |
| 13. Feeling good about oneselfac | 3.09 | 3.31 | −.11 | −.18 | −.15 | −.16 | −.07 | −.14 | −.06 | −.08 | −.05 | −.11 | −.11 | −.16 | .72 | |
| 14. Appreciating life moreac | 3.16 | 3.31 | −.10 | −.20 | −.02 | .07 | −.02 | −.16 | −.16 | −.08 | −.11 | −.06 | −.10 | −.04 | .79 |
| Daughter | Son | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Loss of privacybcd | .32 | .25 | .76 | .55 | .62 | .63 | .53 | .58 | .44 | .53 | .53 | .60 | .59 | −.18 | −.17 | |
| 2. Limits on social lifeacd | .46 | .39 | .88 | .77 | .76 | .88 | .64 | .68 | .54 | .61 | .66 | .75 | .67 | −.09 | −.09 | |
| 3. Giving constant attention | .23 | .18 | .78 | .81 | .58 | .63 | .69 | .62 | .49 | .57 | .55 | .65 | .68 | .01 | .02 | |
| 4. Less time for family membersabcd | .42 | .28 | .51 | .77 | .44 | .82 | .54 | .56 | .40 | .54 | .55 | .63 | .56 | −.02 | −.05 | |
| 5. Giving up vacations or hobbiesabcd | .46 | .33 | .59 | .82 | .66 | .76 | .57 | .59 | .51 | .54 | .56 | .64 | .58 | −.12 | −.13 | |
| 6. Physical strainab | 1.92 | 1.62 | .51 | .64 | .62 | .40 | .57 | .72 | .65 | .62 | .57 | .58 | .65 | −.08 | −.13 | |
| 7. Emotional strainab | 2.41 | 2.05 | .64 | .74 | .55 | .62 | .65 | .76 | .62 | .59 | .61 | .64 | .68 | −.16 | −.18 | |
| 8. Financial strain | 1.61 | 1.55 | .56 | .61 | .59 | .48 | .59 | .60 | .63 | .51 | .54 | .55 | .59 | −.17 | −.17 | |
| 9. Exhaustionabc | 1.97 | 1.60 | .56 | .61 | .57 | .48 | .57 | .59 | .61 | .53 | .77 | .75 | .74 | −.10 | −.03 | |
| 10. More things than one can handleabc | 1.91 | 1.56 | .43 | .64 | .49 | .57 | .63 | .58 | .65 | .59 | .75 | .79 | .76 | −.08 | −.05 | |
| 11. Don’t have time for oneselfabc | 1.92 | 1.56 | .53 | .79 | .59 | .60 | .71 | .53 | .64 | .64 | .70 | .79 | .73 | −.03 | −.10 | |
| 12. Working hard but no progressab | 1.57 | 1.37 | .50 | .73 | .54 | .51 | .64 | .61 | .65 | .66 | .62 | .70 | .75 | −.15 | −.13 | |
| 13. Feeling good about oneselfac | 3.39 | 3.36 | −.03 | −.09 | .14 | −.08 | −.02 | .09 | −.04 | .10 | .05 | −.04 | −.04 | .05 | .73 | |
| 14. Appreciating life moreac | 3.37 | 3.25 | −.05 | −.13 | .21 | −.07 | .04 | .01 | −.15 | .06 | .07 | .00 | −.01 | .18 | .77 |
Note. Item correlations for wife and daughter caregivers are listed on the upper-off diagonal; item correlations for husband and son caregivers are listed on the lower-off diagonal.
Denotes statistically significant difference between wife and husband caregivers at p < .05.
Denotes statistically significant difference between daughter and son caregivers at p < .05.
Denotes statistically significant difference between wife and daughter caregivers at p < .05.
Denotes statistically significant difference between husband and son caregivers at p < .05.
