Abstract
Objective
We conducted a long-term follow-up (LTFU) assessment of participants from a randomized controlled trial comparing cognitive processing therapy (CPT) with prolonged exposure (PE) for posttraumatic stress disorder (PTSD). Competing hypotheses for positive outcomes (i.e., additional therapy, medication) were examined.
Method
Intention-to-treat (ITT) participants were assessed 5–10 years after participating in the study (M = 6.15, SD = 1.22). We attempted to locate the 171 original participants, women with PTSD who had experienced at least one rape. Of 144 participants located, 87.5% were reassessed (N = 126), which constituted 73.7% of the original ITT sample. Self-reported PTSD symptoms were the primary outcome. Clinician-rated PTSD symptoms, comorbid diagnoses, and self-reported depression were secondary outcomes.
Results
Substantial decreases in symptoms due to treatment (as reported in Resick, Nishith, Weaver, Astin, & Feuer, 2002) were maintained throughout the LTFU period, as evidenced by little change over time from posttreatment through follow-up (effect sizes ranging from pr = .03 to .14). No significant differences emerged during the LTFU between the treatment conditions (Cohen’s d = 0.06–0.29). The ITT examination of diagnostics indicated that 22.2% of CPT and 17.5% of PE participants met the diagnosis for PTSD according to the Clinician-Administered PTSD Scale (Blake et al., 1995) at the LTFU. Maintenance of improvements could not be attributed to further therapy or medications.
Conclusions
CPT and PE resulted in lasting changes in PTSD and related symptoms over an extended period of time for female rape victims with extensive histories of trauma.
Keywords: cognitive processing therapy, prolonged exposure, posttraumatic stress disorder, long-term outcomes, randomized controlled trial
Several treatment guidelines for posttraumatic stress disorder (PTSD) have concluded that cognitive-behavioral treatments (CBTs) are efficacious and are recommended as first-line treatments (Cahill, Rothbaum, Resick, & Follette, 2009; Institute of Medicine, 2007; VA/DoD Guideline Working Group, 2010). The specific CBT protocols of cognitive processing therapy (CPT; Chard, 2005; Monson et al., 2006; Resick et al., 2008; Resick, Nishith, Weaver, Astin, & Feuer, 2002; Resick & Schnicke, 1992) and prolonged exposure (PE; Foa et al., 1999, 2005; Foa, Rothbaum, Riggs, & Murdock, 1991; Schnurr et al., 2007) have both been demonstrated to be efficacious in ameliorating PTSD and comorbid depression, anxiety, guilt, and anger. Both protocols are currently being disseminated throughout U.S. Veterans Affairs (VA) facilities and various branches of the military (Karlin et al., 2010).
One important remaining question is whether PTSD symptom reductions resulting from CBT are long lasting. Follow-up assessments in CBT trials have typically been short (3–6 months). Although some studies have followed participants 1 or more years (Echeburúa, de Corral, Sarasua, & Zubizarreta, 1996; Echeburúa, de Corral, Zubizarreta, & Sarasua, 1997; Foa et al., 1999, 2005; Neuner, Schauer, Klaschik, Karunakara, & Elbert, 2004), most of these studies had small samples or followed only those who completed treatment and not the intention-to-treat (ITT) sample. There are two notable exceptions. Hien et al. (2009) conducted a multisite trial comparing seeking safety with an educational control condition for substance dependence and comorbid PTSD symptoms (either full or partial PTSD diagnosis). The ITT sample was followed for 1 year (N = 215 at 1-year follow-up). Unfortunately, treatment dropout was high, with only 12% of the sample completing the 12-session protocol, and there were no significant improvements in substance dependence. However, there were overall improvements in PTSD symptoms, which were maintained over the follow-up period; the two conditions did not differ significantly. Schnurr et al. (2003) followed participants in a large VA multisite trial for up to 24 months after completion of a 30-week trauma-focused group treatment. Although ITT analyses revealed that CBT demonstrated only modest efficacy and did not improve symptoms more than in the control condition, there was no apparent decrement in improvements over the follow-up period. Tarrier and Sommerfield (2004) conducted one of only two studies that followed participants for 5 years after treatment. Their randomized controlled trial found both cognitive therapy and imaginal exposure to be highly efficacious. Although the follow-up sample was small (n = 32 of 54 in the ITT sample) and excluded treatment dropouts (but included those who did not start), they found that both treatments produced good and lasting outcomes. Cognitive therapy was significantly more efficacious at follow-up than was imaginal exposure, with none of the cognitive therapy participants meeting criteria for PTSD 5 years later. Four of 17 imaginal exposure participants met PTSD criteria, a percentage similar to that for those who had retained their diagnosis at posttreatment and 6-month follow-up (Tarrier et al., 1999).
The only other PTSD treatment study that examined participants 5 or more years after treatment was a study of eye movement desensitization and reprocessing therapy by Macklin et al. (2000). Thirteen of 17 veterans who had been treated, and 14 who had not been treated, were assessed 5 years following treatment. They found that the modest gains observed at posttreatment had not only disappeared at follow-up, but participants had significantly worsened from their pretreatment scores.
As this review reveals, there is a dearth of literature on long-term outcomes of PTSD treatment with large samples, particularly for treatments such as CPT and PE, and there are methodological limitations of these studies. The purpose of this study is to report the findings from a long-term follow-up (LTFU) assessment of a randomized controlled trial comparing CPT with PE as the control condition because it was the most established treatment at the time, as well as a waiting list control (Resick et al., 2002). In the original trial, participants improved markedly with both CPT and PE compared with the waiting list condition; CPT and PE did not statistically differ on PTSD or depression outcomes but did differ on guilt cognitions and physical symptoms (Galovski, Monson, Bruce, & Resick, 2009; Resick et al., 2002), with CPT resulting in fewer guilt cognitions and physical symptoms compared with PE. There were small to medium effect sizes favoring CPT over PE on every measure in the ITT sample through the 9-month follow-up.
