Abstract
Intimate partner violence (IPV) exposure was examined as a predictor of treatment engagement (i.e., starting and completing therapy) and treatment outcome in 150 women taking part in a dismantling study of cognitive processing therapy (CPT) for posttraumatic stress disorder (PTSD; Resick et al., 2008). Results indicate that women in a current intimate relationship with recent IPV (i.e., past year) were less likely to begin treatment relative to women who reported past IPV only or no history of IPV. For women who began treatment, IPV exposure was not predictive of whether or not they completed treatment. Among women who began treatment, the frequency of IPV was associated with treatment outcome such that women who experienced more frequent IPV exhibited larger reductions in PTSD and depression symptoms over the course of treatment, but experienced similar levels of PTSD and depression severity at the 6-month follow-up. Findings highlight the importance of targeting treatment engagement among women who report recent IPV and suggest that women who have experienced frequent IPV respond well to CPT treatment in spite of their IPV experiences.
Intimate partner violence (IPV) is a significant public health problem with estimates indicating that between 25 and 54% of women experience IPV in their adult lifetime (Thompson et al., 2006). In the United States, nearly 10% of women experience severe IPV victimization (hitting with a fist or object, beating up, threatening or assaulting with a weapon) at least once in their lifetime (Wilt & Olson, 1996). Approximately 2 million women are severely assaulted by their intimate partners each year (Riggs, Caulfield, & Street, 2000). IPV is associated with numerous short- and long-term mental health consequences, most commonly, posttraumatic stress disorder (PTSD) and depression (Jones, Hughes, & Unterstaller, 2001). PTSD and depression are often chronic in this population and can persist long after IPV has ended (Campbell & Soeken, 1999). As the recognition of IPV as a serious problem increases, more attention has been paid to cognitive–behavioral treatment development for IPV survivors (Iverson, Shenk, & Fruzzetti, 2009; Johnson & Zlotnick, 2006; Kubany, Hill, & Owens, 2003; Kubany et al., 2004). However, it is not well understood how exposure to IPV can impact women's engagement in and response to treatment. The current study examined IPV exposure as a predictor of treatment engagement and treatment outcome among women who had PTSD secondary to interpersonal victimization and were participating in a randomized controlled trial (RCT) of cognitive processing therapy (CPT; Resick et al., 2008).
CPT for PTSD is a cognitive therapy that was originally developed for female survivors of rape (Resick & Schnicke, 1992, 1993). It has been used to treat trauma survivors with complex clinical presentations and extensive comorbidities (e.g., Chard, 2005; Resick, Nishith, & Griffin, 2003; Resick et al., 2008). Although not specifically designed for female survivors of IPV, CPT has demonstrated efficacy for PTSD and depression following numerous forms of interpersonal victimization, including childhood physical and sexual assault and adulthood physical and sexual assault (Chard, 2005; Resick, Nishith, Weaver, Astin, & Feuer, 2002; Resick et al., 2008). CPT is also effective in reducing anger, dissociation, shame, guilt, and other symptoms that are common among female survivors of IPV (Resick et al., 2003, 2008). Therefore, CPT is an ideal treatment modality for exploring the role of IPV exposure in treatment engagement and outcome.
When predicting whether IPV exposure predicts women's ability to engage in PTSD treatment, as defined as starting and completing therapy, it is important to distinguish between women with recent IPV, past IPV, and those who have never experienced IPV. Women who are in a relationship with recent IPV may experience numerous obstacles that impact their ability to participate in and benefit from psychosocial treatment. Potential barriers to treatment engagement include safety concerns (Petersen, Moracco, Goldstein, & Clark, 2004), child care, financial and housing difficulties (Cattaneo & Goodman, 2005), disruptions in psychosocial functioning (Bogat, Levendosky, Theran, van Eye, & Davidson, 2003), and guilt (Street & Arias, 2001). Additionally, research suggests that even women who are not in a current IPV relationship, but have experienced past IPV, may experience difficulties accessing and utilizing personal and social resources (Foa, Cascardi, Zoellner, & Feeny, 2000; Johnson, Zlotnick, & Perez, 2008). As such, IPV survivors may have higher risk for nonengagement relative to women who have never experienced IPV. Therefore, the current study examines the effect of recent IPV, past IPV, and no IPV exposure on treatment engagement. Findings from such an analysis have important implications in terms of helping clinicians identify women who may be at risk for nonengagement as well as inform clinicians about what strategies would be most helpful in assisting IPV survivors with PTSD relative to other forms of interpersonal trauma survivors.
It is also unknown whether IPV (either previous or recent) is associated with poor treatment outcome. Kubany and Watson (2002) argue that there are several factors that complicate treatment of PTSD in IPV survivors relative to other types of trauma survivors, including victimization by more than one IPV perpetrator, repeated and multiple forms of IPV exposure, attachment to IPV perpetrators, and greater vulnerability to shame and guilt relative to women who have not experienced IPV. Additionally, IPV frequency is consistently associated with negative psychosocial outcomes, including PTSD and depression severity (Johnson et al., 2008; Resick, 2004). Thus, women who have experienced more frequent IPV may respond differently to treatment. Moreover, IPV may be a unique form of interpersonal trauma because women who experience violence from a partner often experience repeated incidences of IPV that increase in frequency and severity over time (Cattaneo & Goodman, 2005; Holtzworth-Munroe, Smutler, & Bates, 1997). Additionally, research suggests that violence perpetrated by an intimate partner may be especially damaging to women's mental health relative to assaults from nonintimate partners due to a greater sense of betrayal when the perpetrator is an intimate partner (e.g., Temple, Weston, & Marshall, 2007). Finally, IPV often leads to physical injuries (Campbell, 2003); and injuries sustained during interpersonal trauma are associated with poor treatment outcome in PTSD treatment (Hembree, Street, Riggs, & Foa, 2004). Therefore it is possible that women who have experienced severe or frequent IPV in a recent or past relationship may respond less favorably to treatment relative to other trauma survivors.
Alternatively, it is possible that the “type” of trauma endured is less important when treating IPV survivors than effectively treating the underlying PTSD. Research with other trauma populations has shown that it is the PTSD symptoms rather than the type of trauma that is associated with impaired functioning (Shea et al., 2000). Given that cognitive–behavioral interventions for PTSD have demonstrated positive treatment effects in IPV survivors (Johnson & Zlotnick, 2006; Kubany et al., 2003, 2004) and that cognitive–behavioral treatments for PTSD are effective in reducing PTSD, even among multiply victimized samples (e.g., Foa et al., 2005; Resick et al., 2002, 2008), it is possible that treating PTSD and depression among IPV survivors is similar to treating women who experience PTSD as a result of different types of interpersonal victimizations. This remains an empirical question. In order to advance the field's knowledge about treatment engagement and treatment outcome for IPV survivors, it is imperative that research identifies whether IPV survivors begin, complete, and respond differently to empirically supported PTSD treatments relative to participants who have not endured IPV.
