Abstract
In the immediate aftermath of a traumatic event, many individuals experience physiological reactivity in response to reminders of the traumatic event that typically lessens over time. However, an overreliance on avoidant coping strategies may interfere with the natural recovery process, particularly for those who are highly reactive to trauma reminders. In the current investigation, we examined avoidant coping as a moderator of the association between heart rate reactivity to a trauma monologue measured shortly after a traumatic event and severity of posttraumatic stress disorder (PTSD) symptoms measured several months later. Fifty-five female survivors of assault completed PTSD diagnostic interviews and a self-report coping measure and participated in a trauma monologue procedure that included continuous heart rate measurement. These procedures were completed within 1 month of the assault and again 3 months postassault. After we controlled for the effect of initial symptom levels, the interaction of heart rate reactivity to the trauma monologue and avoidant coping measured at Time 1 was associated with PTSD symptom severity at Time 2. Individuals who are relatively highly reliant on avoidant coping strategies and relatively highly reactive to trauma reminders may be at greatest risk of maintaining or potentially increasing their PTSD symptoms within the first few months following the trauma. These findings may help inform early intervention efforts for survivors of traumatic events.
Keywords: posttraumatic stress disorder, avoidance, coping, psychophysiology, heart rate
In the weeks following a traumatic event, most individuals experience at least some symptoms characteristic of posttraumatic stress disorder (PTSD). Many, but not all, trauma survivors experience a profound reduction or complete remittance of these symptoms over the course of the first several months (Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). Identifying the subset of traumatized individuals who do not recover but instead maintain PTSD symptoms over time is a critical research question. Physiological reactivity and coping style are two potential risk factors with promising empirical support. For example, increased heart rate measured shortly after a traumatic event is associated with increased risk for PTSD (Yehuda, McFarlane, & Shalev, 1998). Further, increased heart rate reactivity to trauma reminders is associated with greater maintenance of PTSD symptoms over time (Blanchard et al., 1996).
A central tenet common to “gold-standard” treatments for PTSD is that avoidance plays a pivotal role in PTSD symptom maintenance (Foa & Rothbaum, 1998; Resick & Schnicke, 1993). Accordingly, it is not surprising that avoidant coping is associated with PTSD symptom severity both concurrently (Bryant & Harvey, 1995) and longitudinally (Benotsch et al., 2000). Avoidance has been theorized to interfere with successful processing of the trauma memory, habituation of negative emotions associated with the trauma memory, and extinction of fear responses conditioned to internal or external trauma reminders (Foa & Rothbaum, 1998; Keane & Barlow, 2002). Thus, individuals who are relatively reliant on avoidant coping may be particularly likely to exhibit a strong association between physiological reactivity to trauma reminders and PTSD symptom maintenance. Avoiding trauma memories or reminders may impede the natural recovery process that would allow for heightened arousal to decrease over time (Foa & Kozak, 1986). Avoidance may also reinforce PTSD symptoms by signaling the individual that the memories are in fact dangerous (Foa & Kozak, 1986). In contrast, the relationship between physiological reactivity and PTSD symptoms over time might be weaker for those who are less reliant on avoidant coping strategies.
The common assumption in PTSD theories is that avoidance interferes with recovery by preventing trauma survivors from habituating to the trauma memory (Foa & Rothbaum, 1998; Keane & Barlow, 2002); however, the way in which avoidance could affect the relationship between trauma reactivity and PTSD symptoms over time has not been tested. Instead, most studies have focused on the direct relationship between avoidance and PTSD. However, this design does not adequately test the mechanism by which avoidance is assumed to impact PTSD. If avoidance interferes with natural recovery from a trauma memory, then presumably avoidance would be more detrimental for individuals who are relatively more reactive to the memory.
