Abstract
Background
The inflammatory response is prominent in the pathogenesis of dermal leishmaniasis. We hypothesized that regulatory T cells (Tregs) may be diminished in chronic dermal leishmaniasis (CDL) and contribute to healing during treatment.
Methodology/Principal Findings
The frequency and functional capacity of Tregs were evaluated at diagnosis and following treatment of CDL patients having lesions of ≥6 months duration and asymptomatically infected residents of endemic foci. The frequency of CD4+CD25hi cells expressing Foxp3 or GITR or lacking expression of CD127 in peripheral blood was determined by flow cytometry. The capacity of CD4+CD25+ cells to inhibit Leishmania-specific responses was determined by co-culture with effector CD4+CD25− cells. The expression of FOXP3, IFNG, IL10 and IDO was determined in lesion and leishmanin skin test site biopsies by qRT-PCR. Although CDL patients presented higher frequency of CD4+CD25hiFoxp3+ cells in peripheral blood and higher expression of FOXP3 at leishmanin skin test sites, their CD4+CD25+ cells were significantly less capable of suppressing antigen specific-IFN-γ secretion by effector cells compared with asymptomatically infected individuals. At the end of treatment, both the frequency of CD4+CD25hiCD127− cells and their capacity to inhibit proliferation and IFN-γ secretion increased and coincided with healing of cutaneous lesions. IDO was downregulated during healing of lesions and its expression was positively correlated with IFNG but not FOXP3.
Conclusions/Significance
The disparity between CD25hiFoxp3+ CD4 T cell frequency in peripheral blood, Foxp3 expression at the site of cutaneous responses to leishmanin, and suppressive capacity provides evidence of impaired Treg function in the pathogenesis of CDL. Moreover, the concurrence of increased Leishmania-specific suppressive capacity with induction of a CD25hiCD127− subset of CD4 T cells during healing supports the participation of Tregs in the resolution of chronic dermal lesions. Treg subsets may therefore be relevant in designing immunotherapeutic strategies for recalcitrant dermal leishmaniasis caused by Leishmania (Viannia) species.
Author Summary
The immune inflammatory response is a double edged sword. During infectious diseases, regulatory T cells can prevent eradication of the pathogen but can also limit inflammation and tissue damage. We investigated the role of regulatory T cells in chronic dermal leishmaniasis caused by species of the parasite Leishmania that are endemic in South and Central America. We found that although individuals with chronic lesions have increased regulatory T cells in their blood and at skin sites where immune responses to Leishmania were taking place compared to infected individuals who do not develop disease, their capacity to control the inflammatory response to Leishmania was inferior. However, healing of chronic lesions at the end of treatment was accompanied by an increase in the number and capacity of regulatory T cells to inhibit the function of effector T cells that mediate the inflammatory response. Different subsets of regulatory T cells, defined by the expression of molecular markers, were identified during chronic disease and healing, supporting the participation of distinct regulatory T cells in the development of disease and the control of inflammation during the healing response. Immunotherapeutic strategies may allow these regulatory T cell subsets to be mobilized or mitigated to achieve healing.
Introduction
Dermal leishmaniasis (DL) caused by species from the Viannia subgenus is characterized by a paucity of parasites in lesions associated with a robust inflammatory response and frequently follows a chronic course [1]. Both cutaneous and muco-cutaneous presentations of chronic dermal leishmaniasis (CDL) caused by Leishmania (Viannia) are associated with elevated cellular immune responses [2], [3]. Human studies and a recent murine model of chronic dermal disease have shown that a mixed Th1/Th2 cytokine pattern occurs in CDL caused by L. (Viannia), with prominent secretion of IFN-γ, IL-13, IL-10 and TNF-α [4]–[6]. Even though regulatory mechanisms are likely to have a significant role in the development of such an immune response, little is known about their impact in determining susceptibility and shaping disease outcome.
Regulatory T cells (Tregs) maintain tolerance to self tissues by inhibiting the action of auto-antigen reactive lymphocytes in an antigen-specific manner. In infectious diseases, Tregs also regulate the intensity and duration of immune responses, limiting damage to self tissues [7]–[8]. In the murine model of DL caused by L. major, Tregs have been shown to promote parasite persistence and reactivation in the resistant strain C57Bl/6 while inhibiting pathology in the susceptible Balb/c strain [9]–[12]. Tregs also suppressed pathology in mouse strains susceptible to disease caused by L. amazonensis [13]. These observations indicate that regulation of Leishmania-specific responses by Tregs may differentially alter the outcome of infection according to the susceptibility phenotype dictated by the host response. In resistant individuals, excessive Treg action may interfere with elimination of infection, whereas in susceptible individuals deficient Treg function may lead to excessive inflammation and dermal pathology.
Studies in humans infected with species from the Viannia subgenus have demonstrated that T cells with regulatory phenotype and function are present in cutaneous lesions [14]–[17]. An association between increased Foxp3 expression and unresponsiveness to treatment and chronic disease has been reported in human DL caused by L. guyanensis infection [16]–[17]. In contrast, no differences were found in the frequency of Tregs in peripheral blood between asymptomatically infected individuals (AI) and patients with CDL in L. braziliensis infection [14]. Hence, the role of Tregs in the pathogenesis of DL and their participation in the therapeutic response remain unclear.
The purpose of this study was to evaluate the role of Tregs in CDL caused by species of the Viannia subgenus and in the resolution of chronic lesions following treatment with pentavalent antimony. We found that lack of regulation of IFN-γ secretion by Tregs was associated with development of chronic disease, while an increase of Treg function after treatment was associated with lesion healing.
Methods
Experimental Strategy and Rationale
In this study, asymptomatic infection was considered to approximate clinical resistance to natural infection, and chronic disease to define a clinically susceptible phenotype, analogous to the healing and non-healing phenotypes in murine models of cutaneous leishmaniasis. Because AI and DL patients evidently remain infected indefinitely [18]–[23], exposure to Leishmania antigens would persist in both clinical outcomes. Since DL is generally a self-resolving disease, discrimination of spontaneous healing and chronic disease is not reliably determined during early or intermediate stages of evolution. However, longer times of evolution (chronic disease) have been shown to be associated with increased immune reactivity to Leishmania antigens including significantly higher antibody titers and DTH responses [2]. Furthermore, Th1/Th2 transcription factor expression and inflammatory cytokine responses distinguished asymptomatic clinical outcome and chronic cutaneous disease [5]. The rationale for analyzing the Treg response in asymptomatic infection and chronic disease was, therefore, that these phenotypically distinguishable outcomes are natural expressions of clinical resistance and susceptibility to human dermal leishmaniasis.
Ethics Statement
All participants provided written informed consent. The study protocol, consent forms and all procedures were approved by the CIDEIM Institutional Review Board for the ethical conduct of research involving human subjects.
