Abstract
We conducted contact tracing and high-risk group screening using pooled real-time polymerase chain reaction (PCR) to support malaria elimination in Thailand. PCR detected more Plasmodium infections than the local and expert microscopists. High-throughput pooling technique reduced costs and allowed prompt reporting of results.
Thailand's National Malaria Control and Elimination Strategy aims to free 80% of the country from locally acquired malaria by the year 2020 (Bureau of Vector-Borne Diseases, Ministry of Public Health, Thailand, unpublished data). However, the elimination of local transmission requires rapid detection and treatment of all infections, including those infections in asymptomatic individuals who may serve as important reservoirs.1–3 Currently, malaria case detection for surveillance depends on microscopy or rapid diagnostic tests, but both methods miss low parasite densities on the order of 10 parasites/μL. Such submicroscopic infections are detectable by polymerase chain reaction (PCR) and are common in areas with low and unstable malaria.4–7 Efforts to control and eliminate malaria from Trat province on the border with Cambodia are intensifying because of the potential spread of artemisinin resistance. The detection of submicroscopic cases may facilitate containment efforts and help preserve artemisinin-based combination therapies for effective malaria treatment (Bureau of Vector-Borne Diseases, Ministry of Public Health, Thailand, unpublished data).
Real-time PCR is a highly sensitive tool for detecting and speciating Plasmodia. Pooling samples before analysis facilitates the large-scale application of this technique for surveillance by reducing cost and analysis time.7,8 As Thailand aims for malaria elimination, including elimination of artemisinin-resistant parasites, improvements in case detection are necessary. We aimed to determine if pooled real-time PCR could be integrated with the existing active case detection systems in Thailand and if so, if it would be more effective than microscopy for identifying low-density parasitemias.
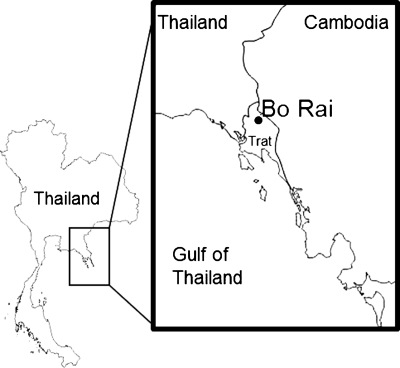
A single index case, with mixed P. falciparum–P. vivax infection, was identified during hospitalization for severe malaria in July of 2011 through passive case detection. This infection was likely acquired during frequent forest exposure. Two weeks after this identification, 187 residents in Bo Rai district, Trat province, Thailand (Figure 1) were contacted over 3 days according to the policies of the National Malaria Control Program of Thailand, which includes contact tracing (Case Investigation Survey) and high-risk group screening (Special Case Detection). For contact tracing, we screened neighbors within 1 km of the index case. For high-risk group screening, we screened soldiers from Khao Lan and Ban Sapanhin army camps and residents of Takang and Ban Samoh villages, which have a high proportion of Burmese Mon migrants.
Figure 1.
Map of Thailand and highlight of screening site in Bo Rai district in Trat province, Thailand, in June 21–22, 2011.
We administered a questionnaire to collect demographic information and risk factors for malaria, such as history of fever and malaria, bed net use, and recent travel to forest areas. Blood was collected and prepared as a thick smear, and 30 μL were applied to filter paper for dried blood spots. Blood smears were interpreted by both local malaria clinic staff and national expert microscopists at the Bureau of Vector-Borne Diseases in Nonthaburi according to the current World Health Organization (WHO) guidelines.