Our aim in the current study was to investigate whether the use of avoidant coping strategies moderates the association between heart rate reactivity to a trauma monologue procedure (i.e., trauma reactivity) performed shortly after that traumatic experience occurred and PTSD symptoms over time. As part of a larger study, women who were sexually or physically assaulted were assessed within 1 month of the assault (Time 1 [T1]) and again 3 months postassault (Time 2 [T2]). We hypothesized that use of avoidant coping strategies at T1 would moderate the relationship between T1 trauma recovery and T2 PTSD symptoms and diagnostic status, after we controlled for initial PTSD symptoms or diagnosis. Specifically, we predicted that the relationship between trauma recovery and PTSD symptoms would be stronger for individuals who endorsed relatively high levels of avoidant coping than for individuals who endorsed lower levels of avoidant coping. Additionally, because approach coping strategies are hypothesized to be more adaptive, we believed that a similar analysis in which approach coping was tested as the moderator would yield an opposite pattern of results. Specifically, the association between trauma reactivity and PTSD symptoms would be stronger for individuals endorsing relatively low levels of approach coping than for individuals endorsing higher levels of approach coping.
Method
Participants and Procedures
Crime victims, all survivors of physical or sexual assault, participated in a longitudinal investigation of factors associated with recovery from assault (Griffin, Resick, & Mechanic, 1997; Gutner et al., in press). Potential participants were excluded if they reported prescription drug use that might confound autonomic responses (e.g., anticholinergics, beta blockers) or demonstrated current psychosis, inebriation during assessment, or substantial reading difficulties. Presence of psychotic symptoms was assessed with the Structured Clinical Interview for DSM–III–Revised–Patient Edition, With Psychosis Screen (Spitzer, Williams, Gibbon, & First, 1990). We assessed acute psychosis and inebriation using clinical judgment. Illiteracy was determined by the participant’s ability to explain the consent form. The procedure order was (a) self-report questionnaires, (b) trauma monologue task, and (c) diagnostic interviews.
These procedures were first completed within 1 month of the assault (T1) and then 3 months postassault (T2). Fifty-five participants with available data on the constructs of interest were included in the present study. Participants were primarily single (62% single, 15% married or living with a partner, 24% separated or divorced) and of African American descent (69%; 29% White, 2% American Indian). Mean age was 29.2 years (SD = 7.5), and mean years of education was 12.7(SD = 2.4). Most participants (80%) reported an annual income of less than $20,000. For most participants (85%), the index traumatic event was sexual assault. On average, participants had been a victim of crime 4.5 times (SD = 3.8) at T1 and experienced an additional 0.5 crimes (SD = 1.6) between assessments. Few reported receiving psychotherapeutic interventions between assessments: 51% of participants received no therapy, and 78% received fewer than six sessions. One participant (2%) reported receiving psychotropic medications. Eleven participants (20%) reported discussing the event with a member of the clergy.
Measures
Coping Strategies Inventory (CSI; Tobin, Holroyd, & Reynolds, 1984)
This 72-item scale measures the use of avoidance and approach coping strategies in response to a specific event, which in this study was the identified assault. The Disengagement Coping subscale, used to measure avoidance coping, assesses respondents’ attempts to mitigate distress through focusing their attention away from the source of stress. Conversely, the Engagement Coping subscale, used to measure approach coping, assesses respondents’ attempts to alleviate distress by employing strategies that directly confront the source of stress. The CSI has demonstrated sound factor structure (Tobin, Holroyd, Reynolds, & Wigal, 1989) and validity (Tobin et al., 1984) and had excellent internal consistency in the current sample (disengagement coping α = .91; engagement coping α = .94). For the current study, T1 avoidant (i.e., Disengagement) coping and approach (i.e., Engagement) coping subscales were included in the analyses.
Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995)
This interview is used to assess the frequency and intensity of PTSD symptoms. For this study, PTSD symptoms since the assault were assessed at T1, and PTSD symptoms in the previous month were assessed at T2. The CAPS has been shown to have excellent psychometric properties (Blake et al., 1995). Two types of CAPS variables were computed for both T1 and T2: (a) PTSD symptom severity and (b) PTSD diagnostic status (i.e., presence or absence of PTSD). Total scores for PTSD symptom severity were the sum of the frequency and intensity scores for the 17 symptoms (range = 0–136). For exploratory analyses, severity scores were computed for four separate PTSD symptom clusters (King, Leskin, King, & Weathers, 1998): reexperiencing, effortful avoidance, numbing, and hyperarousal. For diagnosis of PTSD, the Diagnostic and Statistical Manual of Mental Disorders (4th ed., DSM–IV; American Psychiatric Association, 1994) required endorsement of at least one reexperiencing symptom, three avoidance symptoms, and two arousal symptoms resulting in demonstrated functional impairment. A positive PTSD diagnosis also required endorsement of fear, helplessness, or horror in response to the assault. The symptom duration criteria was waived at T1 but included at T2.
