Abstract
Background
Little information is available on factors that predict adherence to patching in infants. We evaluated data from the Infant Aphakia Treatment Study (IATS), a randomized clinical trial of treatment for infants with unilateral congenital cataracts, to investigate factors associated with successful adherence to patching protocols.
Subjects and Methods
In the IATS, patching was prescribed 1 hour daily per month of age until 8 months of age and 50% of waking hours thereafter. A centrally located staff member inquired about adherence to patching in a phone interview with the primary caregiver. Analyses used χ2 tests of independence and logistic regression to identify predictors of reported adherence and of achieving adherence rates of at least 75% (“good”) and 90% (“excellent”).
Results
A total of 104 caregivers provided data on patching 3 months after surgery, at which time 60% reported patching at least 75% of the prescribed time. Reported adherence was not associated with the type of treatment (P = 0.73) but was better in children with private insurance (P = 0.01) and for children with mothers reporting lower levels of parenting stress (P = 0.03).
Conclusions
Most caregivers reported being able to adhere to prescribed patching shortly after extraction of a unilateral congenital cataract. The type of correction (IOL vs contact lens) was not associated with the amount of patching achieved, whereas family socioeconomic status and maternal stress appeared to play a role.
Children born with visually significant unilateral congenital cataracts often have poor visual outcomes. Previous reports have suggested that achieving good visual outcome usually requires early surgical removal of the cataract,1–3 consistent visual correction of the aphakia or residual refractive error,4 and good adherence to a regimen of occlusion of the fellow eye.4, 5
Occlusion therapy is often difficult for caregivers.6, 5 Allen and colleagues2 reported that occlusion therapy was abandoned prior to 4 years of age in nearly one-third of children treated for unilateral cataract. Earlier studies reported that language barriers, parental education, and socioeconomic status7 were related to adherence to occlusion therapy in children with amblyopia. However, it is unclear to what extent these findings are applicable to occlusion therapy in infants because the amount of patching achieved by caregivers likely varies by the developmental level of the child and the depth of amblyopia.7 For example, in studies of preschool-aged children, it is difficult to disentangle the effects of developmental level, degree of amblyopia, and caregiver characteristics on patching in children with long-standing amblyopia. In contrast, adherence to patching in infancy relies primarily on the caregiver since infants are less able to resist occlusion or to remove the patch themselves.
The Infant Aphakia Treatment Study (IATS) presented an opportunity to identify factors that affect patching shortly after cataract surgery, early in the first year of life, when caregiver characteristics are most likely to influence adherence and when child behavior and differences in vision are least likely to play a substantial role. The IATS is a multicenter, randomized, controlled clinical trial comparing intraocular lens (IOL) to contact lens treatment after cataract surgery performed at 1 to 6 months of age in children with unilateral congenital cataract. We hypothesized that IOL, higher socioeconomic status, and lower levels of parenting stress would be associated with better adherence to patching.
Subjects and Methods
The overall design of the IATS and results of the visual acuity assessment at 12 months of age have previously been published.8, 9 The study was approved by the Institutional Review Boards of all participating institutions and adhered to the tenets of the Declaration of Helsinki.
Prescribed Patching
Patching was prescribed for all patients throughout the first year of life. Starting the second week after cataract surgery, caregivers were instructed to have the child wear an adhesive occlusive patch over the fellow eye 1 hour daily per month of age until the child was 8 months old. Thereafter, caregivers were told to patch their child 50% of waking hours. Patches were provided to patients at no cost to minimize financial barriers to patching. Deviations from prescribed patching protocols, both over- and underpatching, were not considered to be protocol violations.
Adherence to the patching regimen was assessed every 3 months starting 3 months after surgery. A trained interviewer from the Data Coordinating Center completed a 48-hour recall interview with the primary caregiver. The timing of the interview was determined using an algorithm that distributed the preferred day of the call evenly throughout the week; caregivers were not informed in advance about the specific day or times of the interview. The semistructured interview elicited specific information about the times the child was asleep, the times spectacles or contact lenses were worn, and the times that the child’s fellow eye was occluded. The interviews were conducted by one of three trained interviewers (one English-speaking, one Spanish-speaking, and one Portuguese-speaking) in the caregiver’s primary language so that the caregiver was interviewed by the same person on each occasion. The vast majority (>95%) were performed by the English-speaking interviewer. Although data on adherence were collected at multiple time points, the current analysis reports data collected at the first of these interviews, which was conducted 3 months after surgery. Data from the second interview, 6 months after surgery, is also presented to confirm the relationships observed using data collected 3 months earlier.
