Abstract
Background
Congestive Heart Failure (CHF) is common and costly, and despite pharmacologic and technical advances, outcomes remain suboptimal.
Objective
To examine whether hospitals that have more experience caring for patients with CHF provide better, more efficient care.
Design
We used national Medicare claims data from 2006–2007 to examine the relationship between hospitals’ case volume and quality, outcomes, and costs for patients with CHF.
Setting
4,095 U.S. hospitals
Patients
Medicare fee-for-service patients with a primary discharge diagnosis of CHF
Measurements
Hospital Quality Alliance (HQA) CHF process measures, 30-day risk-adjusted mortality rates, 30-day risk-adjusted readmission rates, and costs per discharge.
Results
Hospitals in the lowest volume group had lower performance on HQA measures than medium- or high-volume hospitals (80.2% versus 87.0% versus 89.1%, p<0.001). Within the low volume group, being admitted to a hospital with a higher case volume was associated with lower mortality, lower readmission, and higher costs. For example, in the lowest volume group of hospitals, an increase of 10 cases of CHF was associated with 1% lower odds of mortality, 1% lower odds of readmissions and $22 higher costs per case. We found similar though smaller relationships between case volume and both mortality and costs in the medium and high-volume hospital cohorts.
Limitations
Our analysis was limited to Medicare patients 65 years of age or older; risk adjustment was performed using administrative data.
Conclusions
Experience with managing CHF, as measured by an institution’s volume, is associated with higher quality of care and better outcomes for patients, but at a higher cost. Understanding which practices employed by high-volume institutions account for these advantages can help improve quality of care and clinical outcomes for all CHF patients.
Introduction
Congestive Heart Failure (CHF) is the most common cause of hospitalization in the Medicare program, leading to nearly 1.4 million hospitalizations and $17 billion in total spending in 2007 alone.(1, 2) Despite pharmacologic and technical advances in the diagnosis and management of CHF, outcomes remain suboptimal: in the first 30 days after a hospitalization for CHF, one in ten patients has died, and of those who survive, one in four has been readmitted.(3) Given the high clinical and financial burden of this disease, especially among the elderly, there is intense interest in both improving outcomes and decreasing costs of care.
Consequently, it is important to understand why some hospitals perform better than others on both processes and outcomes of care for CHF, and why some hospitals are able to do so at lower cost. One possibility is that experience, as measured by volume, drives performance. A large body of literature suggests that for surgeries such as coronary artery bypass grafting, esophagectomy, and pancreatectomy,(4–7) as well as for cardiovascular procedures such as percutaneous coronary intervention,(8–10) hospitals performing a higher volume of procedures have better outcomes, often with a lower complication rate and, consequently, lower costs. However, studies that have examined the volume-outcome relationship for medical conditions, such as CHF, acute myocardial infarction, chronic obstructive pulmonary disease, and pneumonia, are decidedly mixed in their results,(11–14) and none to our knowledge have examined the impact of volume on costs for medical illness – a particularly important consideration in an increasingly cost-conscious health care environment.
Therefore, we sought to examine the relationship between a hospital’s volume of CHF and its performance on CHF processes of care, outcomes of care (mortality and readmission), and costs of care. We hypothesized that hospitals with a high volume of CHF patients would have higher adherence to quality process measures, lower mortality rates, lower readmission rates, and lower costs of care than hospitals with a low volume of CHF patients. Further, we postulated that the effect of volume would be independent of other factors such as the size of the hospital or whether it is a teaching institution.
Methods
Data
We used the Medicare Provider Analysis Review (MedPAR) 100% files from 2006 and 2007, which include all hospitalizations for Medicare Fee-for-Service enrollees, and examined hospitalizations for patients age 65 or older with the primary discharge diagnosis of CHF (International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9) codes 398.91, 404.x1, 404.x3, 428.0 to 428.9) between January 1, 2006 and November 30, 2007. Discharges occurring in December 2007 were excluded because we lacked 30 days of follow-up to determine clinical status. We followed the CMS methodology for classifying “index admissions;”(15) as a result, patients could be included in the sample more than once. Thus, while our analysis is carried out at the discharge level, we refer to individual discharges as patients for ease of presentation. We excluded federal hospitals and those located outside the 50 states and the District of Columbia, and based on recommendations from The Joint Commission on appropriate sample size for performance analysis,(16) we further excluded 441 hospitals with fewer than 25 Medicare CHF discharges over the 23-month period. Our final sample consisted of 4,095 hospitals and 1,029,497 discharges (>99.5% of eligible CHF discharges).
We obtained hospital characteristics from the 2007 American Hospital Association annual survey, including hospitals’ size, nurse-to-census ratio, ownership, proportion of patients who had Medicare or Medicaid insurance, membership in a hospital system, membership in the Council of Teaching Hospitals (COTH), presence of a cardiac intensive care unit, location, and census region. Nurse-to-census ratio was calculated by dividing the number of full-time equivalent nurses on staff by 1000 patient-days.
Outcomes
We used the September 2008 release of the Hospital Quality Alliance (HQA) data, which provides performance data from calendar year 2007 on clinical quality process measures. We calculated an overall CHF summary performance score for each hospital, based on their score on each of the four HQA CHF quality measures: percent of CHF patients given discharge instructions, an evaluation of left ventricular systolic function, an angiotensin coverting enzyme (ACE) inhibitor or angiotensin receptor blocker for left ventricular systolic dysfunction, and smoking cessation advice and counseling.