Interviewers were trained master’s-level clinicians who received ongoing supervision, and each interview was discussed in a diagnostic consensus meeting. The interviews were audiotaped, and 23% (49/216) of T1 tapes and 11% of the T2 tapes (15/131) from the larger longitudinal study were scored by a second rater. Inter-rater reliability for PTSD diagnosis was excellent (T1 κ = .92; T2 κ = .84).
Trauma reactivity
Participants were seated in a comfortable chair in an 8 × 10 ft., sound-insulated, temperature- and humidity-controlled room and connected to physiological monitoring devices. Heart rate was measured continuously throughout the task by a modular system (Coulbourn Instruments, Allentown, PA). An optical blood flow transducer was attached to the distal phalanx of the second finger of the nondominant hand. This signal was converted by a tachometer into beats/minute (bpm). Heart rate was collected at a rate of five samples per second.
Heart rate was measured throughout five phases each lasting 5 min: (a) initial baseline, (b) monologue about a neutral topic, (c) neutral recovery phase, (d) monologue about the traumatic event, and (e) trauma recovery phase. Participants sat alone for the first, third, and fifth phases and were told to relax but were not instructed on what to think about. Before each monologue phase (neutral and trauma), the interviewer gave each participant a prompt sheet that listed possible topics to discuss. During the neutral monologue phase, the interviewer listened as participants described some past neutrally valenced event from the prompt sheet (e.g., “a meal you cooked”). Similarly, during the trauma monologue phase, the interviewer listened as participants described the traumatic event as guided by the prompt sheet. Prompt questions included time, location, and their reactions, thoughts, and feelings during the assault. If the participant fell silent during the monologue phases, the prompt sheets were used to elicit further speech.
Average heart rate was calculated for each phase after invalid samples, most likely due to movement artifacts, were removed. Heart rate averages for the five phases were 72.6 bpm (SD = 8.0) for baseline, 77.1 bpm (SD = 8.6) for neutral monologue, 73.6 bpm (SD = 7.9) for neutral recovery, 77.9 bpm (SD = 9.3) for trauma monologue, and 75.0 bpm (SD = 7.5) for trauma recovery. To create the trauma reactivity score, we subtracted average heart rate during the 5 min immediately preceding the trauma phase (the neutral recovery phase) from the average heart rate during the 5 min immediately following the trauma phase (the trauma recovery phase). This method captures changes in participants’ heart rate in response to discussing their trauma without the additional error variance in heart rate that is associated with measurements collected when participants are engaged in the act of speaking. We centered trauma reactivity and coping scores prior to computing Trauma Reactivity × Coping interaction scores.
Six participants were eliminated from the analyses due to invalid physiological readings. Of these, four were excluded for having more than 50% invalid heart rate samples, and two were excluded on the basis of outlier trauma reactivity scores (3 or more SDs from the mean).
Results
At T1, 78% of participants met PTSD diagnostic criteria (except for the symptom duration criteria) while 55% met PTSD diagnostic criteria at T2. Looking across time points, 42% of participants met PTSD diagnostic criteria at both assessments, 36% met criteria only at T1, 13% met criteria only at T2, and 9% did not meet criteria at either assessment. PTSD symptom severity scores significantly decreased from T1 to T2 (Table 1), Cohen’s d = .82, t(48) = 7.08, p < .001.
Table 1.
