Abstract
Chronically critically ill patients are a growing population. A pilot study determined nurses’ and family caregivers’ prior knowledge of the date of discharge for these patients. Despite complex needs, nurses and family caregivers were not aware of discharge until close to the target date.
Ms. M. is a 77-year-old female who came to the emergency department from home with complaints of increasing chest pain with activity over the past 2 weeks. She was diagnosed with an acute MI, and a cardiac catheterization revealed 90% blockages of six main coronary arteries. She underwent successful coronary artery bypass surgery but her postoperative course was complicated by hypotension, renal insufficiency, and volume overload. When Ms. M. remained on mechanical ventilation for 11 days, she joined one of the fastest growing subsets of patients — the chronically critically ill. On the 26th day of her admission, she was discharged from the acute care hospital to a rehabilitation center. Despite this protracted hospitalization and complicated course, the family caregivers and staff nurses were not aware of her impending discharge until the date of discharge. After only 7 days, the patient was readmitted to the acute care hospital for respiratory distress due to volume overload, pulmonary edema, and impending renal failure.
Background
Unfortunately, the scenario described is common among the chronically critically ill patient population. The chronically critically ill (CCI) are a recently recognized and growing population of patients who have endured prolonged periods of mechanical ventilation and subsequent lengthy hospitalizations while recovering from a variety of critical illnesses (Douglas et al., 1997; Nasraway, Button, Rand, Hudson-Jinks, & Gustafson, 2000). They typically require long stays in acute care and their hospital mortality rates average 35%–50% (Douglas & Daly, 2003; Kleinpell & Ferrans, 1998; Rudy et al., 1995; Votto, Brancifort, Scalise, Wollschlager, & ZuWallack, 1998). Their overall 1-year mortality rate has been reported as high as 55%–65% (Douglas, Daly, Gordon, & Brennan, 2002; Douglas et al., 1997; Heyland, Konopad, Noseworthy, Johnston, & Gafni, 1998; Scheinhorn, Chao, Stearn-Hassenpflug, LaBree, & Heltsley, 1997).
The American Association of Critical Care Nurses’ (AACN) Standards of Care for Acute and Critical Care Nursing include providing continuity of care for patients as one of the roles in nursing (AACN, 2000). On average, 74% of the CCI are transferred from the intensive care unit to a medical/surgical nursing unit prior to discharge (Higgins, 2001–2006).
For the CCI, extensive preparation is necessary prior to hospital discharge (Carasa & Nespoli, 2002). Historically, nurses have played a crucial role in the discharge of all patients from acute care institutions. Frequently, however, limited time and resources do not allow nurses the opportunity to complete these preparations. Although little data currently exist to substantiate this point, potentially negative consequences can result from abbreviated discharge planning. In fact, 38% of CCI patients will be readmitted within 6 months of their acute care discharge (Douglas, Daly, Brennan, Gordon, & Uthis, 2001).
Decreases in length of hospital stay are driven by both insurance/cost-management (Medical College of Wisconsin, 2003) and medical technology (Pearson, Proctor, Wilcockson, & Allgar, 2004) and they can contribute to initiation of discharge planning at short notice. Nurses must use every opportunity to prepare patients and families for discharge (London, 2004). For patients who are discharged home, staff nurses often work with an interdisciplinary team (Carasa & Nespoli, 2002) to arrange home care and necessary equipment; they also may make follow-up appointments and ensure prescriptions are written. When staff nurses are not aware of the discharge date, patients may leave the hospital without needed preparation, adequate follow-up plans, or the opportunity to ask pertinent questions. The CCI have complicated care needs at the time of discharge that warrant careful planning. Hence, it is important for nurses and family members/caregivers to be notified and prepared for discharge well in advance of the discharge date. However, nursing data have failed to address how well patients and family members believe they have been prepared for discharge (Leske & Pelczynski, 1999; Scherbring, 2002; Victor & Vetter, 1988). After extensive review of the literature (CINAHL 1982-present, Medline 1966-present, Proquest Nursing Journals 1985-present), authors were unable to locate any studies that provide data on “awareness of discharge date.”