We extracted genomic DNA (gDNA) from dry blood spots into 150 μL using 20% Chelex-100 (Bio-Rad, Richmond, CA) as outlined in the work by Plowe and others.9 We conducted pooling (1:4) of samples and real-time PCR as previously reported7 after validating the protocol with specimens containing as few as 10 parasites/μL. Briefly, we amplified the 18S Plasmodium rRNA gene in pools of gDNA (2 μL per sample) with the pan-species assay. We individually tested constituent samples from positive pools and amplified positive samples with the speciation assay. We modified the speciation assay so that the two multiplex reactions amplified P. falciparum/P. vivax and P. malariae/human GapDH, respectively. All reactions were amplified in duplicate, and all reaction plates included two positive samples and one negative control. All real-time PCRs were run with the Bio-Rad CFX96 Real-Time PCR System, and amplification curves were evaluated with Bio-Rad CFX Manager. Data were entered into Microsoft Excel 2010 (Microsoft, Redmond, WA) and analyzed in SAS, version 9.2.2 (SAS, Cary, NC).
Of 187 individuals studied, 126 individuals were identified through contact tracing, and the remaining 61 individuals were identified through high-risk group screening (Table 1 ). The majority of the study population was between the ages of 15 and 49 years (84.7%) and male (64.2%). Two-thirds were Thai citizens (65.3%); the rest were Cambodian (8.7%) or Burmese Mon (26.0%). The majority of foreigners (74.0%) were migrants living in Thailand for 6 months or more, and over one-half of the individuals were rubber plantation workers (62.6%). Self-reported adherence to bed net use was high. Almost all (94.0%) reported always using a bed net, and 94.3% of those individuals visiting forest areas in the past month reported that they took a bed net or insecticide-treated hammock.
Table 1.
Characteristics of a population cross-section at risk for malaria from Bo Rai district in Trat province, Thailand, in June 21–22, 2011
| Subjects (N = 187*) | ||
|---|---|---|
| Number | Percent | |
| Age (years) | ||
| < 15 | 1 | 0.7 |
| 15–49 | 127 | 84.7 |
| 50+ | 22 | 14.7 |
| Missing | 37 | |
| Gender | ||
| Male | 95 | 64.2 |
| Female | 53 | 35.8 |
| Missing | 39 | |
| Ethnicity | ||
| Thai | 98 | 65.3 |
| Cambodian | 13 | 8.7 |
| Burmese Mon | 39 | 26.0 |
| Missing | 37 | |
| Residency status† | ||
| Thai | 98 | 66.2 |
| M1 migrant (≥ 6 months) | 37 | 25.0 |
| M2 migrant (< 6 months) | 13 | 8.8 |
| Missing | 39 | 8.8 |
| Occupation | ||
| Rubber plantation worker | 92 | 62.6 |
| Soldier | 38 | 25.9 |
| Other | 17 | 11.6 |
| Missing | 40 | |
| Self-reported fever in past 3 days | ||
| Yes | 6 | 4.1 |
| No | 141 | 95.9 |
| Missing | 40 | |
| Confirmed malaria case in past 3 months‡ | ||
| Yes | 5 | 3.4 |
| No | 144 | 96.6 |
| Missing | 38 | |
| Frequency of bed net use | ||
| Always | 140 | 94.0 |
| Not always or never | 9 | 6.0 |
| Missing | 38 | |
| Forest visit in past month§ | ||
| Yes | 30 | 20.4 |
| No | 117 | 79.6 |
| Missing | 40 | |
Questionnaire data were available for all 61 individuals from the high-risk group screening and only 89 of 126 (70.6%) individuals from contact tracing.
†Thai indicates citizen of Thailand, M1 indicates migrant living in Thailand for greater than 6 months, and M2 indicates migrant living in Thailand for less than or equal to 6 months.
‡Self-reported malaria case in the 3 months preceding blood collection that was confirmed and treated at a malaria clinic or hospital.
§Self-reported visit or stay overnight in forest areas in the past month.