Descriptive Statistics and Correlations
| Variable | M | SD | Zero-order correlation
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |||
| 1. T1 PTSD total | 68.8 | 24.4 | |||||||||||||
| 2. T1 reexperiencing | 19.4 | 8.2 | .90*** | ||||||||||||
| 3. T1 effortful avoidance | 11.0 | 3.6 | .50*** | .36* | |||||||||||
| 4. T1 numbing | 14.1 | 9.7 | .88*** | .72*** | .39** | ||||||||||
| 5. T1 hyperarousal | 16.1 | 10.4 | .81*** | .66*** | .24 | .54*** | |||||||||
| 6. T1 trauma reactivity | 1.4 | 4.6 | −.10 | −.09 | .15 | −.20 | −.03 | ||||||||
| 7. T1 avoidant coping | 68.8 | 29.1 | .48*** | .48*** | .48** | .37** | .31* | −.15 | |||||||
| 8. T1 approach coping | 69.5 | 21.1 | −.35** | −.30* | −.03 | −.32* | −.36* | .12 | −.23 | ||||||
| 9. T2 PTSD total | 47.0 | 28.8 | .68*** | .61*** | .29* | .48*** | .72*** | −.02 | .42** | −.24 | |||||
| 10. T2 reexperiencing | 13.8 | 8.5 | .51*** | .50*** | .11 | .31* | .60*** | .03 | .37** | −.15 | .89*** | ||||
| 11. T2 effortful avoidance | 7.9 | 4.3 | .60*** | .53*** | .51*** | .41** | .54*** | −.05 | .52*** | −.25 | .77*** | .60*** | |||
| 12. T2 numbing | 9.2 | 9.6 | .66*** | .52*** | .29* | .58*** | .62*** | −.01 | .30* | −.28 | .85*** | .62*** | .59*** | ||
| 13. T2 hyperarousal | 24.2 | 8.2 | .61*** | .58*** | .22 | .37** | .71*** | −.04 | .37** | −.18 | .93*** | .83*** | .67*** | .68*** | — |
Note. N = 49. T1 = Time 1; T2 = Time 2; Posttraumatic Stress Disorder (PTSD) total = total severity score for the Clinician-Administered PTSD Scale (CAPS); reexperiencing, effortful avoidance, numbing, and hyperarousal = severity scores for the PTSD symptom clusters.
p < .05.
p < .01.
p < .001.
To examine coping style as a moderator of the relationship between trauma reactivity and PTSD symptom severity, we performed a series of multiple regressions. We entered T2 PTSD symptom severity as the dependent variable (DV) and entered trauma reactivity, coping style, and the interaction of coping style and trauma reactivity as independent variables (IVs), while also controlling for T1 PTSD symptom severity. See Table 1 for descriptive statistics and correlation coefficients for these variables. Results of the regression equations are presented in Table 2.1
Table 2.
Regression Analyses of Coping Styles Moderating the Relationship Between T1 Trauma Reactivity (TR) and T2 Posttraumatic Stress Disorder (PTSD) Symptom Severity
| Dependent/independent variable | β | Squared semi-partial r | R2/ΔR2 | Model F |
|---|---|---|---|---|
| T2 PTSD symptoms | 14.03*** | |||
| 1. T1 PTSD symptoms | .67*** | .34 | .46 | |
| 2. TR | .02 | .00 | .02 | |
| Avoidant coping | .17 | .02 | ||
| 3. TR × Avoidant Coping | .30* | .08 | .08 | |
| T2 PTSD reexperiencing symptoms | 5.91*** | |||
| 1. T1 reexperiencing symptoms | .45** | .16 | .25 | |
| 2. TR | .05 | .00 | .03 | |
| Avoidant coping | .22 | .04 | ||
| 3. TR × Avoidant Coping | .28* | .07 | .07 | |
| T2 PTSD effortful avoidance symptoms | 6.70*** | |||
| 1. T1 effortful avoidance symptoms | .36* | .09 | .26 | |