Given that negative and positive experiences are two separate constructs, we examined whether their proportions or means vary by caregivers’ gender and relationship to care recipients. When the proportions or means of these items are examined across genders, most items (except items 3 and 8) show significant differences in the proportions or means between wife and husband caregivers and/or between daughter and son caregivers. Specifically, compared with their male counterparts, wife and daughter caregivers were more likely to have less time for family members (item 4), give up vacations or hobbies (item 5), have physical or emotional strain (items 6 and 7), feel exhaustion (item 9), feel that they have more things to do than one can handle (item 10), not have time for oneself (item 11), and work hard but no progress (item 12). In addition, some gender differences were observed only for particular relationships. Whereas wife and husband caregivers reported similar likelihoods of losing their privacy (item 1), daughter caregivers were more likely to say they lost privacy than were son caregivers. In contrast, whereas daughter and son caregivers expressed similar likelihoods of feeling limitations on their social lives, wife caregivers were more likely to report such limits than were husband caregivers (item 2). As for the items measuring positive caregiving experience, gender differences were found only between wife and husband caregivers, with wife caregivers feeling less good about themselves (item 13) and appreciating life less (item 14) than husband caregivers.
When negative and positive caregiving experiences are examined across relationships, the majority of measures (except items 3, 6, 7, 8, and 12) show significant differences in the proportions or means between wife and daughter caregivers and/or between husband and son caregivers. Specifically, compared with wife and husband caregivers, daughter and son caregivers were more likely to report loss of privacy (item 1), limits on social lives (item 2), less time for family members (item 4), and giving up vacations or hobbies (item 5), respectively. In addition, some relationship differences were observed only for a specific gender. Whereas husband and son caregivers reported having similar levels of exhaustion (item 9), feeling they had more things than one can handle (item 10), and having less time for themselves (item 11), wife caregivers reported more exhaustion, having fewer things than one can handle, and having more time for themselves than daughter caregivers. Regarding the items measuring positive caregiving experience, a relationship difference was found between wife and daughter caregivers only, with wife caregivers feeling less good about themselves (item 13) and appreciating life less (item 14) than daughter caregivers.
The finding that negative and positive caregiving experiences varied by gender and relationship implies that risk factors of caregiving experiences may also differ for caregivers of different genders and in different relationships. Results in Table 2 show that female caregivers had completed fewer years of schooling and reported more problem behaviors of care recipients than did male caregivers. Compared with son caregivers, daughter caregivers were more likely to be minorities, spent less time working but more hours helping, and received more reciprocal help from care recipients and support from friends or relatives.
Table 2.
Caregivers’ Demographic Characteristics, Care Recipients’ Problem Behavior and Dependency, Caregivers’ Involvement, Reciprocal Help from Care Recipients, and Social Support Available for Caregivers
| Wife | Husband | Daughter | Son | |
|---|---|---|---|---|
| Caregivers’ demographic characteristics | ||||
| Race and ethnicitybc | ||||
| White | 83.75 | 90.84 | 76.27 | 86.07 |
| Black | 4.76 | 3.51 | 12.33 | 7.47 |
| Hispanic | 6.44 | 3.43 | 7.55 | 4.27 |
| Other race | 5.04 | 2.30 | 3.85 | 2.14 |
| Educationabcd | ||||
| Less than high school | 31.68 | 29.02 | 12.34 | 12.06 |
| High school graduate | 38.57 | 29.58 | 33.53 | 29.64 |
| Post high school | 20.78 | 26.23 | 32.00 | 27.72 |
| Bachelor’s degree or higher | 8.96 | 15.17 | 22.13 | 30.57 |
| Number of hours working per week (0-80)bcd | 3.54 | 3.17 | 16.72 | 20.80 |
| Self-reported healthc | ||||
| Poor | 6.19 | 6.98 | 5.01 | 7.58 |
| Fair | 25.83 | 26.15 | 19.85 | 16.83 |
| Good | 50.11 | 43.25 | 49.23 | 47.01 |
| Excellent | 17.87 | 23.62 | 25.92 | 28.58 |
| Care recipients’ problem behavior (15-60)ab | 19.67 | 18.31 | 20.01 | 18.88 |
| Care recipients’ dependency (0-24) | 13.07 | 12.22 | 11.86 | 10.76 |
| Caregivers’ involvement (0-168)bcd | 32.85 | 30.31 | 25.02 | 19.96 |
| Reciprocal help from care recipients (0-5)bcd | 2.77 | 2.98 | 2.58 | 2.33 |
| Availability of other caregivers (1 = Yes)cd | 55.83 | 60.11 | 69.57 | 69.96 |
| Family conflict (4-16)cd | 4.76 | 4.54 | 5.66 | 5.42 |
| Support from friends or relatives (7-28)bc | 22.08 | 21.54 | 22.80 | 21.82 |
| N | 357 | 265 | 649 | 281 |
Note. Column totals in each panel may deviate slightly from 100% due to rounding errors.