There were four primary outcomes for this analysis: processes of care (HQA score), outcomes of care (30-day all-cause mortality and readmission rates), and costs of care. Because we lacked patient-level HQA data, we examined the relationship between case volume and HQA performance at the hospital level; for the remaining three outcomes, the unit of analysis was the individual discharge. Each patient’s likelihood of mortality and readmission was adjusted for patient characteristics using the Elixhauser comorbidity adjustment scheme, which has been derived and validated on administrative data.(17–19) Each patient’s costs were adjusted using an approach we and others have previously described, regressing costs on patient-level factors (age, gender, race, comorbidities), hospital-level factors that might be expected to cause cost differences but are not within the hospital’s control (Medicare Wage Index, income and poverty rate in the community), and the pursuit of costly missions including teaching (as measured by the Intern and Resident to Bed ratio) and caring for the poor (as measured by the Disproportionate Share Hospital Index).(20, 21)
Analysis
We examined associations between our primary predictor, hospital volume of CHF patients, as a continuous variable, and each of the four outcomes, first with all outcomes aggregated at the hospital level. We thought the relationships between volume and outcomes might be nonlinear and therefore, created risk-adjusted nonparametric curves using the Loess locally weighted scatterplot smoothing method to examine these relationships. Based on these curves, we divided the patients in our sample into three groups: those discharged from the lowest-volume hospitals (25–200 discharges in our 23-month study period), those discharged from medium-volume hospitals (201–400 discharges), and those discharged from the highest-volume hospitals (greater than 400 discharges). Although the natural cut-points varied across outcomes, for ease of presentation, we used a single set of cut-points; however, we ran models using alternative cut-points as well; we describe these results qualitatively, and full results are available in the appendix (appendix Table 2).
We created unadjusted linear regression models for our continuous outcomes (HQA score and cost), and logistic regression models for our binary outcomes (30-day mortality and 30-day readmission), at the hospital level for HQA score and at the discharge level for mortality, readmission, and cost. First, in order to quantify the impact of volume on outcomes within each group of hospitals, we performed linear spline analyses, using the number of discharges from each hospital during our study period as the primary predictor, with knots at the breakpoints used to define the groups (200 and 400 discharges). For each outcome, we subsequently further adjusted for key hospital characteristics identified above. We hypothesized that there would be significant collinearity between case volume and number of hospital beds, and indeed this was the case; we chose to exclude number of beds from our primary models, but provide results with number of beds included in the models in the appendix (appendix Table 3)..
Finally, in order to provide information about differences between the groups, as a secondary analysis, we also examined volume group as a categorical variable and used it as our primary predictor in both bivariate and multivariate analyses for each of the outcomes.
A two-sided p-value of less than 0.05 was considered to be statistically significant. All analyses were performed using SAS software (version 9.2, Cary, NC, USA). This study was granted exemption by the Harvard School of Public Health Institutional Review Board within the Office of Human Research Administration.
Role of the funding source
Dr. Joynt was supported by NIH Training Grant T32HL007604-24, Brigham and Women's Hospital, Division of Cardiovascular Medicine, and by American Heart Association Clinical Research Program Grant #10CRP3780037. The funders had no role in the study.
Results
The 1,029,497 discharges that met our criteria for inclusion were divided into three groups by the case volume of the discharging hospital. Clinical characteristics of these patients are shown in Table 1a. Structural characteristics of the hospitals from which patients in each of the groups were discharged are shown in Table 1b. Hospitals in the lowest-volume group were mostly small in size (75%); only 16% of these hospitals had cardiac intensive care capabilities, and just two percent were major teaching hospitals. Hospitals in the highest-volume group were mostly medium or large in size (64% and 34%, respectively), and the majority of these hospitals had cardiac intensive care units (69%). Nearly 20% of the hospitals in the highest-volume group were major teaching hospitals, and all were urban in location.
Table 1.
| a: Patient characteristics by hospital quartile of heart failure volume | ||||
|---|---|---|---|---|
| Patient characteristics | Low Volume (25–200 discharges) N=176,981 |
Medium Volume (201–400 discharges) N=248,251 |
High Volume (401 or more discharges) N=604,265 |
|
| Age | 81 (74, 87) | 80 (74, 86) | 80 (74, 86) | |
| Female sex | 59% | 57% | 55% | |
| Race | White | 87% | 84% | 84% |
| Black | 9% | 10% | 12% | |
| Hispanic | 2% | 2% | 2% | |
| Other | 3% | 3% | 2% | |
| Diabetes without complications | 30% | 28% | 26% | |
| Diabetes with complications | 5.4% | 6.0% | 5.8% | |
| Hypertension | 54% | 57% | 58% | |
| Renal failure | 8% | 12% | 14% | |
| Valvular heart disease | 1.8% | 2.6% | 3.4% | |
| Peripheral vascular disease | 6.5% | 7.0% | 7.4% | |
| Chronic pulmonary disease | 35% | 37% | 36% | |
| b: Hospital characteristics by category of heart failure volume | ||||
|---|---|---|---|---|
| Hospital characteristics | Low Volume (25–199 discharges) N=2133 |
Medium Volume (200–399 discharges) N=970 |
High Volume (400 or more discharges) N=992 |
|
| Number of CHF discharges in 23 months, median (25th, 75th) | 85 (51, 132) | 284 (236, 339) | 602 (493, 1160) | |
| Hospital beds, median (25th, 75th) | 54 (25, 102) | 164 (114, 237) | 330 (234, 455) | |
| Hospital size | Small (6–99 beds) | 73% | 19% | 2% |
| Medium (100–399 beds) | 25% | 74% | 64% | |
| Large (400+ beds) | 2% | 7% | 34% | |
| Average length of stay for CHF in days, median (25th, 75th) | 4.0 (3.5, 4.6) | 4.8 (4.3, 5.4) | 5.2 (4.7, 5.7) | |
| Nurse-to-census ratio, median (25th, 75th) | 7.0 (4.5, 9.9) | 6.2 (4.9, 7.8) | 6.1 (5.1, 7.4) | |
| Cardiac intensive care | 16% | 37% | 69% | |
| Ownership | For-profit | 16% | 21% | 12% |
| Non-profit | 54% | 64% | 80% | |
| Public | 31% | 15% | 8% | |
| Proportion of Medicare patients, median (25th, 75th) | 51 (43, 59) | 45 (40, 52) | 45 (40, 51) | |
| Proportion of Medicaid patients, median (25th, 75th) | 16 (9, 20) | 17 (13, 22) | 16 (11, 20) | |
| Member of hospital system | 40% | 52% | 54% | |
| Major teaching hospital | 2% | 6% | 18% | |
| Urban location | 61% | 93% | 100% | |
| Region | Northeast | 8% | 17% | 24% |
| Midwest | 34% | 23% | 26% | |
| South | 38% | 41% | 41% | |
| West | 21% | 19% | 8% | |
Groups may not sum to 100% due to rounding.