For the current study, follow-up assessments were conducted 5–10 years after treatment with the goal of examining long-term outcomes among all participants who were randomized in the original trial, except those who were removed from the study due to meeting the exclusion criteria during treatment. Although the original study did not include assessment of participants if they dropped out of treatment, the current study includes all of the originally randomized participants, irrespective of treatment completion. Self-reported PTSD symptoms were the primary outcome; self-reported depression severity and several common comorbid diagnoses were also examined as outcomes. In addition to examining self-report measures, we examined diagnoses of PTSD, major depressive disorder, panic disorder, and substance dependence/abuse according to clinician interview. Further, we examined whether receiving medication or psychotherapy after participation in the trial accounted for any positive findings during the LTFU. Finally, we examined clinically significant improvement in PTSD symptoms.
Method
The Institutional Review Board (IRB) of the University of Missouri–St. Louis approved the protocol, and participants gave written informed consent prior to enrollment that included follow-up contact information. In the original trial, the 9-month follow-up was not originally proposed. When the IRB approved recontacting participants for the 9-month follow-up (Resick et al., 2002), we requested approval from the participants for possible other follow-ups, and participants supplied us again with updated follow-up contact information. The IRB later approved the LTFU data collection specifically. During the data collection, the first author moved to the Department of Veterans Affairs, and under its requirements, the IRB of the VA Boston Healthcare System provided oversight of data analyses.
Participants
The parent study (Resick et al., 2002) included 171 adult women randomized into the study who had experienced at least one rape a minimum of 3 months prior to seeking treatment (no upper limit). Most participants (86%) had experienced other traumatic victimizations in addition to the index rape. Forty-one percent of the sample had been sexually abused (genital contact) as children. The participants reported an average of 6.4 adult crime incidents (SD = 4.9) in addition to the index rape. Participants on medications were stabilized per psychiatric consult based on type of medication. Participants had to agree to refrain from other trauma-focused psychotherapy but were permitted to continue with stabilized medications or ongoing supportive therapy.
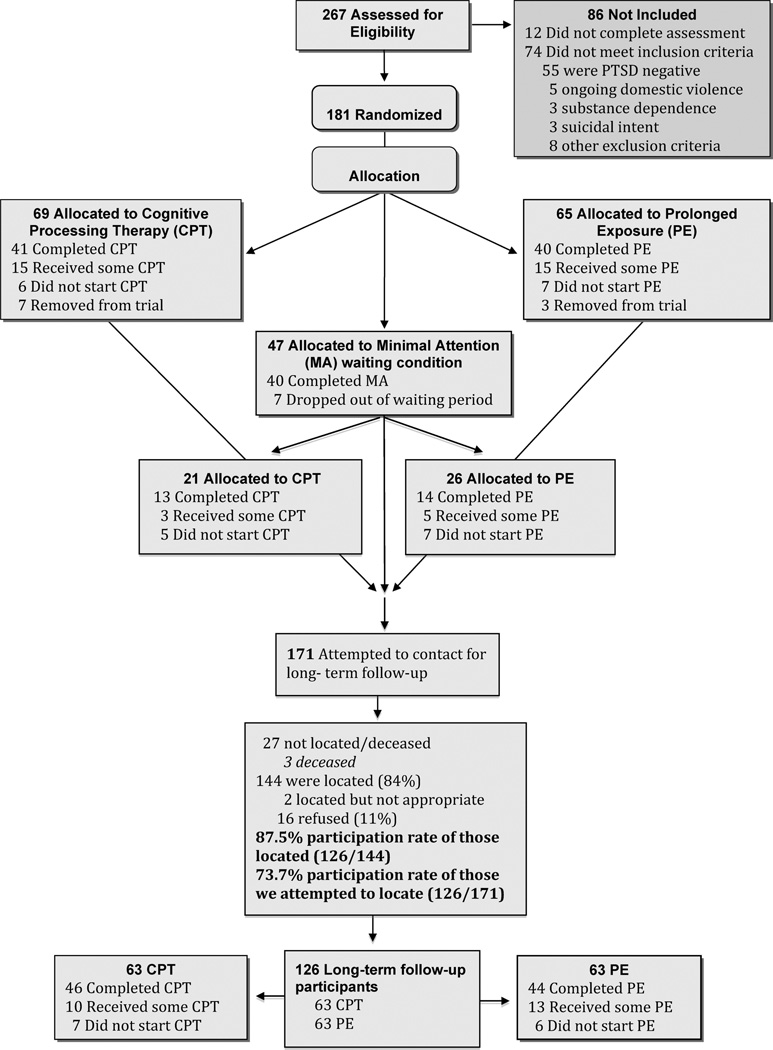
Exclusion criteria included current psychosis, suicidal intent, active self-harm behavior, current dependence on drugs or alcohol, and illiteracy. Neither personality disorders nor dissociation or dissociative disorders or any other Axis I disorder was excluded. Participants reporting current stalking or involvement in an abusive relationship were excluded. In the case of marital rape, participants must have been out of the relationship for at least 6 months. Typical for studies of the time (Foa et al., 2005), anyone who met the exclusion criteria during treatment (e.g., change of medication) was allowed to complete treatment, but no further data were collected (n = 10; see Figure 1).
Figure 1.
CONSORT flow chart for the entire study, including the long-term follow-up.
Figure 1, the CONSORT chart, shows the flow of participants through the parent study and LTFU (see Table 1 for demographic information at the pretreatment and LTFU assessment occasions). A paired-sample t test indicated that the number of years of education reported at the LTFU was significantly more than the number of years reported at the pretreatment assessment, t(118) = 5.31, p < .001. A related-samples Friedman’s two-way analysis of variance (ANOVA) indicated that on average participants endorsed a higher income category at the LTFU (mean rank = 1.73) compared with the pretreatment assessment (mean rank = 1.27), χ2(1, N = 73) = 24.01, p < .001. A repeated-measures logistic regression indicated that a higher proportion of participants indicated being in a committed relationship at the LTFU (39%) compared with the pretreatment assessment (24%), Wald χ2(1, N = 170) = 7.40, p < .01.