Measures of adherence were derived from caregivers’ reports of the times that the child wore a patch. We used this information to calculate the percentage of prescribed patching that was achieved, calculated as the number of waking hours during which the patch was worn divided by the number of waking hours patching was prescribed (ie, age in months for infants <8 months of age or 50% of waking hours for older infants). We also developed two dichotomous measures of adherence: good and excellent adherence, since predictors of adherence might influence the shape of the distribution without influencing the overall mean. Good adherence to prescribed occlusion therapy was defined as a parental report of at least 75% of prescribed patching. This definition is consistent with definitions used in other clinical trials.10, 11 We defined excellent patching as reportedly achieving at least 90% of prescribed patching.
Predictors of Patching Adherence
Children were randomly assigned to receive either an IOL at the time of extraction or to remain aphakic. Contact lenses were prescribed for aphakic children and spectacles were prescribed to correct any residual refractive error in pseudophakic children. Age at cataract extraction was categorized as 28–48 days, 49 days to 3 months, or 3 months plus 1 day to <7 months. Total parenting stress, stressful life events, and maternal education (less than a high school diploma, high school diploma or GED, education beyond high school) were obtained from the Parenting Stress Index (PSI),12 which was administered, along with the Ocular Treatment Index,13 as a Caregiver Questionnaire, at the 3 months’ postoperative visit. The total stress score was comprised of stress related to both parent and child characteristics. It included child characteristics such as distractibility, adaptability, mood, and the degree to which the child was demanding and reinforced the parent. Parent characteristics included competence, isolation, depression, and spousal support. The life stress score represented situational stress that was beyond caregiver control. The stress measures were each categorized into three approximately equal groups to create a comparison of those with the lowest, middle and highest levels of reported stress. For the majority of caregivers, parenting stress levels reported were within the normal range; only 11 (10.1%) caregivers reported stress levels in the top 15% of population norms. Race (white vs other), ethnicity (Hispanic vs other), child’s sex and the availability of private insurance at entrance to the study were obtained from data collected at the first visit.
Analytic Methods
Analyses were conducted using SAS 9.1 (SAS Institute Inc, Cary, NC) and SPSS 17.0 (SPSS Inc, Chicago, IL) statistical packages. We used t tests, one-way ANOVAs, and linear regression to identify factors that affected percentage of prescribed patching as reported by caregivers. We used χ2 tests of independence and logistic regression to identify factors that predicted good and excellent adherence to prescribed occlusion therapy. Statistical significance was defined at α = 0.05. Forward stepwise linear and logistic regression were used for multivariate modeling; variables significant at P = 0.05 were entered into the model. For the subgroup of caregivers whose children had a 6-month adherence interview prior to having their visual acuity assessed at 12 months of age, we repeated the analyses to confirm our findings.
Results
A total of 114 children and their families participated in the IATS study. Participation rates have been previously described.9 Complete data on adherence to patching and potential predictors were available 3 months after surgery for 104 children: 5 of the 114 were excluded because the adherence interview was not completed, 4 because the caregiver did not complete the PSI, 1 because too many items were left blank to accurately compute a total stress scale on the PSI.
More than 40% (n = 48) of the children were under 5 months of age at the time the information on adherence was obtained 3 months after surgery; two-thirds (65.4%) were under 6 months of age. The oldest child was 10 months of age (Table 1). Thus most of the children were neither walking nor talking.
Table 1.