No infections were detected in 187 slides by the microscopist at the local malaria clinic, and only one infection of P. falciparum (0.5%) was detected by an expert microscopist at the central laboratory. Conversely, pooled real-time PCR detected four infections from the same 187 samples (2.1%), including the microscopy-positive P. falciparum case and three P. vivax infections. Subsequent reexamination of PCR-positive slides by the expert microscopist confirmed that two of tree P. vivax cases not initially detected by microscopy were positive when more microscopic fields were examined. Two P. vivax infections were identified through high-risk group sampling (2 of 61 samples positive; 3.3%), whereas the remaining two cases were identified by contact tracing (2 of 126 samples positive; 1.6%). Thus, none of four PCR-positive samples were identified by a local microscopist, and retrospective examination by an expert microscopist confirmed parasites in three of four samples. With real-time PCR as the referent, expert microscopy showed 25% sensitivity and 100% specificity (Table 2 ).
Table 2.
Comparison of expert microscopy and real-time PCR results for malaria surveillance in 187 individuals from Bo Rai district in Trat province, Thailand in June 21–22, 2011
| Method | Positive | Negative | Sensitivity |
|---|---|---|---|
| Local microscopist (blinded) | 0 | 187 | 0 |
| Expert microscopist (blinded) | 1 | 186 | 25% |
| Expert microscopist (unblinded) | 3 | 183 | 75% |
| Real-time PCR | 4 | 182 | 100% |
Sensitivity was calculated with real-time PCR as the gold standard.
The P. falciparum infection identified through contact tracing was in a 27-year-old Thai male fruit plantation worker who reported having had a confirmed case of malaria in the past 3 months. He had a parasite density of 240 parasites/μL detected by the blinded expert microscopist. The patient returned to the malaria clinic with symptoms before microscopy and PCR results were reported.
Two of three P. vivax cases were identified through high-risk group screening and were Burmese Mon male rubber plantation workers. The first case was a 27-year-old living in Thailand for less than 6 months; the second case was a 40-year-old living in Thailand for more than 6 months. These infections were only detected by microscopy after PCR results were known, with parasite densities of 32 and 48 parasites/μL, respectively. All three cases reported always using a bed net. No demographic or risk factor information was available for the third P. vivax case identified through contact tracing.
Active case detection using pooled, real-time PCR detected more infections (4) than either the local (0) or expert microscopist (1). Confirmation of positive samples after reexamination by microscopy suggests that PCR did not produce false positives. Modification of routine program activities to collect dry blood spots in addition to blood smears was uncomplicated logistically and required little additional training for malaria clinic staff.
The total cost of screening 187 individuals was 29,220 Baht ($974 US), which included labor and materials. Screening with 1:4 pooling reduced the number of PCR reactions required from 191 to 67 (65%) without reducing the detection limit of the assay. Based on a cost of 37.50 Baht ($1.25 US) per sample,7 the improved efficiency of pooling translates to cost savings of 4,650 Baht ($155 US) in this study.
Sample preparation and analysis of 187 samples, including DNA extraction and PCR analysis, was completed rapidly (in 4 days) at the central laboratory. Results were reported to local malaria clinics 1 week after sample collection and allowed for prompt treatment and follow-up. The delay between sample collection and results because of transportation of samples could be remediated by installing PCR equipment at provincial malaria offices.
In summary, pooled real-time PCR can identify submicroscopic malaria cases that, as potential sources of transmission, must be treated for the success of elimination. Real-time PCR may present a consistent, accurate, and efficient tool for surveillance to assist malaria elimination in Thailand.
ACKNOWLEDGMENTS
The authors thank Vijarn Yisarakun and the malaria clinic staff from the Vector-Borne Disease Center in Trat for their fieldwork support and the villagers for their cooperation. We also acknowledge expert microscopist Pannee Srisawad and the other laboratory technicians at the Bureau of Vector-Borne Diseases. The authors thank Jon Juliano and Steve Taylor for protocols and training in the PCR assays and Naman Shah for his comments and suggestions.
Disclaimer: The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the American Society of Tropical Medicine and Hygiene or the institutions with which the authors are affiliated.
Footnotes
Financial support: This work was funded by the Bill & Melinda Gates Foundation and the Bureau of Vector-Borne Diseases, Department of Disease Control, Ministry of Public Health, Thailand. E.T.R. was supported by a University of North Carolina Entrepreneurial Public Service Fellowship from the Carolina Center for Public Service at the University of North Carolina at Chapel Hill.