Denotes statistically significant difference between wife and husband caregivers at p < .05.
Denotes statistically significant difference between daughter and son caregivers at p < .05.
Denotes statistically significant difference between wife and daughter caregivers at p < .05.
Denotes statistically significant difference between husband and son caregivers at p < .05.
Relative to adult-child caregivers, spouse caregivers had completed fewer years of schooling, spent less time working but more hours helping, received more reciprocal help from care recipients, were less likely to have someone else available to take their place if they could not provide help, and experienced a lower level of family conflict. Daughter caregivers were more likely to be minorities, reported better health, and received more support from friends or relatives than did wife caregivers. In sum, these results suggest that wife, husband, daughter, and son caregivers hold different resources and face different challenges while taking on the caregiver role. In the following, we investigate the relative importance of these risk factors within each type of caregiver and identify common and unique risk factors across the four caregiver types.
Relative importance of risk factors for negative and positive experiences
A multiple-group MIMIC model was estimated to obtain standardized regression coefficients of risk factors for wife, husband, daughter, and son caregivers’ negative and positive caregiving experiences. The model has a root mean square error of .023, a comparative fit index of .979, and a Tucker-Lewis index of .979, suggesting that this model fits the data well. Table 3 shows the standardized coefficients from the regressions of negative and positive caregiving experiences on caregivers’ demographic characteristics, care recipients’ problem behavior and dependency, caregivers’ involvement, reciprocal help from care recipients, and social support available for wife, husband, daughter, and son caregivers. The R2 values for negative caregiving experience are higher than those for positive experience for wife, husband, daughter, and son caregivers, indicating that negative experience is better explained by these risk factors than is positive experience.
Table 3.
Standardized Coefficients for Structural Equation Model of Negative and Positive Caregiving Experiences
| Wife |
Husband |
Daughter |
Son |
|||||
|---|---|---|---|---|---|---|---|---|
| Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | |
| Caregivers’ demographic characteristics | ||||||||
| Race and ethnicity (Reference group: White) | ||||||||
| Black | - | - | - | - | −.100 | - | - | - |
| Hispanic | - | - | - | - | - | .137 | - | - |
| Other race | - | - | - | - | - | - | - | - |
| Education (Reference group: High school graduate) | ||||||||
| Less than high school | - | - | - | - | - | - | - | .247 |
| Post high school | - | - | - | - | - | - | - | - |
| Bachelor’s degree or higher | - | - | - | - | .106 | - | - | - |
| Number of hours working per week | - | - | .132 | - | .101 | - | - | - |
| Self-reported health | −.177 | - | −.172 | - | −.123 | - | - | - |
| Care recipients’ problem behavior | .493 | - | .486 | −.150 | .445 | - | .529 | - |
| Care recipients’ dependency | .322 | - | .201 | - | .136 | - | .139 | - |
| Caregivers’ involvement | - | - | .199 | - | .159 | - | - | - |
| Reciprocal help from care recipients | - | .303 | - | - | - | .162 | - | .205 |
| Availability of other caregivers | −.111 | - | - | - | −.153 | .154 | −.207 | - |
| Family conflict | .125 | - | - | - | .206 | - | .209 | .285 |
| Support from friends or relatives | - | - | - | - | - | .216 | - | - |
| R2 | .602 | .092 | .563 | .022 | .600 | .132 | .541 | .199 |
| Residual correlation between negative and positive experiences | −.212 | - | −.131 | −.192 | ||||
| N | 357 | 265 | 649 | 281 | ||||
| Model fit | χ2 = 1416.741, df = 1170, RMSEA = .023, CFI = .979, TLI = .979 | |||||||
Note. All coefficients significantly differ from zero at p < .05.
-Denotes nonsignificant coefficients or correlations that have been constrained to be zero.
Standardized regression coefficients can be used to compare the relative importance of risk factors within each group of caregivers. Wife caregivers’ negative caregiving experience was inversely associated with caregivers’ health and the availability of other caregivers but positively associated with the care recipient’s problem behavior and dependency and family conflict. Based on the absolute values of the regression coefficients, care recipients’ problem behavior was the most important risk factor related to wife caregivers’ negative experience, whereas the availability of other caregivers was the least. Wife caregivers’ positive experience was positively correlated with reciprocal help from care recipients only, suggesting that caregivers also need to be cared for or appreciated by care recipients. There was no common risk factor for both negative and positive caregiving experiences of wife caregivers.