Table 1.
Demographic Characteristics for Participants in the Two Treatment Conditions
| Pretreatment | |||
|---|---|---|---|
| Characteristic | ITT sample (n = 171) |
LTFU sample (n = 126) |
LTFU (n = 126) |
| Age: M (SD) | 31.99 (9.98) | 32.11 (9.83) | 38.27 (9.64) |
| Years of education: M (SD) | 14.36 (2.34) | 14.43 (2.41) | 15.20 (2.65) |
| Race/ethnicity: n (%) | |||
| African American | 43 (25.1) | 26 (20.6) | 26 (20.6) |
| Caucasian | 121 (70.8) | 95 (75.4) | 93 (73.8) |
| Hispanic | 2 (1.2) | 1 (0.8) | 1 (0.8) |
| Asian | 1 (0.6) | 1 (0.8) | 1 (0.8) |
| Native American | 2 (1.2) | 2 (1.6) | 1 (0.8) |
| Other | 2 (1.2) | 1 (1.2) | 4 (3.2) |
| Marital status: n (%) | |||
| Single | 82 (48.5) | 59 (47.2) | 43 (35.5) |
| Married | 34 (20.1) | 30 (24.0) | 43 (35.5) |
| Separated | 9 (5.3) | 5 (4.0) | 6 (5.0) |
| Divorced | 36 (21.2) | 25 (20.0) | 25 (20.7) |
| Living with someone | 7 (4.1) | 6 (4.8) | 4 (3.3) |
| Widowed | 1 (0.6) | 0 (0.0) | 0 (0.0) |
| Annual income: n (%) | |||
| Less than $5,000 | 19 (18.3) | 11 (14.5) | 5 (4.2) |
| $5,000–$10,000 | 12 (11.5) | 10 (13.2) | 10 (8.3) |
| $10,001–$20,000 | 26 (25.0) | 18 (23.7) | 18 (15.0) |
| $20,001–$30,000 | 17 (16.3) | 13 (17.1) | 19 (15.8) |
| $30,001–$50,000 | 12 (11.5) | 10 (13.2) | 32 (26.7) |
| More than $50,000 | 18 (17.3) | 14 (18.4) | 36 (30.0) |
Note. ITT = intention-to-treat; LTFU = long-term follow-up.
At the LTFU, participants reported a number of negative or traumatic events. Overall, 9% reported experiencing sexual assault, 17% domestic violence, 6% the death of someone in their household, 60% the death of a significant other, 12.5% the homicide of a significant other, 39% other crimes, 18% a serious accident, and 35% a serious illness. None of these percentages significantly varied as a function of treatment condition (all χ2s < 3.36, all ps > .19).
Measures
The PTSD Symptom Scale (PSS; Foa, Riggs, Dancu, & Rothbaum, 1993) is a 17-item scale that assesses all of the criteria for PTSD according to the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; American Psychiatric Association, 1994). For these analyses we used the total frequency score. The PSS was completed at all major assessment periods and once a week during treatment, yielding 11 data points. The Cronbach’s alpha coefficient at the LTFU was .93.
The other self-report and diagnostic interview measures were given on five occasions: pretreatment, posttreatment, and at 3-month, 9-month, and LTFU. The Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) is a 21-item self-report questionnaire widely used in research on depression (Beck, Steer, & Garbin, 1988). Cronbach’s alpha at LTFU was .95. The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) is a semistructured interview used to assess PTSD severity and determine diagnostic status. For each symptom, an independent clinician rated two separate dimensions—frequency and intensity of symptoms—on a scale ranging from 0–4. For a symptom to be considered clinically significant, it had to meet threshold criteria on both dimensions (i.e., at least a 1 on frequency and a 2 on intensity). The Structured Clinical Interview for DSM–IV (SCID; First, Spitzer, Gibbon, & Williams, 1996) is a diagnostic interview based on criteria from the DSM–IV. Three modules were used to assess mood disorders (MDD), panic disorder (PD), and substance use disorders. Each CAPS and SCID-CV interview was audio-recorded. Current diagnosis was based on the current time frame for the respective module, while diagnosis since treatment completion used the “lifetime” modules of the interview measures with the instruction “Since you completed treatment with us on ….”
Assessments were conducted by a team of assessors working on two studies simultaneously: a dismantling study of CPT (Resick et al., 2008) and this LTFU project. The procedure for training and preventing interviewer drift is described in more detail in Resick et al. (2008). Independent assessors were unaware of treatment assignment regardless of study. To determine reliability, interviews were drawn randomly from both studies at any of the intake or follow-up sessions. Unfortunately, of the 550 possible interviews in the two studies, only five were drawn from the LTFU for reliability assessment. Overall, there was 100% agreement on CAPS and PTSD diagnosis, 90% agreement on MDD, and 92% agreement on PD. Cronbach’s alpha for the CAPS severity score at LTFU was .94.
Therapies
CPT is predominantly a cognitive therapy; PE is predominantly an exposure therapy. Manuals for the therapies were Resick and Schnicke (1993) and Foa, Hearst, Dancu, Hembree, and Jaycox (1994), respectively. Both active treatments consisted of 13 hr of therapy administered twice per week but were configured slightly differently to maintain protocol integrity as to how the treatments were practiced at the time. PE started with two 1-hr sessions and then changed to seven 90-min sessions to accommodate imaginal exposures. PE also required approximately 90 min of homework per day: 45 min of listening to the recorded exposure sessions and 45 min of in-vivo exposure. CPT was administered with 10 1-hr sessions and two 90-min sessions (to equate with session time for PE). CPT requires less homework time than does PE.
