Graphical abstract
Highlights
► The paraventricular and supraoptic nuclei of the hypothalamus are regulators of homeostasis. ► Over one hundred G protein-coupled receptors are expressed in each of these nuclei. ► The receptors have many functions including modulating neuropeptide synthesis and release. ► 20–30% of the receptors are ‘orphans’ whose endogenous ligand and function is unknown.
Keywords: G protein-coupled receptor, Paraventricular nucleus, Supraoptic nucleus, Vasopressin, Oxytocin, Corticotropin-releasing factor, Hypothalamo-neurohypophysial system (HNS), Hypothalamus–pituitary–adrenal (HPA) axis
Abstract
G protein-coupled receptors (GPCRs) are the largest family of transmembrane receptors in the mammalian genome. They are activated by a multitude of different ligands that elicit rapid intracellular responses to regulate cell function. Unsurprisingly, a large proportion of therapeutic agents target these receptors. The paraventricular nucleus (PVN) and supraoptic nucleus (SON) of the hypothalamus are important mediators in homeostatic control. Many modulators of PVN/SON activity, including neurotransmitters and hormones act via GPCRs – in fact over 100 non-chemosensory GPCRs have been detected in either the PVN or SON. This review provides a comprehensive summary of the expression of GPCRs within the PVN/SON, including data from recent transcriptomic studies that potentially expand the repertoire of GPCRs that may have functional roles in these hypothalamic nuclei. We also present some aspects of the regulation and known roles of GPCRs in PVN/SON, which are likely complemented by the activity of ‘orphan’ GPCRs.
1. Introduction
The hypothalamo-neurohypophysial system (HNS) responds to dehydration by increasing vasopressin (VP) and oxytocin (OT) gene transcription and translation, and releasing large amounts of VP and OT into the systemic circulation. Similarly, acute and chronic stress, pregnancy, and lactation are all associated with phenotypic changes in the paraventricular (PVN) and/or supraoptic (SON) nuclei of the hypothalamus that include elevations in VP, OT and/or corticotropin-releasing factor (CRF) gene expression [2,42]. Alterations in the pattern and/or level of modulating inputs (e.g., receptor-driven signals) that impinge on the PVN and SON have important functional implications in the control of the HNS and the hypothalamic–pituitary–adrenal (HPA) axis response to stress. The activity of such inputs may drive changes in the PVN/SON VP and OT signature associated with a number of neuroendocrinological disturbances [314], and contribute to the dysregulation of the HPA axis implicated in many conditions including the classical psychosomatic disorders, cardiovascular disease, diabetes and affective disorders such as depression. Receptor function in the PVN/SON may also be altered in immunologically-related disturbances such as immunosuppression and autoimmune, allergic and inflammatory states [48,262].
By virtue of their expression in the PVN and SON, many receptors are key targets for regulating hypothalamic–HNS and -HPA axis activity. There are four major classes of receptors in the central nervous system (CNS) – (1) the ionotropic receptors such as the excitatory glutamate (e.g., N-methyl-d-aspartate (NMDA)) or inhibitory GABAA receptors that create a membrane pore to allow the flow of ions, and have a very rapid response time; (2) receptor tyrosine kinases such as tyrosine kinase receptor type B (TrkB) and the epidermal growth factor receptor (EGFR), which upon stimulation activate intracellular signaling networks like the mitogen-activated protein kinase/extracellular signal-regulated kinase (MAPK/ERK) pathway; (3) nuclear receptors including glucocorticoid, sex steroid and thyroid hormone receptors that regulate transcriptional activation; and (4) G protein-coupled receptors (GPCRs), or seven transmembrane (TM) receptors, occasionally termed heptahelical or ‘serpentine’ receptors. GPCRs constitute the largest superfamily of transmembrane signaling molecules, estimated to comprise about 1900 members (not including pseudogenes) in the rat and mouse genomes, and at least 800 members in the human genome [99]. The proportion of one-to-one GPCR orthologues is approximately 60% between rats and humans, primarily due to divergence in chemosensory receptors that are activated by sensory signals of external origin such as odors, pheromones or tastes. Olfactory receptors make up about 60% of all GPCRs in the rat and mouse genome and 50% in the human genome [99]. Most other GPCRs are activated by a diverse array of endogenous, extracellular (and perhaps intracellular) signals that include photons, biogenic amines, neuropeptides, amino acids, ions, hormones, chemokines, lipid-derived mediators and proteases. Upon ligand binding, GPCRs primarily transduce these signals via the heterotrimeric G proteins into rapid intracellular responses that regulate cell function (e.g., increases in protein kinase C (PKC) and/or protein kinase A (PKA) activity, intracellular Ca2+ and cyclic AMP (cAMP)). It is estimated that 80% of all known hormones and neurotransmitters activate cellular signal transduction mechanisms via GPCRs [21], and a substantial portion (estimates vary between 30% and 60%) of current pharmaceutical agents directly or indirectly act on these receptors [130,205] – angiotensin II and aminergic (adrenoceptor, dopamine, 5-hydroxytryptamine (5-HT)) receptor subtypes feature as prominent drug targets [137]. There are still 120–130 non-chemosensory ‘orphan’ GPCRs for which the corresponding ligands have not yet been identified [99,111].
In this review we will highlight efforts to examine GPCR expression and regulation in the rat PVN and SON by receptor autoradiography (ARG), immunohistochemistry (IHC) and in situ hybridization histochemistry (ISHH) methods in conjunction with more recent transcriptomic approaches (e.g., DNA microarrays) to present an overall estimate of the GPCR repertoire expressed in the PVN and SON. We have collated data on all of the known non-chemosensory GPCRs documented in the on-line International Union of Basic and Clinical Pharmacology Committee on Receptor Nomenclature and Drug Classification database (NC-IUPHAR; http://www.iuphar-db.org/) [111] including orphan GPCRs. These data will be discussed in the context of the regulation and function (and possible redundancy) of GPCRs in the PVN and SON as revealed by current pharmacological/physiological approaches in rats, the species in which the vast majority of studies on the HNS and HPA axis have been conducted. With respect to GPCR localization in the PVN and SON we have endeavored to cite as many of the original reference sources as possible – we apologize in advance if we have inadvertently omitted some citations. The architecture of the PVN/SON, GPCR structure/function studies, and the function of many neurotransmitters/neurohormones in the PVN and/or SON have been extensively reviewed and we shall refer to these papers throughout. In this review we shall use the GPCR subfamily nomenclature (e.g., 5-HT1A; rather than rat gene name (e.g., Htr1a)) as per NC-IUPHAR recommendations [111].
2. Anatomy and function of the rat PVN and SON
The hypothalamus is essential for maintaining homeostatic equilibrium, integrating signals from other brain regions to regulate an assortment of functions including temperature regulation, appetite and fertility. Within the hypothalamus the PVN and SON are two of the most exhaustively studied nuclei and are fundamental in the control of fluid homeostasis, lactation, cardiovascular regulation, feeding behavior, nociception, behavior and the response to stress. The PVN is located either side of the third ventricle, and can be subdivided into five parvocellular (pPVN) (periventricular, anterior, medial, dorsal and lateral parts) and three magnocellular (mPVN) (anterior, medial and posterior parts) divisions [295,316]. The main neuronal populations in the mPVN and pPVN subdivisions are intermingled with interneurons and supporting cells such as glia. The SON straddles the lateral border of the optic chiasm and contains a ‘homogeneous’ population of magnocellular neurons [255]. The large magnocellular neurons in the PVN and SON secrete mainly VP and OT as part of the HNS whereas the smaller parvocellular neurons elaborate primarily CRF, VP and OT as part of the HPA axis and/or regulate autonomic activity. Elegant, detailed studies on the mapping of the spatial organization of major neuroendocrine and non-neuroendocrine neurons in the rat PVN have revealed that although neuroendocrine neuron clusters display a unique distribution pattern, there is extensive overlap between different phenotypes [295]. For instance, there is some intermixing of magnocellular and parvocellular neurons particularly at the mPVN/pPVN border [295], and isolated magnocellular cells in the pPVN have been noted [75]. Moreover, there is evidence that the HNS and HPA axis may functionally overlap but the extent of this interaction is not fully understood [75].
Magnocellular neurons of both the PVN and SON project via the internal zone of the median eminence to the posterior pituitary, and upon appropriate stimulation secrete VP and/or OT into the peripheral blood. Magnocellular VP is released mainly in response to dehydration, hypovolemia and hypotension, while magnocellular OT is primarily involved in the milk ejection reflex during lactation, and uterine contraction at the later stages of parturition [98,255,265,311]. Parvocellular neurons project from the periventricular, anterior, and medial (dorsal portion) parts of the PVN to the external zone of the median eminence, and release their peptides into the hypophysial portal system, a series of blood vessels that bathe the anterior lobe of the pituitary. In response to stressful stimuli, CRF and VP from the dorsomedial pPVN stimulate the release of adrenocorticotropin releasing hormone (ACTH) from the corticotrope cells of the anterior pituitary, which in turn induces the secretion of cortisol (corticosterone (CORT) in rodents) from the adrenal glands. CORT exerts a negative feedback action on the pituitary, PVN and other brain regions such as the hippocampus to restrict the dramatic initial release of ACTH and CORT [7]. OT can either potentiate or inhibit ACTH and/or CORT responses by binding to the pituitary VP V1B receptor or by an action on central OT receptors, respectively [273,354]. In addition, OT stimulates the release of luteinising hormone from gonadotropes, and prolactin from lactotropes in the anterior pituitary [98]. Other parvocellular neuroendocrine cells include those that express growth hormone-releasing hormone (GHRH), somatostatin, dopamine and thyrotropin-releasing hormone (TRH) [295]. Parvocellular neurons from the dorsal, lateral, and medial (ventral portion) regions of the PVN also project to other regions of the brain, in particular to the brain stem and spinal cord [316]. Here the parvocellular neurotransmitters/neuropeptides modulate somatomotor-behavioral and autonomic circuitry; for example, CRF axons terminate in regions such as the locus coeruleus, where the peptide is reported to interact with noradrenergic neurons [72,332], VP neurons project to autonomic nuclei in the brainstem and spinal cord, and are involved in cardiovascular control [20,259,300], while parvocellular OT released in the hindbrain/spinal cord influences nociception, gastric reflexes, cardiovascular responses, yawning and penile erection [98,163,204,259]. Moreover, dendritically released neuropeptides from magnocellular perikarya may act locally or diffuse away from the PVN/SON, contributing to the central OT and VP pool [204]. It has been proposed that centrally released OT and VP from dendrites and/or parvocellular projections modulates behavior e.g., maternal and affiliative behavior, sexual behavior, and social recognition [107,204,309].
The PVN and SON are subject to regulation by many brain regions including the hindbrain/brainstem, limbic regions, lamina terminalis system, and other hypothalamic nuclei, and also from chemicals/hormones such as estrogen and CORT that can pass the blood brain barrier [63,114,223,298,316]. As such the PVN/SON is modulated by a considerable array of neurotransmitters and hormones. For example, neurons of the PVN/SON are immersed in glutamatergic and GABAergic terminals that provide major stimulatory and inhibitory tone, respectively. Input from the hindbrain to the PVN and SON includes catecholamine and serotonergic afferents from the ventral medulla, and catecholamine projections from the nucleus of the solitary tract and locus coeruleus, all of which may co-express additional neurotransmitters or neuropeptides [298,316,331]. The PVN and SON also receive efferents from the subfornical organ, and those projecting to the PVN have been shown to contain angiotensin II [82], while neuropeptide Y (NPY)- and pro-opiomelanocortin (POMC)-expressing neurons projecting to the PVN from the arcuate nucleus [283] are essential for the complex control of feeding behavior [285]. Further, parvocellular and magnocellular neurons of the PVN/SON coexpress many neuroactive substances (e.g., CRF, galanin, cholecystokinin, enkephalin, and vasoactive intestinal peptide (VIP)) that may have a paracrine/autocrine action on PVN/SON neurons [39,47]. Importantly, in response to various physiological conditions the PVN and SON exhibit a considerable degree of morphological (e.g., glial cell remodeling [115]) and functional plasticity. This can manifest itself by changes in neuronal excitability [84,322] that may be accompanied by enhanced co-expression of certain neuropeptides (e.g., VP in CRF pPVN neurons after stress exposure [2,39]) and/or altered neuro-transmitter/peptide release [42,202].
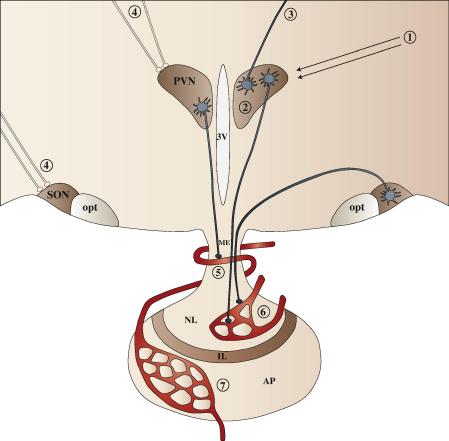
The defined cytoarchitecture of the rat PVN and SON and the features of the neurons contained within and projecting from these nuclei (e.g., large size of magnocellular cells; accessibility to experimental manipulation with reference to the SON in particular; physiologically defined outputs) make these brain regions excellent models to investigate GPCR function. As shown in Fig. 1, GPCRs can modulate PVN/SON activity at a number of levels.
Fig. 1.
Schematic diagram representing the possible roles of GPCRs in modulating PVN/SON activity. (1) Hormonal signals from peripheral blood may regulate PVN/SON activity directly (substances such as neuropeptide Y and orexin A [153,154] that can pass through the blood brain barrier activating GPCRs), or indirectly (e.g., activation of GPCRs in the circumventricular organs by humoral factors like cytokines, or neuropeptides such as angiotensin II [92] can regulate neurotransmitter/neuropeptide-expressing neurons projecting to the PVN/SON). (2) Local release of neurotransmitters from within PVN/SON (e.g., from dendrites) that act on GPCRs may have potential autocrine/paracrine effects on PVN/SON neurons e.g., priming of OT neurons by dendritically released OT in parturition/lactation [204]. In addition, neurotransmitters (e.g., melatonin, GnRH [335]) released from alternate (ventricular bordering) brain regions may reach the PVN via the ventricular system, and act to regulate neuronal activity via GPCRs. Similarly, dendritically released OT and VP from PVN neurons may permeate into the cerebrospinal fluid of the third ventricle and diffuse to, and act on, GPCRs in distant brain regions [335]. (3) GPCRs may modulate the activity of neurons that project away from the PVN/SON (e.g., parvocellular PVN projections to the hindbrain), acting directly on perikarya within the PVN/SON and/or at the nerve terminals in different brain regions. (4) GPCRs may be present on/or near the nerve terminals of interneurons (e.g., GABAergic and glutamatergic) within the PVN/SON and/or neurons originating from other regions (e.g., alternate areas of the hypothalamus, hippocampus, amygdala, brainstem), that synapse with PVN/SON soma, possibly regulating postsynaptic neurotransmitter release or acting directly to stimulate/inhibit PVN/SON neuronal activity. (5) GPCRs present in the external zone of the median eminence could modulate the secretion of CRF/OT/VP from parvocellular neurons into the portal blood stream, and GPCRs in the pituitary could have a direct effect on hormone release e.g., regulate VP/OT release from the neural lobe (6) and ACTH (amongst other neuroendocrine hormones) from the anterior lobe (7). PVN, paraventricular nucleus; SON, supraoptic nucleus; ME, median eminence; NL, neural lobe; IL, intermediate lobe; AP, anterior pituitary; opt, optic tract; 3 V, third ventricle.