Husband caregivers’ negative caregiving experience was inversely related to caregivers’ health but positively related to the number of hours working, care recipients’ problem behavior and dependency, and caregivers’ involvement. Care recipients’ problem behavior was the most important risk factor for husband caregivers’ negative experience, whereas the number of hours working was the least. Husband caregivers’ positive experience was negatively associated with care recipients’ problem behavior. Care recipients’ problem behavior was a risk factor for both negative and positive caregiving experiences of husband caregivers.
Daughter caregivers’ negative caregiving experience was inversely correlated with being Black, caregivers’ health, and the availability of other caregivers, but was positively correlated with having a bachelor’s degree or higher, the number of hours working, care recipients’ problem behavior and dependency, caregivers’ involvement, and family conflict. Care recipients’ problem behavior was the most important risk factor for daughter caregivers’ negative experience, whereas being Black was the least. Daughter caregivers’ positive experience was positively related to being Hispanic, receiving reciprocal help from care recipients, the availability of other caregivers, and support from friends or relatives. Support from friends or relatives was the most important risk factor for daughter caregivers’ positive experience, whereas being Hispanic was the least. The availability of other caregivers was a risk factor for both negative and positive caregiving experiences of daughter caregivers.
Son caregivers’ negative caregiving experience was inversely associated with the availability of other caregivers, but positively associated with care recipients’ problem behavior and dependency and family conflict. Care recipients’ problem behavior was the most important risk factor for son caregivers’ negative experience, whereas care recipients’ dependency was the least. Son caregivers’ positive experience was positively related to having a less than high school education, reciprocal help from care recipients, and family conflict. The positive association between family conflict and positive experience implies that unlike wife and daughter caregivers, son caregivers were able to find positive meaning from care provision when family conflict was high. Family conflict was the most important risk factor of son caregivers’ positive experience, whereas reciprocal help from care recipients was the least. Family conflict was a risk factor for both negative and positive caregiving experiences of son caregivers.
In sum, different risk factors that were related to both negative and positive experiences were found for husband, daughter, and son caregivers, respectively, but no common risk factor was found for wife caregivers. Moreover, when more than one risk factor was associated with caregiving experiences, the ranking of the importance of these risk factors also varied by caregivers’ gender and relationship. These findings suggest that risk factors associated with both negative and positive experiences vary by caregivers’ gender and relationship.
Common and unique risk factors across caregivers’ gender and relationship
When coefficients were compared across wife, husband, daughter, and son caregivers in Table 3, we found that two common risk factors (i.e., care recipients’ problem behavior and dependency) were related to negative caregiving experience for all four groups of caregivers. In contrast, two unique factors (i.e., being Black and having a bachelor’s degree or higher) were associated with negative experience for daughter caregivers only. Other risk factors that were associated with negative experiences appeared in two or three groups of caregivers. The number of hours working and caregiver’s involvement were risk factors for husband and daughter caregivers’ negative experience, but not that of wife and son caregivers. Poor health was a risk factor for wife, husband, and daughter caregivers’ negative experience, but not son caregivers’. The availability of other caregivers and family conflict were risk factors for wife, daughter, and son caregivers’ negative experience but not husband caregivers’.
In addition, there was no common risk factor correlated with positive caregiving experience for all four groups of caregivers. By contrast, one unique factor was found for husband caregivers (i.e., care recipients’ problem behavior), three unique factors for daughter caregivers (i.e., being Hispanic, the availability of other caregivers, and support from friends or relatives), and two unique factors for son caregivers (i.e., having a less than high school education and family conflict). Only one risk factor that was associated with positive experience appeared in three groups of caregivers: Reciprocal help from care recipients was a risk factor for wife, daughter, and son caregivers, but not for husband caregivers.
To conclude, only two common risk factors related to negative caregiving experience and no common risk factor related to positive caregiving experience were identified for the four groups of caregivers. Most risk factors for negative and positive experiences varied by caregivers’ gender and relationship. This finding underscores the importance of considering the intersection of caregivers’ gender and relationship to care recipients when examining caregiving experiences.