Sample/Methods
The purpose of this pilot study of a small convenience sample (n=16) of chronically critically ill patients was to determine nurses’ and family caregivers’ prior knowledge of the date of discharge from an acute care hospital. This study was conducted as part of two larger NIH grants (NINR-05005 and NINR-05207) investigating weaning and post-discharge outcomes, respectively, of the CCI. Enrollment criteria included more than 3 days on mechanical ventilation, 18 years of age or older, and no prior chronic home ventilation. Approval for both the parent studies and pilot study were received from the hospital’s institutional review board.
Within 48 hours of the discharge, investigators contacted the primary family caregivers (family member or friend) and staff nurse assigned to the patient on the day of discharge to ask, “When were you first notified of the discharge date for your family member/friend/patient?” In addition, continuity of care was assessed with a single question asked of the nurses, “Is the discharge date the first day you cared for the patient?” Responses were coded 0 if family caregiver and nurses responded that they were notified of discharge on the date of discharge, 1 if they knew about the discharge 1 day prior to date of discharge, 2 if they knew about the discharge 2 days prior to date of discharge, and so forth.
Results
Caregiver data were available for 12 of 16 subjects. The mean age (SD) of the family caregivers was 57.9 (16.1). Seventy-five percent (n=9) of the family caregivers were women. The primary relationship of the family caregivers to patients was as follows: 42% (n=5) were non-relatives, 33% (n=4) children, 17% (n=2) spouses, and 6% (n=1) the sibling.
Table 1 lists the descriptive characteristics of the patient sample (n=16). These data provide some indication of severity and complexity of the patients’ illness episodes. The mean length of stay for the subjects was 26.3 days (range=11–52). Half of the sample (n=8) were discharged from the ICU and the other half from the medical/surgical nursing division. At discharge, 31% (n=5) of the sample were on partial or full mechanical ventilation. Sixty percent (n=9) of the patients required tracheostomy care and 75% (n=12) required oxygen. Five patients (36%) were readmitted to the acute care hospital within 2 months of discharge. Of those, two had multiple re-admissions within this period.
Table 1.
Characteristics of Patient Sample (N=16)
| Variables | Mean (SD) | Median | Range |
|---|---|---|---|
| Age | 62.3 (17.7) | 64.0 | 24–83 |
| APACHE III (Admission) | 61.7 (28.9) | 48.5 | 29–125 |
| LOMV* | 15.7(11.7) | 11.0 | 4–42 |
| LOS* | 26.3(12.7) | 23.0 | 11–52 |
| # of Pre-Existing Conditions | 5.1 (2.9) | 5.5 | 1–12 |
|
| |||
| Variables | n | % | |
|
| |||
| Gender | |||
| Female | 9 | 56 | |
| Male | 7 | 44 | |
| Race | |||
| Caucasian | 12 | 75 | |
| Minority | 4 | 25 | |
| Living at Home Prior to Hospital Admission | |||
| Yes | 15 | 94 | |
| No | 1 | 6 | |
| Type of Admission | |||
| Planned | 2 | 13 | |
| Unplanned | 14 | 88 | |
| Primary Diagnostic Classification | |||
| Cardiologic | 5 | 31 | |
| Respiratory | 5 | 31 | |
| Neurologic | 6 | 38 | |
| Disposition | |||
| Long-term care | 14 | 88 | |
| Home with home care | 2 | 13 | |
| On Mechanical Ventilation at Discharge | |||
| Yes | 5 | 31 | |
| No | 11 | 69 | |
| Readmission Within 2 Months of Hospital Discharge (n=T4) | |||
| Yes | 5 | 36 | |
| No | 9 | 64 | |
= days
LOMV = Length of Mechanical Ventilation
LOS = Length of Stay
Figure 1 summarizes data regarding knowledge of discharge date for both the family caregivers and staff nurses. On average, family caregivers knew of the discharge date 1.4days (range=0–7) and the nurses 0.6 days (range=0–4) prior to discharge. For eight (50%) of the nurses, the patient’s discharge day was the first time they cared for the patient. The nurses were then divided into two groups based on whether they provided care only on date of discharge or cared for the patient more than 1 day. A t-test indicated no statistically significant differences between these two groups related to timing of the nurse’s (p=0.18) or family caregiver’s notification of discharge (p=0.07). No statistically significant correlations existed between length of mechanical ventilation (r=0.17; p=0.53) or length of stay (r=0.16; p=0.59) and the number of days the staff nurses were aware of the discharge date prior to discharge. The data reflect the minimal notice of discharge date by both the family caregivers and the nurses. Because 50% of the nurses had not cared for the patient prior to the discharge date, the 0.6 days’ notice may stem from lack of communication among staff members or actual last-minute discharge planning.