3. Structure and function of GPCRs
In the CNS, GPCR ligands function mainly as slow neuromodulators rather than the fast, small molecule neurotransmitters such as glutamate and GABA acting on ionotropic receptors. Traditionally GPCRs are regarded as plasma membrane-bound receptors, although some are not highly expressed on the cell surface (e.g., human gonadotropin releasing hormone (GnRH) receptor [83] and the putative estrogen receptor GPER [266]), and increasing evidence suggests that functional GPCRs may be found in intracellular compartments such as the endoplasmic reticulum, golgi apparatus, nuclear membrane and even inside the nucleus itself [26,43,51,264,266]. The structure/function relationship of GPCRs has been covered extensively and we refer the reader to a number of excellent recent reviews (e.g., [59,128,274]). At a basic level all GPCRs have a common structure of seven membrane-spanning domains, flanked by an extracellular amino terminus and an intracellular carboxyl terminus. The transmembrane (TM) domains are formed by seven hydrophobic α-helices linked by alternating extracellular and intracellular loops. Much of what we know about GPCR ligand-binding pockets and G protein-coupling domains comes from site-directed mutagenesis and chimeric receptor studies assisted on occasions by computational modeling (e.g., [95,349,351]). In general, this large body of work has revealed that the extracellular and TM domains are responsible for ligand binding, while intracellular domains dock and activate G proteins, and anchor the receptor to the membrane. The intracellular domains are also targets for post-translational modification such as phosphorylation which play a critical role in GPCR ‘memory’ resulting in reduced (desensitization) or augmented (sensitization) responses [90]. GPCR desensitization in response to agonist stimulation is common to nearly all GPCRs, and typically involves GPCR kinase (GRK)- or other kinase-induced phosphorylation of the activated GPCR, and recruitment of β-arrestins to uncouple the receptor from its associated G protein, and targeting of the GPCR for endocytosis by linking it to ‘adaptor’ molecules such as clathrin [90,326]. The amino terminus invariably contains N-linked glycosylation sites involved in intracellular receptor trafficking, membrane expression and ligand binding [350], and the carboxyl terminus hosts sites for palmitoylation to facilitate interaction with the membrane, and together with phosphorylation sites have roles in receptor dimerization and internalization, and intracellular signaling [134]. GPCRs can be grouped into four main classes based on shared sequence motifs: (1) Class A (rhodopsin-like), the largest GPCR class that includes the earliest GPCRs cloned (β2-adrenoceptor [69], acetylcholine M1 [170]) and the aminergic, olfactory and majority of neuropeptide GPCRs; (2) Class B (secretin-like), comprising calcitonin, glucagon, CRF and parathyroid hormone receptors that have a characteristic long amino-terminus tail containing three conserved disulfide bonds; (3) Class C (metabotropic glutamate-like) with an amino terminus consisting of two lobe-like structures that resemble that of a ‘venus flytrap’ (e.g., metabotropic glutamate, calcium-sensing, and GABAB receptors); and (4) Frizzled/Smoothened receptors, which are the sole members of the fourth group. Frizzled receptors have a large amino terminus, and are important in embryonic development and adult tissue homeostasis, while Smoothened receptors contribute to the hedgehog signaling system, and are involved in embryogenesis and tumorigenesis [111,246].
For many years the prototypical reference for GPCR organization in the lipid bilayer has been based on rhodopsin and its high-resolution X-ray crystallographic structure [248]. The successful crystallography of hormone-binding GPCRs is a significant breakthrough in GPCR research that has required the recombinant generation of high levels of GPCR protein, enhancing their stability (e.g., using stabilizing ligands) and structural modifications to encourage crystal formation. The structures of a number of Class A GPCRs (e.g., β1- and β2-adrenoceptors [52,263]; adenosine A2A receptor [142] and the minimally active conformation of opsin (the ligand-free form of rhodopsin) [249]) have now been elucidated, confirming that essentially all Class A (and by extension Classes B and C) GPCRs possess seven membrane-spanning helical domains arranged in a bundle with a cytoplasmic eighth helix immediately following TM7. One insight from the small number of X-ray crystallography studies to date is that each subfamily of GPCRs possesses its own unique mode of natural ligand binding reflecting their unique structure. In the rat genome there are a total of 356 non-chemosensory GPCRs of which 132 are classified as orphans [111].
GPCRs are coupled to G proteins that are comprised of three subunits: Gα, Gβ and Gγ. Stimulation from physiological, environmental or experimental signals provokes a conformational change in the receptor-7TM structure, catalyzing the replacement of GDP for GTP on the Gα subunit. Subsequently, Gα detaches from Gβγ to create two separate components that can activate a multitude of intracellular signaling pathways e.g., Gα may increase adenylyl cyclase activity, whilst Gβγ can independently act to stimulate phospholipases and MAPK/ERKs, and activate ion channels. Heterotrimeric G proteins are encoded by a family of related genes that comprises 21 Gα, 5 Gβ and 12 Gγ mammalian genes, giving rise to a variety of G protein combinations [70]. They are categorized into four main groups according to the structure and function of the α subunit: Gαs, Gαq/11, Gαi, and Gα12/13 [246]. Gαs typically activates adenylate cyclases that catalyze the production of cAMP from ATP, stimulating PKA activity. Gαq/11 couples to and activate phospholipase Cβ (PLCβ), and increases intracellular Ca2+ and PKC activity. Gαi often inhibits adenylate cyclase activity, impeding cAMP synthesis, as well as activating G protein-coupled potassium channels. The remaining group of G proteins is the Gα12/13 family that regulate the small G protein Rho through Rho-specific guanine nucleotide exchange factors [254].
A typical feature of GPCR signaling is that by activating a cascade of signal transduction mediators the signals can be amplified. Cross-talk between GPCRs, or GPCRs and other proteins at the cell surface (e.g., via oligomerization) and in the cytoplasm (e.g., via convergent signaling pathways such as Gs/Gq/Gi− and receptor tyrosine kinase-activation of MAPK–ERKs) can modify GPCR-mediated signaling. In addition, GPCRs vary in their specificity for activating/coupling to the G protein subtypes with some activating only one Gα subtype while others are more promiscuous and couple to a number of Gα proteins to activate multiple intracellular signaling cascades. The ability of GPCRs to activate more than one class of G proteins can depend on receptor density, the nature of the ligand (different responses to two ligands can confer ‘functional selectivity’), tissue distribution, and on its localization within specialized compartments of the plasma membrane which may depend on whether the GPCR is active in a monomeric or oligomeric form [158,219,355,371]. One facet of GPCR intracellular signaling that should not be overlooked is that some GPCRs can activate both G protein-dependent and G protein-independent pathways. For example, angiotensin II AT1A receptor-triggered transactivation of the EGFR, and β-arrestin-dependent and -independent AT1A receptor internalization can take place independently of G protein activation [81]. In addition, AT1A-mediated activation of ERK features both Gq- and β-arrestin-dependent pathways [181], while β2-adrenoceptor stimulation of the MAPK–ERK pathway is Gs-coupled and Gα-independent/tyrosine kinase Src-dependent at low and high concentrations of stimulating agonist, respectively [313]. Overall it is apparent that GPCRs dynamically interact with numerous associated proteins as part of a tightly regulated signaling network, and this interaction in different tissues reflects the types of signaling components within a given cell and the receptor’s physiological role.
4. GPCR expression in the PVN and SON
Over 90% of non-chemosensory GPCRs are expressed in the mouse brain with a large proportion (82% of those examined by RT-PCR) expressed in the hypothalamus [334]. The profiles of the vast majority of GPCRs are unique, and when combined with brain region-specific intracellular signaling component expression (see Section 4.1 below), yield thousands of GPCR signaling combinations for the modulation of physiological processes. Some GPCRs even appear to be relatively confined to the CNS, although it is rare to find evidence of CNS exclusivity if techniques such as reverse-transcription (RT)-PCR or EST profiling (e.g., see http://www.ncbi.nlm.nih.gov/UniGene/) are used.
After a flourish of research in the 1980s/early 1990s localizing GPCRs by receptor autoradiography (ARG), more recent developments in immunohistochemistry (IHC), in situ hybridization histochemistry (ISHH), transcriptome approaches such as DNA microarrays and ex vivo/in vivo electrophysiological methods have greatly contributed to our understanding of the regulation of the PVN/SON activity by GPCR-based signaling. The PVN and SON are highly vascularized and blood vessel elements and ‘supporting’ cells such as glial cells express GPCRs. In the following sections we focus on the expression of GPCRs in neurons of the rat PVN and SON, although it should be emphasized that this has not been conclusively demonstrated in all studies, e.g., receptor ARG and DNA microarray experiments.
4.1. Intracellular signaling components in the PVN/SON
We would expect that cells in the PVN and SON are equipped with the appropriate sets of receptors and various intracellular signaling components to sense and respond to perturbations in homeostasis. Regulation of both GPCR signaling molecules and GPCRs themselves (see Section 5) will contribute to the adaptive responses of the PVN and SON. The distribution of various GPCR cytoplasmic signaling components in the PVN/SON has not been extensively studied, although the function of various G proteins and other intracellular signal transduction mediators involved in GPCR-mediated effects has been implicated in a number of studies. Immunoreactive (ir)-Gβ1–5 and γ3 are expressed at low levels in the rat PVN and the expression of the various β subunits is increased by repeated restraint [178,191]. While ISHH studies suggest that there are very low levels of PKC subunit mRNAs in the rat PVN and SON [32], other studies point to the expression of ir-PKC-δ in neuronal cell bodies in the PVN/SON, and ir-PKC-ϕ in PVN fibers [138], and phosphatidylcholine specific phospholipase C-mediated VP release from the hypothalamus in vitro appears to involve PKC activation [343]. Osmotic stimulation increases Gαi and Gαs mRNAs in the magnocellular PVN and SON, and cAMP in the SON [368], while Gαq appears to participate in high-salt induced VP secretion in Dahl salt-sensitive rats [336]. Of the nine adenylate cyclase isoforms only type 2 appears to be strongly expressed in the PVN and SON [227]. Elevated cAMP within PVN/SON neurons may stimulate cAMP response elements in gene promoters to alter neuropeptide (or GPCR) gene transcription, exemplified by studies showing cAMP-driven CRF and VP gene expression in the PVN [9,42,139,356]. The PVN and SON also express mRNAs for numerous members of the regulators for G protein signaling (RGS) family including RGS4, 5, 7, 8 and 9 [101] – these proteins modulate the function of the Gα and Gβ subunits, and the gene expression of at least one member (RGS4) in the PVN has been shown to be downregulated by repeated stress [237]. Other studies suggest that the spatial distribution of some signaling molecules within the PVN may be functionally relevant, e.g., RGS4 and Gαq/11 mRNAs are found in both pPVN and mPVN neurons while RGS7 gene expression is confined to the mPVN [292].
Gene expression profiling [124] considerably extends early studies [194] cataloguing some GPCR-related signaling molecules in the PVN and SON. A plethora of gene transcripts relevant to GPCR signal transduction has been revealed (see Supplementary Tables 1 and 2), including those encoding the relatively abundantly expressed Ca2+-binding calmodulins, endocytosis adaptor molecules dynamin and clathrin, various RGS and G proteins, and a number of PKC, phospholipase C and D, and cAMP isoforms. While the presence and anatomical distribution of the majority of these transcripts has not been validated by other criteria (e.g., IHC, ISHH, RT-PCR), the data indicates that the PVN and SON express a considerable network of intracellular signaling proteins that could potentially be enlisted upon GPCR activation.
4.2. Detection of GPCR proteins by receptor autoradiography (ARG)
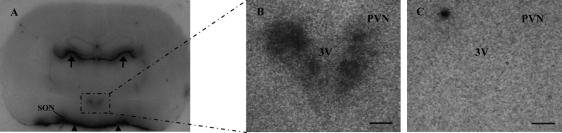
The advent of molecular biological techniques that resolved the genetic fingerprint of GPCRs led to the popular use of GPCR antibodies – generated from predicted protein sequences of cloned GPCR DNA sequences – to visualize GPCR protein expression by techniques such as IHC. Prior to this receptor ARG was a popular tool to delineate GPCR binding sites in brain and peripheral tissues since it provided the ability to anatomically resolve receptor protein expression and to quantitate receptor levels. The method can give higher (cellular) resolution if tissue sections are apposed against emulsion-coated coverslips [365] rather than against X-ray film. A major consideration when using receptor ARG is that not all pharmacologically defined binding sites necessarily represent physiologically active receptors – in a famous ‘caveat’ to those undertaking receptor studies, Cuatrecasas and Hollenberg [62] described how iodinated insulin appears to bind with high affinity to non-biological surfaces like talc with characteristics – except ‘biological activity’ – that are commonly attributed to specific hormone–receptor interactions. Moreover, while radiolabeled ligands may bind ‘functional’ (capable of binding an agonist) GPCRs they may not bind to the entire receptor pool e.g., they may only bind to high affinity binding sites, receptor–G protein interactions critical for agonist binding may be disrupted during the receptor ARG procedure, and ‘immature’ GPCRs that have not been post-translationally modified and/or possess the requisite tertiary structure, or degraded GPCRs may not bind the ligand. Other limitations of the technique include the masking of binding sites by endogenous ligand, although this is usually minimized by buffer pre-washes prior to ligand incubation. Receptor binding studies on tissue homogenates (infrequently if ever used for GPCR expression in the PVN/SON) or receptor ARG are critically dependent on the specificity and selectivity of the radiolabeled ligand employed – high affinity radioligands selective for a particular GPCR subclass are not always available. Specific binding is defined as for receptor binding assays on tissue homogenates, and includes diminution of bound radioactivity by the addition of excess cold ligand and establishing a pharmacological profile using closely- and distantly-related compounds. Knockout mice (providing the distribution of GPCRs in rat and mouse are the same) are an invaluable addition in validating radioligands for a specific receptor. Detection of low amounts of protein also depends on the sensitivity and specific activity of the radioligand, e.g., iodinated versus tritiated ligands can be used for shorter exposure times against film but offer lower resolution. An example of receptor ARG for the apelin APJ receptor is shown in Fig. 2. In this particular case there is almost a perfect overlap between APJ binding sites and APJ mRNA as shown by ISHH [243] – such a strong correlation between receptor protein and mRNA is not always the case since GPCR mRNA is present primarily in cell bodies whereas the corresponding protein may be present at distant sites, e.g., on projecting axon terminals. IHC and ultrastructural studies are mandatory to address the potential mismatch between GPCR protein and GPCR mRNA in the brain.
Fig. 2.
Receptor autoradiographical localization of the apelin APJ receptor with the APJ agonist 125I-(Pyr1)apelin-13 in 20 μm sections of adult male Sprague–Dawley rat brain. APJ ARG was performed with modifications of a previously described procedure [156]. Sections were incubated with 0.5 nM 125I-(Pyr1)apelin-13 (Perkin Elmer, Cambridgeshire, UK) alone (A,B) or in the presence (C) of 1 μM cold ligand ((Pyr1)-apelin-13; Bachem, Germany), and exposed to emulsion-coated X-ray film (Amersham Hyperfilm 3H) for 25 days which was then developed manually as per the manufacturer’s instructions. APJ binding sites in brain structures coincides with the mRNA distribution (see Fig. 4H in [243]) – binding in the SON is obscured by the intense labeling of the basal (free) surface of the hypothalamic diencephalon (arrowheads). Arrows point to APJ binding in the dorsal surface of the thalamus. B and C are a magnification of the PVN – labeling (B) present in both the magnocellular and medial parvocellular PVN is displaced by excess cold ligand (C). Scale bars, 200 μm.
The list of the 25 GPCR subfamilies detected in the PVN/SON by receptor ARG is shown in Supplementary Table 3. The number is likely incomplete since not all the literature covering GPCR receptor ARG in the brain encompasses the pertinent hypothalamic levels, and even when the relevant brain levels have been included in some studies it is often difficult to ascertain if binding is above background levels. Critically receptor ARG (and other receptor protein or RNA detection techniques) does not directly inform about GPCR function. This can be addressed in part by ‘functional’ ARG with [35S]GTPγS to map region-specific, GPCR ligand-dependent activation of G proteins [112,303]. Although it has not used extensively in the PVN and SON, [35S]GTPγS binding ARG has demonstrated ‘active’ neuropeptide Y1 and Y2 [286], and cannabinoid CB1 [121] binding sites in the PVN. Positron emission topography (PET) is an alternative imaging technique to visualize GPCRs non-invasively in the PVN and SON in vivo; while the technique is relatively low resolution and there is a dearth of suitable GPCR ligands for such studies, there are a few publications (e.g., 5-HT1A receptors in the rat PVN [12]) indicating that this approach may be a useful adjunct to receptor ARG studies in the future.