Age at 3 months' postsurgical adherence interview
| Age in months | N | % |
|---|---|---|
| <5 | 48 | 46.2 |
| 5 | 20 | 19.2 |
| 6 | 15 | 14.4 |
| 7 | 6 | 5.8 |
| 8 | 9 | 8.6 |
| >8 | 6 | 5.7 |
| Total | 104 |
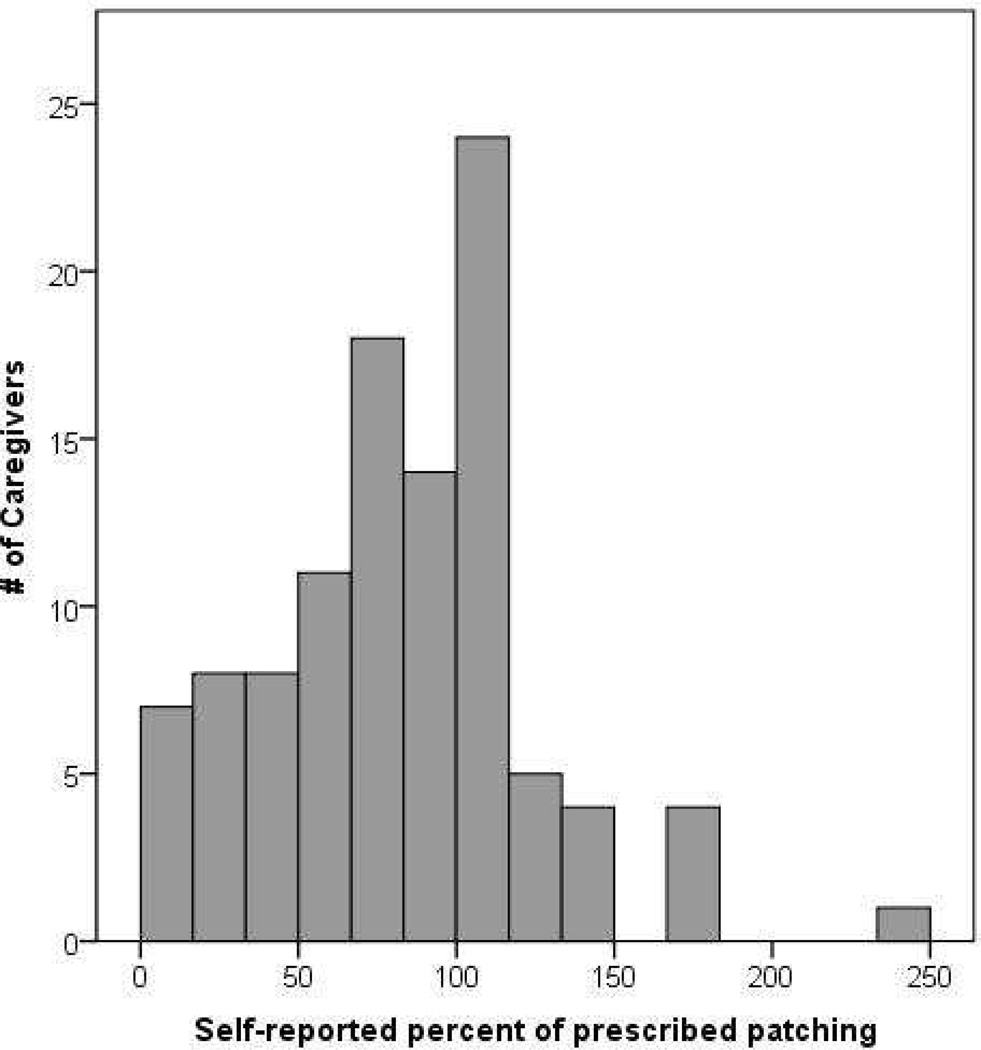
Overall, caregivers reported achieving the majority of prescribed patching (Figure 1). Three months after surgery, 60%% (n = 62) of parents reported achieving at least 75% of prescribed patching; nearly half (n = 49) reported achieving at least 90%. The median amount of patching reported was 85% and the mean was 82%. Only 3 caregivers reported no patching at all.
FIG 1.
Distribution of percent of prescribed patching reported by caregivers of IATS patients 3 months after cataract surgery. The mean self-reported percentage of prescribed patching was 82.5 ± 42.9%.