The majority of studies examining treatment response among those undergoing treatment for PTSD (e.g., Ehlers et al., 1998; Foa, Riggs, Massie, & Yarczower, 1995; van Minnen, Arntz, & Keijsers, 2002) have used bivariate correlations or hierarchical regression data analytic techniques. These methods do not account for the change in symptoms over time and often exclude individuals with missing data, leading to an incomplete picture of the findings (McArdle & Bell, 1998). In the present study, we utilized hierarchical linear modeling to accommodate missing data, such that data were analyzed for all women who were randomized to treatment, regardless of whether they had missing data. Similarly, we included 9 assessment points to assess treatment response, as assessed by changes in PTSD and depressive symptoms. Specifically, in addition to pretreatment, posttreatment, and 6-month follow-up assessments, participants completed self-report measures of PTSD and depression severity every week during their 6 weeks of treatment, resulting in a total of 9 assessment points (Resick et al., 2008). The use of multiple time points is a strength of this study because it leads to greater power to detect predictors of treatment response (Schnurr, 2007).
The aims of this study were to conduct a secondary analysis of an RCT of CPT for PTSD among interpersonal trauma survivors (Resick et al., 2008) to examine IPV status as a predictor of (a) treatment engagement (i.e., starting and completing therapy); and (b) treatment outcome, defined as reductions in self-reported PTSD and depressive symptoms. The purpose of the larger RCT was to conduct a dismantling study of CPT in which the full protocol was compared with its constituent components: cognitive therapy only (CPT-C) and written accounts (WA) for the treatment of PTSD and comorbid symptoms. In the RCT, Resick and her colleagues (2008) found that women in each of the three conditions exhibited significant reductions in PTSD and depressive symptoms, but that the CPT-C condition demonstrated more improvement in PTSD symptoms relative to the WA condition. Based on previous literature, we hypothesized that women in a current relationship with IPV within the past year (i.e., women who experienced recent IPV) would demonstrate lower treatment engagement, as measured by the likelihood of starting and completing therapy, relative to women who endorsed past IPV only or no IPV exposure. Regarding treatment outcome, for women who began therapy, we hypothesized that the frequency of IPV endured would be associated with less improvement in PTSD and depressive symptoms during treatment relative to participants who had not been exposed to IPV.
Method
Participants
Procedures and findings for the larger RCT are described in full detail in Resick et al. (2008). In brief, participants were recruited broadly in a metropolitan city in the Midwestern United States through referrals from victim assistance agencies, community therapists, flyers, and newspaper advertisements. Women were informed that the purpose of the study was to examine the effectiveness of psychological therapy for the psychological effects of sexual or physical assault on victims. Exclusion criteria for the larger trial included illiteracy, current psychosis, suicidal intent, dependence upon drugs or alcohol, current stalking, or IPV from a current partner within the past 6 months. Women were included in the trial if they were age 18 and over, met Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV; American Psychiatric Association [APA], 1994) criteria for PTSD as measured by the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) secondary to sexual or physical assault in childhood or adulthood, and were at least 3 months posttrauma (no upper limit). Inter-rater reliability for PTSD diagnostic status on the CAPS was excellent in the RCT, with 100% agreement for a random sample of CAPS interviews (see Resick et al., 2008, for further details).
This study includes 150 women who were randomized to receive full CPT (n = 53), the cognitive portion only (CPT-C; n = 47), or the written accounts only (WA; n = 50). Women were an average of 35.4 years of age (SD = 12.4, range: 18–74). Over half of the women (62%) were Caucasian, 34% were African American, and 4% identified themselves as belonging to another racial group. On average, participants reported 13.8 years of education (SD = 2.8, range: 6–20) and approximately half (53.7%) had an annual income of less than $20,000 per year. The majority of the women in this sample had experienced multiple forms of interpersonal violence victimization. Approximately 84% of the sample endorsed adult physical assault (including, but not limited to IPV), 80.7% endorsed adult sexual victimization, 78% reported child sexual abuse (60% penetrative sexual abuse), and 77% reported childhood physical abuse on the Standardized Trauma Interview (Resick, Jordan, Girelli, Hutter, & Marhoeder-Dvorak, 1988).
Of the 150 women, 48 (32.0%) women reported that they had never experienced IPV (no IPV group), 79 (52.7%) had experienced past IPV only (past IPV group), and 23 (15.3%) reported IPV within the past year from their current partner (recent IPV group). The three IPV groups are hereafter referred to as IPV status groups. There were no differences across the three treatment conditions in terms of IPV status. Significant group differences were apparent on two demographic variables among the three IPV status groups. The recent IPV group had a higher percentage of African American women, χ2(2, N = 150) = 7.98, p < .01, R2 = .05, and fewer years of education, F(2, N = 150) = 6.67, p < .01, partial η2 =.08. There was also a nonsignificant trend for those in the recent IPV group to be younger, F(2, N = 150) = 3.64, p = .06, partial η2 = .10. Planned comparisons indicated that there were no significant differences in PTSD or depression severity among the three IPV status groups. See Table 1 for sample characteristics by IPV group status. Additionally, there were no significant differences among the three IPV status groups in terms of the number or types of exposures to other forms of interpersonal violence, including childhood physical and sexual abuse, adult physical assault from a nonintimate partner, and sexual assaults in adulthood. There were also no significant differences among the three groups for the number or type of current comorbid diagnoses. Major depressive disorder, panic disorder, and substance abuse were assessed by the Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID; First, Gibbon, Spitzer, & Williams, 1996). Finally, there were no significant differences between the recent IPV group (26.1%) and the past IPV group (26.6%) in terms of the proportion of women identifying IPV as their index traumatic event.
Table 1.
Descriptive Statistics for Demographic, Predictor, and Outcome Variables
| Measure | ITT sample N=150 M (SD) or n (%) |
No IPV N=48 M (SD) or n (%) |
Past IPV N=79 M (SD) or n (%) |
Recent IPV N=23 M (SD) or n (%) |
|---|---|---|---|---|
| Demographic Variables | ||||
| African American | 51 (34%) | 10 (21%)a | 30 (38%)b | 11 (48%)b |
| Age | 35.44 (12.39) | 31.19 (2.71)a | 39.12 (12.28)b | 31.87 (9.02)a |
| Years of Education | 13.81 (2.78) | 14.55 (1.93)a | 13.86 (2.39)a | 12.11 (3.50)b |
| Predictor and Outcome Variables | ||||
| IPV Frequency | 26.78 (41.88) | 0.00 (0.00)a | 37.50 (44.85)b | 45.82 (48.87)c |
| Initial PTSD | 29.17 (9.51) | 27.88 (8.43) | 29.70 (9.84) | 30.09 (10.62) |
| Initial Depression | 26.56 (11.21) | 25.58 (10.56) | 26.25 (11.26) | 29.65 (12.27) |
Note. ITT=intent-to-treat sample; IPV=intimate partner violence.