Procedures
Potential participants were recruited widely throughout the region and treated at a trauma center located on a university campus. Following initial assessment and invitation into the trial, participants were randomized by the data manager to CPT, PE, or waiting list. The waiting list participants were also randomized into CPT or PE in case they did not improve by the end of the waiting period and wanted treatment. Because improvements were similar to those for the delayed treatment participants (Resick et al., 2002), they were combined with the original CPT or PE groups for follow-up analyses. For the LTFU, all participants who were randomized into the trial (and not removed from the trial at any point) were invited to participate, regardless of whether and how much therapy they received (n = 171).
A number of steps were taken to locate participants for the LTFU assessments. We began with contact information collected during earlier assessments. Next, we attempted to locate people through various websites available to the general public or specifically geared toward journalists. When those options were exhausted, we enlisted the location assistance of a survey research firm. Once located with identity confirmed, former participants were invited to participate. If they still lived locally, they were invited to return to the university to complete the assessments. If they had moved out of the area, they were interviewed by telephone by clinicians and were mailed the packet of self-report measures to complete. Prior research with both the CAPS and the SCID-CV has established that in-person and telephone assessments are comparable (Aziz & Kenford, 2004; Crippa et al., 2008; Rohde, Lewinsohn, & Seeley, 1997). Assessors were again unaware of assigned treatment condition and treatment status of participants at the LTFU. There were no adverse events associated with the follow-up assessments. Of course, over such a long time period the participants had experienced many adverse events, but none were attributed to the therapy they had received years before or to the LTFU assessment itself. Participants were paid $75 for their participation.
Data Analyses
Linear mixed-effects modeling was used to examine change over time in the outcomes using HLM 6: Hierarchical Linear and Nonlinear Modeling (Raudenbush, Bryk, & Congdon, 2005). This approach is uniquely suited to the current data and offers several advantages over more traditional approaches (e.g., repeated-measures ANOVA). In this study there was considerable variability in the timing of assessments, which was readily handled using the mixed-effects approach, with time analyzed as number of months1 since baseline assessment. Because mixed-effects models are also robust to unbalanced designs (i.e., variability in total number of assessments), we were able to examine our ITT sample without using any missing data algorithms.
Piecewise modeling of the outcomes over time was undertaken to estimate different slopes from pre- to posttreatment (Epoch 1) and posttreatment to LTFU (Epoch 2) using procedures described by Singer and Willett (2003). Because PSS data were collected multiple times during treatment and at the major assessment points, we were able to model both slope and level changes across the epochs. To accomplish this, the following three time variables were included: (a) number of months since baseline (i.e., time), (b) a dummy-coded variable indicating whether each assessment was during (coded as 1) or after (coded as 0) treatment (i.e., epoch), and (c) the product of these two variables, which represents the change in slope across the two epochs. With Epoch 2 (i.e., the follow-up period) coded as 0, the regression coefficients for the time variable provided an estimate of change over time during the follow-up period, which was the only estimate of interest for the current study.2
Although the approach just described better captures the processes occurring during and after treatment, having only two assessment points for the first epoch for the outcomes collected on five occasions (i.e., BDI and CAPS) precluded a test of level change across the epochs. Therefore, these piecewise models were conducted in a different manner. First, the time variable was rescored so that it was zero for every participant at the posttreatment assessment. Thus, the time variable for the follow-up time periods was number of months since the posttreatment assessment, while this time variable for the baseline assessment was set at −1 multiplied by the number of months between the baseline and posttreatment assessment. For example, if the original time variable for a participant consisted of 0, 2.4, 5.5, 11.7, and 73.7 months for the baseline, posttreatment, 3-month follow-up, 9-month follow-up, and LTFU assessments, respectively, then the recoded time variable for this participant would be coded as −2.4, 0, 3.1, 9.3, and 71.3 months. A second time variable that represented the number of months prior to the baseline assessment (e.g., coded as −2.4, 0, 0, 0, and 0 for the previous example) was created. When these two time variables were entered into the Level 1 equation predicting the outcome variable, the regression coefficient for first time variable provided an estimate of change during Epoch 2, while the regression coefficient for the second time variable represented the difference in the rate of change over time between the two epochs (Singer & Willett, 2003). Because the current article is exclusively concerned with Epoch 2, we report the estimates for the first time variable (i.e., change over time during the follow-up period).
We examined several alternative ways to model change over time. As indicated by the deviance statistic (a log-likelihood-based goodness-of-fit statistic) and the amount of within-subject variance accounted for, a linear–linear change model (linear change in both epochs as modeled by the number of months since baseline assessment) fit the data best for the PSS data collected across 11 assessment occasions and the CAPS and BDI collected across five assessment occasions.
All of the time coefficients described earlier were modeled as random effects that specify variation in the time coefficients across participants. To examine treatment effects, a dummy-coded treatment condition variable was included as a Level 2 predictor for each of the time coefficients described earlier (Cohen, Cohen, West, & Aiken, 2003). This enabled us to examine whether change over time during either epoch significantly varied as a function of treatment condition.3
For estimates of within-subject effect sizes, we report the partial correlation coefficients (pr) for each coefficient. Kirk (1996) suggested .10, .24, and .37 for small, medium, and large effect sizes, respectively. For estimates of between-groups effect sizes, we report Cohen’s d and use descriptors of effect size offered by Cohen (1988): d = 0.25 for small, .50 for medium, and .80 for large.