Adherence to patching 3 months after surgery was similar in children who received an IOL and those who remained aphakic (Table 2). Caregivers with higher socioeconomic status, measured as higher maternal education and availability of private insurance, were more likely to adhere to patching 3 months after surgery than were other parents. Caregivers reporting the lowest levels of total parenting stress also reported achieving the highest percentage of prescribed patching and total parenting stress was weakly correlated (r = −0.22; 95% CI, −0.48 to 0.03) with the proportion of prescribed patching that caregivers reported achieving, accounting for about 4% of the observed variance in reported adherence to prescribed patching. Neither life stress (r = −0.11, P = 0.26) nor age at surgery (measured in days) (r = −0.07, P = 0.48) were associated with adherence to prescribed patching. Although the mean adherence to patching did not differ by age at surgery, children who were older at the time of surgery were less likely to be patched at least 90% of the prescribed time than were those who were younger when the cataract was removed. Additionally, parents reporting the lowest levels of parenting stress and life stress reported more patching and were more likely to report achieving at least 90% of prescribed patching than were caregivers reporting greater amounts of stress.
Table 1.
Relationships among treatment, demographic characteristics and stress levels and adherence to patching 3 months after cataract extraction
| Variable | N | % of prescribed patching | Prescribed patching | |||
|---|---|---|---|---|---|---|
| ≥75% | ≥90% | |||||
| Mean ± SD | P valuea | |||||
| Overall | 104 | 82.5 ± 42.9 | 60% | 47% | ||
| Treatment | IOL | 51 | 81.0 ± 47.9 | 0.73 | 57% | 45% |
| CL | 53 | 84.0 ± 37.9 | 62% | 49% | ||
| Age at surgery | 28 to 48 days | 46 | 91.0 ± 47.9 | 0.18 | 63% | 61% |
| 49 days to 3.0 months | 30 | 78.4 ± 36.6 | 60% | 47% | ||
| 3.1 to <7 months | 28 | 73.1 ± 38.9 | 54% | 25% | ||
| Sex | Male | 50 | 76.9 ± 48.0 | 0.20 | 48% | 38% |
| Female | 54 | 87.8 ± 37.2 | 70% | 56% | ||
| Race | White | 89 | 80.55 ± 41.8 | 0.25 | 64% | 54% |
| Other | 16 | 93.74 ± 46.8 | 58% | 45% | ||
| Hispanic | Yes | 15 | 85.6 ± 59.6 | 0.77 | 61% | 48% |
| No | 89 | 82.0 ± 39.8 | 53% | 40% | ||
| Insurance | Private | 64 | 90.6 ± 39.4b | 0.01 | 69%b | 56%b |
| Other | 40 | 69.6 ± 45.5 | 45% | 33% | ||
| Maternal | <High school | 10 | 60.1 ± 41.2 | 0.07 | 30%b | 20%b |
| education | High school grad | 23 | 79.7 ± 48.1 | 52% | 39% | |
| Some college | 41 | 78.7 ± 41.1 | 62% | 45% | ||
| College grad | 29 | 98.0 ± 38.3 | 72% | 66% | ||
| Parenting stress | Lowest third | 37 | 97.1 ± 43.4b | 0.03 | 73% | 65% |
| Middle third | 33 | 75.9 ± 38.4 | 52% | 36% | ||
| Highest third | 34 | 73.1 ± 43.4 | 53% | 38% | ||
| Life stress | Lowest third | 39 | 91.2 ± 40.47 | 0.06 | 69% | 56% |
| Middle third | 33 | 68.2 ± 36.9 | 49% | 39% | ||
| Highest third | 32 | 86.7 ± 48.4 | 59% | 44% | ||
CL, contact lens; IOL, intraocular lens
t test or ANOVA for % of prescribed patching, Χ2 test of independence or gamma for achieving >75% and >90 prescribed patching.
P < 0.05.