Receptor ARG rarely has the sensitivity or resolution of IHC. Moreover, in the absence of selective ligands to define a GPCR family in the PVN/SON, IHC and/or ISHH with subtype-selective antibodies and DNA/RNA probes, respectively, can elaborate a specific GPCR receptor subtype.
4.3. Immunohistochemistry (IHC) to visualize GPCR expression
Since GPCR-specific and -selective ligands are not available for all GPCRs, antibodies have been a popular option to detect many GPCRs. IHC employing primary GPCR antibodies traced with secondary antibodies to permit fluorescent or chromogenic detection of ir-proteins is a valuable technique to localize GPCR expression in sections of the PVN and SON, offering a far greater lateral and axial resolution than receptor ARG. A major consideration in all GPCR protein and mRNA detection techniques is specificity. The GPCR field is awash with reports of GPCR antibodies that don’t ‘work’ between laboratories, those that have stopped working after new batches were purchased, and those that give no staining. For antibodies in particular and the IHC method in general, the evaluation of specificity has provoked numerous comments in the past with many concluding that antibody specificity is a difficult criterion to fulfil [315]. There are well-established controls for IHC procedures, including the absence of staining when the antibody is pre-absorbed with the immunizing antigen, although this only proves that the antibody bound the added antigen and not that the antibody is ‘specific’ for the GPCR, and the presence by Western blotting of the appropriate GPCR molecular sizes which may correspond to post-translationally modified and/or oligomeric forms. However, other points related to antibody use and storage (e.g., possibility of ‘carrier’ antibodies contributing to staining patterns; tendency of antibodies to form aggregates at 4 °C; potential instability of immunoglobulin fractions or affinity-purified antisera; prolonged storage times between fixation, sectioning and staining; inefficient blocking of immunoglobulin Fc receptors (which are present in the PVN/SON [124]) – e.g., see [348] tend to be under-appreciated and often overlooked, and can lead to increased non-specific, or variable or complete absence of specific staining. Alterations in IHC staining patterns between different antibody batches (either from different animals or different bleeds from the same animal) can often be explained by the inherent characteristics of the normal immune response, e.g., decreasing antibodies titers, or high-affinity antibodies present in an early bleed may be replaced by high-avidity antibodies (perhaps with a lower relative concentrations of specific versus ‘less-specific’ immunoglobulins) as the immune response proceeds. The majority of GPCR antibodies for IHC are raised to short, synthetic GPCR peptides (‘haptens’) usually coupled to a carrier (e.g., keyhole limpet hemocyanin or sometimes bovine serum albumin) to enhance the anti-hapten antibody response, or less frequently to partially purified native or recombinant GPCRs. Invariably the antibodies are a polyclonal mixture (monoclonal antibodies have only been used occasionally (e.g., see [275,288,370]) and directed to regions that are most divergent between different GPCR subclasses, N- or C-terminus moieties being the most attractive targets. Most GPCRs are post-translationally modified [53,326,350], a crucial point in GPCR antibody production since regions that can be potentially glycosylated, phosphorylated or acylated in vivo may mask an epitope to hinder antibody recognition. On the flip side, phosphospecific GPCR antibodies can be made (e.g., [330]). Antibodies can also conceivably differentially react to ligand-activated versus unoccupied GPCR conformations, and antibodies raised against denatured GPCR proteins may not recognize the ‘native ‘ (usually fixed) GPCR in tissue sections.
For GPCRs, serious specificity concerns have been raised in a number of articles contesting the reliability of many GPCR antibodies for IHC (e.g., [224]). In contrast the specificity of antibodies to neuropeptides and other cellular constituents are rarely indicted to the same degree, commensurate with the diverse, largely structurally non-conserved nature of GPCR ligands compared with the often, high amino acid homology between different GPCR subtypes. A recent review of studies using antibodies against 19 α1- and β1-adrenoceptor, acetylcholine, dopamine and galanin receptor subtypes for immunoblotting and IHC concluded that apparent lack of specificity of GPCR antibodies appears to be the rule rather than the exception [224]. Some sensible suggestions for improving GPCR antibody validation have been made [149,224]. These include the reduction of immunostaining following GPCR knockdown using RNA interference (although a lack of knowledge of GPCR mRNA and protein turnover may make this problematic – see Section 5 below) and obtaining similar staining patterns with antibodies against different GPCR epitopes, although it is rare to find studies using two or more antibodies to detect GPCRs by IHC in the PVN and SON (exceptions include the dopamine D4 [67] and glutamate mGlu1 [161] GPCRs). Similarly, the absence of GPCR immunostaining in GPCR knockouts has also been advocated as a desired IHC control [224]. Assuming that an antibody is truly GPCR-specific in both rats and mice, and there are no species differences in the GPCR distribution between these animals, the absence of immunostaining in tissues from a knockout animal in which the entire GPCR protein coding sequence has been eliminated should serve as an excellent ‘negative’ control in IHC on rat tissues. However, if the knockout targeting construct does not include the relevant protein region to which the antibody was raised, it is possible that the antibody could react to a protein translated in-frame from the targeting construct in vivo, and lack of staining is not a foregone conclusion. While we do not necessarily share the outlook that the specificity of most GPCRs is suspect, a review of the literature emphasizes that caution is warranted, especially when using some commercially prepared antibodies [105,256]. We have not endeavored to evaluate the specificity of antibodies used to detect GPCRs in the PVN and SON. However the expression of many GPCRs detected by IHC (see Supplementary Table 4) has been validated by other methods (which also have their own specificity issues).
Individual GPCR numbers per cell are usually quite low in the brain, with lower estimates ranging from 100 to 300 receptors per cell (very low copy number) to upwards of 2000–6000 receptors per cell (around physiological levels for many GPCRs – e.g., see [152] and references therein)). By way of comparison, cells engineered to express recombinant GPCRs can achieve levels of greater than 100,000 receptors in each cell. The threshold of detection for a ‘good’ antibody in IHC is probably in the order of 10–1000 receptors per cell depending on the staining and microscopical method used (e.g., see [54,73]). The detection of ir-GPCRs in cell bodies, axons, dendrites and terminals, and in intracellular organelles such as endosomes, endoplasmic reticulum and the nucleus by IHC with conventional light microscopy can be facilitated by the use of high-resolution optical imaging techniques like confocal microscopy. GPCRs are highly mobile and traffic between different subcellular compartments in the PVN and SON, and are probably dendritically sorted as in other brain regions [269]. For example, IHC has revealed that the tachykinin NK3 receptor translocates to the nucleus of VP and non-VP PVN neurons in a stimulus-dependent manner, where it may play a role in transcriptional regulation [110,131].
CNS GPCRs are not particularly abundant proteins and their signals (and non-specific staining) can be enhanced by using modified IHC protocols incorporating tyramide signal amplification (TSA) [25]. Even with improvements in IHC detection, however, it is often difficult to discern whether GPCR staining is associated with the cell surface in detergent (e.g., Triton X-100)-treated sections of fixed tissue, although there are some examples of uniform or punctate staining closely apposed to the plasma membrane (e.g., tachykinin NK3 [131]; PTH2 parathyroid hormone [341] receptors). In most cases in the PVN and SON ir-GPCR staining is quite nondescript and apparently found mainly intracellularly, which has important functional implications for some GPCRs that are thought to be active inside the cell (e.g., the putative estrogen receptor GPER [266]). For the majority of GPCRs, an intracellular versus plasma membrane distinction may ‘simply’ reflect the detection of mature GPCRs in the endocytic pathway and/or immature GPCR pools (presumably functionally inactive) yet to be presented to the plasma membrane. In a few instances light microscopic studies have been reinforced by higher magnification immuno-electron microcopy, e.g., in the PVN and SON ir-GABAB1 is mainly associated with the endoplasmic reticulum, golgi apparatus and large membrane-bound vesicles, while a small amount of staining is found close to the plasma membrane [268]. The possible functional relevance of ir-GPCR localization in PVN and SON neurons is supported by other studies, e.g., staining for the CB1 cannabinoid receptor, a GPCR that inhibits the release of excitatory and inhibitory neurotransmitters in the brain [253], is clearly present in GABAergic terminals and fibers surrounding oxytocinergic PVN neurons [45]. The CB1 receptor appears to be synthesized in the PVN and SON [217] but other GPCRs such as the prostanoid EP3 receptor [234] appear to be confined to fiber terminals presumably as part of afferent projections to the PVN/SON. So IHC can give some idea of the pre/post-synaptical localization of GPCRs in the PVN and SON.
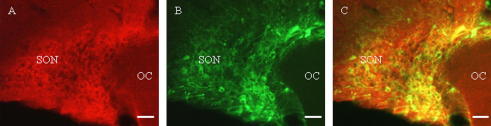
Strong indirect evidence that GPCRs in the PVN and SON may be functionally important also comes from studies where ir-GPCRs have been localized to phenotypically-identified neurons. For example, α1D-adrenoceptor [280] and angiotensin AT1A [245] receptors are both located in pPVN CRF-expressing neurons, the 5-HT1A/2A [370], apelin APJ [327], chemokine CXCR4 [44], estrogen GPER [31,116] – see Fig. 3.), GABAB1/B2 [268], κ opioid [299] and tachykinin NK3 [110] receptors are expressed in VP and/or OT neurons, whereas the glutamate mGlu1 receptor has been identified in both CRF and VP neurons [165]. VP, OT and CRF (and TRH, dopamine, GHRH and somatostatin) neurons in the PVN and SON also express additional neuropeptides that could be co-regulated [39]. The presence of VP V1A receptors on VP neurons [133] and OT receptors on OT neurons [215] suggests that these receptors may act in an autocrine fashion to regulate the release of their own cognate ligands. Moreover, the demonstration that some GPCRs (e.g., apelin APJ [327], estrogen GPER [116], and parathyroid hormone PTH2 [341] receptors) are present on both PVN and SON neuronal cell bodies, fibers and terminals (e.g., in the median eminence or in the posterior pituitary) suggests that GPCRs may act at different locations to alter neuropeptide or neurotransmitter synthesis and/or release (see Fig. 1). Based on its intracellular, and to a minor degree cell surface localization, the estrogen GPER receptor is an example of a GPCR that may be functionally active on or in neuronal cell bodies in the PVN and SON, dendrites, and axonal projections through the internal zone of the median eminence and posterior pituitary nerve terminals [116]. Given the breadth of ir-GPCR distributions in the PVN and SON, and the estimated number of neurons in the PVN and SON (e.g., there are about 1000 and 3000 VP neurons in the rat PVN and SON, respectively, and approximately 1250 OT neurons in both nuclei – [267], it is extremely likely that many GPCRs are co-expressed in individual neurons. In fact, the possible co-existence of two (or more) different GPCRs in the same neuron would support the concept that GPCRs may physically interact (see Section 6 below) in the PVN and SON. However, demonstrating co-expression of two or more proteins in a cell is difficult, although not impossible (see [33,235]) using antibodies raised in the same species to detect non-abundant proteins. In the SON and elsewhere in the brain GPCR co-expression appears to be the case for the two subunits (each a 7TM ‘receptor’) of the GABAB receptor, GABAB1 and GABAB2 [268], which must heterodimerize for functional GABAB responses [216].
Fig. 3.
Double label immunofluorescence for GPER and VP in the adult. male Sprague–Dawley rat SON. Images for GPER (A; red) and VP (B; green) immunoreactivity were merged (C; overlap yellow). 50–70% and 40–60% of VP and OT magnocellular neurons, respectively, express ir-GPER [116]. Antibodies and method are described previously [116]. OC, optic chiasm; SON, supraoptic nucleus. Scale bars, 50 μm.
There are a number of mismatches between GPCR protein and mRNA as determined by receptor ARG and/or IHC and ISHH, respectively. For example, binding studies with an iodinated glucagon GLP-1 receptor agonist detect dense labeling in the median eminence and posterior pituitary where there is no GLP-1 receptor mRNA [100,293]. Conversely, GLP-1 receptor mRNA is concentrated in the PVN where only weak binding is observed and where ir-GLP-1 fiber terminals are closely associated with OT- and CRF-expressing neurons [324]. The apparent discrepancies between GPCR protein and mRNA localizations highlight technical issues (e.g., sensitivity) and where GPCR transcription in cell bodies, translation in cell bodies and perhaps axons and dendrites, and transport along axonal and dendritic fibers may occur in the PVN and SON.
4.4. In situ hybridization histochemistry (ISHH) localization of GPCR mRNA
ISHH was introduced in 1969 [40,91,147] as a method to detect specific mRNAs within cells by hybridizing labeled RNA, cDNA, or short oligonucleotide DNA probes to target sequences in tissue samples. Employing IHC in concert with ISHH can provide converging anatomical evidence to form testable hypotheses and support data on GPCR function in the PVN and SON. High throughput ISHH as advocated for mapping high-resolution gene expression in the brain ([182] – see Allen Brain Atlas @ http://brain-map.org) is usually satisfactory for abundant genes. Apart from a few notable exceptions such as the cannabinoid CB1 receptor gene that is highly expressed in many brain regions [217], most GPCR mRNA(s) are not as abundant as those encoding ionotropic receptors and are visualized usually after weeks–months exposure against X-ray film or photographic emulsion. However, refinements in the ISHH method permit the detection of as few as 10–20 mRNA copies per cell [294], sensitive enough to visualize the majority of the rarest GPCR transcripts, and to compare changes in GPCR gene expression at the cellular level by counting silver grains or at the macroscopic level by image analysis and densitometry with reference to the appropriate autoradiographic standards (as for receptor ARG). ISHH detection sensitivity can also be enhanced by using multiple oligonucleotide probes to different regions of the designated mRNA, or by a number of amplification methods such as TSA (see Section 4.3 above).
Cloning of the mammalian GPCR cDNAs, or identification of GPCR DNA sequences using homology-based searching tools, has provided the platform to map GPCR transcript expression in the brain by ISHH. More often than not 35S-labeled antisense RNA probes targeting a large part of the GPCR mRNA (e.g., approx. 300–600 bp RNA probes (riboprobes) for proteins whose coding regions average about 1000–1500 bp in length) are used for optimal GPCR transcript detection: these can be labeled to a higher specific activity, and bind more strongly to target mRNA sequences, than oligonucleotide probes. The use of long riboprobes and even short oligonucelotides (typically 40–48 bp) introduces its own set of problems since hybridization to closely related GPCR subtypes may occur if probes are designed to a relatively well-conserved part of the GPCR mRNA sequence. GPCR-subtype specificity is usually increased if regions such as the 3′-untranslated (UTR) of GPCRs are targeted (providing the G/C content of the probe is not so low to preclude high stringency washes). However, specificity concerns may also be compounded if sense probes used as negative controls for antisense probe binding label the tissue of interest (one definition of ‘non-specific’ hybridization), which is not implausible since over 50% of the mammalian genome can produce transcripts from both DNA strands [155]. Evidence that the complementary DNA strand of a GPCR gene can code for another gene is provided by the study of Foletta and coworkers [85], where a sense VP V2 receptor probe which does not hybridize to the V2 receptor-expressing kidney [247], detected transcripts for a Rho GTPase activating protein in the brain. It is generally advised to use well-characterized probes (e.g., ones that has been validated by Northern blots, and gives appropriate hybridization patterns in control tissues), or more than one probe (and corresponding sense ‘control’) against a target sequence to minimize erroneous interpretations of ISHH labeling patterns. Our experience and that of many other laboratories using ISHH is that, as in the case of antibodies and IHC, there is often significant variability in the signal/noise ratios for different probes directed to the same GPCR mRNA target.