Human Subjects
Participants were residents of endemic areas for L. panamensis and L. braziliensis located within the southwestern Pacific coast region of Colombia (Departments of Valle del Cauca and Nariño) [24]. We included cases caused by both of these species of the Viannia subgenus because there is significant overlap of clinical presentations and broad measures of immune responses (DTH, lymphocyte proliferation and antibody titer) in patients with dermal disease caused by these species [2], [25]. AI had a positive LST and no evidence or history of dermal lesions. CDL patients had dermal lesions of ≥6 months duration, parasitological diagnosis by microscopic examination of tissue samples from lesions, culture or biopsy, and had not received anti-leishmanial treatment before enrollment. All subjects had negative serology for HIV and HTLV-1. A LST was performed in all participants and evaluated at 48 hours as previously described [26]. Leishmanin (Instituto Nacional de Salud, Colombia) was composed of equal amounts of L. panamensis and L. amazonensis promastigote proteins at a concentration of 5 µg/mL. Peripheral blood samples (100 mL), and skin biopsies from a leishmaniasis lesion and LST reaction site were obtained upon entry into the study. The species of parasite strains isolated from patients with a positive culture were determined as previously described [27]. CDL patients were treated with meglumine antimoniate at a dose of 20 mg Sb/kg/day. After treatment, a second 100 mL blood sample and a biopsy from the same lesion site were obtained and clinical responses were evaluated. Complete healing was defined as total re-epithelialization and absence of any evidence of inflammation for all lesions. Partial healing was estimated as the percentage of reduction of ulcer/plaque area or nodule volume. Skin biopsies from four healthy volunteers were obtained for normalization of gene expression data. Biopsies were obtained using a 4 mm disposable punch, embedded in OCT, frozen and stored in liquid nitrogen until processed.
Cell Isolation
PBMCs were isolated by centrifugation over Histopaque-1077 (Sigma-Aldrich, St. Louis, MO). CD4+CD25− and CD4+CD25+ cells were isolated by MACS using the CD4+CD25+ Regulatory T cell isolation kit (Miltenyi Biotec, Bergisch-Gladbach, Germany) following the manufacturer's instructions. Purity assessed by staining with anti-CD4 and anti-CD25 was ≥90% for both populations. Monocytes were isolated by allowing PBMCs to adhere to plastic for 2 hours followed by three washes with PBS. Purity assessed by staining with anti-CD14 was ≥65% and contaminating CD4hi lymphocytes were <5%.
Evaluation of Cell Marker Expression
PBMCs from 12 AI, 14 CDL patients before treatment, and 11 CDL patients after treatment were suspended in FACS buffer (1× PBS, 1% BSA, 0.1% NaN3) and incubated for 30 minutes with anti-CD4-APC (BD Biosciences, San Jose, CA), anti-CD25-PE (Miltenyi Biotec) and anti-CD127-FITC (eBioscience, San Diego, CA) or anti-CD4-FITC (BD Biosciences), anti-glucocorticoid-induced TNF receptor family-related protein (GITR)-PE and anti-CD25-APC (eBioscience). For evaluation of forkhead box p3 (Foxp3), cells were stained with anti-CD4-FITC and anti-CD25-APC, fixed and permeabilized using the Fixation and Permeabilization kit (eBiosciences), and incubated with anti-Foxp3-PE or anti-Rat IgG2a-PE (eBioscience). After washing, cells were analyzed in a Navios flow cytometer (Beckman Coulter, Brea, CA) and data was analyzed using FlowJo 7.6 software (Tree Star, Inc., Ashland, OR). Gates used for analysis were set using isotype controls.
Co-Culture of CD4+CD25− and CD4+CD25+ Cells
Killed promastigotes of the L. panamensis strain MHOM/COL/81/L13 were prepared by the freeze/thaw method, as previously described [28]. CD4+CD25− cells from 12 AI, 14 CDL patients before treatment, and 11 CDL patients after treatment were incubated with 5 µM carboxyfluorescein diacetate succinimidyl diester (CFSE, Invitrogen, Carlsbad, CA) for 10 minutes at 4°C, washed three times with PBS and resuspended in RMPI 1640 (Sigma-Aldrich) with 10% FBS (Gibco, Carlsbad, CA), 2 mM L-glutamine, penicillin (100 U/mL) and streptomycin (100 mg/mL). 1×106 CD4+CD25− cells per well were distributed in 24 well plates with 2×105 L. panamensis promastigotes, 5×105 monocytes from the same subject (used as antigen presenting cells, APCs), or phytohaemagglutinin (PHA, Sigma-Aldrich) 10 µg/mL, and CD4+CD25+ cells at 1∶0, 4∶1 or 1∶1 CD4+CD25−: CD4+CD25+ cell ratios, in a final volume of 1 mL. After 5 days of incubation at 37°C with 5% CO2, cells and supernatants were harvested for evaluation of proliferation and cytokine secretion, respectively. Cells were stained with anti-CD4-APC and analyzed by flow cytometry. CFSE fluorescence in CD4+CD25− cells was evaluated in the CD4+ gate. Unlabeled CD4+CD25+ cells and CD4+ lymphocytes contaminating the APC preparation were gated out of the analysis (Figure S1A). Regions were drawn for each proliferation peak induced by PHA (Figure S1B) and the proliferation index (PI) was calculated with the formula PI = Σ(% in region×2n−1), where n is the region number [29]. Interferon-γ (IFN-γ) and interleukin-10 (IL-10) were measured in supernatants by ELISA as previously described [28]. Co-cultures were considered to have positive proliferation or IFN-γ secretion when the value in wells with CD4+CD25− cells, APCs and L. panamensis or PHA was higher than the mean+2SD of the control wells without APCs, L. panamensis or neither. The percent inhibition of proliferation or IFN-γ secretion by CD4+CD25+ cells was calculated in positive co-cultures using the formula: (value without CD4+CD25+ cells - value with CD4+CD25+ cells)/(value without CD4+CD25+ cells) ×100. Negative results were considered 0% inhibition.
Real-Time PCR Analysis
RNA was isolated from LST biopsies from 5 AI and 7 CDL patients and lesion biopsies from 11 CDL patients both before and after treatment using the RNeasy mini kit (QIAGEN, Valencia, CA) according to the manufacturer's instructions. For cDNA synthesis, 100 ng total RNA was transcribed with the High-capacity cDNA reverse transcription kit (Applied Biosystems, Foster City, CA), following the manufacturer's instructions. Gene expression was measured in real-time with the CFX966 Real Time System (Bio-Rad, Hercules, CA) using Taqman Universal PCR master mix and Taqman gene expression assays for GAPDH (Hs99999905m-1), FOXP3 (Hs01085835-m1), IFNG (Hs00174143-m1), IL10 (Hs00174086-m1) and IDO (Hs00158027-m1) genes (Applied Biosystems), following the manufacturer's instructions. The expression levels of FOXP3, IFNG, IL10 and IDO relative to healthy skin were calculated using the ΔΔCT method, as previously described [30], using GAPDH as endogenous reference gene and four healthy skin biopsies as calibrators.
Statistical Analysis
The Kolmogorov-Smirnov test was used to determine parametric or non-parametric distribution of the data. Thereafter, for comparisons between AI and CDL patients, parametric data were analyzed using student t-test, and the Mann-Whitney test was applied for non-parametric data. For comparisons between CDL patients before and after treatment, parametric and non-parametric data were analyzed using the paired t-test and the Wilcoxon signed-rank test, respectively. Correlation analyses were conducted using the Spearman coefficient. Statistical significance was defined as p<0.05. All data were analyzed using Prism 5 software (GraphPad Software, Inc., La Jolla, CA).
Results
Clinical Characteristics of the Study Subjects
Twelve AI and 14 CDL patients participated in this study. There were no significant differences in age, gender or size of LST reaction between AI and CDL patients (data not shown). The clinical characteristics of CDL patients are summarized in Table 1. Three patients were lost to follow-up. The other eleven patients were evaluated at a second visit within 24 days of completing treatment. Five patients showed complete healing, and lesions in six patients had substantially improved though not completely healed (Table 1).