We conducted stepwise linear and logistic regression models to identify factors that continued to be associated with adherence while simultaneously adjusting for other potential predictors of adherence. The availability of private insurance (P = 0.01) was associated with an average increase of 21% in percentage of prescribed patching that caregivers reported achieving. Additionally, children whose parents had private insurance had more than twice the likelihood of achieving at least 75% of prescribed patching (OR, 2.5; 95% CI, 1.1–5.7). Parents of boys were less likely than parents of girls to achieve this level of patching (OR, 0.4; 95% CI 0.2–1.0). Older age at surgery (OR = 2.8; 95% CI, 0.9–9.2 for age >3 months versus age <49 days), not having private insurance (OR = 2.7; 95% CI, 1.1–6.5) and higher levels of parenting stress (OR, 0.4; 95% CI, 0.1–1.0 for parents reporting the highest levels of stress relative to those reporting the lowest stress levels) were associated with a reduced likelihood of achieving at least 90% of prescribed patching.
Adherence was assessed in 96 infants 6 months after surgery. An adherence interview was conducted 6 months after surgery with caregivers of another 15 children, but these data were not included because the interview took place after the visual acuity assessment at 12 months of age. The median amount of patching reported 6 months after surgery was 77%. More than one-third (37.5%) of caregivers reported achieving at least 90% of prescribed patching; nine caregivers reported no patching at this time.
In a linear regression model, higher levels of parenting stress reported three months after surgery (β = −0.3; 95% CI, 0.6–0.0; P < 0.01) were associated with poorer adherence to patching 6 months after surgery and parents of white children reported an average of 27% more patching than parents of nonwhite children (95% CI, 42.3–7.1). Similarly, in a logistic regression model, parents of nonwhite children were 22% as likely to report achieving at least 75% of prescribed patching (OR, −0.22; 95% CI, 0.7–0.8) as white children, and parents reporting the medium (OR, 0.3; 95% CI, 0.1–1.0) and the highest levels of life stress (OR, 0.3; 95% CI, 0.1–0.9) were less likely to report achieving at least 90% of prescribed patching 6 months after surgery as parents reporting the lowest levels of life stress. Having private insurance was not significantly associated with adherence 6 months after surgery.
Discussion
Although a number of studies have reported on adherence to patching in children, few data are available to help clinicians predict adherence to patching regimens in infants treated for congenital cataracts. It is likely that caregivers’ characteristics play an enhanced role in determining adherence to occlusion therapy in infancy since babies are less able to resist patching than older children.
Although there was substantial variation in the amount of patching reported by caregivers three months after surgery the majority of caregivers in the IATS trial were able to adhere to prescribed patching during this time period. These findings are inconsistent with other studies of adherence to occlusion therapy in young children that suggest many caregivers are unable to achieve a high degree of adherence to occlusion therapy (Loudon SE, Felius J, Simonsz B, et al. Quality of life of children treated with occlusion therapy for amblyopia. IOVS 2005;46:E-Abstract 3596).7, 14 However, Norman and colleagues15 found that parents of amblyopic patients aged 1–8 years reported achieving about three-quarters of the prescribed patching.
It is possible that the high degree of adherence in IATS patients related to the support for patching provided by the study to caregivers. This support included monthly phone calls and financial support for the patches. It is also possible that parents of infants with unilateral cataract were more motivated to patch than parents of older children with amblyopia because the condition was perceived as more serious and/or the treatment perceived as more efficacious than that in older children. Unfortunately, data were not available to assess the perceived efficacy of treatment in this group. Additionally, most of the earlier results on adherence to patching are among preschool-aged children who may be more able to remove patches than infants. Results reported by Chua and colleauges16 that adherence to patching was higher in children < 15 months of age support this idea. We suspect that as the IATS population matures, adherence to patching will decrease and approach levels of patching reported in earlier studies.
