Abstract
OBJECTIVE
To estimate the effectiveness of a behavioral educational intervention to reduce postpartum depressive symptoms among minority mothers.
METHODS
We recruited 540 self-identified black or African American and Latina or Hispanic mothers during their postpartum hospital stay and randomized them to receive a behavioral educational intervention or enhanced usual care. The intervention arm received a two-step behavioral educational intervention that prepares and educates mothers about modifiable factors associated with symptoms of postpartum depression (physical symptoms, low social support, low self-efficacy, and infant factors), bolsters social support, enhances management skills, and increases participants’ access to resources. Enhanced usual care participants received a list of community resources and received a 2-week control call. Participants were surveyed prior to randomization, 3-weeks, 3-months, and 6-months later to assess depressive symptoms. The primary outcome, depression, was assessed using the Edinburgh Postnatal Depression Scale (score of 10 or greater).
RESULTS
Positive depression screens were less common among intervention vs. enhanced usual care post-hospitalization: 3-weeks (8.8% vs. 15.3%, p=.03), 3-months (8.4% vs. 13.24%, p=.09) and 6-months (8.9% vs.13.7%, p=.11). An intention-to-treat repeated measures analysis for up to 6 months of follow-up demonstrated that mothers in the intervention group were less likely to screen positive for depression versus enhanced usual care (odds ratio of 0.67; 95% confidence interval [CI] 0.47–0.97; number needed to treat, 16; 95% CI: 9–112)
CONCLUSION
An action oriented behavioral educational intervention reduced positive depression screens among black and Latina postpartum mothers.
INTRODUCTION
Symptoms of depression postpartum are a major health problem and affect hundreds of thousands of American mothers annually.1–4 Experiencing these symptoms after childbirth has a negative effect on maternal quality of life and ability to function.5, 6 In addition, untreated postpartum depression has an adverse effect upon maternal infant interaction that negatively impact infants' cognitive, social, and emotional development.7–10 The burden of postpartum depressive symptoms is especially high in low-income black and Latina women.3, 11, 12
Prior research by us and others suggest that a range of situational factors such as postpartum physical symptoms, overload from daily demands, and poor social support play a major role in the generation of depressive symptoms.3, 13–15 Based on these findings, we created a behavioral-educational intervention aimed at reducing the frequency of depressive symptoms in postpartum mothers by preparing women about specific situational triggers of depressive symptoms, bolstering their personal and social resources, and suggesting specific actions to enhance their self-management skills to buffer postpartum demands. The intervention was aimed at prevention of depressive symptoms, not treatment of major depression. The primary outcome was the reduction of positive postpartum depression screens among black and Latina mothers randomized to the intervention arm.
METHODS
Participants included 540 self-identified black or African American and Latina or Hispanic postpartum mothers who delivered between April 2009 and March 2010 at a large tertiary inner-city hospital located in East Harlem in New York City. The Program for the Protection of Human Subjects (the Institutional Review Board) at Mount Sinai School of Medicine approved this study. The patient sample was identified through an electronic documentation system for the labor and delivery unit. Eligible participants were black or African American, or Latina or Hispanic, aged 18 years or older, had infants with birth weights of 2500 grams or higher, and 5-minute Apgar scores of 7 or greater. Maternal race, maternal ethnicity, maternal age, infant Apgar scores, and infant birth weight are contained in the electronic system.
To insure eligibility, two bilingual clinical research coordinators asked additional questions of mothers who met initial requirements from the electronic record. Final eligible mothers self-identified as black or African American, or Latina or Hispanic, spoke English or Spanish, and had a working telephone. The clinical research coordinators approached mothers between their delivery day and postpartum day #2 (recruitment was done Mondays through Fridays). Patients were assigned a number between 1 and 20 in order of delivery date and time and then approached in the order set by that day’s list of random numbers generated by the project statistician. Our study team recruited between 12 and 14 patients per week.
After obtaining informed written consent, enrolled participants completed a 20 minute baseline in-hospital survey. Patients were randomized to conditions in four stages. The statistician carried out randomization using a computerized procedure that used a random number generator to assign participants to intervention or enhanced usual care. At the end of each stage, the randomization allocation could be potentially adjusted based on important covariates (e.g. race/ethnicity, EPDS score). No adjustment to randomization was initiated at any time. The research clinical coordinators were blinded to study arm assignment.