| 2. TR | −.07 | .00 | .10 | |
| Avoidant coping | .37* | .09 | ||
| 3. TR × Avoidant Coping | .13 | .02 | .02 | |
| T2 PTSD numbing symptoms | 10.03*** | |||
| 1. T1 numbing symptoms | .64*** | .33 | .34 | |
| 2. TR | .07 | .01 | .02 | |
| Avoidant coping | .16 | .02 | ||
| 3. TR × Avoidant Coping | .36** | .12 | .12 | |
| T2 PTSD hyperarousal symptoms | 13.87*** | |||
| 1. T1 hyperarousal symptoms | .67*** | .41 | .50 | |
| 2. TR | −.02 | .00 | .03 | |
| Avoidant coping | .20 | .03 | ||
| 3. TR × Avoidant Coping | .18 | .03 | .03 | |
| T2 PTSD symptoms | 10.07*** | |||
| 1. T1 PTSD symptoms | .68*** | .40 | .46 | |
| 2. TR | .07 | .00 | .01 | |
| Approach coping | −.03 | .00 | ||
| 3. TR × Approach Coping | .12 | .01 | .01 | |
| T2 PTSD reexperiencing symptoms | 3.78** | |||
| 1. T1 reexperiencing symptoms | .50*** | .22 | .25 | |
| 2. TR | .08 | .01 | .01 | |
| Approach coping | −.02 | .00 | ||
| 3. TR × Approach Coping | .03 | .00 | .00 | |
| T2 PTSD effortful avoidance symptoms | 5.76*** | |||
| 1. T1 Effortful avoidance symptoms | .51*** | .25 | .26 | |
| 2. TR | −.09 | .01 | .07 | |
| Approach coping | −.25 | .06 | ||
| 3. TR × Approach Coping | .13 | .01 | .01 | |
| T2 PTSD numbing symptoms | 6.93*** | |||
| 1. T1 numbing symptoms | .58*** | .29 | .34 | |
| 2. TR | .14 | .02 | .02 | |
| Approach coping | −.15 | .02 | ||
| 3. TR × Approach Coping | .17 | .03 | .03 | |
| T2 PTSD hyperarousal symptoms | 12.01*** | |||
| 1. T1 Hyperarousal symptoms | .74*** | .47 | .50 | |
| 2. TR | −.01 | .00 | .01 | |
| Approach coping | .06 | .00 | ||
| 3. TR × Approach Coping | .11 | .02 | .01 | |
Note. Degrees of freedom for the F statistics = 4, 44. T1 = Time 1; T2 = Time 2.
p < .05.
p < .01.
p < .001.
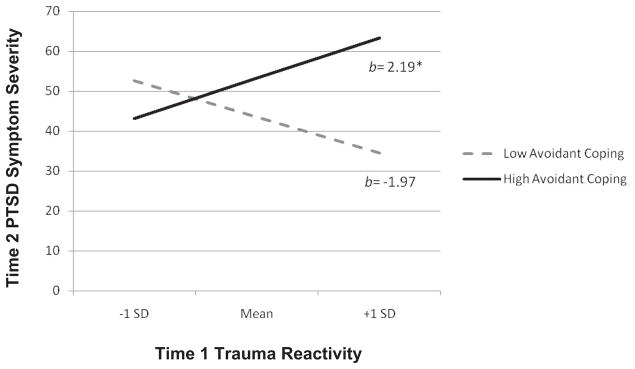
In the regression equation testing avoidant coping as the moderator, the T1 Avoidant Coping × Trauma Reactivity interaction was significantly associated with T2 total PTSD symptom severity after controlling for T1 PTSD symptom severity (β = .30, p < .01). Following Holmbeck’s (2002) methods for probing significant interaction effects, post hoc regressions were conducted to compute simple slopes of the conditional effects of trauma reactivity on T2 PTSD symptoms for participants with high (i.e., 1 SD above the mean) and low (i.e., 1 SD below the mean) avoidant coping scores. As demonstrated in Figure 1, trauma reactivity was positively associated with PTSD symptom severity for relatively high endorsers of avoidant coping, with a significant slope (β = .35, p < .05). In contrast, there was a nonsignificant trend for a negative association between trauma reactivity and PTSD symptom severity for relatively low endorsers of avoidant coping (β = −.32, p = .06).
Figure 1.
Regression lines for associations between trauma reactivity and posttraumatic stress disorder symptoms at Time 2 as moderated by avoidant coping. b = unstandardized regression coefficient (i.e., simple slope); SD = standard deviation. * p < .05.