CHF = congestive heart failure. Groups may not sum to 100% due to rounding.
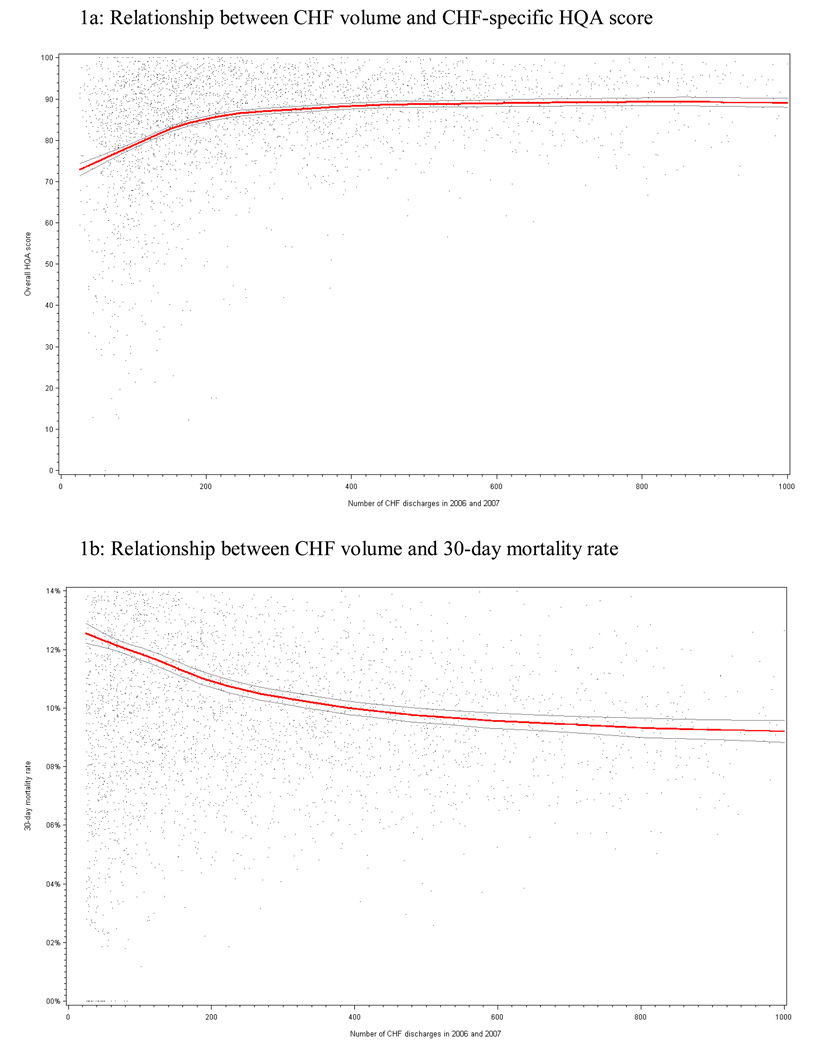
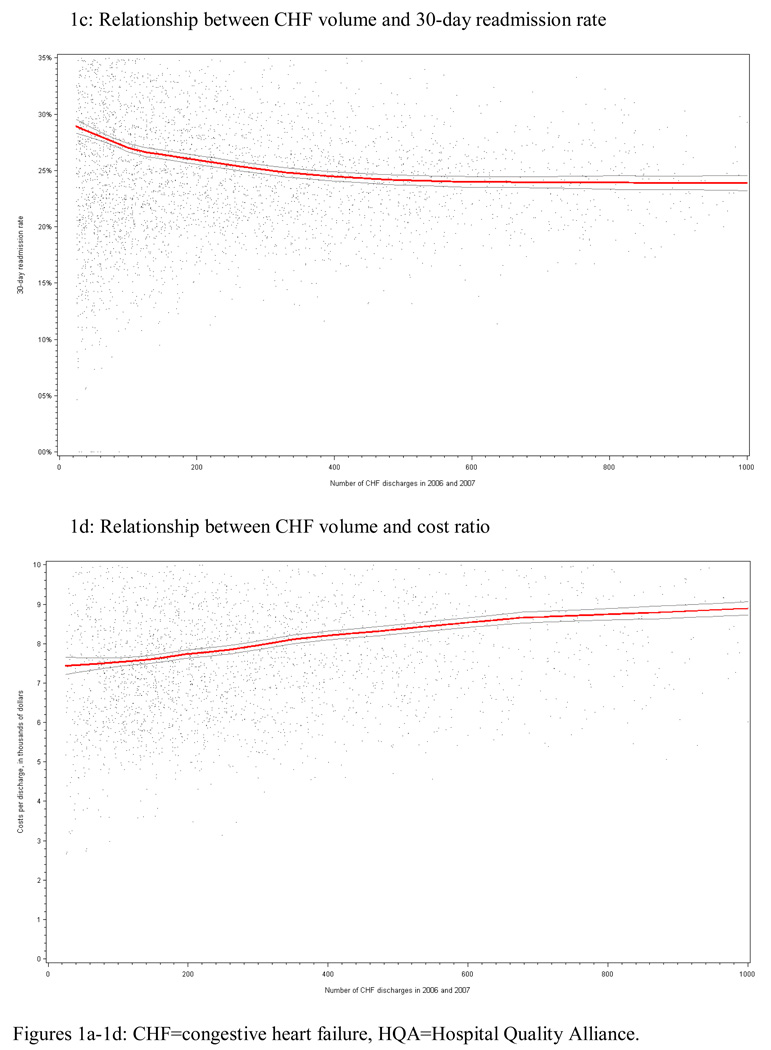
First examining outcomes aggregated at the hospital level, we found a positive relationship between volume and HQA scores, and a negative relationship between volume and both 30-day mortality and readmission rates (Figures 1a–c). For each, there was an initial linear relationship followed by a plateau of the impact of volume on outcomes; the plateau appeared between 200 and 400 discharges over the 23-month study period. Higher-volume hospitals had higher costs than lower-volume centers, and this appeared to be a relationship without an obvious plateau effect (Figure 1d).