Figure 1.
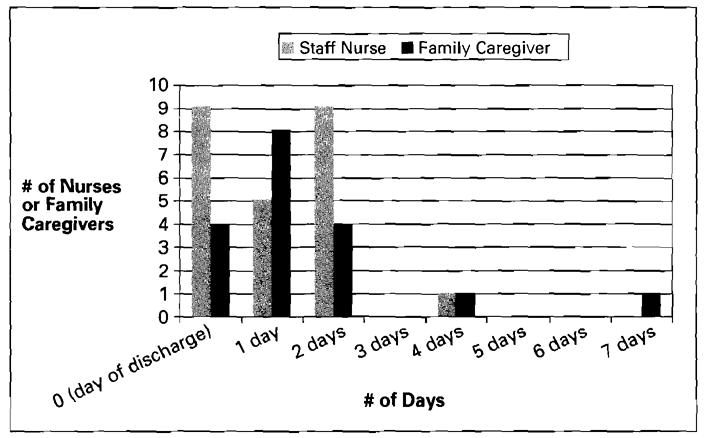
Number of Days Prior to Discharge that Staff Nurse and Family Caregiver Were Aware of Discharge Date
Could Ms. M.’s readmission to the acute care hospital have been avoided if the staff nurse and family caregivers had been aware of the discharge prior to the actual discharge date? A hurried or unplanned discharge can lead to mistakes, which may result in serious consequences, including readmission. In this case, one of the reasons for Ms. M.’s readmission was volume overload resulting in pulmonary edema. A rushed discharge also may result in miscommunication of essential patient data. For example, cognitive deficits, advance directives, identification of supportive family caregivers, and functional ability can make a difference in the discharge process.
The nurse’s role in patient discharge as well as a sample modeling dialogue are presented in Figure 2.
Figure 2.
Nurse’s Role in Patient Discharge
Conclusion
Increasing numbers of CCI individuals spend time in medical-surgical units prior to acute care discharge, and they can present special challenges to discharge planning. Through this pilot study, authors learned several things. First, the study confirmed that, in the fast-paced environment of the acute care hospital, discharge planning may often be overlooked or not well communicated. Second, given the complexity of the care needs of the CCI and the high risk of readmission, discharge planning is an important target for quality improvement in nursing care. Third, having established the feasibility of this method of data collection, authors are better prepared to conduct a larger, more formal study, A larger sample is needed to test hypotheses statistically and to test the necessary interventions to prepare staff nurses, family caregivers, and patients for a better discharge.
Acknowledgments
Funding Sources: NINR-05005, NINR-05207
Contributor Information
Amy R. Lipson, Amy R. Lipson, PhD, is a Project Manager, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH.
Carol Genet Kelley, Carol Genet Kelley, PhD, RN, is an Assistant Professor, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH..
Patricia A. Higgins, Patricia A. Higgins, PhD, RN, is an Assistant Professor, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH.
Barbara J. Daly, Barbara J. Daly, PhD, RN, FAAN, is an Associate Professor, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH.
References
- American Association of Critical Care Nurses (AACN) Standards for acute and critical care nursing practice. 2000 Retrieved December 27, 2004, from http://www.aacn.org.