Letters (a,b,c) signify significant (p<.05) differences across IPV conditions.
Of the 150 women in the intent-to-treat (ITT) sample, 24 never returned for the first session of therapy, 126 women completed one or more therapy sessions (i.e., treatment starters), and 86 women completed all 12 hours of therapy (i.e., treatment completers). Women who began treatment (i.e., treatment starters) completed an average of 9.5 hours of therapy (SD = 5.12, range: 1–12) over the course of 7.3 weeks (SD = 1.3).
Measures
Posttraumatic Diagnostic Scale
The Posttraumatic Diagnostic Scale (PDS; Foa, 1995) is a 49-item self-report measure that assesses trauma history and all DSM-IV criteria for the diagnosis of PTSD. Respondents rate the frequency of each symptom on a scale ranging from 0 to 3, with higher scores indicating higher frequency of PTSD symptoms. The current study examined the PDS symptom severity score that ranges from 0 to 51 and is obtained by summing an individual's responses from each item. The cutoff scores for symptom severity ratings are 0 (no rating), 1–10 (mild), 11–20 (moderate), 21–35 (moderate to severe), and > 36 (severe). The PDS has demonstrated reliability and validity (Foa, Cashman, Jaycox, & Perry, 1997). The coefficient alpha for the current study was .88.
Beck Depression Inventory-II
The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) consists of 21 items assessing depressive symptoms corresponding with DSM-IV criteria for major depressive disorder. The cutoff scores are as follows: 0–13 (minimal depression), 14–19 (mild depression), 20–28 (modmoderate depression), and 29–63 (severe depression). Higher total scores indicate more severe depressive symptoms. The BDI-II has demonstrated reliability and validity in heterogeneous outpatient samples (Beck et al., 1996). The coefficient alpha for the current study was .91.
Conflict Tactics Scale-Physical Aggression Subscale
IPV was assessed with a modified version of the original Conflict Tactics Scale–Physical Aggression Subscale (CTS; Straus, 1979), which has demonstrated reliability and validity (Hornung, McCullogh, & Sugimoto, 1981). The 8-item Physical Assault subscale of the CTS was administered. Respondents reported on the frequency of abusive behaviors perpetrated by their current partner and most recent previous partner. Respondents were asked about IPV perpetrated by their current partner within the past year (i.e., physically violent acts from a current partner within the past year) and IPV by a previous partner during the last year they were together. If respondents had multiple partners who engaged in IPV in the past, they were asked to respond in terms of the one who most frequently used IPV. The scores for each item ranged from 0 (never) to 6 (more than 20 times), and severity scores were calculated by summing the midpoints of the response categories for each item (e.g., 6 to 10 times was recoded as 8; see Straus, 1979).
Two IPV variables were created: IPV status and IPV frequency. IPV status was a categorical variable indicating whether the participant (a) was in a current relationship in which she was the victim of physical aggression within the past year (i.e., recent IPV group), (b) was previously (but not currently) in a relationship in which she was the victim of physical aggression (i.e., past IPV group), or (c) was never in a relationship in which she was the victim of physical aggression (i.e., no IPV group). IPV frequency was computed by taking the maximum frequency score from either the current or previous relationship. This strategy was adopted to create more dispersion in the IPV frequency variable and because initial analyses revealed that relatively few participants endorsed recent IPV (n = 23), and these participants were likely to drop out of the study before treatment began. The Physical Assault subscale of the CTS had coefficient alphas of .89 for recent IPV and .88 for past IPV.
Trauma Related Guilt Inventory
The Trauma Related Guilt Inventory (TRGI; Kubany et al., 1996) is a 32-item inventory with scales to assess several components of trauma-related guilt. Items are scored on a 5-point scale ranging from 1 (never/not at all true) to 5 (always/extremely true). For the current study, the Guilt Cognitions subscale was examined, which has demonstrated reliability and validity, including internal consistency reliability of .86 and moderate correlations with PTSD and depression symptoms in a trauma sample (Kubany et al., 1996). In this study, the coefficient alpha for the Guilt Cognitions subscale was .89.
Procedure
As noted previously, all participants were randomly assigned to one of three treatment conditions: CPT, CPT-C, or WA. Therapists included one woman with a master's degree and seven women with doctorates in clinical psychology. Each therapist conducted approximately equal numbers of therapy cases in each condition. All treatment sessions were videotaped and treatment adherence and competence were closely monitored (see Resick et al., 2008, for further details). All three treatments were intended to be completed within 6 weeks and were equated for amount of therapy time (i.e., 12 hr), but they were delivered slightly differently. CPT and CPT-C consisted of 12 sessions, each 60 min in length, conducted twice per week. WA had, in the first week, two separate 60-min sessions; thereafter, the sessions were 2 hr in length and held once a week, for a total of 7 sessions. An upper limit for therapy completion was set at 12 weeks. Women completed self-report measures of PTSD and depression severity at pretreatment, every week during their 6 weeks of treatment, posttreatment, and at 6-month follow-up, resulting in a total of 9 assessment points. Women completed the self-report measures of PTSD and depression severity at the beginning of therapy sessions once per week during treatment. A brief description of the three treatments follows:
Cognitive Processing Therapy
CPT followed the manual as written by Resick and Schnicke (1993) including updated forms found in Resick, Monson, and Chard (2007). CPT is a structured protocol in which the primary aim of therapy is to help the client learn skills to recognize and challenge cognitive distortions, first regarding his or her worst traumatic event and then the meaning of the event(s). The full CPT package includes detailed written accounts (WA) of the traumatic event and daily readings of these written accounts during a portion of the therapy. Cognitive therapy is used during sessions and via worksheets to help clients identify problematic cognitions that have become a style of responding. Therapy includes education about PTSD, identification of relationships between events, thoughts, and emotions, and the development of alternative, more balanced thinking.
Cognitive Therapy Only
The CPT-C protocol was identical to the full CPT except for the omission of the detailed writing account. There is an additional emphasis on cognitive skills, including further applications of worksheets for homework.
Written Accounts
As noted in Resick et al. (2008), the configuration of the WA protocol was developed to maintain the integrity for the spirit of the written account in the full CPT protocol. Specifically, the WA therapy structure and the configuration of written accounts are designed to be implemented faithfully to CPT but also as close as possible to the way Prolonged Exposure (PE; Foa et al., 1999) was implemented in a previous trial comparing CPT and PE (Resick et al., 2002). The WA condition expands upon the written accounts component of CPT and participants were asked to engage in their writing during sessions. Sessions 1 and 2 were an hour each and consisted of an overview of the treatment, education regarding PTSD, instructions regarding subjective units of distress (SUDS), and script construction. During the remaining five sessions, participants briefly met with the clinician and then spent 45–60 min writing about their worst trauma accompanied by SUDS ratings at the beginning and end of the writing assignment, as well as ratings of strong emotions. Following the end of the written assignment, the client read the account to the therapist. Upon completion of the reading, therapists made nondirective and supportive comments, facilitated emotional processing, and provided education, but were not allowed to conduct any cognitive therapy or try to challenge the client's cognitive distortions. For homework, clients were asked to complete their WA if they did not during the session, read it daily, and record SUDS ratings.