In an effort to confirm that these results were not due to the content overlap between avoidant coping and the behavioral avoidance PTSD symptoms, we conducted secondary analyses to examine the associations among trauma reactivity, avoidant coping, and four PTSD symptom clusters (reexperiencing, effortful avoidance, numbing, and hyperarousal) among the full sample. The series of regression equations in which avoidant coping was tested as a moderator of the relationships between trauma reactivity and the four PTSD symptom clusters revealed a similar pattern of results for reexperiencing and numbing symptoms (Table 2). The T1 Avoidant Coping × Trauma Reactivity interaction was significantly associated with both T2 reexperiencing and numbing symptom severity. Post hoc probing revealed that trauma reactivity was positively associated with reexperiencing and numbing symptom severity for relatively high endorsers of avoidant coping, with significant slopes (β = .35, p < .05, for reexperiencing; β = .47, p < .01, for numbing). In contrast, the associations between trauma reactivity and reexperiencing and numbing symptom severity for relatively low endorsers of avoidant coping were negative but nonsignificant (β = −.25, p = .22, for reexperiencing; β = −.32, p = .08, for numbing).
The T1 Avoidant Coping × Trauma Reactivity interaction was not significantly associated with T2 effortful avoidance or hyper-arousal symptom severity (Table 2). However, T1 avoidant coping was a significant predictor of T2 active avoidance symptoms. Given that the Avoidant Coping × Trauma Reactivity interaction did not predict active avoidance symptoms, the results of our primary analyses cannot be attributed solely to content overlap between avoidant coping measure and effortful avoidance symptoms of PTSD.
To assess whether the Avoidant Coping × Trauma Reactivity interaction predicted PTSD diagnostic status, we conducted a logistic multiple regression with T2 PTSD diagnostic status as the DV and trauma reactivity, coping style, and the interaction of coping style and trauma reactivity were entered as IVs, while also controlling for T1 PTSD diagnostic status. While the overall model was not significant, χ2(4) = 7.72, p = .10, a significant main effect did emerge for avoidant coping, B = 0.03, p < .05.
A parallel set of linear and logistic regression equations computed with approach coping style as the moderator revealed no significant main effects or interactions involving approach coping or trauma reactivity for total PTSD severity or the four PTSD clusters (Table 2). However, when predicting PTSD diagnostic status, in addition to a significant overall model, χ2(4) = 9.50, p = .05, approach coping emerged as a significant negative predictor (B = −0.05, p < .01).
Discussion
Earlier research has suggested that overreliance on avoidant coping strategies may interfere with natural recovery from traumatic events. However, the results of the current investigation suggest that this may only be true for individuals who are highly reactive to trauma reminders. The combination of high physiological reactivity and greater use of avoidant coping strategies may interfere with natural processing of trauma memories and therefore be associated with relatively more severe PTSD symptoms 3 months later (after initial PTSD symptoms have been statistically controlled). Inversely, for individuals who are less reliant on avoidant coping strategies, greater initial reactivity to the trauma monologue procedure was associated with relatively less severe PTSD symptoms 3 months postassault. However, this association was not statistically significant. Thus, the combination of high reactivity to trauma reminders and limited use of avoidant coping strategies may be conducive to natural recovery from traumatic memories. The current study provides the first empirical support for the theoretical assumption that avoidance would be more detrimental for individuals who are relatively more reactive to the trauma memory.
It appears that the moderating effect of avoidant coping on the relationship between trauma reactivity and PTSD symptoms may be particularly strong for reexperiencing and numbing symptoms. Given theoretical models that posit trauma survivors shift between the opposing internal responses of intrusion (or reexperiencing symptoms) and denial (of which numbing is a component) until the trauma resolves (Horowitz, 1986), it is not surprising that individuals who are less likely to naturally recover may have both sustained reexperiencing and numbing symptoms over time.
This pattern was specific to avoidant coping strategies. Although the current data suggest that avoidant coping may interfere with recovery of PTSD symptoms over time for some individuals, it does not yield support for approach coping as a facilitator of recovery. These null results may be at least partly explained by the study’s small sample size, which limited power to detect a small effect. However, it is also possible that approach and avoidant coping are not opposite effects, as evidenced by the relatively small and nonsignificant correlation coefficient (see Table 1) but may be orthogonal processes.