Figure 1.
Relationship between CHF volume and processes, outcomes, and costs of care
Linear relationship between case volume and outcomes
Using spline models, and adjusting for patient characteristics, each 10-discharge increase in volume was associated with an 0.75 point increase in HQA score in the lowest-volume group of hospitals and a 0.13 point increase in the medium-volume group of hospitals; there was no significant relationship in the high-volume group, reflecting the plateau effect seen in the Loess curves (Table 2a, middle columns). Once we additionally adjusted for hospital characteristics (Tables 2a, rightmost columns), volume retained a relationship with HQA score in the lowest-volume group only.
Table 2.
The relationship between case volume and processes and outcomes of care, stratified by volume group
| a: The relationship between case volume and processes of care for heart failure, stratified by volume group | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted analysis | Adjusted for hospital characteristics | ||||||||
| Volume group |
Number of hospitals |
Change per 10 pt increase in volume |
P | Mean | P | Change per 10 pt increase in volume |
P | Mean | P |
| Overall Hospital Quality Allinace Score | |||||||||
| Low | 1,388 | 0.75 (0.64, 0.87) | <0.001 | 80.2 | <0.001 | 0.58 (0.47, 0.69) | <0.001 | 82.2 | <0.001 |
| Medium | 964 | 0.13 (0.06, 0.20) | <0.001 | 87.0 | <0.001 | 0.04 (−0.03, 0.11) | 0.29 | 86.5 | 0.55 |
| High | 991 | −0.00 (−0.02, 0.02) | 0.84 | 89.1 | Ref | −0.02 (−0.04, 0.00) | 0.09 | 86.9 | Ref |
| ACE inhibitor or ARB for patients with left ventricular systolic dysfunction | |||||||||
| Low | 378 | −0.19 (−0.33, −0.06) | 0.005 | 89.3 | 0.12 | −0.12 (−0.25, 0.02) | 0.09 | 89.5 | 0.83 |
| Medium | 866 | 0.08 (0.02, 0.14) | 0.004 | 89.0 | 0.004 | 0.04 (−0.02, 0.09) | 0.21 | 89.4 | 0.54 |
| High | 989 | −0.00 (−0.02, 0.02) | 0.98 | 90.1 | Ref | −0.02 (−0.03, 0.00) | 0.06 | 89.6 | Ref |
| Assessment of left ventricular function | |||||||||
| Low | 1,388 | 0.80 (0.69, 0.91) | <0.001 | 86.1 | <0.001 | 0.59 (0.49, 0.70) | <0.001 | 88.4 | <0.001 |
| Medium | 964 | 0.16 (0.09, 0.22) | <0.001 | 93.6 | <0.001 | 0.04 (−0.02, 0.10) | 0.20 | 92.9 | 0.11 |
| High | 991 | 0.01 (−0.00, 0.03) | 0.23 | 96.3 | Ref | −0.00 (−0.02, 0.02) | 0.91 | 93.8 | Ref |
| Discharge instructions | |||||||||
| Low | 1,161 | 0.69 (0.49, 0.89) | <0.001 | 70.9 | <0.001 | 0.55 (0.35, 0.75) | <0.001 | 72.3 | <0.001 |
| Medium | 964 | 0.12 (0.00, 0.23) | 0.04 | 76.6 | 0.13 | 0.06 (−0.05, 0.18) | 0.29 | 76.5 | 0.96 |
| High | 991 | −0.02 (−0.06, 0.01) | 0.17 | 78.0 | Ref | −0.04 (−0.08, −0.00) | 0.03 | 76.6 | Ref |
| Smoking cessation counseling | |||||||||
| Low | 168 | 0.33 (0.18, 0.48) | <0.001 | 92.3 | <0.001 | 0.28 (0.13, 0.42) | <0.001 | 93.1 | <0.001 |
| Medium | 510 | 0.10 (0.03, 0.15) | 0.003 | 95.8 | 0.004 | 0.07 (0.01, 0.14) | 0.03 | 96.1 | 0.16 |
| High | 889 | 0.01 (−0.01, 0.02) | 0.45 | 97.0 | Ref | 0.00 (−0.01, 0.01) | 0.99 | 96.7 | Ref |
| b: The relationship between case volume and outcomes and costs of care for heart failure, stratified by volume group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted analysis | Adjusted for hospital characteristics | |||||||||
| Volume group |
Number of patients |
Number of hospitals |
Change per 10 pt increase in volume* |
P | Mean | P | Change per 10 pt increase in volume* |
P | Mean | P |
| 30-day mortality | ||||||||||
| Low | 176,985 | 2,129 | −0.009 (−0.012, −0.007) | <0.001 | 10.5% | <0.001 | −0.009 (−0.01, −0.006) | <0.001 | 10.2% | <0.001 |
| Medium | 248,251 | 970 | −0.006 (−0.007, −0.004) | <0.001 | 9.3% | <0.001 | −0.005 (−0.007, −0.004) | <0.001 | 9.3% | <0.001 |
| High | 604,265 | 992 | −0.0008 (−0.001, −0.0004) | <0.001 | 8.5% | Ref | −0.0007 (−0.001, −0.0003) | 0.001 | 8.6% | Ref |
| 30-day readmission | ||||||||||
| Low | 146,671 | 2,133 | −0.009 (−0.01, −0.006) | <0.001 | 27.7% | <0.001 | −0.003 (−0.006, 0.0004) | 0.09 | 26.1% | 0.34 |
| Medium | 214,024 | 970 | −0.003 (−0.004, −0.0009) | 0.002 | 26.0% | <0.001 | −0.0001 (−0.002, 0.001) | 0.87 | 25.9% | 0.73 |
| High | 545,405 | 992 | 0.0001 (−0.0002, 0.0004) | 0.40 | 25.5% | Ref | −0.00 (−0.0004, 0.0003) | 0.76 | 25.8% | Ref |
| Costs per discharge | ||||||||||
| Low | 125,300 | 1,181 | $21.78 (1.92, 41.61) | 0.03 | $7,189 | <0.001 | $29.88 (9.81, 49.95) | 0.004 | $7,321 | <0.001 |
| Medium | 253,205 | 956 | $35.76 (24.94, 46.59) | <0.001 | $7,579 | <0.001 | $28.83 (18.07, 39.59) | <0.001 | $7,702 | <0.001 |
| High | 621,913 | 987 | $10.13 (6.67, 13.59) | <0.001 | $8,382 | Ref | $8.59 (5.13, 12.05) | <0.001 | $8,320 | Ref |