Data analysis
Chi-square and logistic regression analyses were used to examine potential differences in treatment engagement based on IPV status groups (no IPV, past IPV, recent IPV). Logistic regression was also used to examine whether IPV status predicted treatment completion. Growth curve modeling conducted within a multilevel regression framework was then used to examine IPV frequency as a predictor of treatment response in terms of reductions in PTSD and depression symptoms (e.g., Raudenbush, 2001; Raudenbush & Bryk, 2002; Singer & Willett, 2003). We used the HLM software program (HLM 6; Raudenbush, Bryk, & Congdon, 2005) with full maximum likelihood estimation. One of the advantages of multilevel regression using HLM is that this approach can accommodate missing data. Therefore, participants who attended at least one therapy session (i.e., treatment starters) were included in the estimation of the final solution regardless of whether they completed additional therapy sessions or posttreatment assessments.
Results
IPV status as a predictor of treatment engagement
To examine the relationship between IPV status and treatment engagement and noncompletion, the contingencies depicted in Table 2 for the ITT sample was first evaluated. The overall chi-square test was statistically significant, χ2 (4, N = 150) = 10.94, p = .03, R2 = .04. The recent IPV group had a higher proportion of women who never began treatment (38%) than the past IPV group (11%) and no IPV group (13%). Follow-up logistic regression analyses were conducted using a dichotomous variable (i.e., attended at least one therapy session or not). Dummy-coded variables representing IPV status were entered into the logistic regression equation. Results indicated that IPV status was a significant predictor of whether or not women started treatment, χ2(2, N = 150) = 8.91, p < .05, R2 = .06, with the no IPV (Odds Ratio [OR] = 4.50) and past IPV (OR = 5.00) groups significantly more likely to start treatment compared to the recent IPV group.
Table 2.
IPV Status by Completion Status
| IPV Status | Never Started | Non-Completion | Completed | Totals |
|---|---|---|---|---|
| Recent IPV | 9 (39.1%) | 4 (17.4%) | 10 (43.5%) | 23 |
| Past IPV | 9 (11.4%) | 22 (27.8%) | 48 (60.8%) | 79 |
| No IPV | 6 (12.5%) | 14 (29.2%) | 28 (58.3%) | 48 |
| TOTALS | 24 (16.0%) | 40 (26.7%) | 86 (57.3%) | 150 |
Note. IPV=intimate partner violence.
To rule out the possibility that this finding might be due to demographic variables (i.e., race, age, and education), more severe PTSD, or treatment condition, the associations between these variables and whether or not treatment was started was examined. Only race was a significant predictor of whether or not treatment was started, with African Americans less likely to start treatment compared to women of other racial groups (b = 1.18, p < .05, OR = 3.27). When both race and IPV status were simultaneously included in a logistic regression analysis, both were significant predictors of whether or not treatment was started. The overall effect of IPV status remained significant, χ2(2, N = 150) = 7.65, p < .05, R2 = .03. Though the ORs comparing the likelihood to start treatment between the recent and no IPV status conditions (OR = 3.47) and the recent and past IPV status conditions (OR = 4.87) dropped slightly, both associations remained statistically significant (p's < .05). The association between African American status and likelihood to start treatment remained significant when controlling for IPV status (b = 1.18, p < .05, OR = 3.27). Therefore, both IPV status and African American status were independent predictors of treatment engagement, such that participants with recent IPV and those who were African American were less likely to start treatment after completing the initial pretreatment assessment sessions regardless of which treatment they were randomized to receive in the RCT.
Although the recent IPV group is relatively small (n = 23) we conducted post-hoc analyses of variance to examine differences between those who started treatment (n = 14) and those who did not start treatment (n = 9) on a number of pretreatment characteristics including initial PTSD and depression severity, recent IPV frequency, past IPV frequency, and guilt cognitions. None of the differences reached statistical significance. However, the associated effect size (Cohen's d) for PTSD, depression, and guilt cognitions exceeded .50, the cutoff that is typically adopted to indicate a medium effect. Relative to women with recent IPV who started treatment, participants with recent IPV who did not start treatment reported lower PTSD severity (M = 26.56 vs.M = 32.36, Cohen's d = .55) and lower depression severity (M = 25.33 vs. M = 32.43, Cohen's d = .58). However, relative to those women with recent IPV who started treatment, those with IPV who did not start treatment reported higher levels of guilt cognitions (M = .42 vs. M = .07, Cohen's d = .52).
It was next examined whether IPV status impacted treatment completion. A logistic regression revealed that for those participants who started treatment (n = 126), IPV status did not predict who completed treatment (i.e., attended all 12 of the available treatment hours as defined in Resick et al., 2008), χ2(2, N = 126) = .12, p = ns). Neither demographic factors nor treatment condition significantly predicted who completed treatment. Therefore, although individuals reporting recent IPV were less likely to begin treatment, once they started, they were just as likely to complete the treatment protocol as the comparison groups regardless of the treatment condition. In addition, among participants who started treatment, neither IPV status, F(2, 123) = .96, ns, partial η2 = .02, nor IPV frequency (r = −.15, ns) was significantly associated with the proportion of treatment sessions attended. These findings suggest that IPV exposure did not adversely impact treatment completion or amount of therapy attendance among those individuals who started treatment.
IPV status as a predictor of treatment response
In order to examine IPV frequency as a predictor of treatment response, a series of growth curve models were conducted within a multilevel regression approach (e.g., Raudenbush, 2001; Raudenbush & Bryk, 2002; Singer & Willett, 2003) using HLM with full maximum likelihood estimation (Raudenbush et al., 2005) with the subsample of participants who attended at least one treatment session (i.e., treatment starters; 24 participants of the ITT sample dropped out before attending one treatment session). Orthogonal polynomial contrasts were used to model linear and quadratic change across the nine assessment time points. The advantage of using orthogonal polynomial contrasts to examine curvilinear change is that this method decomposes the overall trajectory into different sources of unique variance, unlike the power polynomial approach in which the linear time coefficient is conditional on how time is coded (Ployhart, Holtz, & Bliese, 2002).