Patients randomized to the intervention arm were given a 2-step behavioral educational intervention. The in-hospital component of the intervention involved a 15-minute, in hospital review of a patient education pamphlet and partner summary sheet by the mother with a masters-trained bilingual social worker. The pamphlet represented each potential trigger of depressive symptoms as a “normal” aspect of the postpartum experience, and provided specific suggestions for management. For example, the prevalence of moderate or heavy vaginal bleeding immediately postpartum was depicted by 8 of 10 female silhouettes colored red; only 1 of 10 was red 3 months post delivery. Simple “to do” statements (Rest; Use pads) were listed between the two rows of figures. Postpartum and 3 month rates and intermediate “to do” lists also were provided for c-section site pain, episiotomy site pain, urinary incontinence, breast pain, back pain, headaches, hair loss, hemorrhoids, feeling sad and blue/depressive symptoms, and infant colic. A separate page was dedicated to social support and “helpful organizations” were listed. The partner summary sheet spelled out the typical pattern of experience for mothers postpartum, i.e., it was designed to “normalize” the feelings and behaviors experienced and enacted by most mothers postpartum and stressed the importance of social support for the patient. The social worker reviewed the patient education pamphlet and partner summary sheet with the patient during her postpartum hospital stay and answered questions.
The second and final component of the intervention was a two-week post delivery call in which the social worker assessed patients’ symptoms, skills in symptom management, and other needs. The “to do” lists to help alleviate symptoms were reviewed when needed and patient and social worker created action plans to address current needs including accessing community resources. Fidelity of the intervention was maintained by repeated training and review of scripts for both the in person in-hospital and telephone components of the intervention. Approximately 5% of both in-hospital sessions and two-week telephone needs assessment were observed by a physician or project manager on the team.
The content of the intervention was based on responses from our prior studies, focus groups with postpartum mothers, obstetricians, psychiatrists, social workers, and our community advisory board. The intervention was pilot tested with 50 diverse postpartum mothers and revised based on feedback from pilot study participants, the results from two focus groups conducted with black and Latina postpartum mothers, and feedback from community advisory board members (community representatives from Harlem). Content, pictures, wording, and length were revised according to input from these sources. Materials were translated to Spanish and back translated for accuracy and consistency of meaning.
Enhanced usual care patients received routine postpartum hospital education, (i.e. discharge materials, television educational programs on infant care, breastfeeding, and peripartum care). To insure equivalent contact, patients assigned to enhanced usual care control received a two-week post delivery call to inform them of future surveys and a list of health-related and community resources was mailed to them.
Interviewers were blinded to study arm assignment. All study participants were interviewed by phone at 3-weeks (mean days = 27.6, SD 5.8; median days = 27, range of 20 to 52), 3-months (mean days = 83.5, SD 7.8; median days = 81, range of 76 to 124) and at 6-months (mean days = 175.6, SD 8.9; median days = 174, range of 165 to 218) to assess depressive symptoms and contributing and buffering factors. Postnatal depressive symptoms were assessed using the 10-item Edinburgh Postnatal Depression Scale (EPDS). The EPDS is a common measure used in research to assess symptoms of postpartum depression in both treatment and prevention trials, and has been validated in many postpartum populations and different languages.16–29 The recommended cut-off score of 10 or greater has sensitivities of 0.59–0.81 and specificities ranged from 0.77–0.88 for major and minor depression.2 The Patient Health Questionnaire-9 was also administered and a comparison was made between the EPDS and PHQ-9 scores over time in a secondary analysis. Survey items also included questions on sociodemographics, clinical characteristics such as antepartum complications, comorbid conditions (e.g. diabetes, hypertension, asthma, thyroid disease, heart disease), past depression history, anxiety, social support, and healthcare factors. Medical charts were reviewed for parity, delivery type, insurance, past medical history, maternal complications, delivery complications, and infant outcomes.
After patients were consented and completed the baseline survey, women reporting high levels of depressive symptoms (EPDS of 13 or greater, PHQ-9 of 20 or greater, or suicidal ideation) were referred for inpatient psychiatric assessment and possible treatment. To address risk over time, all mothers, including those referred for inpatient assessment at baseline, were retained in the study, and mothers who reported high levels of depressive or suicidal symptoms at any time point were referred for psychiatric assessment/treatment. Analyses excluding mothers referred for baseline psychiatric intervention during hospitalization were planned a-priori.