As outlined in Supplementary Table 4, a large number of GPCR mRNAs have been detected in the cell bodies of PVN and SON neurons. By and large there is general agreement on steady-state GPCR gene expression in the PVN and SON between laboratories but some exceptions are apparent in the literature. For example, while Hurbin and coworkers [132,133] detected VP V1B receptor mRNA and protein expression in the mPVN and SON using short oligonucleotide probes and receptor antibodies, respectively, others found only occasional V1B receptor mRNA-expressing cells in the pPVN using riboprobes directed against the 3′UTR of the receptor [366]. Studies such as these emphasize the importance of probe specificity and the limits of ISHH, and raise questions of mRNA and protein turnover (see Section 6).
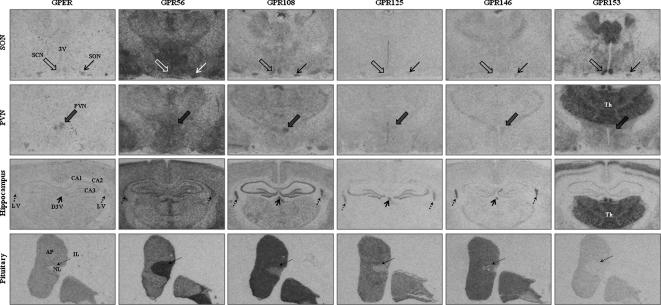
Like IHC, ISHH is also amenable to co-expression studies, whether combined with IHC or alternatively used alone to investigate the expression of two distinct transcripts in neuronal cell bodies. For example, 5-HT2C [118], adrenoceptor α1B [65], CRF1 [136] and melanocortin MC4 [201] receptor mRNAs are predominantly found in CRF neurons, neuromedin U NMU2 receptor mRNA is mainly present in OT neurons [260], and neuropeptide Y Y1 receptor transcripts are co-expressed with TRH mRNA in pPVN cells [160]. Of the 52 GPCRs with known ligands detected in the PVN by IHC, 34 of the corresponding mRNAs have also been detected in the same or independent studies (see Supplementary Table 4). A further 9 orphan GPCR mRNAs are also present in the PVN/SON as detected by ISHH (see Supplementary Table 7). Examples of the ISHH patterns of some of these are shown in Fig. 4. The great majority of GPCRs are expressed in both the pPVN and mPVN (e.g., 5-HT1A/2A [370]; α1D-adrenoceptor [280]; apelin APJ [243,327]; calcium-sensing CaS [272]; CRF1 [136]; melanocortin MC4 [201]; prostanoid EP1/4 [244] receptors). Some GPCRs appear to be preferentially expressed in the pPVN (e.g., consistent with regulating stress or autonomic responses), or mPVN (e.g., compatible with regulating water homeostasis or reproductive status) by either IHC and/or ISHH (pPVN: 5-HT2C [118]; angiotensin AT1A [245]; prolactin-releasing peptide PRRP [195] receptors; mPVN: chemokine CXCR4 [44]; neuromedin U NMU2 [260]; κ opioid [299] receptors). One GPCR (neuropeptide FF/neuropeptide AF NPFF1) seems to be PVN-specific in rats [103], although ir-NPFF1 fibers found just dorsal to the SON, as in humans [102], may project to the SON [143] and be responsible for the inhibitory effects of centrally administered NPFF on hypovolemia-induced VP secretion into the blood [10].
Fig. 4.
Examples of in situ hybridization histochemistry (ISHH) for some orphan GPCR mRNAs, and the putative estrogen receptor GPER mRNA (columns), in sections of SON/PVN/hippocampus and pituitary gland (rows) from adult male Sprague Dawley rats. Images are of 12 μm sections hybridized with 35S-UTP labeled riboprobes exposed to film (Amersham Hyperfilm MP) for 6 weeks. As the distribution of the rat GPER mRNA (and protein) has been well characterized [116], and is expressed at low levels in the PVN and SON, the GPER probe acted as a positive (method) control for the orphan probes. A comprehensive mRNA (or protein) distribution for most of the orphans has yet to be described. The GPER probe clearly labels the SON (thin arrow), PVN (filled thick arrow), and anterior and intermediate lobe (long dashed arrow) of the pituitary gland, while no signal is present in the neural lobe. An extremely faint signal is also observed in the SCN (unfilled thick arrow) and CA1/CA2 and CA3 hippocampal regions. The positional arrows of labeled structures shown in the GPER distribution are indicate in subsequent images for the orphan GPCRs. GPR56 transcripts appear to be ubiquitously distributed throughout the sections shown, although a more intense labeling is seen in the SON, CA1–3 and the lateral ventricles (short dashed arrow), and to a lesser extent in the PVN. The intermediate lobe and neural lobe of the pituitary are also intensely labeled with the GPR56 probe, while the anterior pituitary is moderately labeled. GPR108 mRNA is highly expressed in the SCN, SON, PVN, CA1–3 (and dentate gyrus), dorsal third and lateral ventricles, and all three lobes of the pituitary (anterior and intermediate lobe > neural lobe). GPR125 mRNA expression is observed in the dentate gyrus and CA3 of the hippocampus, and the dorsal third and lateral ventricles, with faint expression seen in the PVN/SON. The anterior lobe of the pituitary are strongly labeled with the GPR125 probe with faint, diffuse signal in the intermediate and neural lobes. GPR146 mRNA is present in the PVN/SON, and is highly expressed in the dorsal third and lateral ventricles and anterior lobe of the pituitary, with moderate/faint expression found in intermediate and neural lobes. GPR153 labeling is striking throughout the thalamus, in the SCN, and in several cortical layers, with moderate signal in the PVN/SON, and weak expression in CA1–3 of the hippocampus and anterior pituitary. Sections hybridized with sense riboprobes for all GPCRs as controls showed only background/or were absent of hybridisation signal (data not shown). 3 V, third ventricle; SCN, suprachiasmatic nucleus; PVN, paraventricular nucleus; Th, thalamus; CA1–CA3, CA1–CA3 regions of the hippocampus; D3 V, dorsal third ventricle; LV, lateral ventricle; AP, anterior pituitary; IL, intermediate lobe of the pituitary; NL, neural lobe of the pituitary. The rat orphan GPCR probes were generated by PCR using 125 ng rat genomic DNA (extracted from rat testis) as a template. PCR primers incorporating recognition sequences for restriction endonucleases (underlined) were used to generate products of approximately 300–500 bp in size. All probes were targeted to the 3′-untranslated (UTR) region (or C-terminal into 3′-UTR in the case of GPR125) of each GPCR mRNA. GPR56 primers, upstream: 5′-CCTCTGAATTCGGGGTGCACATGCATGGC-3′; downstream: 5′-CAGACAAGCTTGGAAGATGCTCAGCTCCTA-3′, corresponding to bp2376–2844 of the rat GPR56 gene (Genbank Accession number NM_152242) were used to generate a 469 bp product which yielded a 453 bp probe when digested with EcoRI–HindIII. GPR108 primers, upstream: 5′-ACTTCCCCGAGTTCAGAGATCCGCCTTC-3′; downstream: 5′-AATCAAAGCTTTATGAAGCCCAGGCTCT-3′, corresponding to bp1749–2093 of the rat GPR108 gene (NM_199399) were used to generate a 345 bp product which gave a 329 bp probe following digestion with AvaI–HindIII. GPR125 primers, upstream: 5′-CCAAGGAATTCAGCTGCAGCTGA CCTTGA-3′; downstream: 5′-TTTTTAAGCTTTGGGGAAGGGCAATTTAG -3′, corresponding to bp4198–4549 of the rat GPR125 gene (XM_223485) were used to generate a 352 bp product which gave a 336 bp probe when digested with EcoRI–HindIII. GPR146, upstream: 5′-GGGCCGAATTCCAAGGAGAGGGCCTGACCA-3′; downstream: 5′-TCCTCAAGCTTTAACACTGGTATTTGCGA-3′, corresponding to bp1202–1718 of the rat GPR146 gene (XM_573364) were used to generate a 517 bp product which yielded a 501 bp probe following digestion with EcoRI–HindIII. GPR153, upstream: 5′-CCCCAGAATTCATGCAGACGGAAGAGGC-3′; downstream: 5′-AAGGAAAGCTTGCTCAATAGAACTTGTT-3′, corresponding to 2059–2521 of the rat GPR153 gene (NM_001034855) were used to generate a 463 bp product which gave a 447 bp probe after digestion with EcoRI–HindIII. Recognition sequences for endonucleases facilitated cloning into the RNA-generating vector pGEM4z (Promega, WI, USA), and sense and antisense probes were generated using T7 and SP6 polymerases (antisense: generated with T7 polymerase following linearization with the opposing restriction endonuclease; sense: generated with SP6 polymerase following linearization with the opposing restriction endonuclease) with 35S-UTP and the MAXIscript in vitro kit (Ambion, TX, USA). The integrity of each probe was verified by DNA sequencing. Rat GPR30 probes were generated as previously described [116]. All in situ hybridization experiments were performed as described in detail at http://intramural.nimh.nih.gov/lcmr/snge/Protocols/ISHH/ISHH.html.
4.5. Transcriptomic analysis of GPCR expression in the PVN/SON
RT-PCR-based methods have been used to delineate a partial GPCR transcriptome in a number of tissues including mouse heart [228] and brain [334]. Only the odd study has used PCR to detect the expression of an individual GPCR gene in dissected PVN/SON [58,200,291,310]. Large-scale transcriptome analysis of enriched genes, including some GPCR transcripts, has been performed in a number of mouse brain regions including striatum, frontal cortex, hippocampus and amygdala [19,97,183]. Recently DNA microarray-based transcriptomal analysis of the rat PVN, SON, subfornical organ and area postrema, and mouse SON was reported from our laboratories [124,123,122,308]. There are some limitations associated with such ‘global’ studies in rats as highlighted previously [124]. For example, manual rather than laser dissection of PVN and SON was used so a small amount of surrounding tissue such as the 3rd ventricle could have been included in the samples. In addition, most but not all GPCRs with known ligands, or orphan GPCRs are represented on the Affymetrix 230 2.0 rat genome chip interrogated – examples of some ‘missing’ GPCRs include the bombesin BB3 receptor and the orphan GPCRs GPR101 and GPR165. Furthermore, some rare GPCR transcripts in the PVN and SON may escape detection, or some probe sets may have failed in some or all of the replicates, thus excluding them from analysis – examples of this are the apelin APJ, estrogen GPER, and VP V1A receptors which are readily detected by receptor ARG, IHC and/or ISHH in the PVN and SON. Bearing these points in mind, we have constructed a list of the GPCRs genes considered present by DNA microarrays in the PVN and SON (Supplementary Tables 4–6). The relative abundance of GPCR transcripts in both hypothalamic nuclei varies from those that are highly expressed such as various GABAB subunits, and neurotensin NTS2 and endothelin ETB receptors, to the less highly expressed purinergic P2Y13, adenosine A3, and metabotropic glutamate mGlu4 and mGlu7 receptors. About 80% of GPCR transcripts in the PVN are also present in the SON, and approximately 70% and 50% of transcripts for GPCRs with known ligands in the PVN and SON, respectively, has been validated by receptor ARG, IHC and/or ISHH. This includes some GPCR transcripts (e.g., parathyroid hormone PTH1 and neuropeptide Y Y5 in the PVN/SON) that are towards the lower limits of detection. The GPCR gene lists include 14–16 ‘new’ GPCRs with known ligands, such as adenosine A2B, chemokine CXCR3 and CXCR7, lysophospholipid LPA1 and S1P1, metabotropic glutamate mGlu4, purinergic P2Y13 and protease-activated PAR1 receptors, and 17–21 ‘new’ orphan GPCRs (see Supplementary Table 7) whose localization in the PVN and SON is unvalidated on review of the literature, and which may represent novel targets for future physiological studies. Another interesting feature of the transcriptomic data is that by virtue of multiple oligonucleotide probe sets representing some genes on the array chip, a number of GPCR splice variants appear to be present in the PVN and SON. Alternate splicing of pre-mRNAs is one mechanism for increasing diversity in the transcriptome. Although approximately half of GPCR genes are devoid of introns within their coding sequence, those that possess introns can theoretically undergo alternative splicing and this may have consequences on GPCR functions such as altered pharmacological profiles, constitutive activity and subcellular localization [214]. Examples of GPCRs that exhibit varying degrees of alternate splicing include the GABAB1 subunit [345], NOP opioid [361], metabotropic glutamate [240] endothelin ETA [113] and parathyroid hormone PTH1 [150] receptors, all of which have potential isoforms identified by DNA microarrays in the PVN and SON. Transcriptome analysis of the PVN and SON also reveals four GABAB1 subunit isoforms (a, f, g, j) – and IHC and ISHH studies indicate that at least two GABAB1 subunits (B1a and B1b) are expressed in the PVN and SON [89,22]. There are 12 GABAB1 variants (a-k including c-a and c-b) in total, the majority of which are secreted forms that may confer functional differences to the GABAB1/B2 heterodimer [325].
It is very likely that the number of GPCR genes expressed in the PVN and SON in the DNA microarray studies outlined above is an underestimate, and would be expanded further by transcriptomic experiments on single neurons. High throughput, deep/next generation sequencing (e.g., RNASeq [339]) of single cell cDNA libraries from pPVN, mPVN and SON neurons, similar to that reported for electrophysiologically identified warm sensitive neurons from the anterior hypothalamic pre-optic area [73], would reveal GPCR splicing complexity, rare GPCR transcripts and also those GPCR genes that are co-expressed (and thus are candidates for heterodimerization) in PVN/SON neurons.
4.6. Numbers of GPCRs in the PVN and SON: an overview
Embracing the data from the various detection methods outlined above we have arrived at a conservative estimate of the number of GPCRs expressed in the PVN and SON (Table 1). Of the 224 known non-chemosensory GPCRs in the rat genome 101 are present in the PVN (with a further 14 from unvalidated DNA microarrays), and 80 are present in the SON (excluding another 16 from unvalidated DNA microarrays). Interestingly, of the 132 orphan non-chemosensory GPCRs in the rat genome 22 (9 validated) and 24 (9 validated) are present in the PVN and SON, respectively. The GPCRs encompass the vast majority (33 that are activated by different peptide classes from 46 GPCR families in total) of GPCR families excluding chemosensory and orphan GPCRs present in the rat genome (Table 2). The estimate includes a few instances where GPCR ligands appear to have functional effects (e.g., anaphylatoxin, formyl peptide, kisspeptin, leukotriene, melatonin, motilin, platelet-activating factor and trace amine receptors; see Supplementary Table 9) in the PVN/SON but their presence has not been confirmed by any of the detection criteria reviewed. It should also be emphasized that, as far as we are aware, none of the GPCR cDNAs/genes in the PVN and SON have been sequenced. Variations in GPCR sequences and/or potential splicing patterns may have an impact on the function of PVN/SON GPCRs.
Table 1.
Summary of GPCRs expressed in the rat PVN and SON.
| GPCRs expressed in the PVN and SON | |
|---|---|
| Total number of known GPCRsa | 224 |
| Number of orphan GPCRsa | 96 (class A), 29 (class B) and 7 (class C) = 132 |
| Known GPCRs in rat PVN | 94 + 7 based on functional criteria + 14 unvalidated arrays |
| Orphan GPCRs in rat PVN | 9 by ISHH + 17 unvalidated arrays |
| Known GPCRs in rat SON | 74 + 6 based on functional criteria + 16 unvalidated arrays |
| Orphan GPCRs in rat SON | 9 by ISHH + 21 unvalidated arrays |
Numbers based on lists in the on-line IUPHAR Database of Receptors and Ion Channels (http://www.iuphar-db.org/index.jsp) [111] excluding chemosensory (e.g., olfactory, vomeronasal, taste) receptors and possible spliced (see Supplementary Tables 5 and 6) GPCR variants.
Table 2.