This study has a number of methodological strengths, including the longitudinal design and the timing of the first assessment within 1 month of the traumatic event. However, there are also methodological limitations to be considered when one is interpreting these results. First, although the analyses conducted for this study are consistent with Baron and Kenny’s (1986) definition of moderation, they are not consistent with Kraemer and colleagues’ stricter definition of moderation that requires the moderator to temporally precede the independent variable (Kraemer, Kiernan, Essex, & Kupfer, 2008). With no temporal precedence of the moderator, it is conceivable that trauma reactivity, rather than avoidant coping, could be conceptualized as the moderator. Finally, the study’s relatively small sample size may have contributed to the null findings regarding interaction effects when predicting PTSD diagnostic status. The limited number of participants who changed diagnostic status from T1 to T2 may have also contributed to the lack of power for detecting interaction effects in these analyses. These results suggest that, when predicting the categorical diagnostic status variable, coping alone may be the better predictor.
Avoidant coping and physiological reactivity to trauma reminders have been studied extensively, but separately, in relation to their role in risk for PTSD. In the current study (Table 1), we replicated the association between avoidant coping and PTSD symptoms commonly found in the literature (e.g., Benotsch et al., 2000) but not the association between trauma reactivity and PTSD symptoms (e.g., Blanchard et al., 1996). Because there are relatively few studies of the longitudinal relationships between physiologic reactivity to trauma narratives and PTSD symptoms over time and because at least one study has shown greater reactivity to be associated with lower symptoms longitudinally (Halligan, Michael, Wilhelm, Clark, & Ehlers, 2006), more research on this topic clearly is needed.
Although avoidance has been posited to impede natural recovery from negative emotions associated with the traumatic memory (Foa & Rothbaum, 1998; Keane & Barlow, 2002), data concerning how avoidant coping and physiological reactivity interact to predict PTSD symptoms over time are important to validate these models. Results from the current study provide support for the theory that these risk factors interact such that individuals who are relatively highly reliant on avoidant coping strategies and relatively highly reactive to trauma reminders may be at greatest risk of having their PTSD symptoms remain, or even increase, in the months following a traumatic event.
Because of longitudinal design of this study and the timing of the assessments, these results may help inform early intervention for trauma survivors. Early intervention efforts in the wake of trauma have been controversial, with mixed reports about effectiveness and concern that iatrogenic effects may be introduced (Feldner, Monson, & Friedman, 2007). The results of this investigation suggest that early intervention efforts may only be useful for certain subsets of trauma survivors. Survivors who are both relatively reliant on avoidant coping strategies and highly reactive when discussing their traumatic event may be less likely to recover without intervention and, therefore, might benefit from early intervention targeted at reducing the use of avoidance coping strategies. While additional research validating these results and addressing more complex interrelationships of PTSD risk factors is necessary, these results represent an important initial attempt to identify the interactive effects critical for understanding the process of early recovery from traumatic events.
Acknowledgments
This material is based upon work supported by a National Institute of Mental Health Grant R01-MH46992 awarded to Patricia A. Resick. Additional support was provided to Suzanne L. Pineles through a Career Development Award from the Department of Veterans Affairs. Portions of these results were presented at the 2008 annual meeting of American Psychological Association, Boston, MA. We thank Margaret Bauer for her assistance with this project.
Footnotes
We conducted similar regression equations with the same variables while also controlling for number of therapy sessions and crimes between assessments. These analyses yielded comparable results. Results available upon request from the first author.
Contributor Information
Suzanne L. Pineles, National Center for PTSD, Women’s Health Sciences Division, Veterans Affairs Boston Healthcare System and Department of Psychiatry, Boston University School of Medicine
Sheeva M. Mostoufi, National Center for PTSD, Women’s Health Sciences Division, Veterans Affairs Boston Healthcare System