Sample size was powered to detect a clinically meaningful difference in reduction of symptoms of postpartum depression 3 weeks post randomization for women in the intervention arm in comparison with women in enhanced usual care. Assuming that 46% of black and Latina women would report depressive symptoms (EPDS of 10 or greater) in enhanced usual care (based on published literature and our studies of postpartum depressive symptoms among inner-city black and Latina mothers3,4), our recruitment target of 460 patients (230 per arm) met 90% power based on a two-sided 0.05 level chi-squared test to detect a clinically meaningful 15% reduction in depressive symptoms (from 46% to 31%, a relative risk reduction of about 33%). To allow for decreased power due to patient loss at follow-up we planned to enroll 540 participants.
Data were collected in-person at baseline and by telephone during follow-up interviews by bilingual clinical research coordinators blinded to intervention status. All data were entered directly into a laptop computerized instrument linked to a Microsoft Access database. Participants in the intervention arm (N=270) and enhanced usual care (N=270) were compared at baseline on demographic and clinical characteristics using t-tests and their non-parametric equivalents, chi-square tests, as appropriate. Group differences were summarized by 95% confidence interval estimates. Overall study attrition rate was low and equivalent across treatment groups. The amount of missing data for our primary outcome measure, EPDS, was low at 3-weeks (13%; 71/ 540), 3-months (12%; 62/540) and six months (22%; 117/540), and similar between groups at each time point.
The primary analysis examined the efficacy of the intervention in reducing the likelihood of positive postpartum depression screens. Planned subgroup analyses examined whether the intervention reduced the likelihood of a positive depression screen among mothers who scored below 13 on the EPDS and were therefore not referred for baseline psychiatric intervention. Prior to conducting these analyses, missing data were imputed, i.e. estimated using a multiple imputation approach.30 Data were assumed to be missing at random as baseline characteristics for those missing outcomes at 3-weeks were very similar to those for whom outcomes were available at 3-weeks, with the only significant differences (p<.05) being that those with missing outcomes were more likely to be born in the US, to speak English, and have past history of depression. The regression models used baseline EPDS scores and past depression history. Five complete data sets were created using multiple imputations and analyzed and combined using the MIANALYZE procedure in SAS. The final parameter estimate and the associated standard errors account for both with-in and between-imputation variance. As imputation yielded similar results to the observed trial results both for the total sample and the subgroup analysis including the mothers not referred for intervention (92% of the sample), we present observed results, the more conservative estimate of effect, for both. The logistic regression analyses tested the effect of the intervention on positive depression