Table 1. Clinical characteristics and evolution of chronic dermal leishmaniasis patients.
| Subject code | Isolated parasite | Lesion duration (months) | Lesion number | Lesion Type | Time of second sample (Days after treatment) | % Cureda |
| 111 | ND | 8 | 1 | Nodule | 2 | 50 |
| 112 | L. braziliensis | 6 | 2 | Ulcers | 1 | 100 |
| 113 | L. panamensis | 7 | 1 | Ulcer | Lost to followup | NA |
| 114 | L. panamensis | 6 | 3 | Ulcers | Lost to followup | NA |
| 116 | L. panamensis | 6 | 5 | Ulcers/plaque/mucosal | 1 | 80 |
| 117 | L. panamensis | 18 | 8 | Plaques/papules/mucosal | 24 | 100 |
| 118 | L. panamensis | 6 | 1 | Ulcer | Lost to followup | NA |
| 121 | L. panamensis | 20 | 3 | Plaques/Nodule | 1 | 90 |
| 209 | ND | 6 | 1 | Ulcer | 5 | 100 |
| 214 | ND | 24 | 1 | Ulcer | 2 | 60 |
| 216 | L. braziliensis | 240 | 1 | Ulcer | 2 | 80 |
| 217 | L. panamensis | 36 | 1 | Plaque | 2 | 100 |
| 218 | ND | 48 | 1 | Ulcer | 2 | 80 |
| 223 | ND | 6 | 3 | Plaques | 23 | 100 |
% of surface area of ulcer(s) or plaque(s) healed or volume of nodule(s) reduced at the end of treatment; ND: not determined because culture was not necessary or no strain was obtained; NA: not applicable.
CDL Patients Presented a Higher Frequency of CD4+CD25hiFoxp3+ Cells in Peripheral Blood than AI
High expression of CD25 has been described as a reliable marker for Tregs [31]–[34]. Lack of expression of CD127, expression of GITR, or expression of Foxp3 have also been described as Treg markers [34]–. Therefore, to evaluate the frequency of Tregs in the peripheral blood of AI and CDL patients, we measured the frequency of CD25hi CD4 T cells that expressed each of these markers. We found that CD4+CD25hiFoxp3+ cells were more abundant in the peripheral blood of CDL patients (0.9±0.4% in CDL patients vs. 0.4±0.2 in AI, p = 0.0003; Figure 1A), while significant differences were not observed in the frequency of CD4+CD25hiCD127− and CD4+CD25hiGITR+ cells between the two groups (Figures 1B and C).
Figure 1. CDL patients have a higher frequency of CD4+CD25hiFoxP3+ cells in peripheral blood than AI.
PBMCs from AI (n = 12) and CDL patients (n = 14) were stained for CD4, CD25 and either Foxp3, CD127, or GITR and analyzed by flow cytometry. A. Frequency of CD4+CD25hiFoxp3+ cells. B. Frequency of CD4+CD25hiCD127− cells. C. Frequency of CD4+CD25hiGITR+ cells. ***p<0.001, Mann-Whitney test. The median is represented by a horizontal line.
CD4+CD25+ Cells from AI Demonstrated a Higher Capacity to Suppress CD4 Effector T Cell IFN-γ Secretion than Those from CDL Patients
We evaluated the functional capacity of Tregs to suppress Leishmania-specific proliferation and IFN-γ secretion using co-cultures of CD4+CD25− cells (effectors) and CD4+CD25+ cells (Tregs) from peripheral blood. In the absence of Tregs, proliferation and IFN-γ secretion were induced by L. panamensis antigens in effector T cells from all CDL patients and 9 of 12 AI. Proliferation was significantly higher for CDL patients in relation to AI (p = 0.037, Figure 2A), while no statistically significant differences were detected for IFN-γ secretion (Figure 2B). No significant effector functions were observed in the absence of either APCs or L. panamensis antigens (Figures 2A and B), indicating that they were the result of antigen-specific APC-T cell interactions. L. panamensis induced similar levels of proliferation and IFN-γ secretion in patients infected with L. panamensis or L. braziliensis and in patients in which infecting species was undetermined (data not shown), confirming recall of T cell responses across species. High levels of proliferation were induced by PHA in all subjects (Figure 2A), while IFN-γ secretion was low with this stimulus under the conditions of assay (Figure 2B), being positive only for 6 AI and 3 CDL patients.
Figure 2. CD4+CD25+ cells from AI have a higher capacity to suppress IFN-γ secretion by effector cells.
CD4+CD25− (effector) cells from AI (n = 12) and CDL patients (n = 14) were cultured for 5 days with antigen presenting cells (APCs), L. panamensis (L.p.), or both, or with PHA, as indicated. A. Proliferation of CD4+CD25− cells. B. IFN-γ levels secreted by CD4+CD25− cells. Positive proliferation and IFN-γ secretion were defined as levels above the mean+2SD of control wells from the same donor. For subjects whose effector cells showed positive proliferation and IFN-γ secretion (n = 9 for AI and n = 14 for CDL patients, L.p.+APCs stimulation; n = 12 for AI and n = 14 for CDL patients, PHA stimulation), cultures were conducted in the presence or absence of CD4+CD25+ (regulatory) cells. C. Inhibition of CD4+CD25− cell proliferation induced by L.p.+APCs or PHA by CD4+CD25+ cells. D. Inhibition of CD4+CD25− cell IFN-γ secretion induced by L.p.+APCs by CD4+CD25+ cells. 1∶1 effector∶Treg ratio could not be tested in 3 AI because insufficient numbers of CD4+CD25+ cells were obtained (n = 6 for AI and n = 14 for CDL patients); *p<0.05, Mann-Whitney test. A and B show means with SEM. C and D show the mean as a horizontal line.
Suppression assays with L. panamensis stimulation were performed at effector∶Treg ratios of 4∶1 and 1∶1 in subjects that had positive effector functions, except for three AI from whom the number of CD4+CD25+ cells isolated was insufficient to evaluate the 1∶1 ratio. At a 4∶1 effector∶Treg ratio, no statistically significant differences in antigen-specific suppression were detected between AI and CDL patients (Figures 2C and D). At a 1∶1 effector∶Treg ratio, suppression of IFN-γ secretion was significantly higher in AI compared to CDL patients (80±6.1% vs. 48±9.2%, p = 0.044; Figure 2D) whereas suppression of proliferation was not significantly different between the two groups (Figure 2C). To evaluate suppression after a polyclonal stimulus, inhibition of proliferation by Tregs at a 4∶1 ratio was evaluated after PHA stimulation. No significant differences in suppression of proliferation induced by PHA were detected between AI and CDL patients (mean inhibition 19.5±4.1% and 25.9±5.8%, respectively; p = 0.313; Figure 2C).
FOXP3 Expression Is Higher in LST Sites of CDL Patients than AI
We next examined the influence of Tregs in situ by measuring the transcription of genes related to immune regulation and inflammation at the site of injection of leishmanin antigen from 5 AI and 7 CDL patients. We evaluated the relative expression of four genes: FOXP3, IFNG, IL10, and 2,3 indoleamine deoxygenase (IDO), an enzyme expressed by APCs that is involved in immune regulation through the catabolism of the essential aminoacid tryptophan [38], [39]. We found that the relative expression of FOXP3 was significantly higher in CDL patients in relation to AI (relative expression 12.7±4.3 vs. 0.7±0.8, p = 0.046, Figure 3A). No statistically significant differences were found for the other genes, although several individuals with chronic disease showed upregulation of IFNG and IDO (Figures 3B–D).