C. Beth Ready, National Center for PTSD, Women’s Health Sciences Division, Veterans Affairs Boston Healthcare System.
Amy E. Street, National Center for PTSD, Women’s Health Sciences Division, Veterans Affairs Boston Healthcare System and Department of Psychiatry, Boston University School of Medicine
Michael G. Griffin, Department of Psychology, University of Missouri–St. Louis
Patricia A. Resick, National Center for PTSD, Women’s Health Sciences Division, Veterans Affairs Boston Healthcare System; Department of Psychiatry, Boston University School of Medicine; and Department of Psychology, Boston University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. doi:1110.1037/0022-3514.1151.1176.1173. [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Brailey K, Vasterling JJ, Uddo M, Constans JI, Sutker PB. War zone stress, personal and environmental resources, and PTSD symptoms in Gulf War veterans: A longitudinal perspective. Journal of Abnormal Psychology. 2000;109:205–213. doi:210.1037/0021-1843X.1109.1032.1205. [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Buckley TC, Taylor AE, Vollmer A, Loos WR. Psychophysiology of posttraumatic stress disorder related to motor vehicle accidents: Replication and extension. Journal of Consulting and Clinical Psychology. 1996;64:742–751. doi: 10.1037//0022-006x.64.4.742. doi:710.1037/0022-1006X.1064.1034.1742. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG. Processing threatening information in posttraumatic stress disorder. Journal of Abnormal Psychology. 1995;104:537–541. doi: 10.1037//0021-843x.104.3.537. doi:510.1037/0021-1843X.1104.1033.1537. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Monson CM, Friedman MJ. A critical analysis of approaches to targeted PTSD prevention: Current status and theoretically derived future directions. Behavior Modification. 2007;31:80–116. doi: 10.1177/0145445506295057. doi:110.1177/0145445506295057. [DOI] [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. doi: 10.1037/0033-2909.99.1.20. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO. Treating the trauma of rape: Cognitive–behavioral therapy for PTSD. New York, NY: Guilford Press; 1998. [Google Scholar]
- Griffin MG, Resick PA, Mechanic MB. Objective assessment of peritraumatic dissociation: Psychophysiological indicators. American Journal of Psychiatry. 1997;154:1081–1088. doi: 10.1176/ajp.154.8.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutner CA, Pineles SL, Griffin MG, Bauer MR, Weierich MR, Resick PA. Psychophysiological predictors of posttraumatic stress disorder. Journal of Traumatic Stress. doi: 10.1002/jts.20582. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halligan SL, Michael T, Wilhelm FH, Clark DM, Ehlers A. Reduced heart rate responding to trauma reliving in trauma survivors with PTSD: Correlates and consequences. Journal of Traumatic Stress. 2006;19:721–734. doi: 10.1002/jts.20167. doi:710.1002/jts.20167. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations [Special issue on methodology and design] Journal of Pediatric Psychiatry. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Horowitz M. Stress response syndromes. Northvale, NJ: Aroson; 1986. [Google Scholar]
- Keane TM, Barlow DH. Posttraumatic stress disorder. In: Barlow DH, editor. Anxiety and its disorder: The nature and treatment of anxiety and panic. New York, NY: Guilford Press; 2002. pp. 418–452. [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. doi: 10.1037/1040-3590.10.2.90. [DOI] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27(2 Suppl):S101–S108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. doi:110.1037/0278-6133.1027.1032(Suppl.).S1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for rape victims: A treatment manual. Thousand Oaks, CA: Sage; 1993. [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5:455–475. doi:410.1002/jts.2490050309. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM–III–Revised–Patient Edition, With Psychotic Screen (SCID-I/P W/PSY SCREEN) Washington, DC: American Psychiatric Press; 1990. [Google Scholar]
- Tobin DL, Holroyd KA, Reynolds RV, Wigal JK. The hierarchical factor structure of the Coping Strategies Inventory. Cognitive Therapy and Research. 1989;13:343–361. doi:310.1007/BF01173478. [Google Scholar]
- Tobin DL, Holroyd KA, Reynolds VC. Unpublished manuscript. Department of Psychology, Ohio University; Athens: 1984. User’s manual for the Coping Strategies Inventory. [Google Scholar]
- Yehuda R, McFarlane AC, Shalev AY. Predicting the development of posttraumatic stress disorder from the acute response to a traumatic event. Biological Psychiatry. 1998;44:1305–1313. doi: 10.1016/s0006-3223(98)00276-5. doi:1310.1016/S0006-3223(1398)00276-00275. [DOI] [PubMed] [Google Scholar]