GPCR families expressed in the PVN.
| GPCR families expressed in the PVN | |
|---|---|
| 5-HT | Melanocortin |
| Acetylcholine muscarinic | Metabotropic glutamate |
| Adenosine | Neuromedin U |
| Adrenoceptor | Neuropeptide FF |
| Angiotensin | Neuropeptide S |
| Apelin | Neuropeptide W |
| Bombesin | Neuropeptide Y |
| Bradykinin | Neurotensin |
| Calcitonin | Opioid |
| Calcium-sensing | Orexin |
| Cannabinoid | P2Y |
| Chemokine | Parathyroid hormone |
| Cholecystokinin | Peptide P518 (QRFP) |
| Corticotropin-releasing factor | Prokineticin |
| Dopamine | Prolactin-releasing peptide |
| Endothelin | Prostanoid |
| Estrogen | Relaxin |
| GABAB | Somatostatin |
| Galanin | Tachykinin |
| Ghrelin | Thyrotropin-releasing hormone |
| Glucagon | Urotensin |
| Histamine | VIP & PACAP |
| Melanin-concentrating hormone | Vasopressin and oxytocin |
There are 46 GPCR families expressed in the PVN, including 33 different peptide classes (in italics). Notably absent are lipid-like GPCRs (e.g., lysophospholipids) which were detected in DNA microarrays but whose presence in the PVN (or SON) has not been validated, and the anaphylatoxin, formyl peptide, kisspeptin, leukotriene, melatonin, motilin, platelet-activating factor, and trace amine GPCRs for which there are functional responses in the PVN following central or peripheral administration of agonists, or in HNS cultures in vitro. The vast majority of GPCRs expressed in the PVN are also present in the SON – the exceptions are members of anaphylatoxin, formyl peptide, leukotriene, platelet-activating factor, and trace amine GPCRs which have not been demonstrated in the SON to our knowledge. To date members of the bile acid, free fatty acid, glycoprotein hormone, gonadotropin-releasing hormone and hydroxyl acid GPCRs families do not appear to be expressed in either the PVN and SON.
5. Regulation of GPCR expression in the PVN and SON
There is ample evidence that GPCR expression can be regulated by, and contribute to changes in PVN and SON neuronal plasticity. Levels of GPCRs are determined in part by the rate of receptor protein synthesis, which can be regulated by either transcriptional or post-transcriptional mechanisms. Unless a reserve of “spare” receptors exists, alterations in cell surface or cytoplasmic GPCR levels can significantly influence receptor signaling capacity. GPCR signaling components (e.g., G proteins) themselves are also dynamically regulated [166,232], and ultimately GPCR expression and function is dependent on a host of factors that influence GPCR desensitization (e.g., following chronic activation of many GPCRs), redistribution and degradation. The role of many intracellular signaling molecules (such as GRKs and arrestins) is critical in regulating these processes. RNA regulation is also very complex, with small RNA molecules like microRNAs (miRs) and piwi-interacting RNAs linked to transcriptional silencing, and long non-coding RNAs involved in transcriptional, post-transcriptional (e.g., RNA alternate splicing, translation) and epigenetic regulation [192].
The apparent absence, or low levels of GPCR expression does not preclude the possibility that some GPCRs may be induced by perturbations of PVN and/or SON neuronal function (e.g., change in osmolality, lactation, stress) as in the case of the CRF1 receptor [206]. Changes in mRNA levels are usually easier to detect by ISHH compared to changes in protein as measured by IHC, but this obviously depends on when the mRNA is assayed after experimental manipulations, since GPCR mRNA turnover may vary considerably. GPCR mRNA and protein turnover has been primarily established in cell lines expressing native or cloned GPCRs and could be quite different in the PVN/SON microenvironment. Half-lives are highly variable and often cell context-dependent, ranging from around 2–20 h for both GPCR mRNA (e.g., acetylcholine m1 [177], α1-adrenoceptor [141], α1-adrenoceptor [278], β2-adrenoceptor [109], leukotriene BLT1 [305] receptors) and GPCR protein at the cell surface (adenosine A1/2A/2B/3 [164], α2A/2B/2C-adrenoceptor [282,353], β2-adrenoceptor [71], calcium-sensing CaS [46], cannabinoid CB1 [220] receptors). The mRNA turnover for a number of GPCRs is also decreased by agonist stimulation [57,109,141,177], emphasizing the importance of local agonist levels in the PVN and SON in regulating both GPCR mRNA and protein levels. In a few of these studies, in contrast to research on GPCR mRNA expression in the PVN and SON, nuclear run-on experiments (requiring a million cell nuclei or more) were used to confirm that changes in mRNA levels were the result of changes in GPCR gene transcription. Nuclear run on experiments provide a measure of the frequency of transcription initiation and are largely independent of the effects of RNA stability. Interestingly, other studies using hybridization of DNA microarrays with steady-state mRNA versus newly transcribed (nuclear run on) RNA have shown that approximately half of stress-regulated genes in H1299 lung carcinoma cells are due to changes in gene transcription with a similar fraction due to changes in mRNA turnover [77]. A point that may be relevant to possible GPCR co-expression and cross-talk in the PVN and SON is that the angiotensin AT1 receptor induces bradykinin B2 receptor transcription activation via the phosphorylation of cAMP response element binding protein (CREB) and assembly of p-CREB on the B2 receptor promoter in kidney collecting duct cells [287].
An alternative method to look at gene transcription rates, and one that is particularly amenable to tissue sections of PVN and SON, is to examine heteronuclear (hn)RNA levels. The binding of probes specific for introns in RNA-coding region of genes can be used to quantify hnRNA levels as an indirect measurement of the transcription rate of genes in response to a particular stimulus. For GPCR genes that contain multiple introns care must be exercised in choosing which introns to target because they can be excised from the nascent pre-mRNA at different rates [174]. ISSH with intron-specific probes has been successfully used to measure hnRNA changes for relatively abundant neuropeptide (e.g., VP, OT and to a lesser extent CRF [120,169,369]) mRNAs, but has not proved particularly useful to assess GPCR transcriptional activity. One exception is the dopamine D2 mRNA distribution in the brain where hnRNA levels are (as expected) a fraction of steady-state mRNA levels [87].
There are numerous studies showing that the expression of PVN/SON neuropeptides, in particular VP, OT and CRF, are developmentally regulated [6,16,317], and that their expression can be altered by experimental manipulations [42,2]. In comparison, reports of ontogenetic variations in GPCR expression in the PVN/SON are scarce, with the transcript or protein level, and/or function of a few GPCRs including the angiotensin II AT1a (mRNA present in PVN E19 onwards [241]), neuropeptide Y1 (mRNA present in PVN P2 onwards coincident with a significant increase in NPY-containing fibers innervating the nucleus [106]), and melanocortin MC4 (mRNA present in PVN and SON at E18 and P27, respectively, approximating the appearance of melanocortin binding sites [162,193]) changing developmentally. At least one GPCR in the PVN and SON is also diurnally regulated – α2-adrenoceptor expression in the PVN peaks at the onset of dark (when CORT levels are highest) whereas in the SON the reverse diurnal pattern is observed [144].
There have been many studies using receptor ARG, IHC or ISHH to demonstrate alterations in GPCR expression by pharmacological or physiological manipulations. More recently, transcriptome approaches have established that dehydration alters the levels of transcripts encoding the cannabinoid CB1, GABAB1j, melanocortin MC4, protease-activated PAR1 and somatostatin sst3 receptors in the rat SON [124]. Changes in GPCR protein and mRNA levels in the PVN/SON in response to agonist or antagonist administration, or physiological perturbations such as adrenalectomy, salt-loading, dehydration, lactation, gestation and stress are commonly less than twofold, but 8–10-fold or higher increases in GPCR mRNA have been reported in some instances – e.g., for the apelin APJ receptor [242] (see Supplementary Table 8). Invariably gene or protein expression has been imaged over the entire PVN and/or SON, so any change in cell-to-cell GPCR expression is often obscured. Importantly, since the vast majority of studies investigate a single experimental time point, it is surprising to note how often it is assumed that changes in GPCR mRNA reflect changes in GPCR protein levels and perhaps receptor function. That this may not always be the case is emphasized in studies where the correlation between mRNA and protein levels has been investigated using transcriptomic- in conjunction with proteomic-approaches. For example, in kidney inner medullary duct cells a large number (approx. 1/3) of proteins that showed significant changes in abundance in kidney inner medullary collecting duct cells following challenge with dDAVP (desmopressin; a VP V2 receptor agonist) did not show a changes in the corresponding mRNA species (measured by interrogating DNA microarrays) [159]. While this result relies heavily on the quantitative accuracy of the methods used, it conceivably highlights an important role in post-transcriptional regulation of protein abundance, and also obviously reflects the dynamics of mRNA versus protein turnover. Impressively, given that the half-life of GPCR mRNA or protein is usually not known, a number of studies have combined receptor ARG (or in some cases IHC) with ISHH to show that alterations in GPCR mRNA levels in the PVN/SON are associated with changes in the corresponding GPCR protein. A few examples of this are the increases in angiotensin AT1A receptor after antagonist administration [210,346], and cholecystokinin CCK1 and CCK2 [125,222], and galanin GAL1 [41] receptors following osmotic perturbations.
There are other, largely unexplored and speculative ways in which GPCRs in the PVN and SON could possibly be regulated. One such mechanism is microRNA (miR)-mediated post-transcriptional regulation. There is substantial evidence that the 3′-UTR of proteins can affect mRNA stability and is involved in regulating gene expression at the post-transcriptional level, and in the case of some GPCRs such as the opioid receptors the length of the 3′-UTR influences receptor protein level [358]. MiRs are short, single-stranded non-protein coding RNAs that tend to suppress target gene expression by binding to their complementary mRNA sequences usually in introns or exons of the 3′-UTR, and have emerged as crucial modulators of gene expression especially in synaptic plasticity. The feasibility of mIR-mediated GPCR mRNA regulation has been demonstrated by miR-23b inhibition of opioid μ receptor expression [358]. Conversely, opioid μ receptor agonists regulate miR-190 activity [372]. Scanning individual GPCRs for consensus miR binding sites that are conserved between species would be a starting point for studies on the potential role of miRs in regulating PVN/SON GPCRs. It is also becoming increasingly clear that epigenetic control of gene (especially CRF and VP) expression in the PVN is important in the HPA axis response to stress (e.g., see [74,233]). DNA methylation and histone modifications have been shown to coincide with the differential expression of the opioid μ receptors in the brain [135].
As noted previously, some GPCRs have very low expression levels (e.g., <1000 receptor copies/cell) and ultimately the demonstration of a ligand-specific function is paramount. For those GPCRs investigated, a functional response has generally been observed where GPCR binding sites, ir-protein and/or mRNA have been detected in the PVN/SON.
6. Functions of GPCRs in the PVN and SON
The actions of numerous neurotransmitters, neuropeptides and hormones in the PVN and SON have been well documented (e.g., [17,63,114,202,204,265,298,316]) and only some salient features will be described here. The tonic and stimulated activity of the PVN and SON is regulated by a number of excitatory and inhibitory neurotransmitters and neuromodulators, including glutamate and GABA, the main excitatory and inhibitory neurotransmitters, respectively, as well as a host of other effectors including angiotensin II, catecholamines, histamine and numerous other neuropeptides that activate GPCRs, and mediators such as humoral factors and nitric oxide (e.g., [37,38,76,140,151,190,298,331]). This regulation can occur directly in the PVN or SON via the effects of neurotransmitters/neuropeptides synthesized within the two nuclei and/or indirectly by interactions with glutamatergic or GABAergic interneurons or afferent projections from other hypothalamic or extrahypothalamic areas that innervate the PVN or SON [82,146,298]. Apparent mismatches between neurotransmitters/neuropeptides and their receptors that are prevalent in the brain [119] may not be such an issue in the PVN and SON where GPCR ligands are available from a number of sources within the nuclei or extra-PVN/SON locations.
In addition to their peptidergic or neurotransmitter phenotypes, neurons in the pPVN, and mPVN and SON have defined electrophysiological characteristics. Classically, under basal conditions OT magnocellular cells are continuously active, whereas the activity of VP magnocellular cells ranges from continuously active to robust phasic to relatively silent [36,204]. Early studies indicated that mPVN and SON neurons have similar electrophysiological properties [11,221,323] whereas pPVN cells exhibited electrophysiological heterogeneity [323]. Neurosecretory neurons concentrated in the medial pPVN have no low threshold spike (LTS) and small T-type Ca2+ currents while in non-neurosecretory cells in the dorsal and ventral pPVN the converse is true [207]. In magnocellular cells bursts of activity often characterize periods of enhanced neuropeptide release. For example, during suckling in the lactating rat and in pregnant animals OT magnocellular neurons discharge synchronously to release large amounts of OT into the systemic circulation which is dependent on dendritic OT release [196,204], and VP magnocellular cells increase their firing (and may switch to phasic activity) to release VP following dehydration [185,337] and hemorrhage [338].
The effects of GPCR ligands on PVN and SON neuronal function can be direct or indirect depending upon whether they are administered peripherally, centrally via the circumventricular organs, or intra-nuclei by injection or iontophoretic application. It should be borne in mind that high doses of GPCR agonists may give ‘pharmacological’ rather than physiological responses, especially when compounds are applied in the vicinity of their presumed site of action. GPCR activation in the PVN/SON has been demonstrated in a number of ways. These include increases in neuronal immediate early gene (e.g., c-fos) activation, changes in electrophysiological characteristics or neuropeptide mRNA or protein levels (e.g., by ISHH, ICH or content of push–pull perfusates or microdialysates), and alterations in any number of physiological end-points such as plasma VP, OT, CRF and ACTH release, water and energy homeostasis, cardiovascular parameters, nociception and behavior (see Supplementary Table 9 for some examples). The specificity of the ligand–GPCR interaction is usually demonstrated by the inhibition of responses with GPCR-selective antagonists or, as in a few cases, by immunoneutralization with neuropeptide/GPCR antibodies (e.g., for NPFF effects on VP release [364]), and more recently by RNA interference-driven gene silencing that has the added advantage over acute administration of synthetic small interfering RNAs of long-term (days–months) GPCR knockdown if viral, GPCR-specific small hairpin (sh)RNA constructs are employed. The sustainable expression of such constructs obviates some of the problems that may be encountered with long GPCR mRNA turnover rates.
6.1. General features of GPCR function in the PVN and SON
With amplification procedures used in various GPCR detection techniques, an important question is what level of GPCR mRNA or protein is physiologically relevant? Radioligand- or fluorescent-ligand binding assays can detect as few as about 50–100 GPCRs per cell (e.g., see [212]) which is sufficient to elicit (although higher levels are probably required to sustain) a signal transduction response in some in vitro systems [297]. In PVN and SON neurons in vivo some GPCRs may be clustered to concentrate their levels at pre- or post-synaptic sites. A number of studies underscore the differences in the sensitivity/specificity of detection techniques used between laboratories, and highlight the importance of obtaining (specific) functional GPCR responses. For example, while VP V2 receptor mRNA was not detected in the PVN or SON by nested PCR in one study [132], V2 receptor mRNA (by PCR on RNA obtained from 20 neurons), V2 receptor protein and apparent functional responses have recently been reported in isolated cells from the SON [281]. Similarly, the lack of angiotensin II AT1A receptor gene expression in the mPVN by ISHH in some studies (e.g., [186]) appears at odds with the AT1-type pharmacological responses observed by electrophysiology in PVN slices [176]. Furthermore, prostanoid EP3 receptor electrophysiological responses have been observed in the SON [290] where no ir-EP3 receptor cell bodies or fibers have been found [234].
It is possible that some of the GPCR effects in the PVN or SON are spurious or redundant in nature, since it is difficult to envisage that every GPCR we have listed (see Tables 1 and 2) has an important role in co-ordinating control of PVN and/or SON function. We are reminded of a comment attributed to Alfred Gilman a number of years ago: “A typical cell has perhaps 50 different receptors, and the cell doesn’t pay attention to just one receptor at a time. How does it know how to interpret the signal from one hormone when it’s listening to 45 other ones at the same time? How does the whole signaling system work as a network? That’s what we want to find out” [184]. Functional studies of GPCRs indicate that they do have individual roles in the PVN and SON and are probably key to neurones integrating multiple functions as outline below (see Supplementary Table 9).