ACE=angiotensin converting enzyme; ARB=angiotensin receptor blocker. The adjusted model accounts for the presence of a cardiac intensive care unit, hospital ownership, teaching status, hospital system membership, proportion of patients with Medicare in the overall hospital population, proportion of patients with Medicaid in the overall hospital population, urban location, and region).
For 30-day mortality and readmissions, change represents the change in the log odds of mortality (or readmissions) per 10 patient increase in case volume. For costs per discharge, change represents the change in dollars per discharge, per 10 patient increase in case volume. Adjusted analyses include the presence of a cardiac intensive care unit, hospital ownership, teaching status, hospital system membership, proportion of patients with Medicare in the overall hospital population, proportion of patients with Medicaid in the overall hospital population, urban location, and region.
We found a significant negative relationship between volume and the odds of mortality for patients discharged from hospitals in each of the three groups of hospitals; the decrease in mortality per 10-discharge increase in volume was largest in the lowest-volume group, intermediate in the medium-volume group, and smallest in the highest-volume group. For readmissions, there was a significant negative relationship between volume and the odds of readmission for the lowest and the medium-volume groups of hospitals, but no relationship was seen in the highest-volume group. The impact of volume on costs per discharge was significant in all three groups of hospitals, although again, the magnitude of the effect was smallest in the highest-volume group. When we adjusted these models for additional hospital characteristics, we found that the effects of volume on mortality and costs remained largely unchanged. However, the impact of volume on readmissions diminished significantly, and the associations were no longer statistically significant. Using cut-points of 100 and 400 cases, the results were qualitatively similar, with the exception that the impact of volume on readmissions was negative and significant in the lowest-volume group, even after adjusting for hospital characteristics.
Between-group comparisons
When we examined whether the average performance varied across these three groups of hospitals, we found results that were analogous to our findings from the linear spline models. For HQA measures, hospitals in the highest-volume group had better performance than those in the medium-volume group or the lowest-volume group (89.1% versus 87.0% versus 80.2%, p<0.001 for each comparison, table 2a). When we further adjusted these results for other hospital characteristics, the lowest-volume group of hospitals continued to have worse performance.
At 30 days, patients admitted to the hospitals in the highest-volume group had, on average, lower mortality rates than those admitted to hospitals in the medium or lowest-volume groups (8.5% versus 9.3% versus 10.5%, p<0.001 for each comparison). We found similar results for readmission rates. Finally, per-discharge costs were higher in the highest-volume group of hospitals than in the medium-volume or lowest-volume groups ($8,382 versus $7,579 versus $7,189, p<0.001 for all comparisons). When we further adjusted these results for other hospital characteristics, once again our findings were comparable to the linear models: the relationships between volume group and mortality and costs remained largely unchanged, while the relationship between volume group and readmission rates was smaller and not significant.
Discussion
We examined the relationship between volume of CHF and clinical processes, outcomes, and costs. We found that patients discharged from hospitals with a higher volume of CHF patients received higher quality of care, on average, and had better outcomes, but at modestly higher cost; these relationships were independent of other key hospital characteristics including teaching status and hospital size. The strongest impact of volume on outcomes was seen in the group of hospitals with the lowest volume (those with a case volume less than 200 over our 23 month study period). The effects of volume on outcomes appeared to diminish beyond 200 to 400 discharges over the study period. Our findings suggest that the volume-outcome relationship, seen previously in procedure-based conditions, also exists for CHF and may extend more broadly to chronic medical conditions.