screens at 3 weeks, 3 months, and 6 months postpartum. We conducted adjusted analyses for the subgroup of mothers not referred for treatment at baseline. We included independent variables that were associated with a positive depression screen at baseline. To assess change over time across groups for the primary outcome, mixed-effects models using maximum likelihood procedures were employed. Significance level of 0.05 was used for the primary outcome of postpartum depression and the final model was adjusted for baseline depression screen.
RESULTS
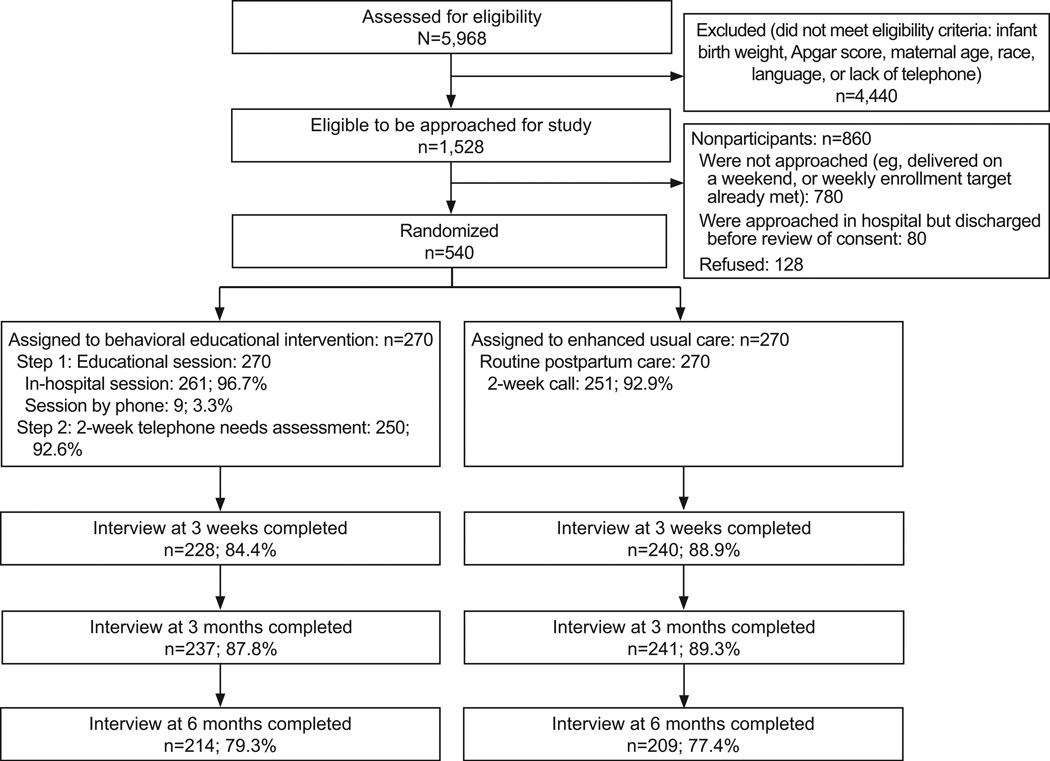
Of the 5,968 deliveries over the study period, 1,528 (25.6%) met the initial eligibility criteria (i.e. were black or Latina, 18 or greater, etc.). A total of 668 (43.7%) of the 1528 eligible mothers were approached in hospital and reviewed the study consent form. Of the 668 mothers, 540 (80.8%) completed the consent process and were enrolled in the trial and 128 (19.2%) mothers declined to participate. (Figure 1) There were no significant differences between those who consented or declined in mean age, insurance status, primary language, or delivery route. Latina mothers were more likely to decline (p<.05) than black mothers. Of the 270 mothers randomized to the intervention arm, 261 received the intervention in hospital though 9 mothers were discharged before the social worker could meet with them. Those 9 patients were sent the education materials and the social worker reviewed the educational materials over the phone. Ninety-three percent (250/270) of the intervention group and 93% (251/270) of the control group were successfully reached for the 2-week calls. Of the 540 enrolled patients, 9 patients withdrew over the 6-month study period. Completion rates for the follow-up interviews were 87% (468/540) at 3-weeks, 89% (478/540) at 3-months, and 78% (423/540) at 6-months. Follow-up was equivalent for intervention and control at 3-weeks (84.4% vs. 88.9%, p=.09), 3-months (87.8% vs. 89.3%, p=.59) and 6-months postpartum (79.3% vs. 77.4%, p=.06). There were no baseline differences in rates of positive depression screens between women lost to follow-up verses those included in the analyses at 3-weeks (19% vs. 15%, p=.28), at 3 months (18% vs. 15%, p=.55), or at 6-months (18% vs. 14%, p=.35).
Figure 1.
Participants' flow through study
The overall mean age of enrolled participants was 28 (range 18–46); 62% were Latina and 38% were black, 63% had Medicaid insurance, 56% earned ≤ $30,000 annually, 35% were foreign born, and 21% spoke Spanish as their primary language. Baseline characteristics of the intervention and control groups are described in Table 1. There were no clinically important differences between the two groups at baseline except that comorbid conditions were more prevalent among the controls than intervention group (27% vs. 20%, p=.05). The mean EPDS scores at baseline were 4.2 (SD 4.6) in the intervention group and 4.5 (SD 4.9) in the control group. Forty-five mothers (20 in the intervention group and 25 in the control group) had high levels of depressive symptoms at baseline and were referred for psychiatric assessment / possible treatment while in the hospital.
Table 1.