Figure 3. Relative expression of FOXP3 is higher in leishmanin skin test (LST) sites from CDL patients.
RNA was isolated from biopsies of LST sites from AI (n = 5) and CDL patients (n = 7) and the expression of FOXP3 (A), IFNG (B), IL10 (C) and IDO (D) was measured by qRT-PCR. The expression of each gene relative to healthy skin of four normal controls was calculated using the ΔΔCT method. *p<0.05, unpaired t-test. The median is represented by a horizontal line.
CD4+CD25hiCD127− Cells and Suppression by CD4+CD25+ Cells Increased after Treatment of CDL
At the end of treatment of CDL, the proportion of CD4+CD25hiCD127− cells increased significantly, from 1.5±0.2% to 2.3±0.3% (p = 0.0009, Figure 4B), whereas the frequency of CD4+CD25hiFoxp3+ and CD4+CD25hiGITR+ cells did not change significantly (Figure 4A and C). Proliferation and IFN-γ secretion in the absence of Tregs did not change significantly at the end of treatment, although significant proliferation was no longer observed in one patient (data not shown). In the presence of Tregs at a 1∶1 effector∶Treg ratio, 8 of 10 CDL patients demonstrated increased inhibition of proliferation by CD4+CD25+ cells at the end of treatment and 9 of 11 showed an increase in inhibition of IFN-γ secretion (Figures 4D and F). Inhibition of both parameters increased significantly for the group as a whole, with the mean percent inhibition of proliferation increasing from 21.9% to 46.5% (p = 0.025, Figure 4D) and the mean inhibition of IFN-γ secretion rising from 47.2% to 81.3% (p = 0.007, Figure 4F). Suppression of proliferation induced by PHA did not change significantly after treatment (p = 0.99; Figure 4E).
Figure 4. Treg frequency and function increase after treatment of CDL.
Frequency of cells with a Treg phenotype in PBMCs and suppressive capacity of CD4+CD25+ cells were determined for CDL patients (n = 11) before and after treatment. A. Frequency of CD4+CD25hiFoxp3+ cells. B. Frequency of CD4+CD25hiCD127− cells. C. Frequency of CD4+CD25hiGITR+ cells. D. Inhibition of CD4+CD25− cell proliferation by CD4+CD25+ cells at a 1∶1 ratio after stimulation with L. panamensis (L.p.) and APCs. E. Inhibition of CD4+CD25− cell proliferation by CD4+CD25+ cells at a 4∶1 ratio after stimulation with PHA. F. Inhibition of CD4+CD25− cell IFN-γ secretion by CD4+CD25+ cells at a 1∶1 ratio after stimulation with L.p. and APCs. Inhibition was calculated only for subjects that had proliferation and IFN-γ levels above the average+2SD of control wells from the same co-culture (n = 10 for proliferation and 11 for IFN-γ secretion with L.p. stimulation and n = 11 for PHA stimulation). *p<0.05, paired t-test, **p<0.01, Wilcoxon signed-rank test.
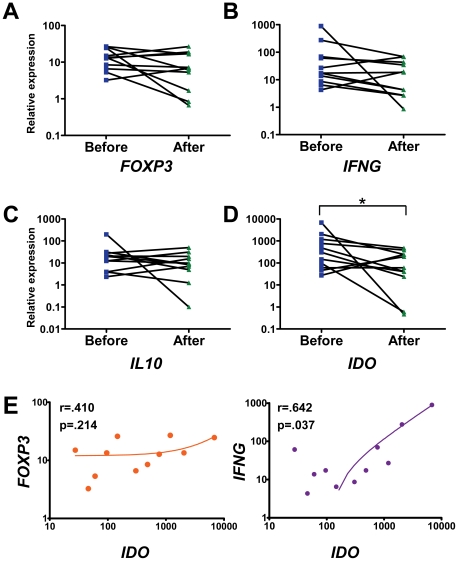
Expression of IDO in CDL Lesions Decreased after Treatment and Was Correlated with IFNG Expression
The relative expression of FOXP3 and IL10 did not change significantly after treatment of CDL (Figures 5A and C). The relative expression of IFNG decreased in 8 out of 11 patients at the end of treatment, with the mean value declining from 127.0±80.3 to 24.3±7.9. However, this difference was not statistically significant (p = 0.148, Figure 5B). Finally, although the expression of IDO in chronic lesions at the start of the study varied widely between individuals, at the end of treatment the expression of this gene was significantly downregulated from 1087±601 to 154±50 (p = 0.037, Figure 5D). Because IDO expression in APCs is upregulated by both inflammatory signals (particularly IFN-γ) [40], [41] and Tregs (through CTLA4-B7 interactions) [42], we examined whether IDO expression was correlated with that of IFNG or FOXP3 in CDL lesions. Our analysis revealed a significant positive correlation between IFNG and IDO expression. In contrast, FOXP3 expression was not significantly correlated with IDO expression (Figure 5E). Thus, IDO expression in the skin of CDL patients was most likely upregulated by IFN-γ.
Figure 5. Relative expression of IDO decreases in CDL patients after treatment and is correlated with IFNG.
RNA was isolated from biopsies of lesions from CDL patients (n = 11) before and after treatment and the expression of FOXP3 (A), IFNG (B), IL10 (C) and IDO (D) was measured by qRT-PCR. The expression of each gene relative to healthy skin of four normal controls was calculated using the ΔΔCT method. E. Correlation between the relative expression of IDO and FOXP3 (left panel) or IFNG (right panel). *p<0.05, Wilcoxon signed-rank test.
Suppression in Co-Cultures of Effector CD4 T Cells and Tregs Was Not Mediated by IL-10
To determine whether suppression of effector functions was attributable to IL-10 secretion by CD4+CD25+ cells, we evaluated IL-10 in the supernatants of the effector-Treg co-cultures. The presence of CD4+CD25+ cells in the co-cultures did not result in higher IL-10 concentrations in any of the study groups (Figure 6). To the contrary, analysis of co-cultures at the 1∶1 ratio (n = 31) for all groups revealed significantly lower IL-10 secretion in the presence of CD4+CD25+ cells (Figure 6). Therefore, inhibition of effector CD4 T cell functions in this in vitro system was not attributable to IL-10 secretion by Tregs. Rather, these results indicate that IL-10 secretion by CD4+CD25− effector T cells and/or APCs was also inhibited by Tregs.
Figure 6. IL-10 does not mediate suppression of effector functions by CD4+CD25+ cells.
IL-10 was measured in supernatants from the CD4+CD25−-CD4+CD25+ co-cultures by ELISA. The level of IL-10 in the absence (1∶0 ratio) or presence (1∶1 ratio) of CD4+CD25+ cells is shown for AI (n = 6), CDL patients before treatment (n = 14), CDL patients after treatment (n = 11) and all co-cultures combined (n = 31). **p<0.01, Wilcoxon signed-rank test. Means with SEM are shown.
Discussion
The regulation of adaptive immune responses is indispensable for the effective clearance of antigen without harm to self tissues. Although the importance of Tregs in this process is well established, evaluation in human disease is challenging because of the increasing recognition of the complexity of their phenotype and function. To clarify the role of Tregs in the pathogenesis and healing of DL caused by species of the Viannia subgenus, we studied a cohort of subjects from an area in Colombia endemic for L. panamensis and L. braziliensis. Comparisons of the frequency and suppressive function of cells expressing Treg markers in peripheral blood and the expression of genes related to inflammation and regulation in the skin of AI and CDL patients, and CDL patients before and after treatment, yielded evidence that Tregs participate in clinical resistance/susceptibility and lesion healing.