Although the average amount of patching did not differ significantly by age at surgery, earlier surgical removal of the cataract was associated with achieving at least 90% of the prescribed patching 3 months after surgery. It is possible that this is an artifact related to the protocol that prescribed more patching in the first few months of surgery among children treated at older ages. There is some evidence to support this notion since 6 months after surgery, a time when nearly all infants were of an age at which patching for 50% of waking hours, the age at surgery was unrelated (r = 0.10, P = 0.35) to adherence. However, it may also relate to the fact that older infants are more able to resist efforts at patching16 and/or the possibility that older children may have a greater degree of amblyopia resulting from a longer period of visual deprivation. Some support for the latter explanation is provided by Loudon et al who noted that adherence with occlusion therapy was poorer in children with more severe amblyopia.7
Earlier studies reported that language barriers, parental education and socioeconomic status7, 17, 18 were related to adherence to occlusion therapy in children with amblyopia. Our analysis failed to support a relationship between adherence to prescribed patching three months after surgery and either ethnicity or race but did observe that that caregivers with access to private health insurance reported being more adherent than other caregivers. Further, race was associated with adherence to patching 6 months after surgery. We believe that these findings reflect an effect of socioeconomic status, since the study contributed financially to the treatment costs for all participants, including physician fees when necessary. It is not clear what aspect of socioeconomic status (eg, health literacy, family support, access to care, etc) may influence adherence to patching. However, this finding supports earlier suggestions that it is important to educate caregivers on the importance of occlusion in a way that is understandable to them,6, 7, 15, 17 and to inquire about financial barriers that may interfere with optimal patching adherence.
We focused our analyses on the period shortly after surgery and when most children were neither talking nor walking to provide the cleanest estimate of the caregiver’s role in adhering to prescribed patching. However, we do not suggest that we have examined the effect of all possible caregiver characteristics; nor can we rule out the possibility that the child’s temperament plays a role.
We found evidence to support the hypothesized association between caregiver stress, as measured by the PSI, and adherence to the prescribed patching regimen. However, the directionality of the association between adherence and parenting stress is unclear because stress was reported around the time of the three month 48-hour telephone interview. It is possible that parenting stress influenced the amount of patching achieved by caregivers, but it is also possible that caregivers who found it difficult to patch had increased levels of stress as a result of this difficulty. The observed association may also result from a combination of these two effects. One earlier study found that patching did not produce psychological distress among caregivers, but other studies have found measures of caregiver stress to be associated with patching in children with amblyopia.15, 17 We chose not to assess parenting stress at study enrollment or at the time of surgery because we believed that the stress of receiving a diagnosis of unilateral congenital cataract, processing the information and the needed treatments, and of coping with a young infant’s surgery would elevate parenting stress scores and therefore not reflect longer-term, chronic stress potentially predictive of patching.
We do not believe that the observed relationship between stress and adherence is attributable to confounding since parenting stress was not associated with age at surgery, sex, race, ethnicity, maternal education, or life stress. Parenting stress was associated with treatment, but treatment was not found to predict adherence. The availability of private insurance was associated with both treatment and parenting stress; however, both stress and private insurance were included in the linear regression models.
Some investigators support the use of electronic monitoring for adherence because of the possibility that caregivers may over-report adherence.14, 19 However, these devices are expensive and may not be acceptable to parents during infancy. Therefore, while we believe that our data are useful for identifying patterns of adherence to occlusion therapy in this group, we suggest caution in interpreting the specific percentages of time that caregivers report patching given concerns about possible over-reporting.
Our data suggest that most caregivers are able to adhere to prescribed patching shortly after extraction of a unilateral congenital cataract, that such adherence is unrelated to IOL implantation, and that parenting stress may be related to adherence to occlusion therapy in infancy.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
A complete listing of the Infant Aphakia Treatment Study Group is provided in e-Supplement 1, available at jaapos.org.