Demographic and Clinical Characteristics of Study Participants
| Behavioral Educational Intervention (n=270) |
Enhanced Usual Care (n=270) |
P | |
|---|---|---|---|
| Demographic Characteristics | |||
| Age, mean (SD), y | 28 (6) | 27 (6) | 0.10 |
| Race, n (%) | 0.44 | ||
| Black or African American | 97 (36) | 106 (39) | |
| Hispanic or Latina | 173 (64) | 164 (61) | |
| Birthplace, n (%) | 0.41 | ||
| U.S.-born | 169 (63) | 178 (66) | |
| Foreign-born | 101(37) | 92 (34) | |
| Hispanic ethnicity, n (%) | 0.49 | ||
| Puerto Rican | 57 (21) | 60 (22) | |
| Dominican | 28 (10) | 25 (9) | |
| Mexican or Chicano | 38 (14) | 41 (15) | |
| Cuban | 0 (0) | 2 (1) | |
| Other | 43 (16) | 34 (13) | |
| Language, n (%) | 0.45 | ||
| English | 210 (78) | 217 (80) | |
| Spanish | 60 (22) | 53 (20) | |
| Education, n (%) | 0.46 | ||
| Less than High School | 58 (21) | 61 (22) | |
| High School | 59 (22) | 70 (26) | |
| Some college or technical school | 83 (31) | 83 (31) | |
| College graduate | 70 (26) | 56 (21) | |
| Insurance, n (%) | 0.87 | ||
| Medicaid or Medicaid managed care | 183 (69) | 184 (70) | |
| Private or other | 81 (31) | 79 (30) | |
| Marital status, n (%) | 0.85 | ||
| Single, separated, divorced, or widowed | 102 (38) | 104 (39) | |
| Marriedor living as if married | 168 (62) | 166 (61) | |
| Parity, n (%) | 0.70 | ||
| Primiparous | 107 (41) | 113 (42) | |
| Multiparous | 156 (59) | 154 (58) | |
| Breastfeeding, n (%) | 0.51 | ||
| Yes | 213 (79) | 206 (77) | |
| No | 57 (21) | 63 (23) | |
| Clinical characteristics Delivery type, n (%) | 0.83 | ||
| Cesarean | 105 (39) | 103 (38) | |
| Vaginal | 164 (61) | 167 (62) | |
| Comorbid condition, n (%) | 0.05 | ||
| Yes | 53 (20) | 72 (27) | |
| No | 217 (80) | 197 (73) | |
| Antepartum complication, n (%) | 0.52 | ||
| Yes | 65 (24) | 59 (22) | |
| No | 203 (76) | 210 (78) | |
| Past history of depression, n (%) | 0.43 | ||
| Yes | 42 (16) | 49 (18) | |
| No | 227 (84) | 221 (82) | |
| Treatment for depression this pregnancy, n (%) | 0.45 | ||
| Yes | 7 (3) | 10 (4) | |
| No | 263 (97) | 260 (96) | |
| Positive baseline depression screen (Edinburgh Postnatal Depression Scale score of 10 or higher), n (%) | 0.34 | ||
| Yes | 37 (14) | 45 (17) | |
| No | 233 (86) | 225 (83) |
SD, standard deviation.
In the intention-to-treat analysis (N=540) mothers in the intervention arm were less likely to screen positive for depression than mothers in the control arm: at 3 weeks 8.8% (20/227) vs. 15.3% (37/242), p=.03 respectively; at 3-months 8.4% (20/237) vs. 13.2% (32/242), p=.09 respectively; and at 6-months 8.9% (19/214) vs.13.7%, p=.11, respectively. Repeated measure analysis showed that the intervention was protective against a positive depression screen for up to 6-months of follow up (OR of 0.67; 95% CI: 0.47–0.97; number needed to treat of 16; 95% CI: 9–112).
Subgroup analyses were planned to estimate the effect of the intervention on mothers not referred for baseline psychiatric assessment/treatment as this intervention was aimed at prevention not treatment of mothers with severe depressive symptoms. Analyses of the 495 mothers who did not receive an additional psychiatric intervention at baseline showed that mothers in the intervention arm were less likely to screen positive for depression than mothers in the control arm at 3-weeks (7.1% vs. 14.4%, p=.01), 3-months (6.3% vs. 11.4%, p=.058) and 6-months (7.5% vs.13.1%, p=.068). See Table 2. In multivariable analyses controlling for baseline depression scores, past history of depression, country of birth, language, social support, and presence of comorbid clinical condition, mothers in the intervention arm vs. controls were less likely to screen positive for depression at 3-weeks, adjusted OR= 0.37 (95% CI 0.17 – 0.79), at 3-months, adjusted OR=0.45 (0.21–0.92), and at 6-months, adjusted OR= 0.51 (0.24–1.07). Repeated measure analysis showed that the intervention was protective against a positive depression screen score for up to 6-months of follow up (OR of 0.57; 95% CI: 0.37–0.88) among mothers not referred for psychiatric intervention at baseline.
Table 2.
Subgroup Analyses for Mothers Without Severe Baseline Depressive Symptoms at Baseline (n=495).
| Postpartum Follow-up |
Odds Ratio for Positive Depression Screen Intervention Compared With Enhanced Usual Care |
|
|---|---|---|
| Unadjusted Odds Ratio (95% CI) |
Adjusted Odds Ratio* (95% CI) |
|
| 3 Weeks | 0.45 (0.24–0.86) | 0.37 (0.17–0.79) |
| 3 Months | 0.52 (0.26–1.03) | 0.45 (0.21–0.92) |
| 6 Months | 0.54 (0.27–1.06) | 0.51 (0.24–1.07) |
| Longitudinal Analysis† | 0.57 (0.37–0.88) | |
Multivariable models also included baseline positive depression screen, country of birth, language, comorbid condition, past depression history, and social support.