Change in the levels of intracellular signal transduction molecules (see Section 4.1) and immediate early gene activation [126,127] are frequently used as indices of neuronal activity in the PVN and SON, and are particularly amenable to cell imaging techniques. For example, agonist-induced increases in intracellular Ca2+ or ERK activation have been shown for 5-HT1A [61], α1A-adrenoceptor [301], dopamine D4 [23], melanocortin MC4 [277], purinergic P2Y1 [302], OT [24,172,277], VIP/PACAP [66] and VP V1A [104] receptors. These are often accompanied by increases in PVN or SON c-fos expression, as demonstrated for many GPCRs such as the 5-HT2A/2C [180], CRF1 [251], dopamine D4 [23], glucagon GLP-1 [175], melanocortin MC4 [157], motilin [359], neuropeptide FF/neuropeptide AF NPFF1 [145], prolactin-releasing peptide PRRP [218,362] and tachykinin NK3 [157] receptors. One of the most extensively studied functional aspects of GPCRs in pPVN presympathetic and/or endocrine, mPVN and SON neurons, is their often profound affects on neuronal excitability, examples of which are shown in Supplementary Table 9, and include presynaptic effects mediated via metabotropic glutamate receptors [28,29,284] and endocannabinoids (acting through cannabinoid CB1 receptors) [68,277] in the SON, and GABA release in presympathetic pPVN neurons [49,188].
GPCR activation in the PVN/SON can alter neuropeptide or GPCR gene synthesis (e.g., see [3,79,80,167,201,346]) and/or the release of neurotransmitters/neuropeptides from dendrites and/or axon terminals. Local dendritic release of neuropeptides acting in an autocrine or paracrine fashion are likely to be important factors in determining the sensitivity and plasticity of PVN and SON neurons to their multitude of inputs [173,202,204,231]. Dendritic peptides may also regulate local blood flow [5] and have local (e.g., OT is anxiolytic via the PVN OT receptor [333]) and distant effects on behavior [204]. Examples of GPCRs that modulate neuropeptide release, typically performed in studies measuring VP and/or OT release from large magnocellular cells, rather than CRF release from the smaller pPVN neurons, include the α1-adrenoceptors (inhibit intra-PVN hypoxia-induced CRF release [50]), apelin APJ (increases firing rate of VP neurons and VP dendritic release [327]), histamine H1/2 (increases dendritic release of OT via stimulating noradrenaline release [18]), melanocortin MC4 (increases Ca2+ in OT neurons; stimulation of dendritic, and inhibition of terminal OT release [204,276]), κ opioid (locally released dynorphin inhibits VP neurons and is essential for expression of VP neuron phasic activity; inhibits VP terminal release [34,36]), VIP/PACAP (stimulates somatodendritic and terminal VP release [208,289]), VP V1A (acting on autoreceptors to excite and inhibit quiescent and phasic VP neurons, respectively [35,203,204]), and OT (stimulates dendritic OT release via OT receptor; inhibits OT neurons by increasing endocannabionoid inhibition of glutamate release [204]) receptors.
The release of neurohypophysial hormones from posterior pituitary nerve terminals, and CRF and other pPVN products from the median eminence into the anterior pituitary portal circulation is often reflected by increased circulating levels of VP and OT, ACTH (due to the action of CRF, VP and other ACTH secretagogues) and CORT, and thyroid hormones, and in changes in water homeostasis (principally brought about by altered VP secretion) (Supplementary Table 9 gives some examples). GPCRs can also modulate autonomic functions by activating secretory and non-secretory pPVN neurons. For example, central or intra-PVN administration of a number of GPCR ligands results in orexigenic (e.g., ghrelin [291], galanin [171], and NPY agonists via Y1 and Y5 [151] receptors) or anorexigenic (e.g., via CRF1 [117], melanocortin MC4 [94], neuropeptide S NPS [78], and neuromedin U [357] receptors) effects, and alter cardiovascular parameters (e.g., angiotensin AT1 [13], CRF2 [189], tachykinin NK3 [320], and urotensin II UT [342] receptors), nociception (e.g., α-adrenoceptors [374]), body temperature (e.g., acetylcholine muscarinic receptors [319]), and penile erection (e.g., dopamine receptors [312]).
6.2. Possible GPCR co-expression in the PVN and SON
We do not know how many GPCRs are co-expressed in PVN/SON neurons, and different complements of GPCRs may be expressed in subsets of neurons such as magnocellular VP cells with different basal electrical activity, magnocellular neurons with different neuropeptidergic phenotypes, mPVN versus pPVN neurons, or pPVN endocrine versus non-endocrine neurons. However, extrapolating from the study on single warm-sensitive neurons (transcriptomic analysis gave 168 non-olfactory GPCRs of which 27 are orphans [73]) suggests that the number of co-expressed GPCRs is likely to be larger than the number of co-expressed neuropeptides. At least 20 different neuropeptides are co-expressed in magnocellular VP or OT neurons [39] but the extent of the total overlap is unknown. The co-expression of GPCRs raises the question of possible functional consequences of receptor oligomerization in the PVN and SON. The formation of functional GABAB receptors from two GABAB subunits is an example of GPCR heterodimerization that we know occurs in the PVN and SON [373]. Of the GPCRs listed in Supplementary Table 4, there is also a high degree of colocalization of 5HT1A and 5HT2A in OT and CRF neurons in the PVN where activation of one receptor subtype may induce the desensitization of the other [370]. There are many examples of apparent GPCR homodimerization and heterodimerization in the literature [225], and a number of consequences of GPCR oligomerization such as changes in receptor expression, compartmentalization, recycling, turnover and degradation have been noted mainly in in vitro studies [88,304]. Assuming that oligomerization is relatively stable, co-expressed GPCRs may allow graded regulation of a population of functionally equivalent neurons in the PVN and SON, as receptor ratios and the levels of their corresponding ligands vary as a function of the physiological and pharmacological state. This could mean that with oligomerization between GPCRs of the same subclass it is possible that the heterodimer acts as a ‘concentration-dependent switch’ where one GPCR is activated by low agonist concentrations whereas the other is activated by higher agonist concentrations. The signaling of one GPCR could be shut down while the other is active, e.g., by internalization of the ‘inactive’ GPCR (e.g., see co-expressed adenosine A1/2A receptors [55]; note that the four adenosine receptor subtypes are all possibly expressed in the PVN (see Supplementary Table 4)). Moreover, the heterodimer may have new signaling modalities e.g., switching to coupling to a new G protein to activate a new signaling pathway (e.g., see co-expressed dopamine receptors [179]). To add to the complexity, GPCRs may also physically associate with non-GPCRs e.g., the dopamine D5 receptor and the GABAA γ2 ligand-gated ion channel subunit appear to complex leading to an attenuation in D5 receptor-mediated cAMP accumulation and GABAA-mediated current [198].
6.3. Possible function of orphan GPCRs
Some orphan GPCRs, or indeed some GPCRs with known endogenous ligands, may be constitutively active in the PVN and SON. This is not as far-fetched as it may seem since constitutive activity in GPCRs is a relatively well-known phenomenon that can be signaling pathway-dependent, and can result from the overexpression of receptors in native tissue or heterologous systems, and/or by changes in the DNA (introduced or somatic mutations) or RNA (visa vi RNA editing as in the 5-HT2C receptor [213]) sequence of GPCRs. For example, isoforms of the histamine H3 receptor are constitutively active pre- and post-synaptically in native brain cortical tissue [230], and in cell lines α1A- and α1B-adrenoceptors (which can heterodimerize) [60], bradykinin B2 [261], ghrelin [129], melanocortin MC4 [239] and neurotensin NTS2 [129] receptors exhibit constitutive activity, and co-expression of the constitutively active histamine H1 receptor with the 5-HT1B receptor confers constitutive activity on the latter receptor [14]. All these GPCRs are expressed in the PVN and SON. The orphan GPCRs GPR3, 6, 12, 20, 26 (present in SON by DNA microarrays), 39, 61 (present in PVN and SON by DNA microarrays) and 78 also alter basal signal transduction activity when expressed in vitro [129,148,321,329]. Although we may be able to predict changes in GPCR activity based on altered GPCR sequences, the demonstration of constitutive activity in the PVN and SON needs to be functionally-based. A component of the high, basal [35S]GTPγS labeling in the rat PVN [1] may reflect constitutive basal activity of known and/or orphan GPCRs. Highly expressed, constitutively active GPCRs may account in part for the molecular mechanisms regulating signal transduction effectors in PVN/SON neurons. Some of these molecules e.g., cAMP, Ca2+, have key roles in axonal growth of developing or regenerating neurons (e.g., [226]). Constitutive activity may also underlie ligand-independent functions of orphan GPCRs such as involvement in GPCR heterodimerization and altering target GPCR function – an example of this is the orphan GPCR GPR50 heterodimerizing with the melatonin MT1 receptor to inhibit its activity (see [187]). In fact, constitutive activity is observed in the PVN and SON. For example, nitric oxide whose generation is enhanced by many GPCR agonists, and which has general inhibitory neuroendocrine and autonomic effects in the PVN and SON [306], constitutively restrains ongoing firing in SON neurons [307]. As to GPCR-‘specific’ effects, very recently the melanocortin MC4 receptor was shown to be constitutively active in the mouse PVN [96].
There are a number of candidate substances that may be ligands for orphan GPCRs expressed within the PVN and SON. These include peptides that modulate PVN/SON function and/or are perhaps expressed in mPVN and SON, or pPVN neurons. Various peptides derived from larger precursor molecules (and isolated by proteomic methods) are expressed in the PVN/SON, such as: (1) the neuroendocrine regulatory peptides (NERPS-1/2), which are products of the VGF gene that colocalize with VP in the storage granules of the PVN and SON of both rats and humans, and suppress basal, hypertonic saline- or angiotensin II-induced VP release [328,363]; (2) neuronostatin, a product of the somatostatin gene that depolarizes or hyperpolarizes PVN magnocellular, parvocellular or preautonomic neurons and administered centrally increases blood pressure and decreases food intake and water drinking [279]; (3) nesfatin-1, an amino-terminal fragment derived from NEFA/nucleobindin 2 (NUCB2) [93] that is present in VP and OT neurons [30], elevates intracellular Ca2+ in dissociated hypothalamic [30] and isolated PVN [211] neurons, alters the electrophysiological properties of PVN neurons [257], increases OT release from PVN tissue slices [211] and administered centrally increases c-fos in the PVN/SON and decreases food intake via an OT-dependent, leptin-independent melanocortin pathway [211,93] (note that it has been reported that nesfatin activates GPR12 [229], an orphan GPCR which exhibits constitutive activity [321]); and (4) augurin, a product of the c2orf40 gene which encodes the esophageal cancer-related gene 4 (ECRG4) protein) [318] that is present in PVN and SON OT and VP neurons [271], increases VP and CRF release from hypothalamic explants and elevates plasma ACTH levels when administered centrally or intra-PVN [318]. It is interesting to note that peptidomics of the rat SON has identified 20 unique peptides from known pro-hormones [27]. Candidate orphan GPCR ligands are not restricted to peptides and their by-products and post-translationally modified counterparts, but could also include compounds such as steroids (e.g., glucocorticoids) that are known to interact with the PVN/SON. There are a number of ‘fast’, apparently non-genomic effects of steroids [199] and their metabolites (e.g., see [236]) that may be mediated by GPCRs, including chemosensory receptors, in the PVN/SON and other brain regions. A comparison of brain region and peripheral tissue localization and effects of candidate orphan GPCR ligands with the anatomical distribution of orphan GPCR gene expression could possibly contribute to GPCR ‘deorphanization’ in the PVN and SON.
7. Concluding remarks
The neuronal universe of GPCRs and associated signaling components in the PVN and SON is expanding: removal of one constituent may not upset the fabric of the system in its basal state (e.g., there is probably some redundancy in the system) but we can measure alterations in individual elements, and these may influence the function of the system as a whole as it responds to different stimuli. It is evident that GPCR gene expression and protein data, preferably verified by at least two methods, needs to be complemented with functional data. Single cell transcriptomic profiling (including deep sequencing) will likely extend the number of potentially functional GPCRs in PVN and SON neurons, but such studies will possibly have to sample a number of different neuronal populations to deal with the heterogenous nature of the cells. These experiments can be performed on electrophysiologically-identified neurons, or on cells that have been identified by complementary techniques such as high-resolution 2-photon Ca2+ imaging that has been extensively used in other brain regions like the hippocampus (e.g., [258]). GPCRs are not abundant compared to most cytoplasmic proteins, and are difficult to analyze by gel-based techniques such as 2D-difference gel electrophoresis (DIGE) due to their inherent hydrophobicity and insolubility in standard detergents. Global proteomic approaches to analyze GPCR expression are still not within reach, currently requiring methods such as selectively tagging (e.g., by biotinylation) cell surface proteins, various chromatography techniques including immobilized-metal affinity chromatography (IMAC), or the isotope-coded affinity tag (ICAT) method prior to protein analysis by mass spectrometry [344].
It is likely in the future that high-resolution RNA-[347] and protein-tracking methods will be used in conjunction with functional imaging to study the consequences of spatial and temporal changes in GPCR expression in the PVN, SON and elsewhere in the brain. Concerning the detection of GPCR proteins themselves, although fluorescent and biotinylated GPCR ligands have been available since the 1970s, it is only fairly recently that improved fluorophores and conjugation methods with increased signal/noise ratios and bioactivity have made these compounds viable alternatives to radiolabeled compounds in viewing the native tissue distributions of GPCRs. For example, while fluorescent GPCR ligands may not have been specifically applied to either PVN or SON sections or viable tissue, they have been used to detect relatively abundant GPCRs such as α-adrenoceptors in arteries and dopamine receptor subtypes in brain [8,64]. We are in the midst of an era where fluorescent GPCR ligands can also potentially be used to investigate GPCR internalization and fluorescence resonance energy transfer (FRET)- and bioluminescence energy transfer (BRET)-based measurements to reveal oligomer formation between homologous or heterologous GPCRs, or between other proteins in single PVN/SON cells or within whole tissue [4].
Undoubtedly valuable physiological information will be obtained by the continued use of murine (and perhaps future rat) GPCR knockout models, even though there are ongoing concerns over compensatory mechanisms possibly distorting phenotypes in global knockouts, potentially different physiological phenotypes (e.g., behavior) on different genetic backgrounds, and the different PVN cytoarchitecture between rats and mice [352]. One mouse line with conditional PVN transcriptional re-activation (i.e., functional recovery) of a GPCR has been reported (melanocortin MC4 receptor [15]) but to our knowledge no inducible (e.g., by drugs such as tetracyclin) PVN/SON GPCR knockouts are available. ‘Translational’ research dictates the importance of applying scientific discoveries into practical applications like improving human health. Variations in GPCR agonist levels or in GPCRs themselves, e.g., brought about by exposure to stressors, is potentially relevant to a number of human conditions such as depression and cardiovascular disorders where GPCR changes may promote pathological outcomes. Studies on GPCRs in the human PVN and SON are relatively scarce and often fraught with over-interpretation when compared with rat experiments, not least because the human PVN does not have the clear anatomical demarcations as its rat equivalent [314]. Species differences in brain GPCR distribution are also not uncommon (and may partly underlie some behavioral phenotypes [367]), advising caution in extrapolating data on GPCRs from animals to humans. However, conservation of GPCR expression in the PVN/SON between rodents and humans or non-human primates reinforces the idea that a particular GPCR may have an important functional role. For example, the 5-HT1A/1C [252], β2-adrenoceptor [197], dopamine D1/2/3/5 [108,270], neuropeptide Y5 [238] and tachykinin NK3 [168] receptors are all present in the human PVN and SON, while CRF1 and VP V1A receptor transcript levels appear to be elevated in the PVN of depressed patients [340]. Other GPCRs like the free fatty acid FFA1 [209] and melatonin MT1 [360] receptors are present in the primate PVN and SON by IHC but to date have not been shown in the same structures in the rat. A number of studies in humans are compatible with those in rats suggesting GPCR action in the PVN. For example, peripheral melatonin modulates the VP response to exercise and hypertonic saline infusion [86], while naloxone (a μ-opioid receptor blocker) enhances the plasma ACTH response to CRF [56]. In non-human primates, the odd study has investigated the effects of intranasal [250] and central [296] administration of GPCR ligands on PVN-based activity. Further exploration of GPCR expression and function in the PVN and SON of humans and experimental animals, including correlative studies on the possible impact of GPCR gene variations (e.g., single nucleotide polymorphisms), will contribute significantly to unraveling the influence of GPCRs on the homeostatic roles of the PVN and SON under normal conditions and in disease states.