We have known that higher volume is associated with better outcomes for major surgeries(4–7) and cardiovascular procedures(8–10) for nearly three decades.(22) However, the relationship between volume and outcomes for medical care is less well-understood. Our findings suggest that, at least for CHF, the effects can be substantial: patients discharged from hospitals with 200 CHF discharges had, on average, 18% lower odds of death compared to those discharged from hospitals with 20 CHF discharges. Given the prevalence of this disease, these differences have important clinical and public health implications. The average hospital with 200 discharges would have an HQA score that was 13.5% higher compared to the hospital with 20 CHF discharges, with the average patient having 18% lower odds of readmission. However, the typical hospital with 200 CHF discharges would cost approximately $400 more per hospitalization. The gains in quality and outcomes appear to be worth the extra cost – but one would need formal and long-term cost-effectiveness analyses to be sure.
How might volume lead to better outcomes? One possible explanation is that greater knowledge of and adherence to process measures account for the differences. However, while high-volume hospitals did have higher HQA scores, these measures are, unto themselves, unlikely to lead to lower short-term mortality or reduced readmissions.(23) It is also possible that high-volume hospitals have both higher HQA scores and better clinical outcomes as a common result of their greater experience in caring for CHF patients. Hospitals with more CHF patients might have more incentive to retain familiarity with professional society care guidelines, or be more likely to have invested in systems to monitor for adherence to quality metrics. Standardized admission or discharge forms, increased familiarity with CHF-specific patient education, or involvement of discharge planners in CHF patients’ care, might also be more prevalent at high-volume institutions, although there are no data currently available to assess this directly. Nurses at high-volume centers might have more familiarity with CHF-specific patient care and education needs, although we do not have data to support or refute this notion. Additionally, high-volume centers might also have specialty inpatient and/or outpatient CHF services, concentrating similar patients under a team of providers; this could improve quality and coordination of care. Further work is needed to explore whether these types of services are more often present in high volume centers and whether they account for some or all of the differences we found.
Finally, it could be that better outcomes lead to higher volume, rather than the other way around. Hospitals that spend more to provide higher-quality services may attract more patients through referral and self-referral, thus increasing case volume. Luft et al examined this possibility using data from 736 hospitals across the country, and using analyses of referrals-in and transfers-out, as well as patterns of mortality for different conditions, concluded that selective referral was important in explaining the volume-outcome relationship.(24) Selective referral requires either that data on hospital quality is available and easy for patients and referring physicians to understand, or that high performing hospitals have a reputation for quality that attracts patients and referring physicians. Prior studies have found that publicly available quality data are rarely used by patients for selecting a hospital or clinician(25) and publishing provider performance has little effect on their market share.(26, 27) Therefore, if selective referral is a key part of the mechanism by which high performing hospitals have higher volume, it is likely through the reputational effects of being a high quality hospital.
Our finding that higher volume was associated with greater inpatient costs is novel, and has important implications for the health policy debate. We unfortunately could not determine how the extra money was spent, or whether extra spending during the index hospitalization led directly to the improved outcomes. Our analysis suggests that the efficiency gains often seen when institutions perform a high volume of surgical procedures may not bear out for conditions like CHF, at least in the short term, and challenge the assumption that hospitals with more experience caring for a particular condition should be able to do so at lower cost. Multiple studies from the Dartmouth Atlas have demonstrated that higher Medicare spending is not associated with better health outcomes at the hospital referral region level or at the individual hospital level.(28–31), although their models of costs examine data over a longer period of time (typically the last 6 months or 2 years of life) and are “looking backwards” after a death. Our costs are episode based and our results are not in direct contradiction to the Dartmouth work. It is possible that intensive care of CHF, while more expensive in the short run, may lead to lower longer-term costs.
We found a threshold beyond which additional volume was associated with little additional benefit. The incremental benefit of volume decreased once volume reached approximately 200 Medicare CHF discharges. The fact that roughly one-third of all U.S. hospitals, caring for nearly half of all patients, achieve this level of experience has important implications for quality improvement and regionalization of care. First, our findings suggest that we can get the largest benefit by targeting quality improvement efforts at hospitals with lower volume. Second, policy makers have advocated that for high-risk surgeries,(4) patients should be sent to the few hospitals that achieve very high volumes. In CHF, this degree of centralization may not be necessary given that a large number of hospitals meet the volume threshold. Interestingly, while improvement in quality of care and clinical outcomes leveled off, there was no obvious threshold effect for costs, suggesting that beyond a certain level of spending, additional resource utilization may not be associated with better outcomes. Whether this is due to unnecessary use of expensive tests or procedures at these very high volume hospitals is unclear, and additional studies are needed to better understand this issue.
Prior studies of the impact of volume on outcomes for medical conditions have demonstrated mixed results. For example, Thiemann et al demonstrated that elderly patients presenting with acute MI had lower rates of 30-day and one-year mortality if they presented to a high-volume hospital.(11) An in-hospital survival benefit in high-volume centers has been seen for patients with AIDS(33–35) and lupus,(36) although we know less about longer-term outcomes for these conditions. However, Lindenauer et al found no relationship between volume and outcomes for chronic obstructive pulmonary disease (COPD),(12) and demonstrated that hospitals with a high volume of pneumonia patients actually had both worse performance on process measures and worse clinical outcomes than hospitals with a lower volume of pneumonia patients.(13) A recent analysis by Ross et al found that hospitals with higher volume had lower 30-day mortality rates for acute myocardial infarction, CHF and pneumonia.(14) Our findings extend this work by both quantifying the benefits of volume on mortality, and by demonstrating that the benefits include better processes and lower readmissions.