Summary and Discussion
This study shows that negative and positive caregiving experiences are two related but separate constructs. Consistent with our hypothesis, female and adult-child caregivers generally expressed more negative experiences than did male and spouse caregivers, respectively. Partially consistent with our expectation, male caregivers were more likely than female caregivers to find positive meaning from care provision, but this occurred among spouses only. In addition, adult-child caregivers tended to acquire personal gratification from care provision more than did spouse caregivers, but this happened among women only.
We found partial support for our hypotheses regarding how risk factors may vary by caregivers’ gender. Specifically, long hours of care provision were more stressful for male caregivers than for female caregivers, whereas reciprocal help from care recipients, the availability of other caregivers, and a lower level of family conflict were more helpful for female caregivers than for male caregivers, but these patterns were observed among spouses only. Support from friends or relatives was more beneficial to female caregivers than to male caregivers, but this occurred among adult children only.
We also found partial support for our hypotheses regarding how risk factors may vary by caregivers’ relationship. The availability of other caregivers and a lower level of family conflict were more helpful in reducing negative experiences for adult-child caregivers than for spouse caregivers, but the associations were found among men only. Support from friends or relatives benefits adult-child caregivers more than spouse caregivers, whereas long hours of care provision hurts adult-child caregivers more than spouse caregivers, but these results only hold among women. In sum, we found that both negative and positive caregiving experiences and their risk factors varied not only by caregivers’ gender but also by their relationships to care recipients.
This study identifies both common and unique risk factors for caregivers of different genders and in different relationships to care recipients. We found that care recipients’ problem behavior and dependency were two common factors contributing to caregivers’ negative experiences. By contrast, the number of hours working per week, self-reported health, caregivers’ involvement, the availability of other caregivers, and family conflict had different effects on the negative caregiving experiences of wives, husbands, daughters, and sons, respectively. As for positive caregiving experiences, we found only unique risk factors, including care recipients’ problem behavior, reciprocal help from care recipients, the availability of other caregivers, and support from friends or relatives. These findings have important implications for both family practitioners and social-service providers.
For family practitioners, the unique risk factors found in this study underscore the need to use adaptive interventions (Collins, Murphy, & Bierman, 2004) in helping caregivers, because while some risk factors are universal, others are not. Thus, when designing adaptive interventions to help caregivers, family practitioners and caregivers can start with common factors and then move on to unique ones.
Moreover, this study suggests different programs that social-service agencies can provide to caregivers. For instance, education and training programs (Burns, Nichols, Martindale-Adams, Graney, & Lummus, 2003; Hébert et al., 2003) can help caregivers understand and manage care recipients’ behavioral problems and thus reduce caregivers’ negative experiences. Because care recipients’ problem behavior is related to negative caregiving experiences for all caregivers, these programs should benefit all caregivers. Similarly, the use of respite care, such as adult day care (Zarit et al., in press), which seeks to lessen care recipients’ dependency on caregivers, should also help all caregivers.
Other interventions, however, may benefit only certain subgroups of caregivers. Specifically, encouraging family members to share caregiving tasks and reducing family conflict may decrease negative feelings for wife and adult-child caregivers only. Reminding caregivers of the importance of taking care of one’s health is likely to increase well-being for spouse and daughter caregivers only, while for only husband and daughter caregivers is obtaining a balance of time spent on caregiving and paid work critical to relieving caregiving strains.
Although these services and programs are available in most communities, Barber and Lyness (2001) have noticed that the sense of family obligation and family boundaries often keep caregivers from using these services. Given that caregivers tend to seek help from friends, churches, or family counselors, it is important for these individuals and groups to pass along information about available social services and programs to caregivers who need support and to assist them in locating appropriate help (Fruhauf & Aberle, 2007; Ramsey, 2008).