Patients with chronic dermal disease had a significantly higher frequency of CD25hiFoxP3+ CD4 T cells in their peripheral blood than infected individuals who did not develop disease. Additionally, FOXP3 expression was upregulated at skin sites of challenge with leishmanin antigen only in CDL patients. These results are consistent with several examples of chronic disease in which Foxp3 is upregulated in T cells [43]–[46] and previous reports of infiltration of dermal lesions caused by L. guyanensis and L. brazilienisis by Foxp3+ cells [15], [16], [47] and upregulation of FOXP3 in lesions from post Kala Azar DL [48]. Foxp3 may therefore constitute a marker for chronic DL caused by L. (Viannia) species.
Although CDL patients had higher numbers of CD25hiFoxp3+ cells in peripheral blood than AI, the capacity of their CD4+CD25+ cells to inhibit pro-inflammatory IFN-γ secretion by effector T cells elicited by Leishmania antigens was lower. This suggests that the CD25hiFoxp3+ cells that accounted for the higher frequency in CDL patients are not specific for Leishmania antigens. Since Foxp3 is a marker of natural Tregs generated in the thymus after interaction with self antigens [37], [51], these cells may be a subset of Tregs specific for self antigens that are released during the inflammatory response [7], [52], [53]. Alternatively, the higher proportion of CD25hiFoxp3+ cells may reflect chronic activation in CDL patients, since FoxP3 can be transiently expressed by activated T cells [49], [50]. However, we do not favor this explanation because high expression of CD25 has been consistently proven to be a marker of Tregs [31]–[34] and effector cells expressing FoxP3 are mostly not CD25hi [50]. Thus, we postulate that CD25hiFoxp3+ Tregs, although more frequent in CDL, are not responsible for the antigen specific suppression demonstrated in the co-culture assays. Rather, this suppression is attributable to a Leishmania-specific, Foxp3− subset. However, we cannot rule out the possibility that Leishmania-specific effector cells acquired resistance to regulation by Tregs after chronic antigenic stimulation in CDL.
Clinical evaluation at the end of treatment with pentavalent antimony showed that all patients had initiated a healing response. Half had already healed completely while the other half showed significant improvement (≥50%, Table 1). Clinical follow-up was possible for 7/11 patients at ≥13 weeks after starting treatment and confirmed that all seven had completely healed (data not shown). Thus, no evidence of treatment failure was seen in this study cohort. The healing responses in this CDL cohort were associated with significant increases in the frequency of CD25hiCD127− CD4 T cells in peripheral blood and in Leishmania-specific inhibition of CD4 T cell effector functions by CD4+CD25+ cells. In fact, of the 11 patients, 10 were able to inhibit IFN-γ secretion by ≥75% at the end of treatment and 9 showed an increase in CD4+CD25hiCD127− cells. Furthermore, transcription of IFNG at the lesion site was not significantly upregulated at the end of treatment, but rather decreased in 8 of the 11 patients. Interestingly, we found that Foxp3 expression did not change after treatment in CD4+CD25hi blood cells or at the lesion site, suggesting that a Foxp3+ subset of Tregs was not responsible for the heightened suppression that was associated with healing. Rather, these findings support the participation of a CD127−, Leishmania-specific subset of Tregs in the healing of chronic dermal lesions caused by L. (Viannia).
Induction of Tregs during chronic infections is the result of antigen presentation in a particular cytokine environment [7], [53]. In the current study, parasite killing mediated by the anti-leishmanial drug would presumably lead to release of antigens, new antigen presentation events and Treg induction and/or activation in the peripheral lymphoid organs [54]. Newly induced Tregs would home to the lesion site to mitigate the inflammatory response and aid in tissue repair. Homing of Tregs to the skin is essential for the maintenance of skin homeostasis and for suppression of Th1 cell-mediated responses [55], [56]. Furthermore, Tregs have been shown to contribute substantially to tissue repair by providing regulation at sites of healing in many experimental models. In an in vitro wound healing model, Tregs were shown to counteract Th17 cell-mediated inhibition of fibroblast migration into the wound [57], and tissue regeneration after kidney injury was shown to depend on inhibition of pro-inflammatory cytokine secretion by Tregs [58]. In another in vitro model, intact extracellular matrix components that gradually replace inflammation-promoting fragmented components during tissue repair induce Tregs and activate their function [59]. Therefore, healing of dermal lesions such as those present in CDL would likely benefit from immune regulation by Tregs. Since all patients had initiated a healing response at the end of treatment, our results are consistent with the participation of a subset of Foxp3− CD127− Leishmania-specific Tregs in lesion resolution.
The limited absolute numbers of CD4+CD25+ cells allowed us to test only two effector∶Treg ratios. Significant differences in antigen-specific suppression were detected at the 1∶1 ratio, but not at the 4∶1 ratio. Since suppression by Tregs is activated through cognate peptide/MHC-TCR interactions [60], the inability to detect suppression at a higher ratio is probably due to the expected low frequency of Leishmania-specific Tregs at the outset of co-culture and the absence of proliferation by these cells [61] (as evidenced by lack of variation in forward scatter, Figure S1A). Therefore, even though the number of Leishmania-specific CD25hi T cells in the co-culture is unknown, the observation of significant suppression indicates that the number reached an effective threshold under the assay conditions at a 1∶1 ratio. In addition, the CD4+CD25+ preparation includes activated effector T cells that upregulate CD25 and, therefore, the number of Tregs in the culture would have been diluted by these cells. For these reasons, we believe that the suppression observed in our system at a 1∶1 ratio reflects the presence of circulating antigen-specific Tregs that can contribute to the mitigation of the inflammatory response upon homing to the lesion site.
We examined the participation of IL-10 in the inhibition of CD4 T cell effector functions in our co-cultures because this cytokine is secreted by T cells with an effector phenotype in intracellular parasitic infections [62]–[64] as well as by Tregs. Furthermore, we have previously determined in a population from the same region that IL-10 is expressed in susceptible individuals and related to both development of CDL and IFN-γ secretion [4]. Hence, it was conceivable that inhibition was due to IL-10 secretion by a CD25+ activated effector population present in the CD4+CD25+ preparation and not by Tregs. The diminished production of IL-10 in co-cultures including CD4+CD25+ cells demonstrated that IL-10 was not responsible for suppression by these cells, supporting the interpretation that the observed inhibition was indeed mediated by bona fide Tregs. We also found that IL10 transcription was not significantly changed at the lesion site immediately following treatment, suggesting that this cytokine is not prominent in the healing process.
IDO is an enzyme expressed by APCs that metabolizes tryptophan, an essential aminoacid for both lymphocyte proliferation and parasite survival [38], [39]. Hence, the expression of IDO in leishmaniasis lesions may regulate the immune response and aid in parasite eradication. Its expression is induced by inflammatory cytokines, including IFN-γ [40], [41], and by Tregs through interaction of CTLA-4 and B7 molecules [42]. Therefore, IDO transcription in the skin may reflect both the inflammatory environment and Treg function. In this study, we found that the expression of IDO was correlated with that of IFNG and not to FOXP3 in CDL patients. This indicates that IDO induction in APCs is not a likely mechanism of suppression used by Tregs that infiltrate sites of ongoing immune responses to Leishmania in CDL patients. Rather, IDO expression reflects the reduced inflammatory environment present at these sites, which is consistent with increased function of a subset of Tregs after treatment.