Power to detect group differences in change over time during Epoch 2 was determined by using the Monte Carlo method (Muthén & Muthén, 2002) with the Mplus statistical software (Muthén & Muthén, 1998–2009). A Monte Carlo simulation study can be used to determine sample size for a specific, hypothesized model (Muthén & Muthén, 2002). This method involves specifying parameter estimates for a given model and generating 10,000 data sets to determine the percentage of time the parameter estimates were statistically significant (at the p < .05 level). Therefore, we could determine power for the exact model that we were evaluating with the exact number of observations available (i.e., 588 observations with participants having either 1, 2, 3, 4, or 5 data points available; M = 3.44), using actual parameter estimates from the data analyses as starting values. This provided us with a precise estimate of power for the pertinent parameters (i.e., the Group × Time During Epoch 2 interaction). For the piecewise regression analysis with CAPS as the outcome variable (assessed at five time points), the power analysis indicated that we had a power of .88 to detect a medium effect size difference (pr = .24) between the two groups in change over time during Epoch 2 and a power of .60 to detect a small–medium difference (pr = .17). The power analysis for the PSS analysis (which included 11 assessment points) indicated that we had a power of .96 to detect a medium effect size difference (pr = .24) between the two groups in change over time during Epoch 2 and a power of .72 to detect a small–medium difference (pr = .17). Thus, the current study was adequately powered to detect meaningful differences between the two groups in change over time during the follow-up period.
To rule out the possibility that the results were accounted for by further psychotherapy after completing the program or medication use at the LTFU assessment, secondary analyses were conducted to evaluate whether these variables predicted outcomes at the LTFU. These analyses were conducted on a restricted sample of participants who provided these data (n = 124). However, these participants were not significantly different on demographic or clinical characteristics from participants who did not provide this information.
Results
Results of Tracking
We attempted to find and assess 171 women from the ITT sample. Of those, contact was never established with 24, and three had died. Of the remaining 144 with whom we established contact and verified previous participation, 16 (11%) declined to participate in the LTFU, and two were judged to be inappropriate due to incoherence. The final sample for the LTFU included 126 women who were assessed 4.5–10 years4 posttreatment; 87.5% (126/144) of these located participants (73.7% of the original sample) completed at least the diagnostic interviews, while 119 completed the entire assessment battery (see Figure 1). However, the use of mixed-effects regression allowed us to include the entire ITT sample in the analyses. The mean number of years from baseline to LTFU was 6.15 (SD = 1.22).
Symptoms Severity Outcomes
PSS (11 assessments)
Table 2 presents the coefficients depicting change over time during the follow-up period (i.e., Epoch 2). During Epoch 2, the CPT group did not exhibit significant change in PTSD symptoms, while the PE group exhibited a slight decrease in symptoms that approached significance (p = .06). The difference in the rate of change during the follow-up period between the groups also approached statistical significance (p = .06).
Table 2.
Results From Epoch 2 (LTFU) of the Piecewise Mixed Effects Regression Analyses Examining Long-Term Effects of CPT and PE
| Measure and approach | ba (SE) | pr/dM |
|---|---|---|
| PSS | ||
| PE | −0.03 (0.02) | 0.14 |
| CPT | 0.01 (0.02) | 0.06 |
| Difference between groups | 0.05 (0.03) | 0.29 |
| CAPS | ||
| PE | −0.02 (0.05) | 0.04 |
| CPT | 0.02 (0.04) | 0.05 |
| Difference between groups | 0.05 (0.06) | 0.12 |
| BDI | ||
| PE | 0.01 (0.02) | 0.03 |
| CPT | 0.02 (0.02) | 0.09 |
| Difference between groups | 0.01 (0.03) | 0.06 |
Note. All ps > .05. The partial correlation coefficient (pr) was reported as an effect size indicator for the within-subject effects, while Cohen’s d was reported for between-groups comparisons. LTFU = long-term follow-up; CPT = cognitive processing therapy; PE = prolonged exposure; PSS = PTSD Symptom Scale; CAPS = Clinician-Administered PTSD Scale; BDI = Beck Depression Inventory.
The metric of b is change in the outcome variable per month.
CAPS and BDI (five assessments)
Participants did not exhibit significant change in the CAPS during the follow-up period (b = −0.001, t = −0.03, ns, pr = .001). There was also no significant difference between the groups in the rate of change in the CAPS during the follow-up period. Similarly, participants did not exhibit significant change on the BDI during the follow up period (b = .02, t = 1.07, ns, pr = .08), and there was no difference between the groups in change over time during the follow-up period (see Table 2).
Potential Moderators
Of the 126 participants who provided LTFU data, the mean percentage of treatment sessions completed was 77% (SD = 38%), with no difference between the two treatment conditions (CPT = 78% vs. PE = 78%). At the LTFU, 73 (60%) of 121 participants indicated that they had received additional treatment since completing the trial, which did not significantly vary as a function of treatment condition (CPT = 59% vs. PE = 62%), χ2(1, N = 121) = 0.01, ns. However, only 15 (12%) of the LTFU sample indicated that the additional therapy they received was for trauma or PTSD, with no difference between treatment condition (CPT = 12% vs. PE = 13%), χ2(1, N = 121) = 0.10, ns. The number of treatment sessions ranged from 0 to 380, with a mean of 34.45 (SD = 68.03) and a median of 6. The distribution was right-skewed, with a modal number of sessions of 0 (n = 46) and a small number of participants (n = 13) reporting 100 or more additional treatment sessions. The number of treatment sessions attended did not significantly vary as a function of group (M = 28.79, SD = 55.90, and 40.20, SD = 40.20, for the CPT and PE conditions, respectively).5 Forty-seven (39%) participants indicated that they had started to take medication since completing the treatment protocol, with no difference between treatment condition (CPT = 41% vs. PE = 37%), χ2(1, N = 121) = 0.17, ns, and 41 (34%) indicated that they were currently taking medication, again with no difference between treatment condition (CPT = 34% vs. PE = 33%), χ2(1, N = 121) = 0.02.
Follow-up regression analyses revealed that the dichotomous variables indicating additional treatment and additional trauma/PTSD treatment did not predict LTFU outcomes on any variables. Number of sessions of therapy received during the LTFU was positively associated with each of the outcome variables. In other words, additional treatment following the trial was associated with worse outcomes at the LTFU assessment. Therefore, additional treatment could not account for the sustained treatment effects reported earlier. Starting medication during the LTFU was associated with higher CAPS and BDI at the LTFU. Participants who reported being prescribed medication at the LTFU assessment scored significantly higher on both of the outcomes. Again, the important aspect of these findings is that medication was associated with more symptoms at the LTFU and, therefore, could not account for the sustained treatment gains reported earlier.