In the context of the current study, the linear trend represents an overall increase or decrease in symptoms from the first assessment point to the last, whereas the quadratic trend examines the possibility that the rate of change was not constant across all assessment periods (e.g., strong decrease that flattens out over time). The inclusion of both time coefficients allowed us to examine moderators of the overall decrease (linear coefficient) and potential differences in how fast change occurred (quadratic coefficient). The primary hypotheses involved a two-way Time × IPV Frequency interaction. Because the overall time effect included both the linear and quadratic time coefficient, the overall Time × IPV Frequency interaction was evaluated by examining the change in goodness of fit as assessed by the deviance statistic when removing the interactions from the model. The difference in the deviance statistic between two models (Δdev) follows a chi-square distribution with degrees of freedom equal to the difference in the number of parameters included across the two models (Raudenbush & Bryk, 2002). In other words, the Time × IPV Frequency interaction was assessed by evaluating whether or not this predicted the outcome variables (PTSD and depressive symptoms) above and beyond the variance accounted for by the main effects of time and IPV frequency. Because the test of the overall effects was based on a chi-square distribution, Cramer's Phi (ϕc), which can be interpreted as variance accounted for, was reported as an effect size indicator. For individual coefficients, the squared partial regression coefficient (pr2) was calculated as an effect size indicator for significant effects with .01, .06, and .14 as suggested cutoffs for small, medium, and large effect sizes, respectively (Kirk, 1996). Because of the findings reported above that IPV status impacts whether or not treatment is actually started, treatment response analyses were conducted for the sample of participants who started treatment (n = 126).
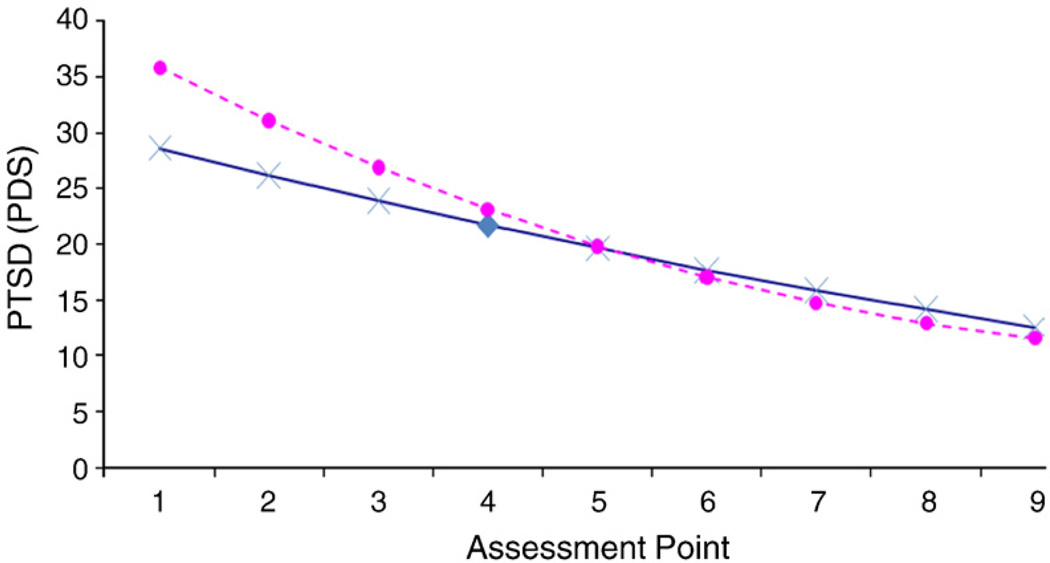
For the model examining change over time in PTSD, the overall Time × IPV Frequency was significant (Δdev = 12.21, df = 2, p < .01, R2 = .10). Examining the regression coefficients revealed a significant linear Time × IPV Frequency interaction (b = −.09, t = −3.33, pr2 = .08, p < .01) but not a significant quadratic Time × IPV Frequency interaction (b = .04, t = 1.03, pr2 = .008, p > .05). This pattern of results suggests that IPV frequency impacted change in PTSD symptoms during the course of treatment. To depict the nature of the interaction, PTSD severity was graphed as a function of time at different IPV frequency levels (no IPV and one SD above the mean of IPV frequency, see Fig. 1). This interaction demonstrates that IPV frequency was associated with higher initial PTSD severity and greater decreases in PTSD severity over time. In order to examine the potential role of treatment condition in driving any findings, treatment condition was added as a covariate in the growth curve models; however, treatment condition did not significantly impact the effect of IPV frequency on change in PTSD symptoms (b = −.09, t = −3.33, pr2 = .08, p < .01). Finally, IPV Frequency × Treatment Condition interaction terms were added as covariates in the growth curve models. None of these interaction terms approached statistical significance, suggesting that the impact of IPV did not significantly vary as a function of treatment condition.
FIGURE 1.
Change in PTSD over time as a function of IPV frequency in the treatment beginner sample (n = 126). X depicts this relationship for participants who did not endorse current or past IPV, whereas ● depicts this relationship for participants who endorsed high levels of IPV frequency (1 standard deviation above the mean).
IPV frequency and PTSD severity demonstrated a significant positive association at the initial assessment (r = .29, p < .05), which may account for the significant association between IPV frequency and decreases over time in PTSD reported above. That is, individuals who reported higher levels of IPV frequency might have greater decreases in PTSD because they started off with more severe PTSD (i.e., a “regression to the mean” phenomenon). To rule out regression to the mean as an alternative explanation of the findings, initial PTSD severity was included as a Level 2 covariate predicting each of the change parameters. When controlling for initial PTSD severity, the significant association between IPV frequency and linear time was reduced somewhat, but remained statistically significant (b = − .06, t = − 2.29, pr2 = .04, p < .05). Finally, there was no significant association between IPV frequency and PTSD severity at the 6-month follow-up assessment (b = − .02, t = .72, pr2 = .004, p > .05).1
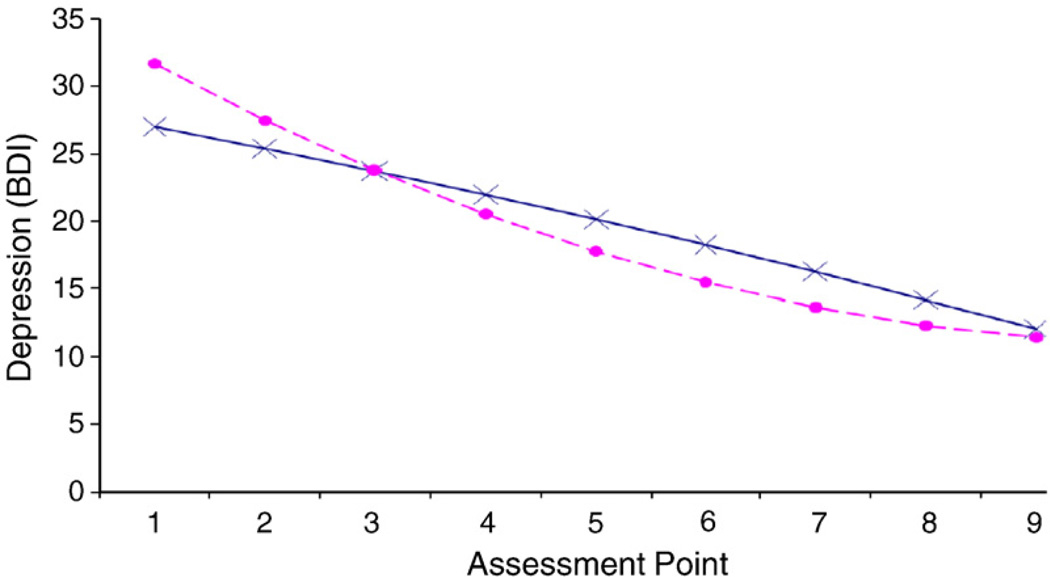
For the model examining change over time in depression, the interaction of Time × IPV Frequency was statistically significant (Δdev = 7.22, df = 2, p < .05, R2 = .06). Again, the linear Time × IPV Frequency interaction (b = − .06, t = − 2.48, pr2 = .05, p < .05) was significant, while the quadratic Time × IPV Frequency interaction was not statistically significant (b = .06, t = 1.28, pr2 = .01, p > .05). Fig. 2 depicts the nature of this interaction. Again, treatment condition was included as a covariate in the growth curve models; however, treatment condition did not significantly impact the effect of IPV frequency on change in depressive symptoms (b = − .06, t = − 2.53, pr2 = .05, p < .05), nor did treatment condition significantly interact with IPV frequency. When controlling for initial depression levels, the linear Time × IPV Frequency interaction (b = − .06, t = − 2.48, pr2 = .03, p = .057) approached statistical significance, with the associated effect size falling between small and medium. Finally, there was no significant association between IPV frequency and depression severity at the 6-month follow-up assessment (b = − .02, t = .65, pr2 = .003, p > .05).