Authors' addresses: Elizabeth T. Rogawski and Steven R. Meshnick, Department of Epidemiology, University of North Carolina, Chapel Hill, NC, E-mails: rogawski@unc.edu and meshnick@email.unc.edu. Kanungnit Congpuong, Prayuth Sudathip, Wichai Satimai, Rungniran Sug-aram, Supannee Aruncharus, Ampai Darakapong, and Suravadee Kitchakarn, Bureau of Vector-Borne Disease, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, E-mails:nungnit@health.moph.go.th, psudathip@gmail.com, wichaisatimai@yahoo.com, run_rungniran@hotmail.com, imp_qmi@hotmail.com, cutetor36@yahoo.com, and kitchakarn@hotmail.com.
References
- 1.The malERA Consultative Group on Diagnoses and Diagnostics A research agenda for malaria eradication: diagnoses and diagnostics. PloS Med. 2011;8:e1000396. doi: 10.1371/journal.pmed.1000396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moonen B, Cohen JM, Snow RW, Slutsker L, Drakeley C, Smith DL, Abeyasinghe RR, Rodrigues MH, Maharaj R, Tanner M, Targett G. Operational strategies to achieve and maintain malaria elimination. Lancet. 2010;376:1592–1603. doi: 10.1016/S0140-6736(10)61269-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perkins M, Bell D. Working without a blindfold: the critical role of diagnostics in malaria control. Malar J. 2008;7:S5. doi: 10.1186/1475-2875-7-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ouédraogo AL, Bousema T, Schneider P, de Vlas SJ, Ilboudo-Sanogo E, Cuzin-Ouattara N, Nébié I, Roeffen W, Berhave JP, Luty AFJ, Sauerwein R. Substantial contribution of submicroscopical Plasmodium falciparum gametocyte carriage to the infectious reservoir in an area of seasonal transmission. PLoS One. 2009;4:e8410. doi: 10.1371/journal.pone.0008410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steenkeste N, Rogers W, Okell L, Jeanne I, Incardona S, Duval L, Chy S, Hewitt S, Chou M, Socheat D, Babin F-X, Ariey F, Rogier C. Sub-microscopic malaria cases and mixed malaria infection in a remote area of high malaria endemicity in Rattanakiri province, Cambodia: implication for malaria elimination. Malar J. 2010;9:108. doi: 10.1186/1475-2875-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris I, Sharrock W, Bain L, Gray K-A, Bobogare A, Boaz L, Lilley K, Krause D, Vallely A, Johnson M-L, Gatton M, Shanks G, Cheng Q. A large proportion of asymptomatic Plasmodium infections with low and sub-microscopic parasite densities in the low transmission setting of Temotu Province, Solomon Islands: challenges for malaria diagnostics in an elimination setting. Malar J. 2010;9:254. doi: 10.1186/1475-2875-9-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor SM, Juliano JJ, Trottman PA, Griffin JB, Landis SH, Kitsa P, Tshefu AK, Meshnick SR. High-throughput pooling and real-time PCR-based strategy for malaria detection. J Clin Microbiol. 2010;48:512–519. doi: 10.1128/JCM.01800-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsiang MS, Lin M, Dokomajilar C, Kemere J, Pilcher CD, Dorsey G, Greenhouse B. PCR-based pooling of dried blood spots for detection of malaria parasites: optimization and application to a cohort of Ugandan children. J Clin Microbiol. 2010;48:3539–3543. doi: 10.1128/JCM.00522-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Plowe CV, Djimde A, Bouare M, Doumbo O, Wellems TE. Pyrimethamine and proguanil resistance-conferring mutations in Plasmodium falciparum dihydrofolate reductase: polymerase chain reaction methods for surveillance in Africa. Am J Trop Med Hyg. 1995;52:565–568. doi: 10.4269/ajtmh.1995.52.565. [DOI] [PubMed] [Google Scholar]