The study has several limitations. First, it would be helpful to consider why these caregivers became primary caregivers in the first place (Henretta et al., 1997). The different experiences of wife, husband, daughter, and son caregivers examined in this study may be attributable to the family and individual factors that affect family members’ decisions to become the primary caregiver. Since we do not have information at the time when these respondents first became caregivers, however, we are unable to take selection into account in the analysis. Second, current data allow us to use only two items to gauge the positive experience of family caregivers—feeling good about oneself and appreciating life more. Although these two items correspond to two main dimensions of positive caregiving experience (Tarlow et al., 2004), they do not fully capture the experience. More items on positive caregiving experience are needed in future data-collection efforts. Third, care recipients’ cognitive impairment could impede the communication between caregivers and care recipients and subsequently affect caregiving experiences (Kasper et al., 1994; Scharlach et al., 2006). Nevertheless, the measure contains much missing data, and thus it would be unlikely to provide a reliable estimate; therefore, we did not include this variable in the analysis. Fourth, some caregivers may not be able to reflect on their caregiving experiences and derive personal satisfaction from them until after that responsibility ends (Mullan, 1992). Other caregivers may feel guilty about not doing enough for or having negative interactions with care recipients when they were alive (Gonyea, Paris, & Zerden, 2008). This study provides only a snapshot of active caregivers. To better understand caregiving experiences, we need to follow up on caregivers after they exit the caregiver role. Last, our analysis is limited to four types of caregivers because the current study focused on comparing caregivers of different genders and in different relationships (i.e., spouse and adult-child caregivers). It is important to examine other types of caregivers, such as grandchildren, as an increasing number of grandchildren are shouldering the responsibility of taking care of their frail grandparents (Fruhauf, Jarrott, & Allen, 2006; Orel & Dupuy, 2002).
Findings from this study point to several directions for future research. First, this study draws on prior literature about the risk factors of negative caregiving experience and examines whether these risk factors are also related to positive caregiving experience. Most of these risk factors did not predict positive caregiving experience in this study. Future studies should go beyond prior research and explore what other risk factors may be associated with positive caregiving experience. Second, we found that son caregivers’ personal gratification was positively related to family conflict. Although this finding is counter-intuitive, it suggests that son caregivers’ caregiving context is very different from other caregivers’. In the United States, it is usually daughters who care for the parents as they age. We know very little about what happens when sons step in to help and how they view their caregiver role (Matthews, 2002). It is plausible that they obtain personal gratification because they “help out” with caregiving responsibilities when family members cannot agree upon an arrangement for care provision. We need more research to understand how sons engage in caregiving and react to stress associated with it. Finally, we found that better-educated daughters experienced more stress from caregiving. We suspected that daughters with more education hold a less traditional gender ideology and thus experience more caregiving strains than daughters with less education. It remains elusive, however, as to why higher incomes and more resources that better educated daughters usually have could not help reduce their negative caregiving experiences. Further studies are needed to disentangle how gender ideology and income resources together affect caregiver stress among educated daughter caregivers.
Acknowledgments
The authors thank Susan L. Brown, the editor, and three anonymous reviewers for their helpful comments. Any opinions expressed here are solely those of the authors and not of the funding agency or Center.
Footnotes
This research was supported by a Faculty Development Award to the first author from the Center for Family and Demographic Research at Bowling Green State University, which receives core funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R24HD050959-07).
A version of this article was presented at the Institute of Gerontology, Wayne State University, Detroit, Michigan on March 8, 2011.
References
- Acock AC. Working with missing values. Journal of Marriage and Family. 2005;67:1012–1028. [Google Scholar]