The relatively small sample size limited our ability to detect statistically significant differences in the expression of the genes IFNG and IDO between AI (healing/clinical resistance) and patients with chronic disease (non-healing/clinical susceptibility) even though several of the latter showed marked upregulation. Furthermore, although we did not determine the mechanism of regulation by CD4+CD25+ cells, the results of functional as well as phenotypic analyses provide compelling evidence of the participation of distinct Treg subsets in both pathogenesis and resolution of CDL caused by Leishmania species of the (Viannia) subgenus. Further characterization of these subsets is warranted since immunotherapeutic strategies targeting these regulatory cells could promote healing of recalcitrant presentations of leishmaniasis.
Supporting Information
Gating strategy for analysis of CD4+CD25− cell proliferation. CFSE labeled CD4+CD25− cells were cultured for 5 days with antigen presenting cells (APCs), L. panamensis, CD4+CD25+ cells or PHA, as indicated. A. Gates for CFSE labeled cells were determined in the CD4+ region to exclude unlabeled cells from the analysis. B. Regions for the proliferating populations were drawn in the CFSE labeled gate based on the peaks induced by PHA and used to calculate the proliferation index (PI) with the formula PI = Σ(% in region×2n−1), where n is the region number. One representative subject is shown.
(TIF)
Acknowledgments
We gratefully acknowledge the provision of training in regulatory T cell isolation by Drs. Gyongyi Szabo and Angela Dolganiuc, University of Massachusetts, and thank Dr. Maria Adelaida Gomez for her assistance in implementing these methods in CIDEIM. The logistic and operational support of Liliana Valderrama in the planning and coordination of laboratory and field activities and the support of the CIDEIM clinical unit staff Dr. Luisa Rubiano, Javier Martinez and Wilson Cortez in the enrollment and clinical care of participants, and sample procurement and management is recognized with gratitude. We thank Rafael Góngora and Olga Fernandez for parasite species identification, Graciela Salinas and Dr. Juan Carlos Bravo for their assistance and support in processing of biopsies, Mauricio Perez for statistical support, James Becerra for data management, and Maria Teresa Ochoa from the University of Southern California for insights and advice during the development of this investigation.
Footnotes
The authors have declared that no competing interests exist.
This work was supported by COLCIENCIAS (grant number 265 2229-459-21594), Fogarty International Center (NIH) (grant number D43 TW006589), and the United States National Institutes of Health (NIH), National Institute of Allergy and Infectious Diseases (grant numbers U19 AI065866 43TW006589 and 1R01AI093775-01). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Murray HW, Berman JD, Davies CR, Saravia NG. Advances in leishmaniasis. Lancet. 2005;366:1561–1577. doi: 10.1016/S0140-6736(05)67629-5. [DOI] [PubMed] [Google Scholar]
- 2.Saravia NG, Valderrama L, Labrada M, Holguín AF, Navas C, et al. The relationship of Leishmania braziliensis subspecies and immune response to disease expression in New World leishmaniasis. J Infect Dis. 1989;159:725–735. doi: 10.1093/infdis/159.4.725. [DOI] [PubMed] [Google Scholar]
- 3.Carvalho EM, Johnson WD, Barreto E, Marsden PD, Costa JL, et al. Cell mediated immunity in American cutaneous and mucosal leishmaniasis. J Immunol. 1985;135:4144–4148. [PubMed] [Google Scholar]
- 4.Castilho TM, Goldsmith-Pestana K, Lozano C, Valderrama L, Saravia NG, et al. Murine model of chronic L. (Viannia) panamensis infection: role of IL-13 in disease. Eur J Immunol. 2010;40:2816–2829. doi: 10.1002/eji.201040384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Díaz YR, Rojas R, Valderrama L, Saravia NG. T-bet, GATA-3, and Foxp3 expression and Th1/Th2 cytokine production in the clinical outcome of human infection with Leishmania (Viannia) species. J Infect Dis. 2010;202:406–415. doi: 10.1086/653829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pirmez C, Yamamura M, Uyemura K, Paes-Oliveira M, Conceição-Silva F, et al. Cytokine patterns in the pathogenesis of human leishmaniasis. J Clin Invest. 1993;91:1390–1395. doi: 10.1172/JCI116341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belkaid Y, Tarbell K. Regulatory T cells in the control of host-microorganism interactions. Annu Rev Immunol. 2009;27:551–589. doi: 10.1146/annurev.immunol.021908.132723. [DOI] [PubMed] [Google Scholar]
- 8.Sanchez AM, Yang Y. The role of natural regulatory T cells in infection. Immunol Res. 2010;49:124–134. doi: 10.1007/s12026-010-8176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Belkaid Y, Piccirillo CA, Mendez S, Shevach EM, Sacks DL. CD4+CD25+ regulatory T cells control Leishmania major persistence and immunity. Nature. 2002;420:502–507. doi: 10.1038/nature01152. [DOI] [PubMed] [Google Scholar]
- 10.Mendez S, Reckling SK, Piccirillo CA, Sacks D, Belkaid Y. Role for CD4(+) CD25(+) regulatory T cells in reactivation of persistent leishmaniasis and control of concomitant immunity. J Exp Med. 2004;200:201–210. doi: 10.1084/jem.20040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aseffa A, Gumy A, Launois P, MacDonald HR, Louis JA, et al. The early IL-4 response to Leishmania major and the resulting Th2 cell maturation steering progressive disease in BALB/c mice are subject to the control of regulatory CD4+CD25+ T cells. J Immunol. 2002;169:3232–3241. doi: 10.4049/jimmunol.169.6.3232. [DOI] [PubMed] [Google Scholar]
- 12.Xu D, Liu H, Komai-Koma M, Campbell C, McSharry C, et al. CD4+CD25+ regulatory T cells suppress differentiation and functions of Th1 and Th2 cells, Leishmania major infection, and colitis in mice. J Immunol. 2003;170:394–399. doi: 10.4049/jimmunol.170.1.394. [DOI] [PubMed] [Google Scholar]
- 13.Ji J, Masterson J, Sun J, Soong L. CD4+CD25+ regulatory T cells restrain pathogenic responses during Leishmania amazonensis infection. J Immunol. 2005;174:7147–7153. doi: 10.4049/jimmunol.174.11.7147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salhi A, Rodrigues V, Jr, Santoro F, Dessein H, Romano A, et al. Immunological and genetic evidence for a crucial role of IL-10 in dermal lesions in humans infected with Leishmania braziliensis. J Immunol. 2008;180:6139–6148. doi: 10.4049/jimmunol.180.9.6139. [DOI] [PubMed] [Google Scholar]
- 15.Campanelli AP, Roselino AM, Cavassani KA, Pereira MS, Mortara RA, et al. CD4+CD25+ T cells in skin lesions of patients with dermal leishmaniasis exhibit phenotypic and functional characteristics of natural regulatory T cells. J Infect Dis. 2006;193:1313–1322. doi: 10.1086/502980. [DOI] [PubMed] [Google Scholar]