FIGURE 2.
Change in Depression (y-axis) over time as a function of IPV frequency for participants who started treatment (n = 126). X depicts this relationship for participants who did not endorse current or past IPV, whereas ● depicts this relationship for participants who endorsed high levels of IPV frequency (1 standard deviation above the mean).
Discussion
The primary goal of this study was to examine IPV status as a predictor of treatment engagement and treatment outcome among women who were taking part in an RCT of CPT for PTSD. It was expected that IPV exposure would influence treatment engagement, such that women who endorsed recent IPV would be less likely to begin and complete treatment. It was also hypothesized that frequency of IPV exposure would be associated with less improvement in PTSD and depressive symptoms over the course of treatment. The hypotheses were partially supported. Recent IPV status was associated with lower likelihood of treatment engagement; however, women who had been exposed to recent or past IPV responded well to CPT and its component parts in terms of treatment completion and treatment outcomes.
As expected, women in an intimate relationship with recent physical violence (i.e., in the past year) began treatment at much lower rates relative to the women with past IPV or no IPV exposure. The presence of recent IPV decreased the likelihood of starting treatment even after accounting for demographic variables and other baseline characteristics. Therefore, it may be the case that women who are in a relationship with recent IPV experience more ambivalence about starting treatment and/or additional treatment barriers. There are many reasons why it may be difficult for women experiencing recent IPV to begin treatment, including fear of their partner finding out they are in therapy, safety concerns (Petersen et al., 2004), a need to prioritize immediate stressors over trauma-focused therapy (Hobfoll, 1989), or limited resources (Foa et al., 2000; Hobfoll, 1989). The post-hoc findings from this study indicated that women with recent IPV who did not begin treatment may be impacted by higher levels of guilt relative to women with recent IPV who began treatment. The fact that they reported lower PTSD and depression symptoms may also speak to therapy being less urgent in the face of other stressors. Less treatment participation may also be understood from a “readiness to change” perspective (Prochaska, Norcross, & DiClemente, 1994).
Regardless of why women with recent IPV are less likely to begin treatment, working with women who have experienced recent IPV in a current relationship to enhance their ability to begin treatment is an important next step. Among participants who started therapy (i.e., attended one or more treatment sessions), past or recent IPV status was not associated with treatment noncompletion and did not adversely impact the proportion of therapy sessions attended. This finding was encouraging because it demonstrates that once a woman with past or recent IPV begins therapy she is able to participate in treatment effectively.
Contrary to our hypothesis, IPV frequency did not adversely impact treatment outcome. Instead, women with frequent IPV who engaged in treatment experienced significantly greater improvements in PTSD and depression over the course of treatment regardless of treatment condition. While IPV frequency was positively associated with initial PTSD and depressive symptoms, IPV frequency remained significantly associated with linear change over time even when initial PTSD severity was included as a covariate in the growth curve analysis. A similar relationship was found for depression, albeit at a marginal level of significance (p = .057). These findings suggest that the differences in linear changes over time were not merely due to the fact that individuals with frequent IPV started with more severe symptoms, and thus had more room for improvement in terms of treatment response. Although regression to the mean could be an alternative explanation for the current findings, it is a phenomenon that occurs most strongly between the first and the second measurement points in longitudinal research. The fact that IPV frequency remained significant after controlling for initial symptom severity coupled with the fact that PTSD and depressive symptoms showed equally strong decreases across all nine measurement points with no indication of leveling off is evidence that differential decreases in symptom severity were not due to regression to the mean.
IPV frequency did not predict PTSD or depression severity at the 6-month follow-up. Thus, it appears that the higher initial symptom levels associated with IPV coupled with somewhat larger decreases in symptom severity over time resulted in similar levels of PTSD and depression at the 6-month follow-up between women with frequent IPV and those without IPV. It is also important to acknowledge that it is unknown whether the reliance on repeated self-reported measures of PTSD and depression may have impacted the present findings (e.g., regression to the mean or practice effects). Future research should investigate the temporal stability of the PTSD and depression measures utilized in the current study to rule out the possibility of practice effects or regression to the mean in accounting for the effect of IPV frequency on treatment outcome.
The current findings are not particularly surprising given that cognitive–behavioral approaches are effective in treating PTSD among multiply victimized trauma survivors, including those with complex clinical presentations common in IPV survivors (e.g., Foa et al., 2005; Resick et al., 2002, 2008). These findings suggest that CPT and its component parts appear to be a good treatment match for IPV survivors. Once IPV survivors engage in CPT they experience rapid improvement in their PTSD and depression in spite of recent or past IPV. Clinicians should always consider the woman's current safety a priority when beginning CPT or any trauma-focused therapy. Specifically, clinicians should help women develop a safety plan, and when appropriate, help the client access appropriate community resources.