We are unaware of prior studies that have directly examined the relationship between volume and costs for medical conditions. Hospitals with higher volumes for surgical procedures usually have lower costs, presumably by reducing costly complications and decreasing length of stay.(37, 38) However, CHF care may fit a different paradigm than a surgical procedure. As policymakers increasingly focus on value (balancing the importance of both outcomes and costs), our findings suggest that there may be no easy solution for improving CHF outcomes and that better care might require greater spending. Further, because CHF is a chronic, relapsing disease, rather than a single episode of care, up-front investment in quality may lead to downstream, rather than immediate, savings. Policy efforts aimed at building greater coordination and accountability among providers may have the potential to encourage hospitals to invest in better clinical CHF care if they create a mechanism through which they could reap the financial benefits of downstream cost savings.
Our study has several limitations. We lack data regarding the clinicians providing care for these patients, and were unable to assess the impact of clinician volume or clinician specialty on outcomes. Similarly, because we used administrative rather than clinical data, while we were able to calculate a nurse-to-patient ratio for each hospital, we did not have data regarding the intensity of nursing care delivered to each patient individually. Additionally, administrative data presents difficulties in terms of our ability to fully account for variations in severity of illness across hospitals. However, although administrative data are imperfect, they are standardized, validated, and increasingly used, even for public reporting. Furthermore, high-volume hospitals generally had sicker patients, and inadequate risk-adjustment may have led to underestimating differences in outcomes between these hospitals and their counterparts with a less complex population. We focused on Medicare patients; while these patients make up more than 80% of CHF admissions,(39) whether our findings apply to non-Medicare patients is unclear. Finally, as with any non-experimental study design, we could not assess whether the relationships we found were causal, or rather markers of other factors associated both with volume and outcomes.
Conclusions
We found that hospitals with greater experience caring for CHF patients provide better care with better outcomes to a sicker patient population but do so at a higher cost. The relationship between volume and outcomes is not fully linear, and the incremental benefits are small after a hospital has achieved a volume of around 200 Medicare patients over 23 months. While further work is needed to better delineate why these relationships exist, our findings suggest that the volume-outcome relationship extends beyond surgical procedures, and provides a new avenue to explore ways to improve the care and outcomes of complex, chronically ill patients.
Supplementary Material
Acknowledgements
The authors had access to all the study data, take responsibility for the accuracy of the analysis, and had authority over manuscript preparation and the decision to submit the manuscript for publication.
We thank Jie Zheng, PhD, from the Department of Health Policy and Management, Harvard School of Public Health, for assistance with statistical programming. Dr. Zheng received compensation as part of regular employment.
Grant support:
Dr. Joynt was supported by NIH Training Grant T32HL007604-24, Brigham and Women's Hospital, Division of Cardiovascular Medicine, and by American Heart Association Clinical Research Program Grant #10CRP3780037.
Footnotes
Disclosures:
Dr. Jha has provided consulting support to UpToDate. Dr. Orav has no conflics to declare. Dr. Joynt has no conflicts to declare.
- Protocol: Available to interested readers by contacting Dr. Joynt at kjoynt@partners.org
- Statistical Code: Available to interested readers by contacting Dr. Joynt at kjoynt@partners.org
- Data: not available
References
- 1.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117(4):e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 2.MedPAC. (Medicare Payment Advisory Commission). A data book: healthcare spending and the Medicare program. 2009 [Google Scholar]
- 3.Krumholz HM. Patterns of Hospital Performance in Acute Myocardial Infarction and Heart Failure 30-Day Mortality and Readmission. Circ Cardiovasc Qual Outcomes. 2009 doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 4.Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001;130(3):415–422. doi: 10.1067/msy.2001.117139. [DOI] [PubMed] [Google Scholar]
- 5.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 6.Hannan EL, Wu C, Ryan TJ, et al. Do hospitals and surgeons with higher coronary artery bypass graft surgery volumes still have lower risk-adjusted mortality rates? Circulation. 2003;108(7):795–801. doi: 10.1161/01.CIR.0000084551.52010.3B. [DOI] [PubMed] [Google Scholar]
- 7.Wu C, Hannan EL, Ryan TJ, et al. Is the impact of hospital and surgeon volumes on the in-hospital mortality rate for coronary artery bypass graft surgery limited to patients at high risk? Circulation. 2004;110(7):784–789. doi: 10.1161/01.CIR.0000138744.13516.B5. [DOI] [PubMed] [Google Scholar]
- 8.Jollis JG, Peterson ED, Nelson CL, et al. Relationship between physician and hospital coronary angioplasty volume and outcome in elderly patients. Circulation. 1997;95(11):2485–2491. doi: 10.1161/01.cir.95.11.2485. [DOI] [PubMed] [Google Scholar]
- 9.McGrath PD, Wennberg DE, Dickens JD, Jr, et al. Relation between operator and hospital volume and outcomes following percutaneous coronary interventions in the era of the coronary stent. JAMA. 2000;284(24):3139–3144. doi: 10.1001/jama.284.24.3139. [DOI] [PubMed] [Google Scholar]
- 10.Hannan EL, Wu C, Walford G, et al. Volume-outcome relationships for percutaneous coronary interventions in the stent era. Circulation. 2005;112(8):1171–1179. doi: 10.1161/CIRCULATIONAHA.104.528455. [DOI] [PubMed] [Google Scholar]
- 11.Thiemann DR, Coresh J, Oetgen WJ, Powe NR. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med. 1999;340(21):1640–1648. doi: 10.1056/NEJM199905273402106. [DOI] [PubMed] [Google Scholar]
- 12.Lindenauer PK, Pekow P, Gao S, Crawford AS, Gutierrez B, Benjamin EM. Quality of care for patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 2006;144(12):894–903. doi: 10.7326/0003-4819-144-12-200606200-00006. [DOI] [PubMed] [Google Scholar]
- 13.Lindenauer PK, Behal R, Murray CK, Nsa W, Houck PM, Bratzler DW. Volume, quality of care, and outcome in pneumonia. Ann Intern Med. 2006;144(4):262–269. doi: 10.7326/0003-4819-144-4-200602210-00008. [DOI] [PubMed] [Google Scholar]
- 14.Ross JS, Normand SL, Wang Y, et al. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med. 2010;362(12):1110–1118. doi: 10.1056/NEJMsa0907130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai MM, Lin Z, Schreiner GC, et al. (Yale-New Haven Health Services Corporation / Center for Outcomes Research and Evaluation (YNHHSC/CORE)) 2009 Measures Maintenance Technical Report: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk Standardized Readmission Measures. 2009
- 16.U.S. Department of Health & Human Services. Hospital Compare - a tool provided by Medicare. [Accessed February 18, 2010]; Available at http://www.hospitalcompare.hhs.gov.