- Barber CE, Lyness KP. Ethical issues in family care of older persons with dementia: Implications for family therapists. Home Health Care Services Quarterly. 2001;20:1–26. doi: 10.1300/J027v20n03_01. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. Wiley; New York, NY: 1989. [Google Scholar]
- Brewster KL, Padavic I. Change in gender-ideology, 1977-1996: The contributions of intracohort change and population turnover. Journal of Marriage and the Family. 2000;62:477–487. [Google Scholar]
- Brody EM. Women in the middle: Their parent care years. 2nd ed Springer; New York, NY: 2004. [Google Scholar]
- Burns R, Nichols LO, Martindale-Adams J, Graney MJ, Lummus A. Primary care interventions for dementia caregivers: 2-year outcomes from the REACH study. The Gerontologist. 2003;43:547–555. doi: 10.1093/geront/43.4.547. [DOI] [PubMed] [Google Scholar]
- Calasanti T, King N. Taking ‘women’s work’ ‘like a man’: Husbands’ experiences of care work. The Gerontologist. 2007;47:516–527. doi: 10.1093/geront/47.4.516. [DOI] [PubMed] [Google Scholar]
- Collins LM, Murphy SA, Bierman KL. A conceptual framework for adaptive preventive interventions. Prevention Science. 2004;5:185–196. doi: 10.1023/b:prev.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer JW, Lee GR, Jankowski TB. Reciprocity, elder satisfaction, and caregiver stress and burden: The exchange of aid in the family caregiving relationship. Journal of Marriage and the Family. 1994;56:35–43. [Google Scholar]
- Feinberg L, Reinhard SC, Houser A, Choula R. Valuing the invaluable: 2011 update, the growing contributions and costs of family caregiving. AARP Public Policy Institute; Washington, DC: 2011. Retrieved from http://www.aarp.org/relationships/caregiving/info-07-2011/valuing-the-invaluable.html. [Google Scholar]
- Fruhauf CA, Aberle JT. Women caring for partners with dementia: A contextual model. In: Linville D, Hertlein KM, Associates, editors. The therapist’s notebook for family health care: Homework, handouts, and activities for individuals, couples, and families coping with illness, loss, and disability. The Haworth Press; Binghamton, NY: 2007. pp. 157–165. [Google Scholar]
- Fruhauf CA, Jarrott SE, Allen KR. Grandchildren’s perceptions of caring for grandparents. Journal of Family Issues. 2006;27:887–911. [Google Scholar]
- Gonyea JG, Paris R, Zerden L. d. S. Adult daughters and aging mothers: The role of guilt in the experience of caregiver burden. Aging & Mental Health. 2008;12:559–567. doi: 10.1080/13607860802343027. [DOI] [PubMed] [Google Scholar]
- Harris PB. The voices of husbands and sons caring for a family member with dementia. In: Kramer BJ, Thompson EH Jr., editors. Men as caregivers: Theory, research, and service implications. Springer; New York, NY: 2002. pp. 213–233. [Google Scholar]
- Hébert R, Lévesque L, Vézina J, Lavoie J-P, Ducharme F, Gendron C, Préville M, Voyer L, Dubois M-F. Efficacy of a psychoeducative group program for caregivers of demented persons living at home: A randomized controlled trial. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2003;58:58–67. doi: 10.1093/geronb/58.1.s58. [DOI] [PubMed] [Google Scholar]
- Henretta JC, Hill MS, Li W, Soldo BJ, Wolf DA. Selection of children to provide care: The effect of earlier parental transfers. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1997;52:110–119. doi: 10.1093/geronb/52b.special_issue.110. [DOI] [PubMed] [Google Scholar]
- Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Ingersoll-Dayton B, Raschick M. The relationship between care-recipient behaviors and spousal caregiving stress. The Gerontologist. 2004;44:318–327. doi: 10.1093/geront/44.3.318. [DOI] [PubMed] [Google Scholar]
- Johnson RW, Wiener JM. A profile of frail older Americans and their caregivers. The Urban Institute; Washington, DC: 2006. Retrieved from http://www.urban.org/UploadedPDF/311284_older_americans.pdf. [Google Scholar]
- Kang SY. Predictors of emotional strain among spouse and adult child caregivers. Journal of Gerontological Social Work. 2006;47:107–131. doi: 10.1300/J083v47n01_08. [DOI] [PubMed] [Google Scholar]
- Kasper JD, Steinbach U, Andrews J. Caregiver role appraisal and caregiver tasks as factors in ending caregiving. Journal of Aging and Health. 1994;6:397–414. doi: 10.1177/089826439400600307. [DOI] [PubMed] [Google Scholar]
- Kramer BJ. Gain in the caregiving experience: Where are we? What next? The Gerontologist. 1997;37:218–232. doi: 10.1093/geront/37.2.218. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. The two-factor model of caregiving appraisal and psychological well-being. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1991;46:181–189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- Lee GR, Netzer JK, Coward RT. Filial responsibility expectations and patterns of intergenerational assistance. Journal of Marriage and the Family. 1994;56:559–565. [Google Scholar]