Limitations of the current study should be noted. The sample consisted largely of low-income women seeking services for distress related to a wide variety of interpersonal traumas. The women in this study were not necessarily seeking treatment for PTSD stemming from IPV and the recent IPV subgroup was small. Therefore, these findings may not generalize to other samples. As noted, women who were in a recent IPV relationship were less likely to engage in treatment (39% did not begin treatment). As a result, it remains unknown how this subsample would have responded to treatment. Similarly, the current study did not examine women's reasons for not starting therapy, limiting the conclusions that can be drawn about why recent IPV leads to lower rates of starting treatment. Additionally, IPV was examined for a limited number of intimate partners: current partner and one identified previous partner (the partner who had most frequently used IPV). It is possible that women had been exposed to more IPV than was measured in the current study. Similarly, the measure of IPV administered in this study did not include measures pertaining to sexual and psychological forms of IPV. In particular, it is likely that many of the women who had experienced previous or recent IPV also experienced psychological abuse because it often precedes and co-occurs with physical IPV (Fritz & O'Leary, 2004) and has detrimental emotional effects even in the absence of physical abuse (Follingstad, 2007). Finally, IPV exposure was not typically the primary index event (the worst trauma) focused on first in treatment (26% of IPV survivors identified IPV as the index event). Therefore, more research is needed to examine the impact of different forms of current and past IPV, as well as when IPV is the index event, on treatment outcome.
Results from the present study justify a more rigorous examination of IPV exposure and its impact on treatment engagement and outcome. Future research should examine interventions aimed at increasing treatment readiness and commitment among women with recent IPV. For instance, it is possible that strategies such as motivational interviewing (Miller & Rollnick, 2002) may enhance treatment engagement. Additionally, it is important to know whether there are unique clinical presentations among IPV survivors that are particularly well suited for various cognitive–behavioral interventions. Although the current study did not find any significant interactions between IPV frequency and treatment condition, it is possible that such analyses were underpowered due to the small subsamples of IPV survivors across the three treatment conditions. Clinical trials utilizing larger and heterogeneous samples of IPV survivors are needed to address these issues. Similarly, given that PTSD symptoms may mediate the relationship between IPV and depression in IPV survivors (Resick, 2004), future research should examine whether changes in PTSD severity during treatment mediates the relationship between IPV status and depression severity following treatment. Finally, given that PTSD is prospectively associated with IPV revictimization (Krause, Kaltman, Goodman, & Dutton, 2006), it is important to determine whether treating IPV survivors' PTSD and depression helps to reduce revictimization in future intimate relationships.
Acknowledgments
Katherine M. Iverson's contribution to the writing of this manuscript was supported by a training grant from the National Institute of Mental Health (T32MH019836) awarded to Terence M. Keane. This research was funded by a grant from the National Institute of Mental Health (R01-MH51509) awarded to Patricia A. Resick.
Footnotes
To test the association between IPV frequency and PTSD scores at the 6-month follow-up period, we had to change the way time was modeled in the analyses. Instead of using the polynomial contrasts used in the primary analyses, we created a time variable that started at 10 for the baseline assessment and decreased by 1 for each subsequent time variable, so that this time variable was coded 1 at the 6-month follow-up period. To account for nonlinear change, we then performed a natural log transformation of this time variable (ln_time; see Singer & Willett, 2003). The ln_time variable was coded 0 at the 6-month follow-up period (the natural log of 1 equals 0). Therefore, when ln_time is entered as a Level 1 predictor of PTSD, the intercept of this equation corresponds to PTSD levels at the 6-month assessment, and adding IPV frequency as a Level 2 predictor of this coefficient allowed us to examine the association between IPV frequency and PTSD levels at the 6-month follow-up assessment. It should also be noted that including initial symptom severity level as a covariate did not affect the relationship between IPV frequency and symptom severity levels at the 6-month follow up; when controlling for initial PTSD levels, this association was still not significant (b = − .04, t = − 1.34, pr2 = .01, p > .05).
Contributor Information
Katherine M. Iverson, Women's Health Sciences Division of the National Center for PTSD, VA Boston Healthcare System and Boston University
Patricia A. Resick, Women's Health Sciences Division of the National Center for PTSD, VA Boston Healthcare System and Boston University
Michael K. Suvak, Women's Health Sciences Division of the National Center for PTSD, VA Boston Healthcare System and Boston University
Sherry Walling, Fresno Pacific University.
Casey T. Taft, Behavioral Sciences Division of the National Center for PTSD, VA Boston Healthcare System and Boston University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Beck AT, Steer RA, Brown KG. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bogat GA, Levendosky AA, Theran S, von Eye A, Davidson WS. Predicting the psychosocial effects of intimate partner violence (IPV): How much does a woman's history of IPV matter? Journal of Interpersonal Violence. 2003;18:1271–1291. doi: 10.1177/0886260503256657. [DOI] [PubMed] [Google Scholar]
- Campbell JC. Risk factors for femicide in abusive relationships: Results from a multisite case control study. American Journal of Public Health. 2003;93:1089–1097. doi: 10.2105/ajph.93.7.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JC, Soeken KL. Women's responses to battering over time: An analysis of change. Journal of Interpersonal Violence. 1999;14:21–40. [Google Scholar]
- Cattaneo LB, Goodman LA. Risk factors for reabuse in intimate partner violence: A cross-disciplinary review. Trauma. Violence, & Abuse. 2005;6:141–175. doi: 10.1177/1524838005275088. [DOI] [PubMed] [Google Scholar]
- Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73:965–971. doi: 10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM, Dumore E, Jaycox L, Meadows E, Foa E. Predicting response to exposure treatment in PTSD: The role of mental defeat and alienation. Journal of Traumatic Stress. 1998;11:457–471. doi: 10.1023/A:1024448511504. [DOI] [PubMed] [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV (SCID) New York: New York State Psychiatric Institute, Biometrics Research Department; 1996. [Google Scholar]
- Foa EB. Posttraumatic stress diagnostic scale [manual] Minneapolis, MN: National Computer Systems; 1995. [Google Scholar]
- Foa EB, Cascardi M, Zoellner LA, Feeny NC. Psychological and environmental factors associated with partner violence. Trauma, Violence, & Abuse. 2000;1:67–91. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SE, Rauch SAM, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Massie ED, Yarczower M. The impact of fear activation and anger on the exposure treatment for posttraumatic stress disorder. Behavior Therapy. 1995;26:487–499. [Google Scholar]
- Follingstad DR. Rethinking current approaches to psychological abuse: Conceptual and methodological issues. Aggression and Violent Behavior. 2007;12:439–458. [Google Scholar]