- 17.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42(4):355–360. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- 19.Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv Res. 2008;8:12. doi: 10.1186/1472-6963-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jha AK, Orav EJ, Dobson A, Book RA, Epstein AM. Measuring efficiency: the association of hospital costs and quality of care. Health Aff (Millwood) 2009;28(3):897–906. doi: 10.1377/hlthaff.28.3.897. [DOI] [PubMed] [Google Scholar]
- 21.Mechanic R, Coleman K, Dobson A. Teaching hospital costs: implications for academic missions in a competitive market. Jama. 1998;280(11):1015–1019. doi: 10.1001/jama.280.11.1015. [DOI] [PubMed] [Google Scholar]
- 22.Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. N Engl J Med. 1979;301(25):1364–1369. doi: 10.1056/NEJM197912203012503. [DOI] [PubMed] [Google Scholar]
- 23.Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. Jama. 2007;297(1):61–70. doi: 10.1001/jama.297.1.61. [DOI] [PubMed] [Google Scholar]
- 24.Luft HS, Hunt SS, Maerki SC. The volume-outcome relationship: practice-makes-perfect or selective-referral patterns? Health Serv Res. 1987;22(2):157–182. [PMC free article] [PubMed] [Google Scholar]
- 25.Schneider EC, Epstein AM. Use of public performance reports: a survey of patients undergoing cardiac surgery. Jama. 1998;279(20):1638–1642. doi: 10.1001/jama.279.20.1638. [DOI] [PubMed] [Google Scholar]
- 26.Mukamel DB, Mushlin AI. Quality of care information makes a difference: an analysis of market share and price changes after publication of the New York State Cardiac Surgery Mortality Reports. Med Care. 1998;36(7):945–954. doi: 10.1097/00005650-199807000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Jha AK, Epstein AM. The predictive accuracy of the New York State coronary artery bypass surgery report-card system. Health Aff (Millwood) 2006;25(3):844–855. doi: 10.1377/hlthaff.25.3.844. [DOI] [PubMed] [Google Scholar]
- 28.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 29.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 30.Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries' quality of care. Health Aff (Millwood) 2004;(Suppl Web Exclusives):W184–W197. doi: 10.1377/hlthaff.w4.184. [DOI] [PubMed] [Google Scholar]
- 31.Yasaitis L, Fisher ES, Skinner JS, Chandra A. Hospital quality and intensity of spending: is there an association? Health Aff (Millwood) 2009;28(4):w566–w572. doi: 10.1377/hlthaff.28.4.w566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ong MK, Mangione CM, Romano PS, et al. Looking forward, looking back: assessing variations in hospital resource use and outcomes for elderly patients with heart failure. Circ Cardiovasc Qual Outcomes. 2009;2(6):548–557. doi: 10.1161/CIRCOUTCOMES.108.825612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bennett CL, Garfinkle JB, Greenfield S, et al. The relation between hospital experience and in-hospital mortality for patients with AIDS-related PCP. Jama. 1989;261(20):2975–2979. [PubMed] [Google Scholar]
- 34.Stone VE, Seage GR, 3rd, Hertz T, Epstein AM. The relation between hospital experience and mortality for patients with AIDS. Jama. 1992;268(19):2655–2661. [PubMed] [Google Scholar]
- 35.Cunningham WE, Tisnado DM, Lui HH, Nakazono TT, Carlisle DM. The effect of hospital experience on mortality among patients hospitalized with acquired immunodeficiency syndrome in California. Am J Med. 1999;107(2):137–143. doi: 10.1016/s0002-9343(99)00195-3. [DOI] [PubMed] [Google Scholar]
- 36.Ward MM. Hospital experience and mortality in patients with systemic lupus erythematosus: which patients benefit most from treatment at highly experienced hospitals? J Rheumatol. 2002;29(6):1198–1206. [PubMed] [Google Scholar]
- 37.Ho V, Aloia T. Hospital volume, surgeon volume, and patient costs for cancer surgery. Med Care. 2008;46(7):718–725. doi: 10.1097/MLR.0b013e3181653d6b. [DOI] [PubMed] [Google Scholar]
- 38.Swisher SG, Deford L, Merriman KW, et al. Effect of operative volume on morbidity, mortality, and hospital use after esophagectomy for cancer. J Thorac Cardiovasc Surg. 2000;119(6):1126–1132. doi: 10.1067/mtc.2000.105644. [DOI] [PubMed] [Google Scholar]
- 39.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the U.S., 1979 to 2004. J Am Coll Cardiol. 2008;52(6):428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.