- Carasa M, Nespoli G. Nursing the chronically critically ill patient. Critical Care Clinics. 2002;10(3):493–507. doi: 10.1016/s0749-0704(02)00008-8. [DOI] [PubMed] [Google Scholar]
- Douglas SL, Daly BJ. Caregivers of long-term ventilator patients: Physical and psychological outcomes. Chest. 2003;123(4):1073–1081. doi: 10.1378/chest.123.4.1073. [DOI] [PubMed] [Google Scholar]
- Douglas SL, Daly BJ, Gordon N, Brennan PF. Survival and quality of life Short-term versus long-term ventilator patients. Chest. 2002;30(12):2655–2662. doi: 10.1097/00003246-200212000-00008. [DOI] [PubMed] [Google Scholar]
- Douglas SL, Daly BJ, Brennan PF, Gordon NH, Uthis P. Hospital readmission among long-term ventilator patients. Chest. 2001;120(4):1278–1286. doi: 10.1378/chest.120.4.1278. [DOI] [PubMed] [Google Scholar]
- Douglas SL, Daly BJ, Brennan PF, Harris S, Nochomovitz M, Dyer MA. Outcomes of long-term ventilator patients: A descriptive study. American Journal of Critical Care. 1997;6(2):99–105. [PubMed] [Google Scholar]
- Heyland DK, Konopad E, Noseworthy TW, Johnston R, Gafni A. Is it ‘worthwhile’ to continue treating patients, with a prolonged stay (>14 days) in the ICU? An economic evaluation. Chest. 1998;114(1):192–198. doi: 10.1378/chest.114.1.192. [DOI] [PubMed] [Google Scholar]
- Higgins PA. Adult failure to thrive in long-term ventilator patients (R01-NR05005) Unpublished grant from National Institutes of Health; 2001–2006. [Google Scholar]
- Kleinpell RM, Ferrans CE. Factors influencing intensive care unit survival for critically ill elderly patients. Heart Lung. 1998;27(5):337–343. doi: 10.1016/s0147-9563(98)90054-1. [DOI] [PubMed] [Google Scholar]
- Leske JS, Pelczynski SA. Caregiver satisfaction with preparation for discharge in a decreased- length-of-stay cardiac surgery program. The Journal of Cardiovascular Nursing. 1999;14(1):35–43. doi: 10.1097/00005082-199910000-00005. [DOI] [PubMed] [Google Scholar]
- London F. How to prepare families for discharge in the limited time available. Pediatric Nursing. 2004;30(3):212–214. 227. [PubMed] [Google Scholar]
- Medical College of Wisconsin. Length of hospital stay continues to decline. 2003 Retrieved January 31, 2005, from http://www.healthlink.mcw.edu/article/1013703780.html.
- Nasraway SA, Button GJ, Rand WM, Hudson-Jinks T, Gustafson M. Survivors of calastrophic illness: Outcome after direct transfer from intensive care to extended care facilities. Critical Care Medicine. 2000;28(1):19–25. doi: 10.1097/00003246-200001000-00004. [DOI] [PubMed] [Google Scholar]
- Pearson P, Proctor S, Wilcockson J, Allgar V. The process of hospital discharge for medical patients: A model. Journal of Advanced Nursing. 2004;45(5):469–505. doi: 10.1111/j.1365-2648.2004.03023.x. [DOI] [PubMed] [Google Scholar]
- Rudy EB, Daly BJ, Douglas S, Montenegro HD, Song R, Dyer MA. Patient outcomes for the chronically critically ill: Special care unit versus intensive care unit. Nursing Research. 1995;44(6):324–331. [PubMed] [Google Scholar]
- Scheinhorn DJ, Chao DC, Stearn-Hassenpflug M, LaBree LD, Heltsley DJ. Post-ICU mechanical ventilation: Treatment of 1,123 patients at a regional weaning center. Chest. 1997;111(6):1654–1659. doi: 10.1378/chest.111.6.1654. [DOI] [PubMed] [Google Scholar]
- Scherbring M. Effect of caregiver perception of preparedness on burden in an oncology population. Oncology Nursing Forum. 2002;29(6):E70–76. doi: 10.1188/02.ONF.E70-E76. [DOI] [PubMed] [Google Scholar]
- Victor CR, Vetter NJ. Preparing the elderly for discharge from hospital: A neglected aspect of patient care? Age Ageing. 1988;17(3):156–163. doi: 10.1093/ageing/17.3.155. [DOI] [PubMed] [Google Scholar]
- Votto J, Brancifort JM, Scalise PJ, Wollschlager CM, ZuWallack RL. COPD and other diseases in chronically ventilated patients in a prolonged respiratory care unit: A retrospective 20-year survival study. Chest. 1998;113(1):86–90. doi: 10.1378/chest.113.1.86. [DOI] [PubMed] [Google Scholar]