- 16.Bourreau E, Ronet C, Darcissac E, Lise MC, Sainte Marie D, et al. Intralesional regulatory T-cell suppressive function during human acute and chronic dermal leishmaniasis due to Leishmania guyanensis. Infect Immun. 2009;77:1465–1474. doi: 10.1128/IAI.01398-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bourreau E, Ronet C, Darsissac E, Lise MC, Marie DS, et al. In leishmaniasis due to Leishmania guyanensis infection, distinct intralesional interleukin-10 and Foxp3 mRNA expression are associated with unresponsiveness to treatment. J Infect Dis. 2009;199:576–579. doi: 10.1086/596508. [DOI] [PubMed] [Google Scholar]
- 18.Saravia NG, Weigle K, Segura I, Giannini SH, Pacheco R, et al. Recurrent lesions in human Leishmania braziliensis infection–reactivation or reinfection? Lancet. 1990;336:398–402. doi: 10.1016/0140-6736(90)91945-7. [DOI] [PubMed] [Google Scholar]
- 19.Wortmann GW, Aronson NE, Miller RS, Blazes D, Oster CN. Cutaneous leishmaniasis following local trauma: a clinical pearl. Clin Infect Dis. 2000;31:199–201. doi: 10.1086/313924. [DOI] [PubMed] [Google Scholar]
- 20.de Oliveira Camera P, Junger J, do Espírito Santo Silva Pires F, Mattos M, Oliveira-Neto MP, et al. Haematogenous dissemination of Leishmania (Viannia) braziliensis in human American tegumentary leishmaniasis. Trans R Soc Trop Med Hyg. 2006;100:1112–1117. doi: 10.1016/j.trstmh.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 21.Vergel C, Palacios R, Cadena H, Posso CJ, Valderrama L, et al. Evidence for leishmania (viannia) parasites in the skin and blood of patients before and after treatment. J Infect Dis. 2006;194:503–511. doi: 10.1086/505583. [DOI] [PubMed] [Google Scholar]
- 22.Schubach A, Haddad F, Oliveira-Neto MP, Degrave W, Pirmez C, et al. Detection of Leishmania DNA by polymerase chain reaction in scars of treated human patients. J Infect Dis. 1998;178:911–914. doi: 10.1086/515355. [DOI] [PubMed] [Google Scholar]
- 23.Schubach A, Marzochi MC, Cuzzi-Maya T, Oliveira AV, Araujo ML, et al. Cutaneous scars in American tegumentary leishmaniasis patients: a site of Leishmania (Viannia) braziliensis persistence and viability eleven years after antimonial therapy and clinical cure. Am J Trop Med Hyg. 1998;58:824–827. doi: 10.4269/ajtmh.1998.58.824. [DOI] [PubMed] [Google Scholar]
- 24.Corredor A, Kreutzer RD, Tesh RB, Boshell J, Palau MT, et al. Distribution and etiology of leishmaniasis in Colombia. Am J Trop Med Hyg. 1990;42:206–214. doi: 10.4269/ajtmh.1990.42.206. [DOI] [PubMed] [Google Scholar]
- 25.Osorio LE, Castillo CM, Ochoa MT. Mucosal leishmaniasis due to Leishmania (Viannia) panamensis in Colombia: clinical characteristics. Am J Trop Med Hyg. 1998;59:49–52. doi: 10.4269/ajtmh.1998.59.49. [DOI] [PubMed] [Google Scholar]
- 26.Guarín N, Palma GI, Pirmez C, Valderrama L, Tovar R, et al. Comparative immunohistological analysis of the Montenegro skin test reaction in asymptomatic infection and in acute and chronic dermal leishmaniasis. Biomedica. 2006;26:38–48. [PubMed] [Google Scholar]
- 27.Saravia NG, Weigle K, Navas C, Segura I, Valderrama L, et al. Heterogeneity, geographic distribution, and pathogenicity of serodemes of Leishmania viannia in Colombia. Am J Trop Med Hyg. 2002;66:738–744. doi: 10.4269/ajtmh.2002.66.738. [DOI] [PubMed] [Google Scholar]
- 28.Bosque F, Saravia NG, Valderrama L, Milon G. Distinct innate and acquired immune responses to Leishmania in putative susceptible and resistant human populations endemically exposed to L. (Viannia) panamensis infection. Scand J Immunol. 2000;51:533–541. doi: 10.1046/j.1365-3083.2000.00724.x. [DOI] [PubMed] [Google Scholar]
- 29.Brusko TM, Hulme MA, Myhr CB, Haller MJ, Atkinson MA. Assessing the in vitro suppressive capacity of regulatory T cells. Immunol Invest. 2007;36:607–628. doi: 10.1080/08820130701790368. [DOI] [PubMed] [Google Scholar]
- 30.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 31.Baecher-Allan C, Viglietta V, Hafler DA. Human CD4+CD25+ regulatory T cells. Semin Immunol. 2004;16:89–98. doi: 10.1016/j.smim.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 32.Wing K, Ekmark A, Karlsson H, Rudin A, Suri-Payer E. Characterization of human CD25+ CD4+ T cells in thymus, cord and adult blood. Immunology. 2002;106:190–199. doi: 10.1046/j.1365-2567.2002.01412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baecher-Allan C, Brown JA, Freeman GJ, Hafler DA. CD4+CD25+ regulatory cells from human peripheral blood express very high levels of CD25 ex vivo. Novartis Found Symp. 2003;252:67–91. doi: 10.1002/0470871628.ch6. [DOI] [PubMed] [Google Scholar]
- 34.Levings MK, Sangregorio R, Sartirana C, Moschin AL, Battaglia M, et al. Human CD25+CD4+ T suppressor cell clones produce transforming growth factor beta, but not interleukin 10, and are distinct from type 1 T regulatory cells. J Exp Med. 2002;196:1335–1346. doi: 10.1084/jem.20021139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seddiki N, Santner-Nanan B, Martinson J, Zaunders J, Sasson S, et al. Expression of interleukin (IL)-2 and IL-7 receptors discriminates between human regulatory and activated T cells. J Exp Med. 2006;203:1693–1700. doi: 10.1084/jem.20060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yagi H, Nomura T, Nakamura K, Yamazaki S, Kitawaki T, et al. Crucial role of FOXP3 in the development and function of human CD25+CD4+ regulatory T cells. Int Immunol. 2004;16:1643–1656. doi: 10.1093/intimm/dxh165. [DOI] [PubMed] [Google Scholar]
- 37.Miyara M, Sakaguchi S. Human Foxp3(+)CD4(+) regulatory T cells: their knowns and unknowns. Immunol Cell Biol. 2011;89:346–351. doi: 10.1038/icb.2010.137. [DOI] [PubMed] [Google Scholar]
- 38.Grohmann U, Fallarino F, Puccetti P. Tolerance, DCs and tryptophan: much ado about IDO. Trends Immunol. 2003;24:242–248. doi: 10.1016/s1471-4906(03)00072-3. [DOI] [PubMed] [Google Scholar]
- 39.Mellor AL, Munn DH. IDO expression by dendritic cells: tolerance and tryptophan catabolism. Nat Rev Immunol. 2004;4:762–774. doi: 10.1038/nri1457. [DOI] [PubMed] [Google Scholar]
- 40.Taylor MW, Feng GS. Relationship between interferon-gamma, indoleamine 2,3-dioxygenase, and tryptophan catabolism. FASEB J. 1991;5:2516–2522. [PubMed] [Google Scholar]
- 41.Hassanain HH, Chon SY, Gupta SL. Differential regulation of human indoleamine 2,3-dioxygenase gene expression by interferons-gamma and -alpha. Analysis of the regulatory region of the gene and identification of an interferon-gamma-inducible DNA-binding factor. J Biol Chem. 1993;268:5077–5084. [PubMed] [Google Scholar]