References
- 1.Frey T, Friendly D, Wyatt D. Re-evaluation of monocular cataracts in children. Am J Ophthalmol. 1973;76:381–388. doi: 10.1016/0002-9394(73)90495-9. [DOI] [PubMed] [Google Scholar]
- 2.Allen RJ, Speedwell L, Russell-Eggitt I. Long-term visual outcome after extraction of unilateral congenital cataracts. Eye (Lond) 2010;24:1263–1267. doi: 10.1038/eye.2009.295. [DOI] [PubMed] [Google Scholar]
- 3.Lambert SR, Lynn M, Drew-Botsch C, et al. Optotype acuity and re-operation rate after unilateral cataract surgery during the first 6 months of life with or without IOL implantation. Br J Ophthalmol. 2004;88:1387–1390. doi: 10.1136/bjo.2004.045609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen YC, Hu AC, Rosenbaum A, Spooner S, Weissman BA. Long-term results of early contact lens use in pediatric unilateral aphakia. Eye Contact Lens. 2010;36:19–25. doi: 10.1097/ICL.0b013e3181c6dfdc. [DOI] [PubMed] [Google Scholar]
- 5.Lundvall A, Kugelberg U. Outcome after treatment of congenital unilateral cataract. Acta Ophthalmol Scand. 2002;80:588–592. doi: 10.1034/j.1600-0420.2002.800606.x. [DOI] [PubMed] [Google Scholar]
- 6.Dixon-Woods M, Awan M, Gottlob I. Why is compliance with occlusion therapty for amblyopia so hard? A qualitative study. Arch Dis Child. 2006;91:491–494. doi: 10.1136/adc.2005.090373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loudon SE, Fronius M, Loman CW, et al. Predictors and a remedy for noncompliance with amblyopia therapy in children measured with the occlusion dose monitor. Invest Ophthalmol Vis Sci. 2006;47:4393–4400. doi: 10.1167/iovs.05-1428. [DOI] [PubMed] [Google Scholar]
- 8.Lambert SR, Buckley EG, Drews-Botsch C, et al. Infant Aphakia Treatment Study Group. A randomized clinical trial comparing contact lens with intraocular lens correction of monocular aphakia during infancy: Grating acuity and adverse events at age 1 year. Arch Ophthalmol. 2010;128:810–818. doi: 10.1001/archophthalmol.2010.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lambert SR, Buckley EG, Drews-Botsch C, et al. Infant Aphakia Treatment Study Group. The infant aphakia treatment study: Design and clinical measures at enrollment. Arch Ophthalmol. 2010;128:21–27. doi: 10.1001/archophthalmol.2009.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birch EE, Cheng C, Stager DR, Jr, Felius J. Visual acuity development after the implantation of unilateral intraocular lenses in infants and young children. J AAPOS. 2005;9:527–532. doi: 10.1016/j.jaapos.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Repka MX, Beck RW, Holmes JM, et al. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121:603–611. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 12.Abidin RR. Parenting Stress Index: Manual, Administration Booklet and Research Update. Charlottesville, VA: Pediatric Psychology Press; 1983. [Google Scholar]
- 13.Drews C, Celano M, Plager DA, Lambert SR. Parenting stress among caregivers of children with congenital cataracts. J AAPOS. 2003;7:244–250. doi: 10.1016/s1091-8531(03)00118-6. [DOI] [PubMed] [Google Scholar]
- 14.Awan M, Proudlock FA, Gottlob I. A randomized controlled trial of unilateral strabismic and mixed amblyopia using occlusion dose monitors to record compliance. Invest Ophthalmol Vis Sci. 2005;46:1435–1439. doi: 10.1167/iovs.04-0971. [DOI] [PubMed] [Google Scholar]
- 15.Norman P, Searle A, Harrad R, Vedhara K. Predicting adherence to eye patching in children with amblyopia: An application of protection motivation theory. Br J Health Psychol. 2003;8:67–82. doi: 10.1348/135910703762879219. [DOI] [PubMed] [Google Scholar]
- 16.Chua BEG, Johnson K, Martin F. A retrospective review of the associations between amblyopia type, patient age, treatment compliance and referral patterns. Clin Experiment Ophthalmol. 2004;32:175–179. doi: 10.1111/j.1442-9071.2004.00794.x. [DOI] [PubMed] [Google Scholar]
- 17.Loudon SE, Passchier J, Chaker L, et al. Psychological causes of non-compliance with electronically monitored occlusion therapy for amblyopia. Br J Ophthalmol. 2009;93:1499–1503. doi: 10.1136/bjo.2008.149815. [DOI] [PubMed] [Google Scholar]
- 18.Hudak DT, Magoon EH. Poverty predicts amblyopia treatment failure. J AAPOS. 1997;1:214–215. doi: 10.1016/s1091-8531(97)90040-9. [DOI] [PubMed] [Google Scholar]
- 19.Fielder AR, Irwin M, Auld R, Cocker KD, Jones HS, Moseley MJ. Compliance in amblyopia therapy: Objective monitoring of occlusion. Br J Ophthalmol. 1995;79:585–589. doi: 10.1136/bjo.79.6.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.