Acknowledgments
GGJH and GRP are supported by PhD Fellowships from the Biotechnology and Biological Sciences Research Council (BBSRC), UK. Support was also received from the British Heart Foundation (CCH and DM), BBSRC (CCH, DM and AMO’C), Medical Research Council UK (DM), Neuroendocrinology Charitable Trust UK (JAR and SJL) and the Wellcome Trust UK (SJL and AMO’C).
Footnotes
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.yfrne.2011.07.002.
Appendix A. Supplementary material
GPCR signal transduction components detected in the PVN by DNA microarrays.
GPCR signal transduction components detected in the SON by DNA microarrays.
GPCRs detected in the rat PVN and SON by receptor ARG.
GPCRs in the paraventricular nucleus (PVN) and supraoptic nucleus (SON) of the rat hypothalamus: a summary of the literature.
GPCRs noted as present in rat PVN arrays.
GPCRs noted as present in rat SON arrays.
Orphan GPCRs in the rat PVN & SON.
Examples of GPCR regulation in the PVN and SON.
Some functions of GPCRs in the rat PVN/SON.
References for Supplementary Tables.
References
- 1.Aaltonen N., Palomäki V.A., Lecklin A., Laitinen J.T. Neuroanatomical mapping of juvenile rat brain regions with prominent basal signal in [(35)S]GTPgammaS autoradiography. J. Chem. Neuroanat. 2008;35:233–241. doi: 10.1016/j.jchemneu.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 2.Aguilera G., Subburaju S., Young S., Chen J. The parvocellular vasopressinergic system and responsiveness of the hypothalamic pituitary adrenal axis during chronic stress. Prog. Brain Res. 2008;170:29–39. doi: 10.1016/S0079-6123(08)00403-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Barazanji K.A., Wislon S., Baker J., Jessop D.S., Harbuz M.S. Central orexin-A activates hypothalamic–pituitary–adrenal axis and stimulates hypothalamic corticotropin releasing factor and arginine vasopressin neurones in conscious rats. J. Neuroendocrinol. 2001;13:421–424. doi: 10.1046/j.1365-2826.2001.00655.x. [DOI] [PubMed] [Google Scholar]
- 4.Albizu L., Cottet M., Kralikova M., Stoev S., Seyer R., Brabet I., Roux T., Bazin H., Bourrier E., Lamarque L., Breton C., Rives M.L., Newman A., Javitch J., Trinquet E., Manning M., Pin J.P., Mouillac B., Durroux T. Time-resolved FRET between GPCR ligands reveals oligomers in native tissues. Nat. Chem. Biol. 2010;6:587–594. doi: 10.1038/nchembio.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alonso G., Gallibert E., Lafont C., Guillon G. Intrahypothalamic angiogenesis induced by osmotic stimuli correlates with local hypoxia: a potential role of confined vasoconstriction induced by dendritic secretion of vasopressin. Endocrinology. 2008;149:4279–4288. doi: 10.1210/en.2008-0387. [DOI] [PubMed] [Google Scholar]
- 6.Altstein M., Gainer H. Differential biosynthesis and posttranslational processing of vasopressin and oxytocin in rat brain during embryonic and postnatal development. J. Neurosci. 1988;8:3967–3977. doi: 10.1523/JNEUROSCI.08-11-03967.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Antoni F.A. Vasopressinergic control of pituitary adrenocorticotropin secretion comes of age. Front. Neuroendocrinol. 1993;14:76–122. doi: 10.1006/frne.1993.1004. [DOI] [PubMed] [Google Scholar]
- 8.Ariano M.A., Monsma F.J., Barton A.C., Kang H.C., Haugland R.P., Sibley DR D.R. Direct visualization and cellular localization of D1 and D2 dopamine receptors in rat forebrain by use of fluorescent ligands. Proc. Natl. Acad. Sci. USA. 1989;86:8570–8574. doi: 10.1073/pnas.86.21.8570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arima H., House S.B., Gainer H., Aguilera G. Direct stimulation of arginine vasopressin gene transcription by cAMP in parvocellular neurons of the paraventricular nucleus in organotypic cultures. Endocrinology. 2001;142:5027–5030. doi: 10.1210/endo.142.11.8595. [DOI] [PubMed] [Google Scholar]
- 10.Arima H., Murase T., Kondo K., Iwasaki Y., Oiso Y. Centrally administered neuropeptide FF inhibits arginine vasopressin release in conscious rats. Endocrinology. 1996;137:1523–1529. doi: 10.1210/endo.137.5.8612481. [DOI] [PubMed] [Google Scholar]
- 11.Armstrong W.E., Smith B.N., Tian M. Electrophysiological characteristics of immunochemically identified rat oxytocin and vasopressin neurones in vitro. J. Physiol. 1994;475:115–128. doi: 10.1113/jphysiol.1994.sp020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aznavour N., Benkelfat C., Gravel P., Aliaga A., Rosa-Neto P., Bedell B., Zimmer L., Descarries L. MicroPET imaging of 5-HT 1A receptors in rat brain: a test-retest [18F]MPPF study. Eur. J. Nucl. Med. Mol. Imaging. 2009;36:53–62. doi: 10.1007/s00259-008-0891-1. [DOI] [PubMed] [Google Scholar]
- 13.Bains J.S., Potyok A., Ferguson A.V. Angiotensin II actions in paraventricular nucleus: functional evidence for neurotransmitter role in efferents originating in subfornical organ. Brain Res. 1992;599:223–229. doi: 10.1016/0006-8993(92)90395-p. [DOI] [PubMed] [Google Scholar]
- 14.Bakker R.A., Casarosa P., Timmerman H., Smit M.J., Leurs R. Constitutively active Gq/11-coupled receptors enable signaling by co-expressed G(i/o)-coupled receptors. J. Biol. Chem. 2004;279:5152–5161. doi: 10.1074/jbc.M309200200. [DOI] [PubMed] [Google Scholar]
- 15.Balthasar N., Dalgaard L.T., Lee C.E., Yu J., Funahashi H., Williams T., Ferreira M., Tang V., McGovern R.A., Kenny C.D., Christiansen L.M., Edelstein E., Choi B., Boss O., Aschkenasi C., Zhang C.Y., Mountjoy K., Kishi T., Elmquist J.K., Lowell B.B. Divergence of melanocortin pathways in the control of food intake and energy expenditure. Cell. 2005;123:493–505. doi: 10.1016/j.cell.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 16.Baram T.Z., Lerner S.P. Ontogeny of corticotropin releasing hormone gene expression in rat hypothalamus – comparison with somatostatin. Int. J. Dev. Neurosci. 1991;9:473–478. doi: 10.1016/0736-5748(91)90033-i. [DOI] [PubMed] [Google Scholar]
- 17.Bealer S.L., Armstrong W.E., Crowley W.R. Oxytocin release in magnocellular nuclei: neurochemical mediators and functional significance during gestation. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;299:452–458. doi: 10.1152/ajpregu.00217.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bealer S.L., Crowley W.R. Stimulation of central and systemic oxytocin release by histamine in the paraventricular nucleus: evidence for an interaction with norepinephrine. Endocrinology. 1999;140:1158–1164. doi: 10.1210/endo.140.3.6601. [DOI] [PubMed] [Google Scholar]
- 19.Becker J.A., Befort K., Blad C., Filliol D., Ghate A., Dembele D., Thibault C., Koch M., Muller J., Lardenois A., Poch O., Kieffer B.L. Transcriptome analysis identifies genes with enriched expression in the mouse central extended amygdala. Neuroscience. 2008;156:950–965. doi: 10.1016/j.neuroscience.2008.07.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benarroch E.E. Paraventricular nucleus, stress response, and cardiovascular disease. Clin. Auton. Res. 2005;15:254–263. doi: 10.1007/s10286-005-0290-7. [DOI] [PubMed] [Google Scholar]
- 21.Birnbaumer L., Abramowitz J., Brown A.M. Receptor–effector coupling by G proteins. Biochim. Biophys. Acta. 1990;1031:163–224. doi: 10.1016/0304-4157(90)90007-y. [DOI] [PubMed] [Google Scholar]
- 22.Bischoff S., Leonhard S., Reymann N., Schuler V., Shigemoto R., Kaupmann K., Bettler B. Spatial distribution of GABA(B)R1 receptor mRNA and binding sites in the rat brain. J. Comp. Neurol. 1999;412:1–16. [PubMed] [Google Scholar]
- 23.Bitner R.S., Nikkel A.L., Otte S., Martino B., Barlow E.H., Bhatia P., Stewart A.O., Brioni J.D., Decker M.W., Moreland R.B. Dopamine D4 receptor signaling in the rat paraventricular hypothalamic nucleus: evidence of natural coupling involving immediate early gene induction and mitogen activated protein kinase phosphorylation. Neuropharmacology. 2006;50:521–531. doi: 10.1016/j.neuropharm.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 24.Blume A., Bosch O.J., Miklos S., Torner L., Wales L., Waldherr M., Neumann I.D. Oxytocin reduces anxiety via ERK1/2 activation: local effect within the rat hypothalamic paraventricular nucleus. Eur. J. Neurosci. 2008;27:1947–1956. doi: 10.1111/j.1460-9568.2008.06184.x. [DOI] [PubMed] [Google Scholar]
- 25.Bobrow M.N., Harris T.D., Shaughnessy K.J., Litt G.J. Catalyzed reporter deposition, a novel method of signal amplification. Application to immunoassays. J. Immunol. Methods. 1989;125:279–285. doi: 10.1016/0022-1759(89)90104-x. [DOI] [PubMed] [Google Scholar]
- 26.Boivin B., Vaniotis G., Allen B.G., Hébert T.E. G protein-coupled receptors in and on the cell nucleus: a new signaling paradigm? J. Recept. Signal Transduct. Res. 2008;28:15–28. doi: 10.1080/10799890801941889. [DOI] [PubMed] [Google Scholar]
- 27.Bora A., Annangudi S.P., Millet L.J., Rubakhin S.S., Forbes A.J., Kelleher N.L., Gillette M.U., Sweedler J.V. Neuropeptidomics of the supraoptic rat nucleus. J. Proteome Res. 2008;7:4992–5003. doi: 10.1021/pr800394e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boudaba C., Di S., Tasker J.G. Presynaptic noradrenergic regulation of glutamate inputs to hypothalamic magnocellular neurons. J. Neuroendocrinol. 2003;15:803–810. doi: 10.1046/j.1365-2826.2003.01063.x. [DOI] [PubMed] [Google Scholar]
- 29.Boudaba C., Linn D.M., Halmos K.C., Tasker J.G. Increased tonic activation of presynaptic metabotropic glutamate receptors in the rat supraoptic nucleus following chronic dehydration. J. Physiol. 2003;551:815–823. doi: 10.1113/jphysiol.2003.042739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brailoiu G.C., Dun S.J., Brailoiu E., Inan S., Yang J., Chang J.K., Dun N.J. Nesfatin-1: distribution and interaction with a G protein-coupled receptor in the rat brain. Endocrinology. 2007;148:5088–5094. doi: 10.1210/en.2007-0701. [DOI] [PubMed] [Google Scholar]
- 31.Brailoiu E., Dun S.L., Brailoiu G.C., Mizuo K., Sklar L.A., Oprea T.I., Prossnitz E.R., Dun N.J. Distribution and characterization of estrogen receptor G protein-coupled receptor 30 in the rat central nervous system. J. Endocrinol. 2007;193:311–321. doi: 10.1677/JOE-07-0017. [DOI] [PubMed] [Google Scholar]
- 32.Brandt S.J., Niedel J.E., Bell R.M., Young W.S. Distinct patterns of expression of different protein kinase C mRNAs in rat tissues. Cell. 1987;49:57–63. doi: 10.1016/0092-8674(87)90755-0. [DOI] [PubMed] [Google Scholar]
- 33.Brouns I., Van Nassauw L., Van Genechten J., Majewski M., Scheuermann D.W., Timmermans J.P., Adriaensen D. Triple immunofluorescence staining with antibodies raised in the same species to study the complex innervation pattern of intrapulmonary chemoreceptors. J. Histochem. Cytochem. 2002;50:575–582. doi: 10.1177/002215540205000415. [DOI] [PubMed] [Google Scholar]
- 34.Brown C.H., Bourque C.W. Autocrine feedback inhibition of plateau potentials terminates phasic bursts in magnocellular neurosecretory cells of the rat supraoptic nucleus. J. Physiol. 2004;557:949–960. doi: 10.1113/jphysiol.2004.063818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brown C.H., Ludwig M., Leng G. Temporal dissociation of the feedback effects of dendritically co-released peptides on rhythmogenesis in vasopressin cells. Neuroscience. 2004;124:105–111. doi: 10.1016/j.neuroscience.2003.11.038. [DOI] [PubMed] [Google Scholar]
- 36.Brown C.H., Scott V., Ludwig M., Leng G., Bourque C.W. Somatodendritic dynorphin release: orchestrating activity patterns of vasopressin release. Biochem. Soc. Trans. 2007;35:1236–1242. doi: 10.1042/BST0351236. [DOI] [PubMed] [Google Scholar]
- 37.Brunton P.J., Arunachalam S., Russel J.A. Control of neurohypophysial hormone secretion, blood osmolality and volume in pregnancy. J. Physiol. Pharmacol. 2008;59:27–45. [PubMed] [Google Scholar]
- 38.Brunton P.J., Russell J.A., Douglas A.J. Adaptive responses of the maternal hypothalamic–pituitary–adrenal axis during pregnancy and lactation. J. Neuroendocrinol. 2008;20:764–776. doi: 10.1111/j.1365-2826.2008.01735.x. [DOI] [PubMed] [Google Scholar]
- 39.Bundzikova J., Pirnik Z., Zelena D., Mikkelsen J.D., Kiss A. Response of substances co-expressed in hypothalamic magnocellular neurons to osmotic challenges in normal and Brattleboro rats. Cell Mol. Neurobiol. 2008;28:1033–1047. doi: 10.1007/s10571-008-9306-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buongiorno-Nardelli M., Amaldi F. Autoradiographic detection of molecular hybrids between RNA and DNA in tissue sections. Nature. 1970;225:946–948. doi: 10.1038/225946a0. [DOI] [PubMed] [Google Scholar]
- 41.Burazin T.C.D., Larm J.A., Gundlach A.L. Regulation by osmotic stimuli of galanin-R1 receptor expression in magnocellular neurones of the paraventricular and supraoptic nuclei of the rat. J. Neuroendocrinol. 2001;13:358–370. doi: 10.1046/j.1365-2826.2001.00640.x. [DOI] [PubMed] [Google Scholar]
- 42.Burbach J.P., Luckman S.M., Murphy D., Gainer H. Gene regulation in the magnocellular hypothalamo-neurohypophysial system. Physiol. Rev. 2001;81:1197–1267. doi: 10.1152/physrev.2001.81.3.1197. [DOI] [PubMed] [Google Scholar]
- 43.Calebiro D., Nikolaev V.O., Persani L., Lohse M.J. Signaling by internalized G-protein-coupled receptors. Trends Pharmacol. Sci. 2010;31:221–228. doi: 10.1016/j.tips.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 44.Callewaere C., Banisadr G., Desarménien M.G., Mechighel P., Kitabgi P., Rostène W.H., Mélik Parsadaniantz S. The chemokine SDF-1/CXCL12 modulates the firing pattern of vasopressin neurons and counteracts induced vasopressin release through CXCR4. Proc. Natl. Acad. Sci. USA. 2006;103:8221–8226. doi: 10.1073/pnas.0602620103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Castelli M.P., Piras A.P., Melis T., Succu S., Sanna F., Melis M.R., Collu S., Ennas M.G., Diaz G., Mackie K., Argiolas A. Cannabinoid CB1 receptors in the paraventricular nucleus and central control of penile erection: immunocytochemistry, autoradiography and behavioural studies. Neuroscience. 2007;147:197–206. doi: 10.1016/j.neuroscience.2007.02.062. [DOI] [PubMed] [Google Scholar]