Repeated measures analysis: adjusted for baseline depression screen.
Among the 45 mothers referred for psychiatric assessment/treatment at baseline there was no significant difference between intervention and control in rates of positive depression screens at 3-weeks, 3-months, and at 6-months postpartum.
DISCUSSION
The results of this trial suggest that a behaviorally focused, educational intervention, delivered in the obstetric setting, has the potential to reduce the likelihood of a positive depression screen among black and Latina mothers. Our intervention, designed to address modifiable, situational factors for the prevention of postpartum depression, was successful in buffering the occurrence of such symptoms; both intent-to-treat analysis and subgroup analysis of mothers not referred for psychiatric intervention at baseline demonstrated that mothers randomly assigned to the intervention were less likely to screen positive for depression during the six-month follow-up period than mothers in enhanced usual care. We believe the significantly lower odds of reporting symptoms indicating a positive screen for depression during the six months of follow-up as compared with controls is clinically important as many of the detrimental effects of postpartum depression impact mothers, infants, and families during this crucial period. Given our success in recruiting 540 black and Latina mothers with only a 19% refusal rate, our results are likely representative for mothers from similar racial and socio-economic backgrounds.
The effect of our intervention appeared somewhat stronger among the 495 mothers not referred for psychiatric assessment and possible treatment at baseline. As the intervention was designed to prevent and not to treat depressive symptoms and those referred were given a potentially stronger personalized assessment/treatment, a behavioral education intervention was unlikely to provide added benefit. For ethical reasons we decided to continue to include, assess and refer for formal assessment and treatment any mother who exceeded the highest cut point (EPDS score of 13 or higher, a PHQ-9 score of 20 or higher, or suicidal ideation) at any point in time. However our data do suggest that in settings where mothers are not screened prior to hospital discharge, the evidence suggests that this intervention shows promise for reducing positive depression screens in the early postpartum period.
Our results suggest that one can address and modify the factors that have been reported to be correlated with and hypothesized to elicit postpartum depressive symptoms.3, 15 Our intervention aimed to increase mother’s knowledge about specific triggers of postpartum depressive symptoms by presenting visual displays of the number of mothers likely to experience each symptom, providing simple “to do’s” to manage each symptom, and was followed by a visual display of the number of mothers likely to still experience these factors at 3 months. The visual representations made clear that these factors were “normal”, manageable with behavioral strategies and tactics, and likely remediated in a defined time frame. It also emphasized the importance of social support. Finally, specific instructions specified to call one’s physician in the event that symptoms did not resolve or worsened, and provided a list of existing health-related community services. Although our study is one of few trials that have successfully reduced postpartum depressive symptoms among black and Latina mothers, our results are consistent with a large Cochrane review which demonstrated that psychosocial interventions to prevent postpartum depression are more likely to be successful if they are individually based, initiated postnatal, and conducted by a health professional.31 Psycho-educational interventions may be especially helpful in the setting of prevention because they avoid some of the stigma associated with mental illness, which is of particular importance for many black and Latina communities.
There were limitations with this trial. First, the rate of positive depressive symptom screens was much lower than rates previously published in the literature on perinatal women of color.3, 32 Previous studies have rates as high as 50% depending on the screening instrument used and population studied.3, 4 Given that the prevalence of depressive symptoms was much lower than expected our power to detect a meaningful difference was extremely limited in this study. Despite the low prevalence of depressive symptoms in this patient sample, the intervention was found to be effective. Second, we used a depression screening instrument rather than a formal structured interview to diagnose depression. Our intervention was implemented in an obstetrics setting where formal assessments are often too burdensome to perform. Further, positive screens for depression, whether or not they are associated with diagnosis of major depressive disorder are associated with multiple negative outcomes for mothers and infants.3,5,13,32 And finally, our trial was implemented in one institution which limits the generalizability of our results. However, the institution serves a very racially, ethnically, and socioeconomically diverse population in a large urban city. Future research should examine the effect of this intervention more broadly (in multiple settings) and this intervention has the potential to be adapted to an outpatient setting.