- Fritz PT, O'Leary KD. Physical and psychological partner aggression across a decade: A growth curve analysis. Violence and Victims. 2004;19:3–16. doi: 10.1891/088667004780842886. [DOI] [PubMed] [Google Scholar]
- Hembree EA, Street GP, Riggs DS, Foa EB. Do assault-related variables predict response to cognitive–behavioral treatment for PTSD? Journal of Consulting and Clinical Psychology. 2004;72:331–334. doi: 10.1037/0022-006X.72.3.531. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist. 1989;44:513–524. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- Holtzworth-Munroe A, Smulter N, Bates L. A brief review of the research on husband violence: Part III—Sociodemographic factors, relationship factors, and differing consequences of husband and wife violence. Aggression and Violent Behavior. 1997;2:285–307. [Google Scholar]
- Hornung CA, McCullough BC, Sugimoto T. Status relationships in marriage: Risk factors in spouse abuse. Journal of Marriage and the Family. 1981;43:675–692. [Google Scholar]
- Iverson KM, Shenk C, Fruzzetti AE. Dialectical behavior therapy adapted for women victims of domestic abuse: A pilot study. Professional Psychology: Research and Practice. 2009;40:242–248. [Google Scholar]
- Johnson DM, Zlotnick C. A cognitive–behavior treatment for battered women with PTSD in shelters: Findings from a pilot study. Journal of Traumatic Stress. 2006;19:559–564. doi: 10.1002/jts.20148. [DOI] [PubMed] [Google Scholar]
- Johnson DM, Zlotnick C, Perez S. The relative contribution of abuse severity and PTSD severity on the psychiatric and social morbidity of battered women in shelters. Behavior Therapy. 2008;39:232–241. doi: 10.1016/j.beth.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Jones L, Hughes M, Unterstaller U. Posttraumatic stress disorder (PTSD) in victims of domestic violence: A review of the research. Trauma, Violence, & Abuse. 2001;2:99–119. [Google Scholar]
- Kirk RE. Practical significance: A concept whose time has come. Educational and Psychological Measurement. 1996;56:746–749. [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton MA. Role of distinct PTSD symptoms in intimate partner reabuse: A prospective study. Journal of Traumatic Stress. 2006;19:507–516. doi: 10.1002/jts.20136. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the trauma-related guilt inventory (TRGI) Psychological Assessment. 1996;8(4):428–444. [Google Scholar]
- Kubany ES, Hill EE, Owens JA. Cognitive trauma therapy for battered women with PTSD: Preliminary findings. Journal of Traumatic Stress. 2003;16:81–91. doi: 10.1023/A:1022019629803. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Hill EE, Owens JA, Iannce-Spencer C, McCaig MA, Tremayne KJ, et al. Cognitive trauma therapy for battered women with PTSD (CTT-BW) Journal of Consulting and Clinical Psychology. 2004;72:3–18. doi: 10.1037/0022-006X.72.1.3. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Watson SB. Cognitive trauma therapy for formerly battered women with PTSD (CTT-BW): Conceptual bases and treatment outlines. Cognitive and Behavioral Practice. 2002;9:111–127. [Google Scholar]
- McArdle JJ, Bell RQ. Recent trends in modeling longitudinal data by latent growth curve methods. In: Little TD, Schnabel KU, Baumert J, editors. Modeling longitudinal and multiple-group data: Practical issues, applied approaches, and scientific examples. Mahwah, NJ: Erlbaum; 1998. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change. NY: Guilford Press; 2002. [Google Scholar]
- Petersen R, Moracco KE, Goldstein KM, Clark KA. Moving beyond disclosure: Women's perspective on barriers and motivators to seeking assistance for intimate partner violence. Women & Health. 2004;40:63–76. doi: 10.1300/j013v40n03_05. [DOI] [PubMed] [Google Scholar]
- Ployhart RE, Holtz BC, Bliese PD. Longitudinal data analysis: Applications of random coefficient modeling to leadership research. Leadership Quarterly. 2002;13:455–486. [Google Scholar]
- Prochaska JO, Norcross JC, DiClemente CC. Changing for good. New York: William Morrow; 1994. [Google Scholar]
- Raudenbush SW. Comparing personal trajectories and drawing causal inferences from longitudinal data. Annual Review of Psychology. 2001;52:501–525. doi: 10.1146/annurev.psych.52.1.501. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Raudenbush S, Bryk A, Congdon R. HLM 6: Hierarchical linear and nonlinear modeling [Computer software and manual] Lincolnwood, IL: Scientific Software International; 2005. [Google Scholar]
- Resick PA. A suggested research agenda on treatment-outcome research for female victims of violence. Journal of Interpersonal Violence. 2004;19:1290–1295. doi: 10.1177/0886260504271339. [DOI] [PubMed] [Google Scholar]
- Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum GA, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76:243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Jordan CG, Girelli SA, Hutter CK, Marhoeder-Dvorak S. A comparative outcome study of behavioral group therapy for sexual assault victims. Behavior Therapy. 1988;19:385–401. [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive processing therapy: Veteran/military version. Washington, DC: Department of Veterans' Affairs; 2007. [Google Scholar]
- Resick PA, Nishith P, Griffin MG. How well does cognitive–behavioral therapy treat symptoms of complex PTSD? An examination of child sexual abuse survivors within a clinical trial. CNS Spectrums. 2003;8:340–355. doi: 10.1017/s1092852900018605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive processing therapy, prolonged exposure and a waiting condition for the treatment of posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for rape victims: A treatment manual. Newbury Park, CA: Sage; 1993. [Google Scholar]
- Riggs DS, Caulfield MB, Street AE. Risk for domestic violence: Factors associated with perpetration and victimization. Journal of Clinical Psychology. 2000;56:1289–1316. doi: 10.1002/1097-4679(200010)56:10<1289::AID-JCLP4>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- Schnurr PP. The rocks and hard places in psychotherapy outcome research. Journal of Traumatic Stress. 2007;20:779–792. doi: 10.1002/jts.20292. [DOI] [PubMed] [Google Scholar]
- Shea MT, Zlotnick C, Dolan R, Warshaw MG, Phillips KA, Brown P, et al. Personality disorders, history of trauma, and posttraumatic stress disorder in subjects with anxiety disorders. Comprehensive Psychiatry. 2000;41:315–325. doi: 10.1053/comp.2000.9007. [DOI] [PubMed] [Google Scholar]
- Singer J, Willett J. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactic (CT) Scales. Journal of Marriage and the Family. 1979;41:75–87. [Google Scholar]
- Street AE, Arias I. Psychological abuse and posttraumatic stress disorder in battered women: Examining the roles of shame and guilt. Violence and Victims. 2001;16:65–78. [PubMed] [Google Scholar]
- Temple JR, Weston R, Marshall LL. Differing effects of partner and nonpartner sexual assault on women's mental health. Violence Against Women. 2007;13:285–297. doi: 10.1177/1077801206297437. [DOI] [PubMed] [Google Scholar]
- Thompson RS, Bonomi AE, Anderson M, Reid RJ, Dimer JA, Carrell D, et al. Intimate partner violence: Prevalence, types, and chronicity across adult women's lifetime. American Journal of Preventative Medicine. 2006;30:447–457. doi: 10.1016/j.amepre.2006.01.016. [DOI] [PubMed] [Google Scholar]
- van Minnen A, Arntz A, Keijsers GPJ. Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behaviour Research and Therapy. 2002;40:439–457. doi: 10.1016/s0005-7967(01)00024-9. [DOI] [PubMed] [Google Scholar]
- Wilt J, Olson D. Prevalence of domestic violence in the United States. Journal of the American Medical Women's Association. 1996;57:77–88. [PubMed] [Google Scholar]