- 42.Fallarino F, Grohmann U, Hwang KW, Orabona C, Vacca C, et al. Modulation of tryptophan catabolism by regulatory T cells. Nat Immunol. 2003;4:1206–1212. doi: 10.1038/ni1003. [DOI] [PubMed] [Google Scholar]
- 43.Andersson J, Boasso A, Nilsson J, Zhang R, Shire NJ, et al. The prevalence of regulatory T cells in lymphoid tissue is correlated with viral load in HIV-infected patients. J Immunol. 2005;174:3143–3147. doi: 10.4049/jimmunol.174.6.3143. [DOI] [PubMed] [Google Scholar]
- 44.Guyot-Revol V, Innes JA, Hackforth S, Hinks T, Lalvani A. Regulatory T cells are expanded in blood and disease sites in patients with tuberculosis. Am J Respir Crit Care Med. 2006;173:803–810. doi: 10.1164/rccm.200508-1294OC. [DOI] [PubMed] [Google Scholar]
- 45.Walther M, Tongren JE, Andrews L, Korbel D, King E, et al. Upregulation of TGF-beta, FOXP3, and CD4+CD25+ regulatory T cells correlates with more rapid parasite growth in human malaria infection. Immunity. 2005;23:287–296. doi: 10.1016/j.immuni.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 46.Lin CY, Tsai MC, Huang CT, Hsu CW, Tseng SC, et al. Liver injury is associated with enhanced regulatory T-cell activity in patients with chronic hepatitis B. J Viral Hepat. 2007;14:503–511. doi: 10.1111/j.1365-2893.2006.00835.x. [DOI] [PubMed] [Google Scholar]
- 47.Souza-Lemos C, de-Campos SN, Teva A, Porrozzi R, Grimaldi G., Jr In situ characterization of the granulomatous immune response with time in nonhealing lesional skin of Leishmania braziliensis-infected rhesus macaques (Macaca mulatta). Vet Immunol Immunopathol. 2011;142:147–155. doi: 10.1016/j.vetimm.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 48.Katara GK, Ansari NA, Verma S, Ramesh V, Salotra P. Foxp3 and IL-10 Expression Correlates with Parasite Burden in Lesional Tissues of Post Kala Azar Dermal Leishmaniasis (PKDL) Patients. PLoS Negl Trop Dis. 2011;5:e1171. doi: 10.1371/journal.pntd.0001171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang J, Ioan-Facsinay A, van der Voort EI, Huizinga TW, Toes RE. Transient expression of FOXP3 in human activated nonregulatory CD4+ T cells. Eur J Immunol. 2007 Jan;37(1):129–38. doi: 10.1002/eji.200636435. [DOI] [PubMed] [Google Scholar]
- 50.Allan SE, Crome SQ, Crellin NK, Passerini L, Steiner TS, Bacchetta R, Roncarolo MG, Levings MK. Activation-induced FOXP3 in human T effector cells does not suppress proliferation or cytokine production. Int Immunol. 2007 Apr;19(4):345–54. doi: 10.1093/intimm/dxm014. [DOI] [PubMed] [Google Scholar]
- 51.Miyara M, Yoshioka Y, Kitoh A, Shima T, Wing K, et al. Functional delineation and differentiation dynamics of human CD4+ T cells expressing the Foxp3 transcription factor. Immunity. 2009;30:899–911. doi: 10.1016/j.immuni.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 52.Bluestone JA, Abbas AK. Natural versus adaptive regulatory T cells. Nat Rev Immunol. 2003;3:253–257. doi: 10.1038/nri1032. [DOI] [PubMed] [Google Scholar]
- 53.Wohlfert E, Belkaid Y. Role of endogenous and induced regulatory T cells during infections. J Clin Immunol. 2008;28:707–715. doi: 10.1007/s10875-008-9248-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kautz-Neu K, Noordegraaf M, Dinges S, Bennett CL, John D, et al. Langerhans cells are negative regulators of the anti-Leishmania response. J Exp Med. 2011;208:885–891. doi: 10.1084/jem.20102318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dudda JC, Perdue N, Bachtanian E, Campbell DJ. Foxp3+ regulatory T cells maintain immune homeostasis in the skin. J Exp Med. 2008;205:1559–1565. doi: 10.1084/jem.20072594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Siegmund K, Feuerer M, Siewert C, Ghani S, Haubold U, et al. Migration matters: regulatory T-cell compartmentalization determines suppressive activity in vivo. Blood. 2005;106:3097–3104. doi: 10.1182/blood-2005-05-1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Crome SQ, Clive B, Wang AY, Kang CY, Chow V, et al. Inflammatory effects of ex vivo human Th17 cells are suppressed by regulatory T cells. J Immunol. 2010;185:3199–3208. doi: 10.4049/jimmunol.1000557. [DOI] [PubMed] [Google Scholar]
- 58.Gandolfo MT, Jang HR, Bagnasco SM, Ko GJ, Agreda P, et al. Foxp3+ regulatory T cells participate in repair of ischemic acute kidney injury. Kidney Int. 2009;76:717–729. doi: 10.1038/ki.2009.259. [DOI] [PubMed] [Google Scholar]
- 59.Bollyky PL, Falk BA, Wu RP, Buckner JH, Wight TN, et al. Intact extracellular matrix and the maintenance of immune tolerance: high molecular weight hyaluronan promotes persistence of induced CD4+CD25+ regulatory T cells. J Leukoc Biol. 2009;86:567–572. doi: 10.1189/jlb.0109001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jonuleit H, Schmitt E, Kakirman H, Stassen M, Knop J, et al. Infectious tolerance: human CD25(+) regulatory T cells convey suppressor activity to conventional CD4(+) T helper cells. J Exp Med. 2002;196:255–260. doi: 10.1084/jem.20020394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baecher-Allan C, Brown JA, Freeman GJ, Hafler DA. CD4+CD25high regulatory cells in human peripheral blood. J Immunol. 2001;167:1245–1253. doi: 10.4049/jimmunol.167.3.1245. [DOI] [PubMed] [Google Scholar]
- 62.Anderson CF, Oukka M, Kuchroo VJ, Sacks D. CD4(+)CD25(−)Foxp3(−) Th1 cells are the source of IL-10-mediated immune suppression in chronic dermal leishmaniasis. J Exp Med. 2007;204:285–297. doi: 10.1084/jem.20061886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jankovic D, Kullberg MC, Feng CG, Goldszmid RS, Collazo CM, et al. Conventional T-bet(+)Foxp3(−) Th1 cells are the major source of host-protective regulatory IL-10 during intracellular protozoan infection. J Exp Med. 2007;204:273–283. doi: 10.1084/jem.20062175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.O'Garra A, Vieira P. T(H)1 cells control themselves by producing interleukin-10. Nat Rev Immunol. 2007;7:425–428. doi: 10.1038/nri2097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Gating strategy for analysis of CD4+CD25− cell proliferation. CFSE labeled CD4+CD25− cells were cultured for 5 days with antigen presenting cells (APCs), L. panamensis, CD4+CD25+ cells or PHA, as indicated. A. Gates for CFSE labeled cells were determined in the CD4+ region to exclude unlabeled cells from the analysis. B. Regions for the proliferating populations were drawn in the CFSE labeled gate based on the peaks induced by PHA and used to calculate the proliferation index (PI) with the formula PI = Σ(% in region×2n−1), where n is the region number. One representative subject is shown.
(TIF)