A behavioral educational intervention, reviewed and modified by mothers and community members, delivered to black and Latina postpartum mothers successfully reduced the likelihood of a positive depression screen in a large urban hospital setting. This first step intervention focuses on educating and preparing mothers for postpartum experiences and increasing their ability to cope with postpartum demands. Although this intervention does not replace treatment for major depression and may be of limited benefit for those with major depression, it successfully reduced positive postpartum depression screens among low-income mothers of color in this study. It is important to note that the effect during the first six-months postpartum would likely benefit infant, mother, and family.
Acknowledgments
Supported by the National Institute for Minority Health and Health Disparities (5P60MD000270-10) and the National Institute for Mental Health (5R01MH77683-2).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: Pfizer supplies medication for an NIH-funded study on the treatment of postpartum depression which is led by Dr. Zlotnick. The other authors did not report any potential conflicts of interest.
Presented at Society of General Internal Medicine 34th Annual Meeting, May 4-7, 2011, Phoenix, Arizona.
REFERENCES
- 1.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S. Births: final data for 2004. Natl Vital Stat Rep. 2006 Sep 29;55(1):1–101. [PubMed] [Google Scholar]
- 2.Gaynes BN, Meltzer-Brody S, Lohr KN, et al. Perinatal Depression: Prevalence, Screening Accuracy, and Screening Outcomes. Paper presented at: AHRQ Publication No. 05-E006-2; February 2005; Rockville. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol. 2005 Jun;105(6):1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zayas LH, Cunningham M, McKee MD, Jankowski KR. Depression and Negative Life Events Among Pregnant African-American and Hispanic Women. Women's Health Issues. 2002;12(1):16–21. doi: 10.1016/s1049-3867(01)00138-4. [DOI] [PubMed] [Google Scholar]
- 5.McKee MD, Cunningham M, Jankowski KR, Zayas L. Health-related functional status in pregnancy: relationship to depression and social support in a multi-ethnic population. Obstet Gynecol. 2001 Jun;97(6):988–993. doi: 10.1016/s0029-7844(01)01377-1. [DOI] [PubMed] [Google Scholar]
- 6.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cogill SR, Caplan HL, Alexandra H, Robson KM, Kumar R. Impact of maternal postnatal depression on cognitive development of young children. Br Med J (Clin Res Ed) 1986 May 3;292(6529):1165–1167. doi: 10.1136/bmj.292.6529.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Field T, Healy B, Goldstein S, et al. Infants of depressed mothers show "depressed" behavior even with nondepressed adults. Child Dev. 1988 Dec;59(6):1569–1579. doi: 10.1111/j.1467-8624.1988.tb03684.x. [DOI] [PubMed] [Google Scholar]
- 9.Field T. Maternal depression effects on infants and early interventions. Prev Med. 1998 Mar-Apr;27(2):200–203. doi: 10.1006/pmed.1998.0293. [DOI] [PubMed] [Google Scholar]
- 10.Righetti-Veltema M, Bousquet A, Manzano J. Impact of postpartum depressive symptoms on mother and her 18-month-old infant. Eur Child Adolesc Psychiatry. 2003 Apr;12(2):75–83. doi: 10.1007/s00787-003-0311-9. [DOI] [PubMed] [Google Scholar]
- 11.Lewis-Fernandez R, Das AK, Alfonso C, Weissman MM, Olfson M. Depression in US Hispanics: diagnostic and management considerations in family practice. J Am Board Fam Pract. 2005 Jul-Aug;18(4):282–296. doi: 10.3122/jabfm.18.4.282. [DOI] [PubMed] [Google Scholar]
- 12.Das AK, Olfson M, McCurtis HL, Weissman MM. Depression in African Americans: breaking barriers to detection and treatment. J Fam Pract. 2006 Jan;55(1):30–39. [PubMed] [Google Scholar]
- 13.Howell EA, Mora PA, DiBonaventura MD, Leventhal H. Modifiable factors associated with changes in postpartum depressive symptoms. Arch Womens Ment Health. 2009 Apr;12(2):113–120. doi: 10.1007/s00737-009-0056-7. [DOI] [PubMed] [Google Scholar]