Diagnosis, Relapse, Clinically Significant Improvement
As shown in Table 3, at pretreatment, 100% of participants met full criteria for PTSD on the CAPS in order to be enrolled in the trial, and many had comorbid diagnoses. The percentages and totals of ITT participants who met criteria for these disorders at the LTFU assessment are also presented in Table 3. Repeated-measures logistic regression was conducted to compare the proportions of PTSD, MDD, and PD diagnoses at the pretreatment assessments with the proportions of these diagnoses at the LTFU assessment. The small number of endorsements of alcohol dependence precluded us from completing this analysis for that outcome. The percentage of participants meeting diagnostic criteria for PTSD (OR = 0.003, p < .001) and MDD (OR = 0.15, p < .001) decreased over time, while the decrease in PD diagnosis was not significant (OR = 0.57, p = .12). No significant Time × Treatment Condition interactions emerged.
Table 3.
Means (and Standard Deviations) and Diagnostic Status of Participants Over Time Across the Two Treatment Conditions
| Variable | Pretreatment | LTFU | Effect size at long term (d) |
χ2 | ||||
|---|---|---|---|---|---|---|---|---|
| N | M (SD) | % | N | M (SD) | % | |||
| Measure | ||||||||
| CAPS total | ||||||||
| CPT | 83 | 73.76 (19.34) | 63 | 26.00 (23.35) | .004 | |||
| PE | 88 | 74.48 (19.53) | 63 | 25.90 (26.05) | ||||
| PSS total | ||||||||
| CPT | 82 | 29.13 (8.41) | 56 | 9.68 (10.38) | .02 | |||
| PE | 88 | 29.60 (8.52 | 56 | 9.89 (10.52) | ||||
| BDI | ||||||||
| CPT | 82 | 24.35 (9.82) | 56 | 9.41 (11.13) | .22 | |||
| PE | 86 | 22.93 (8.31) | 54 | 12.06 (12.68) | ||||
| Diagnosis | ||||||||
| Current PTSD | ns | |||||||
| CPT | 83 | 100 | 63 | 22.2 | ||||
| PE | 88 | 100 | 63 | 17.5 | ||||
| MDD lifetime/since Tx | ns | |||||||
| CPT | 68 | 85.3 | 39 | 56.4 | ||||
| PE | 74 | 83.8 | 44 | 54.5 | ||||
| MDD current | ns | |||||||
| CPT | 79 | 44.3 | 61 | 11.5 | ||||
| PE | 83 | 37.3 | 58 | 6.9 | ||||
| Alcohol lifetime/since Tx | ns | |||||||
| CPT | 70 | 40.0 | 40 | 10.0 | ||||
| PE | 77 | 51.9 | 42 | 9.5 | ||||
| Alcohol current | ns | |||||||
| CPT | 78 | 0.0 | 62 | 3.20 | ||||
| PE | 83 | 2.4 | 60 | 0 | ||||
| Panic lifetime/since Tx | ns | |||||||
| CPT | 69 | 20.3 | 36 | 8.3 | ||||
| PE | 76 | 18.4 | 42 | 21.4 | ||||
| Panic current | ns | |||||||
| CPT | 78 | 10.3 | 60 | 3.3 | ||||
| PE | 83 | 10.8 | 54 | 9.3 | ||||
Note. PTSD measured by the CAPS; other diagnoses based on the Structured Clinical Interview for DSM–IV. LTFU = long-term follow-up; CAPS = Clinician-Administered PTSD Scale; CPT = cognitive processing therapy; PE = prolonged exposure; PSS = PTSD Symptom Scale; BDI = Beck Depression Inventory; PTSD = posttraumatic stress disorder; MDD = major depressive disorder; Tx = treatment.
Of the 98 treatment completers who were assessed at LTFU, there were no differences between CPT and PE in PTSD diagnostic status. For CPT, 18.4% met criteria for PTSD (9/49); for PE, 14.3% met criteria (7/49). Calculating relapse presupposes that someone had recovered in order to relapse. To determine how many participants relapsed at LTFU, we examined participants for whom we had both posttreatment and long-term data. This necessitated only examining successful treatment completers at posttreatment who returned for the follow-up assessment (n = 74).
For the CPT group, there were 39 women who had both posttreatment and LTFU assessments who did not have PTSD at posttreatment. At LTFU, of the 39 who had recovered initially, eight were diagnosed with PTSD at the LTFU (20.5%). For the PE condition, there were 36 women at posttreatment who did not meet criteria for PTSD. At LTFU, only two had relapsed (5.6%). There was a marginally significant finding for PE to have less relapse than CPT at LTFU, χ2(1, N = 75) = 3.8, p = .057.
The relationship between diagnosis and medication use in the ITT sample was examined at the LTFU assessment. Medication use was marginally significantly associated with LTFU PTSD diagnosis, χ2(1, N = 121) = 3.5, p = .06. Of the participants at LTFU who exhibited PTSD, a higher proportion were on medication (12/41 = 29%) than not on medication (12/80 = 15%). There was no significant relationship between medication use and current MDD diagnosis, and few women had current depression. There was, however, a significant relationship between current medication use and MDD diagnosis during the LTFU, χ2(1, N = 78) = 6.5, p = .01. Of the 78 women for whom we had both lifetime MDD diagnosis and medication data in this sample, a higher proportion of women on medication at the LTFU assessment endorsed an MDD diagnoses (22/30 = 73%) sometime during the follow-up period compared with those who were not on medication (21/48 = 44%). Medication use was associated with higher rates of PTSD and MDD. Therefore, medication could not account for the positive outcome at the LTFU assessment.