- Li LW, Seltzer MM, Greenberg JS. Social support and depressive symptoms: Differential patterns in wife and daughter caregivers. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1997;52:200–211. doi: 10.1093/geronb/52b.4.s200. [DOI] [PubMed] [Google Scholar]
- Lutzky SM, Knight BG. Explaining gender differences in caregiver distress: The roles of emotional attentiveness and coping styles. Psychology and Aging. 1994;9:513–519. doi: 10.1037//0882-7974.9.4.513. [DOI] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proceedings of the National Academy of Sciences. 2006;103:18374–18379. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks NF, Lambert JD, Choi H. Transitions to caregiving, gender, and psychological well-being: A prospective U.S. national study. Journal of Marriage and Family. 2002;64:657–667. [Google Scholar]
- Matthews SH. Brothers and parent care: An explanation for sons’ underrepresentation. In: Kramer BJ, Thompson EH Jr., editors. Men as caregivers: Theory, research, and service implications. Springer; New York, NY: 2002. pp. 234–249. [Google Scholar]
- Miller B, Townsend A, Carpenter E, Montgomery RVJ, Stull D, Young RF. Social support and caregiver distress: A replication analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2001;56:249–256. doi: 10.1093/geronb/56.4.s249. [DOI] [PubMed] [Google Scholar]
- Mui AC. Caring for frail elderly parents: A comparison of adult sons and daughters. The Gerontologist. 1995;35:86–93. doi: 10.1093/geront/35.1.86. [DOI] [PubMed] [Google Scholar]
- Mullan JT. The bereaved caregiver: A prospective study of changes in well-being. The Gerontologist. 1992;32:673–683. doi: 10.1093/geront/32.5.673. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus: Statistical analysis with latent variables. Version 6.1 Author; Los Angeles, CA: 2010. [Google Scholar]
- National Alliance for Caregiving Caregiving in the U.S.: A focused look at those caring for the 50+ 2009 Retrieved from http://assets.aarp.org/rgcenter/il/caregiving_09.pdf.
- Neal MB, Ingersoll-Dayton B, Starrels ME. Gender and relationship differences in caregiving patterns and consequences among employed caregivers. The Gerontologist. 1997;37:804–816. doi: 10.1093/geront/37.6.804. [DOI] [PubMed] [Google Scholar]
- Orel NA, Dupuy P. Grandchildren as auxiliary caregivers for grandparents with cognitive and/or physical limitations: Coping strategies and ramifications. Child Study Journal. 2002;32:193–213. [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2003;58:112–128. doi: 10.1093/geronb/58.2.p112. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: A meta-analysis. The Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: An updated meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2006;61:33–45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- Ramsey JL. Forgiveness and healing in later life. Generations. 2008;32:51–54. [Google Scholar]
- Raschick M, Ingersoll-Dayton B. The costs and rewards of caregiving among aging spouses and adult children. Family Relations. 2004;53:317–325. [Google Scholar]
- Royston P. Multiple imputation of missing values. The Stata Journal. 2004;4:227–241. [Google Scholar]
- Royston P. Multiple imputation of missing values: Update. The Stata Journal. 2005;5:188–201. [Google Scholar]
- Scharlach A, Li W, Dalvi TB. Family conflict as a mediator of caregiver strain. Family Relations. 2006;55:625–635. [Google Scholar]
- Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- Stephens MAP, Townsend AL, Martire LM, Druley JA. Balancing parent care with other roles: Interrole conflict of adult daughter caregivers. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2001;56:24–34. doi: 10.1093/geronb/56.1.p24. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Wallhagen MI. Impact on family conflict on adult child caregivers. The Gerontologist. 1991;31:770–777. doi: 10.1093/geront/31.6.770. [DOI] [PubMed] [Google Scholar]
- Tarlow BJ, Wisniewski SR, Belle SH, Rubert M, Ory MG, Gallagher-Thompson D. Positive aspects of caregiving: Contributions of the REACH project to the development of new measures for Alzheimer’s caregiving. Research on Aging. 2004;26:429–453. [Google Scholar]
- Walker AJ, Pratt CC, Eddy L. Informal caregiving to aging family members: A critical review. Family Relations. 1995;44:402–411. [Google Scholar]
- Wolff JL, Kasper JD. Caregivers of frail elders: Updating a national profile. The Gerontologist. 2006;46:344–356. doi: 10.1093/geront/46.3.344. [DOI] [PubMed] [Google Scholar]
- Yee JL, Schulz R. Gender differences in psychiatric morbidity among family caregivers: A review and analysis. The Gerontologist. 2000;40:147–164. doi: 10.1093/geront/40.2.147. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Kim K, Femia EE, Almeida DM, Savla J, Molenaar PCM. Effects of adult day care on daily stress of caregivers: A within-person approach. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. doi: 10.1093/geronb/gbr030. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]