- 14.Howell EA, Mora PA, Chassin MR, Leventhal H. Lack of preparation, physical health after childbirth, and early postpartum depressive symptoms. J Womens Health (Larchmt) 2010 Apr;19(4):703–708. doi: 10.1089/jwh.2008.1338. [DOI] [PubMed] [Google Scholar]
- 15.Howell EA, Mora P, Leventhal H. Correlates of early postpartum depressive symptoms. Matern Child Health J. 2006 Mar;10(2):149–157. doi: 10.1007/s10995-006-0116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987 Jun;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 17.Eberhard-Gran M, Eskild A, Tambs K, Opjordsmoen S, Samuelsen SO. Review of validation studies of the Edinburgh Postnatal Depression Scale. Acta Psychiatr Scand. 2001 Oct;104(4):243–249. doi: 10.1034/j.1600-0447.2001.00187.x. [DOI] [PubMed] [Google Scholar]
- 18.Eberhard-Gran M, Eskild A, Tambs K, Schei B, Opjordsmoen S. The Edinburgh Postnatal Depression Scale: validation in a Norwegian community sample. Nord J Psychiatry. 2001;55(2):113–117. doi: 10.1080/08039480151108525. [DOI] [PubMed] [Google Scholar]
- 19.Harris B, Huckle P, Thomas R, Johns S, Fung H. The use of rating scales to identify post-natal depression. Br J Psychiatry. 1989 Jun;154:813–817. doi: 10.1192/bjp.154.6.813. [DOI] [PubMed] [Google Scholar]
- 20.Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. Br J Psychiatry. 1990 Aug;157:288–290. doi: 10.1192/bjp.157.2.288. [DOI] [PubMed] [Google Scholar]
- 21.Boyce P, Stubbs J, Todd A. The Edinburgh Postnatal Depression Scale: validation for an Australian sample. Aust N Z J Psychiatry. 1993 Sep;27(3):472–476. doi: 10.3109/00048679309075805. [DOI] [PubMed] [Google Scholar]
- 22.Lundh W, Gyllang C. Use of the Edinburgh Postnatal Depression Scale in some Swedish child health care centres. Scand J Caring Sci. 1993;7(3):149–154. doi: 10.1111/j.1471-6712.1993.tb00190.x. [DOI] [PubMed] [Google Scholar]
- 23.Jadresic E, Araya R, Jara C. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Chilean postpartum women. J Psychosom Obstet Gynaecol. 1995 Dec;16(4):187–191. doi: 10.3109/01674829509024468. [DOI] [PubMed] [Google Scholar]
- 24.Zelkowitz P, Milet TH. Screening for post-partum depression in a community sample. Can J Psychiatry. 1995 Mar;40(2):80–86. doi: 10.1177/070674379504000205. [DOI] [PubMed] [Google Scholar]
- 25.Wickberg B, Hwang CP. The Edinburgh Postnatal Depression Scale: validation on a Swedish community sample. Acta Psychiatr Scand. 1996 Sep;94(3):181–184. doi: 10.1111/j.1600-0447.1996.tb09845.x. [DOI] [PubMed] [Google Scholar]
- 26.Areias ME, Kumar R, Barros H, Figueiredo E. Comparative incidence of depression in women and men, during pregnancy and after childbirth. Validation of the Edinburgh Postnatal Depression Scale in Portuguese mothers. Br J Psychiatry. 1996 Jul;169(1):30–35. doi: 10.1192/bjp.169.1.30. [DOI] [PubMed] [Google Scholar]
- 27.Ghubash R, Abou-Saleh MT, Daradkeh TK. The validity of the Arabic Edinburgh Postnatal Depression Scale. Soc Psychiatry Psychiatr Epidemiol. 1997 Nov;32(8):474–476. doi: 10.1007/BF00789142. [DOI] [PubMed] [Google Scholar]
- 28.Carpiniello B, Pariante CM, Serri F, Costa G, Carta MG. Validation of the Edinburgh Postnatal Depression Scale in Italy. J Psychosom Obstet Gynaecol. 1997 Dec;18(4):280–285. doi: 10.3109/01674829709080700. [DOI] [PubMed] [Google Scholar]
- 29.Lawrie TA, Hofmeyr GJ, de Jager M, Berk M. Validation of the Edinburgh Postnatal Depression Scale on a cohort of South African women. S Afr Med J. 1998 Oct;88(10):1340–1344. [PubMed] [Google Scholar]
- 30.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: J. Wiley & Sons; 1987. [Google Scholar]
- 31.Dennis CL, Creedy D. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2004;(4):CD001134. doi: 10.1002/14651858.CD001134.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Seguin L, Potvin L, St-Denis M, Loiselle J. Depressive symptoms in the late postpartum among low socioeconomic status women. Birth. 1999 Sep;26(3):157–163. doi: 10.1046/j.1523-536x.1999.00157.x. [DOI] [PubMed] [Google Scholar]