Because diagnosis could change as a result of change in as little as one symptom, many PTSD studies also examine clinically significant change. Using the criteria of a decrease of 10 points on the CAPS as indicative of improvements in quality of life, as established by Lunney and Schnurr (2007), we examined how many ITT participants achieved at least a 10-point change on the CAPS from pretreatment to the LTFU and found that 93.4% of the CPT and 91.9% of the PE participants achieved this level of improvement. Using the Jacobson and Truax (1991) approach, a reliable clinical change on the CAPS is 20 points (Monson et al., 2008). Given that standard, 88.5% of CPT and 88.7% of PE participants improved by at least 20 points on the CAPS. On average, the CPT group improved by 48.8 points (SD = 26.4), and the PE group improved by 48.9 points (SD = 26.14). If one considers just those who completed treatment, 89.8% of CPT and 85.7% of PE participants improved at least 20 points. None of the percentages varied statistically across the two conditions. Only one person in each condition reported clinically significant worsening at the LTFU for ITT, and only one in PE for treatment completers.
Discussion
This study represents a methodologically rigorous attempt to assess the long-term impact of CBT on PTSD. In the original trial, participants receiving either CPT or PE showed marked improvements in PTSD and depression, from pretreatment to posttreatment. There were few differences between the two treatments in the outcomes. During the follow-up period, PE participants exhibited small decreases in self-reported PTSD symptoms that approached but did not reach statistical significance. Participants in the PE condition also tended (i.e., had an effect that approached but did not reach statistical significance) to have fewer people relapse based on PTSD diagnosis. The ITT examination of diagnostics indicates that 22.2% of CPT and 17.5% of PE participants met the CAPS diagnosis for PTSD at the LTFU. Importantly, the groups did not differ in the amount of improvement that was sustained over the long term. The maintenance of treatment gains throughout the follow-up period, on average 6 years, exhibited by both is impressive, especially considering that these women continued to experience life events that might impact their symptoms. The sustained treatment effects were not accounted for by further psychotherapy after completing one of these treatments or by medication usage at the LTFU. In fact, additional psychotherapy and medication were associated with worse outcomes. In the original trial (Resick et al., 2002), 20% of each group were considered to be nonresponders. Given the strong maintenance of the results of the trial, it might be concluded that those who started medications and received more therapy after the trial continued to be nonresponders.
The original and current follow-up study excluded as few participants as possible so the sample would represent the full range of PTSD clients seen in the community, including those with complex trauma histories and presentations. Only those with imminent harm, active psychosis, illiteracy, and substance dependence were referred for immediate care, and those with medication instability were included once their medications had been stabilized. We made great efforts to include as many participants as possible who were originally randomized to the trial. Therefore, these findings should generalize to women with PTSD and comorbid depression, anxiety disorders, personality disorders, and so forth.
Future research can address limitations of this study by conducting similar clinical trials and LTFU with samples that include men, wider ethnic diversity, and different types of trauma, such as combat. It is unknown whether other trauma populations will have the same long-term results. Because the LTFU was not preplanned, the follow-up assessment had a 5-year time span. Although linear mixed-effects modeling can account for variability in length of time between assessments, it is not clear if the results would have changed if the data had been collected at a single uniform time point. Strengths of the study include the high response rate for the LTFU and the inclusion of all randomized participants from the original trial, not just the treatment completers. It should be noted, however, that this sample includes women who never started treatment, about a quarter who dropped out before completing the full protocol, and some who were nonresponders initially. Despite that, this study found that over 85% of participants who were randomized to one of the two brief treatments reported clinically reliable improvements at an LTFU assessment conducted an average of 6 years later. Unlike the situation with other psychological disorders, which have a high relapse rate, it appears that, in most cases, treatment improvements of PTSD symptoms and diagnosis are long-lasting. Furthermore, comorbid major depression showed the same pattern of sustained recovery. Finally, in the parent study, the women were in their 30s on average. The fact that they reported an increase in education and more stable relationships may be a proxy for improved functioning.
Acknowledgments
This work was supported by National Institute of Mental Health Grant NIH-1 R01-MH51509 awarded to Patricia A. Resick while at the University of Missouri–St. Louis. This article was also supported by the National Center for PTSD, VA Boston Healthcare System. The authors wish to thank the therapists and assessors for their help on this project and Stephanie Wells for her assistance. We also wish to thank all the women who were willing to participate so long after their initial participation in the study.
Footnotes
This study was presented at the 25th annual meeting of the International Society for Traumatic Stress Studies, Atlanta, Georgia, November 2009, and at the 30th annual meeting of the Anxiety Disorders Association of America, Baltimore, Maryland, March 2010.
The number of months was calculated by dividing the number of days since baseline assessment by 30.42. We created the number of months variable in this manner to retain the precision of the number of days while making the units of the unstandardized regression coefficient (b) change in the outcome measure per month, which is easier to interpret than change per day (especially across the LTFU assessment).
The focus of the current article was investigating change over time during the LTFU period (i.e., Epoch 2). We conducted piecewise regression analyses (as opposed to only utilizing data points in Epoch 2) because the piecewise regression approach utilizes all of the information available for each participant to produce the most accurate and powerful estimates of change over time during Epoch 2. Because results occurring during Epoch 1 were published in previous articles, we report only the estimates of change over time during Epoch 2. (See the bottom right panel of Figure 6.2 of Singer & Willett, 2003, for a detailed depiction of the change parameters involved in the model.)
The group coded as 0 on the dummy-coded variable was the reference group. The coefficients for the regression intercept terms provided an estimate for the time coefficients for the reference group, while the coefficients for the dummy-coded variable provided an estimate of the difference in the time coefficients between the two treatment groups (i.e., Condition × Time interaction). To produce estimates of change coefficients for both treatment conditions, we conducted the analysis twice, switching the reference group. Switching the reference group did not impact the overall analyses (i.e., it did not impact the significance or strength of the Condition × Time coefficient). Switching the reference code just changed the interpretation of the intercept code.
Although the intention was to assess participants at least 5 years posttreatment, one participant was assessed at 4.5 years because she was moving out of state.
Because of the skewed distribution of the number of sessions variable, multiple transformations (e.g., natural-log, square root, setting the maximum value = 0) were computed. The two treatment conditions did not vary significantly on any of the transformed variables.
Contributor Information
Patricia A. Resick, National Center for PTSD/VA Boston Healthcare System, Boston, Massachusetts, and Department of Psychiatry, Boston University
Lauren F. Williams, New Mexico VA Healthcare System, Albuquerque, New Mexico
Michael K. Suvak, National Center for PTSD/VA Boston Healthcare System, Boston, Massachusetts
Candice M. Monson, Department of Psychology, Ryerson University
Jaimie L. Gradus, National Center for PTSD/VA Boston Healthcare System and Departments of Psychiatry and Epidemiology, Boston University, Boston, Massachusetts
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. Journal of Psychiatric Practice. 2004;10:307–313. doi: 10.1097/00131746-200409000-00004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Cahill SP, Rothbaum B, Resick PA, Follette VM. Cognitive-behavioral therapy for adults. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: Guilford Press; 2009. pp. 139–222. [Google Scholar]
- Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73:965–971. doi: 10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 2003. [Google Scholar]
- Crippa JAS, de Lima Osório F, Marta Del-Ben C, Santos Filho A, da Silva Freitas MC, Loureiro SR. Comparability between telephone and face-to-face structured clinical Interview for DSM–IV in assessing social anxiety disorder. Perspectives in Psychiatric Care. 2008;44:241–247. doi: 10.1111/j.1744-6163.2008.00183.x. [DOI] [PubMed] [Google Scholar]
- Echeburúa E, de Corral P, Sarasua B, Zubizarreta I. Treatment of acute posttraumatic stress disorder in rape victims: An experimental study. Journal of Anxiety Disorders. 1996;10:185–199. [Google Scholar]
- Echeburúa E, de Corral P, Zubizarreta I, Sarasua B. Psychological treatment of chronic posttraumatic stress disorder in victims of sexual aggression. Behavior Modification. 1997;21:433–456. doi: 10.1177/01454455970214003. [DOI] [PubMed] [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM–IV (SCID) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hearst DE, Dancu CV, Hembree E, Jaycox LH. Prolonged exposure (PE) manual. Medical College of Pennsylvania: Eastern Pennsylvania Psychiatric Institute; 1994. Unpublished manuscript. [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, Yadin E. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Foa EB, Rothbaum B, Riggs D, Murdock T. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Galovski TE, Monson C, Bruce SE, Resick PA. Does cognitive-behavioral therapy for PTSD improve perceived health and sleep impairment? Journal of Traumatic Stress. 2009;22:197–204. doi: 10.1002/jts.20418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell ANC, Cohen LR, Nunes EV. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology. 2009;77:607–619. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Treatment of PTSD: An assessment of the evidence. Washington, DC: National Academies Press; 2007. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Karlin BE, Ruzek JI, Chard KM, Eftekhari A, Monson CM, Hembree EA, Foa EB. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. Journal of Traumatic Stress. 2010;23:663–673. doi: 10.1002/jts.20588. [DOI] [PubMed] [Google Scholar]
- Kirk RE. Practical significance: A concept whose time has come. Educational and Psychological Measurement. 1996;56:746–759. [Google Scholar]
- Lunney CA, Schnurr PP. Domains of quality of life and symptoms in male veterans treated for posttraumatic stress disorder. Journal of Traumatic Stress. 2007;20:955–964. doi: 10.1002/jts.20269. [DOI] [PubMed] [Google Scholar]
- Macklin M, Metzger LJ, Lasko NB, Berry NJ, Orr SP, Pitman RK. Five-year follow-up study of eye movement desensitization and reprocessing therapy for combat-related posttraumatic stress disorder. Comprehensive Psychiatry. 2000;41:24–27. doi: 10.1016/s0010-440x(00)90127-5. [DOI] [PubMed] [Google Scholar]
- Monson CM, Gradus JL, Young-Xu Y, Schnurr P, Price J, Schumm J. Change in posttraumatic stress disorder symptoms: Do clinicians and patients agree? Psychological Assessment. 2008;20:131–138. doi: 10.1037/1040-3590.20.2.131. [DOI] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74:898–907. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5th ed. Los Angeles, CA: Muthén & Muthén; 1998–2009. [Google Scholar]
- Muthén LK, Muthén BO. How to use a Monte Carlo study to decide on sample size and determine power. Structural Equation Modeling. 2002;9:599–620. [Google Scholar]
- Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology. 2004;72:579–587. doi: 10.1037/0022-006X.72.4.579. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A, Congdon R. HLM-6: Hierarchical linear and nonlinear modeling [Computer software and manual] Lincolnwood, IL: Scientific Software International; 2005. [Google Scholar]
- Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum G, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76:243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive processing therapy, prolonged exposure and a waiting condition for the treatment of posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for rape victims: A treatment manual. Newbury Park, CA: Sage; 1993. [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing Axis I and II disorders. American Journal of Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea T, Chow BK, Bernardy N. Cognitive-behavioral therapy for post-traumatic stress disorder in women: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2007;297:820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, Bernardy N. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a Department of Veterans Affairs cooperative study. Archives of General Psychiatry. 2003;60:481–489. doi: 10.1001/archpsyc.60.5.481. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University; 2003. [Google Scholar]
- Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, Barrowclough C. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic post-traumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67:13–18. doi: 10.1037//0022-006x.67.1.13. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Sommerfield C. Treatment of chronic PTSD by cognitive therapy and exposure:5-year follow-up. Behavior Therapy. 2004;35:231–246. [Google Scholar]
- VA/DoD Guideline Working Group. VA/DoD clinical practice guideline for management of post-traumatic stress. 2010 Retrieved from http://www.healthquality.va.gov/ptsd/ptsd-sum_2010a.pdf.