- 46.Cavanaugh A., McKenna J., Stepanchick A., Breitwieser G.E. Calcium-sensing receptor biosynthesis includes a cotranslational conformational checkpoint and endoplasmic reticulum retention. J. Biol. Chem. 2010;285:19854–19864. doi: 10.1074/jbc.M110.124792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ceccatelli S., Eriksson M., Hökfelt T. Distribution and coexistence of corticotropin-releasing factor-, neurotensin-, enkephalin-, cholecystokinin-, galanin- and vasoactive intestinal polypeptide/peptide histidine isoleucine-like peptides in the parvocellular part of the paraventricular nucleus. Neuroendocrinology. 1989;49:309–323. doi: 10.1159/000125133. [DOI] [PubMed] [Google Scholar]
- 48.Charmandari E., Tsigos C., Chrousos G. Endocrinology of the stress response. Annu. Rev. Physiol. 2005;67:259–284. doi: 10.1146/annurev.physiol.67.040403.120816. [DOI] [PubMed] [Google Scholar]
- 49.Chen Q., Li D.P., Pan H.L. Presynaptic α1 adrenergic receptors differentially regulate synaptic glutamate and GABA release to hypothalamic presympathetic neurons. J. Pharmacol. Exp. Therap. 2006;316:733–742. doi: 10.1124/jpet.105.094797. [DOI] [PubMed] [Google Scholar]
- 50.Chen X.Q., Du J.Z., Wang Y.S. Regulation of hypoxia-induced release of corticotropin-releasing factor in the rat hypothalamus by norepinephrine. Regul. Pept. 2004;119:221–228. doi: 10.1016/j.regpep.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 51.Cheng S.B., Graeber C.T., Quinn J.A., Filardo E.J. Retrograde transport of the transmembrane estrogen receptorm, G-protein-coupled-receptor-30 (GPR30/GPER) from the plasma membrane towards the nucleus. Steroids. 2011;76:892–896. doi: 10.1016/j.steroids.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 52.Cherezov V., Rosenbaum D.M., Hanson M.A., Rasmussen S.G., Thian F.S., Kobilka T.S., Choi H.J., Kuhn P., Weis W.I., Kobilka B.K., Stevens R.C. High-resolution crystal structure of an engineered human beta2-adrenergic G protein-coupled receptor. Science. 2007;318:1258–1265. doi: 10.1126/science.1150577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chini B., Parenti M. G-protein-coupled receptors, cholesterol and palmitoylation: facts about fats. J. Mol. Endocrinol. 2009;42:371–379. doi: 10.1677/JME-08-0114. [DOI] [PubMed] [Google Scholar]
- 54.Chung K.Y., Shia J., Kemeny N.E., Shah M., Schwartz G.K., Tse A., Hamilton A., Pan D., Schrag D., Schwartz L., Klimstra D.S., Fridman D., Kelsen D.P., Saltz L.B. Cetuximab shows activity in colorectal cancer patients with tumors that do not express the epidermal growth factor receptor by immunohistochemistry. J. Clin. Oncol. 2005;23:1803–1810. doi: 10.1200/JCO.2005.08.037. [DOI] [PubMed] [Google Scholar]
- 55.Ciruela F., Casadó V., Rodrigues R.J., Luján R., Burgueño J., Canals M., Borycz J., Rebola N., Goldberg S.R., Mallol J., Cortés A., Canela E.I., López-Giménez J.F., Milligan G., Lluis C., Cunha R.A., Ferré S., Franco R. Presynaptic control of striatal glutamatergic neurotransmission by adenosine A1–A2A receptor heteromers. J. Neurosci. 2006;26:2080–2087. doi: 10.1523/JNEUROSCI.3574-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Conaglen J.V., Donald R.A., Espiner E.A., Livesey J.H., Nicholls M.G. Effect of naloxone on the hormone response to CRF in normal man. Endocr. Res. 1985;11:39–44. doi: 10.3109/07435808509035423. [DOI] [PubMed] [Google Scholar]
- 57.Coon S.L., McCune S.K., Sugden D., Klein D.C. Regulation of pineal alpha1B-adrenergic receptor mRNA: day/night rhythm and beta-adrenergic receptor/cyclic AMP control. Mol. Pharmacol. 1997;51:551–557. doi: 10.1124/mol.51.4.551. [DOI] [PubMed] [Google Scholar]
- 58.Coppola J.D., Horwitz B.A., Hamilton J., McDonald R.B. Expression of NPY Y1 and Y5 receptors in the hypothalamic paraventricular nucleus of aged Fischer 344 rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004;287:69–75. doi: 10.1152/ajpregu.00607.2003. [DOI] [PubMed] [Google Scholar]
- 59.Costanzi S., Siegel J., Tikhonova I.G., Jacobson K.A. Rhodopsin and the others: a historical perspective on structural studies of G protein-coupled receptors. Curr. Pharm. Des. 2009;15:3994–4002. doi: 10.2174/138161209789824795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cotecchia S. The α1-adrenergic receptors: diversity of signaling networks and regulation. J. Recept. Signal Transduct. Res. 2010;30:410–419. doi: 10.3109/10799893.2010.518152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Crane J.W., Shimizu K., Carrasco G.A., Garcia F., Jia C., Sullivan N.R., D’Souza D.N., Zhang Y., Van de Kar L.D., Muma N.A., Battaglia G. 5-HT1A receptors mediate (+)8-OH-DPAT-stimulation of extracellular signal-regulated kinase (MAP kinase) in vivo in rat hypothalamus: time dependence and regional differences. Brain Res. 2007;1183:51–59. doi: 10.1016/j.brainres.2007.07.101. [DOI] [PubMed] [Google Scholar]
- 62.Cuatrecasas P., Hollenberg M.D. Binding of insulin and other hormones to non-receptor materials: saturability, specificity and apparent “negative cooperativity”. Biochem. Biophys. Res. Commun. 1975;62:31–41. doi: 10.1016/s0006-291x(75)80401-3. [DOI] [PubMed] [Google Scholar]
- 63.Cunningham E.T., Sawchenko P.E. Reflex control of magnocellular vasopressin and oxytocin secretion. Trends Neurosci. 1991;14:406–411. doi: 10.1016/0166-2236(91)90032-p. [DOI] [PubMed] [Google Scholar]
- 64.Daly C.J., McGrath J.C. Fluorescent ligands, antibodies, and proteins for the study of receptors. Pharmacol. Ther. 2003;100:101–118. doi: 10.1016/j.pharmthera.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 65.Day H.E., Campeau S., Watson S.J., Akil H. Expression of alpha(1b) adrenoceptor mRNA in corticotropin-releasing hormone-containing cells of the rat hypothalamus and its regulation by corticosterone. J. Neurosci. 1999;19:10098–10106. doi: 10.1523/JNEUROSCI.19-22-10098.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dayanithi G., Sabatier N., Widmer H. Intracellular calcium signalling in magnocellular neurones of the rat supraoptic nucleus: understanding the autoregulatory mechanisms. Exp. Physiol. 2000;85:75–84. doi: 10.1111/j.1469-445x.2000.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 67.Defagot M.C., Malchiodi E.L., Villar M.J., Antonelli M.C. Distribution of D4 dopamine receptor in rat brain with sequence-specific antibodies. Brain Res. Mol. Brain Res. 1997;45:1–12. doi: 10.1016/s0169-328x(96)00235-5. [DOI] [PubMed] [Google Scholar]
- 68.Di S., Boudaba C., Popescu I.R., Weng F.J., Harris C., Marcheselli V.L., Bazan N.G., Tasker J.G. Activity-dependent release and actions of endocannabinoids in the rat hypothalamic supraoptic nucleus. J. Physiol. 2005;569:751–760. doi: 10.1113/jphysiol.2005.097477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dixon R.A., Kobilka B.K., Strader D.J., Benovic J.L., Dohlman H.G., Frielle T., Bolanowski M.A., Bennett C.D., Rands E., Diehl R.E., Mumford R.A., Slater E.E., Sigal I.S., Caron M.G., Lefkowitz R.J., Strader C.D. Cloning of the gene and cDNA for mammalian beta-adrenergic receptor and homology with rhodopsin. Nature. 1986;321:75–79. doi: 10.1038/321075a0. [DOI] [PubMed] [Google Scholar]
- 70.Downes G.B., Gautam N. The G protein subunit gene families. Genomics. 1999;62:544–552. doi: 10.1006/geno.1999.5992. [DOI] [PubMed] [Google Scholar]
- 71.Drake M.T., Shenoy S.K., Lefkowitz R.J. Trafficking of G protein-coupled receptors. Circ. Res. 2006;99:570–582. doi: 10.1161/01.RES.0000242563.47507.ce. [DOI] [PubMed] [Google Scholar]
- 72.Dunn A.J., Swiergiel A.H., Palamarchouk V. Brain circuits involved in corticotropin-releasing factor-norepinephrine interactions during stress. Ann. NY Acad. Sci. 2004;1018:25–34. doi: 10.1196/annals.1296.003. [DOI] [PubMed] [Google Scholar]
- 73.Eberwine J., Bartfai T. Single cell transcriptomics of hypothalamic warm sensitive neurons that control core body temperature and fever response Signaling asymmetry and an extension of chemical neuroanatomy. Pharmacol. Ther. 2011;129:241–259. doi: 10.1016/j.pharmthera.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Elliott E., Ezra-Nevo G., Regev L., Neufeld-Cohen A., Chen A. Resilience to social stress coincides with functional DNA methylation of the Crf gene in adult mice. Nat. Neurosci. 2010;13:1351–1353. doi: 10.1038/nn.2642. [DOI] [PubMed] [Google Scholar]
- 75.Engelmann M., Landgraf R., Wotjak C.T. The hypothalamic-neurohypophysial system regulates the hypothalamic–pituitary–adrenal axis under stress: an old concept revisited. Front. Neuroendocrinol. 2004;25:132–149. doi: 10.1016/j.yfrne.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 76.Engelmann M., Ludwig M. The activity of the hypothalamo-neurohypophysial system in response to acute stressor exposure: neuroendocrine and electrophysiological observations. Stress. 2004;7:91–96. doi: 10.1080/10253890410001677240. [DOI] [PubMed] [Google Scholar]
- 77.Fan J., Yang X., Wang W., Wood W.H., Becker K.G., Gorospe M. Global analysis of stress-regulated mRNA turnover by using cDNA arrays. Proc. Natl. Acad. Sci. USA. 2002;99:10611–10616. doi: 10.1073/pnas.162212399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fedelli A., Braconi S., Economidou D., Cannella N., Kallupi M., Guerrini R., Calo C., Massi M., Ciccocioppo R. The paraventricular nucleus of the hypothalamus is a neuroanatomical substrate for the inhibition of palatable food intake by neuropeptide S. Eur. J. Neurosci. 2009;30:1594–1602. doi: 10.1111/j.1460-9568.2009.06948.x. [DOI] [PubMed] [Google Scholar]
- 79.Fekete C., Kelly J., Mihaly E., Sarkar S., Rand W.M., Legradi G., Emerson C.H., Lechan R.M. Neuropeptide Y has a central inhibitory action on the hypothalamic–pituitary–thyroid axis. Endocrinology. 2001;142:2602–2613. doi: 10.1210/endo.142.6.8207. [DOI] [PubMed] [Google Scholar]
- 80.Fekete C., Sarkar S., Rand W.M., Harney J.W., Emerson C.H., Bianco A.C., Beck-Sickinger A., Lechan R.M. Neuropeptide Y1 and Y5 receptors mediate the effects of neuropeptide Y on the hypothalamic–pituitary–thyroid axis. Endocrinology. 2002;143:4513–4519. doi: 10.1210/en.2002-220574. [DOI] [PubMed] [Google Scholar]
- 81.Feng Y.H., Ding Y., Ren S., Zhou L., Xu C., Karnik S.S. Unconventional homologous internalization of the angiotensin II type-1 receptor induced by G-protein-independent signals. Hypertension. 2005;46:419–425. doi: 10.1161/01.HYP.0000172621.68061.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ferguson A.V. Angiotensinergic regulation of autonomic and neuroendocrine outputs: critical roles for the subfornical organ and paraventricular nucleus. Neuroendocrinology. 2009;89:370–376. doi: 10.1159/000211202. [DOI] [PubMed] [Google Scholar]
- 83.Finch A.R., Sedgley K.R., Caunt C.J., McArdle C.A. Plasma membrane expression of GnRH receptors: regulation by antagonists in breast, prostate, and gonadotrope cell lines. J. Endocrinol. 2008;196:353–367. doi: 10.1677/JOE-07-0471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Flak J.N., Ostrander M.M., Tasker J.G., Herman J.P. Chronic stress-induced neurotransmitter plasticity in the PVN. J. Comp. Neurol. 2009;517:156–165. doi: 10.1002/cne.22142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Foletta V.C., Brown F.D., Young W.S. Cloning of rat ARHGAP4/C1, a RhoGAP family member expressed in the nervous system that colocalizes with the Golgi complex and microtubules. Brain Res. Mol. Brain Res. 2002;107:65–79. doi: 10.1016/s0169-328x(02)00448-5. [DOI] [PubMed] [Google Scholar]
- 86.Forsling M.L., Williams A.J. The effect of exogenous melatonin on stimulated neurohypophysial hormone release in man. Clin. Endocrinol. 2002;57:615–620. doi: 10.1046/j.1365-2265.2002.01644.x. [DOI] [PubMed] [Google Scholar]
- 87.Fox C.A., Mansour A., Thompson R.C., Bunzow J.R., Civelli O., Watson S.J. The distribution of dopamine D2 receptor heteronuclear RNA (hnRNA) in the rat brain. J. Chem. Neuroanat. 1993;6:363–373. doi: 10.1016/0891-0618(93)90011-r. [DOI] [PubMed] [Google Scholar]
- 88.Franco R. G-protein-coupled receptor heteromers or how neurons can display differently flavoured patterns in response to the same neurotransmitter. Br. J. Pharmacol. 2009;158:23–31. doi: 10.1111/j.1476-5381.2009.00181.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fritschy J.M., Meskenaite V., Weinmann O., Honer M., Benke D., Mohler H. GABAB-receptor splice variants GB1a and GB1b in rat brain: developmental regulation, cellular distribution and extrasynaptic localization. Eur. J. Neurosci. 1999;11:761–768. doi: 10.1046/j.1460-9568.1999.00481.x. [DOI] [PubMed] [Google Scholar]
- 90.Gainetdinov R.R., Premont R.T., Bohn L.M., Lefkowitz R.J., Caron M.G. Desensitization of G protein-coupled receptors and neuronal functions. Annu. Rev. Neurosci. 2004;27:107–144. doi: 10.1146/annurev.neuro.27.070203.144206. [DOI] [PubMed] [Google Scholar]
- 91.Gall J.G., Pardue M.L. Formation and detection of RNA–DNA hybrid molecules in cytological preparations. Proc. Natl. Acad. Sci. USA. 1969;63:378–383. doi: 10.1073/pnas.63.2.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ganong W.F. Circumventricular organs: definition and role in the regulation of endocrine and autonomic function. Clin. Exp. Pharmacol. Physiol. 2000;27:422–427. doi: 10.1046/j.1440-1681.2000.03259.x. [DOI] [PubMed] [Google Scholar]
- 93.García-Galiano D., Navarro V.M., Gaytan F., Tena-Sempere M. Expanding roles of NUCB2/nesfatin-1 in neuroendocrine regulation. J. Mol. Endocrinol. 2010;45:281–290. doi: 10.1677/JME-10-0059. [DOI] [PubMed] [Google Scholar]
- 94.Garza J.C., Kim C.S., Liu J., Zhang W., Lu X.Y. Adeno-associated virus-mediated knockdown of melanocortin-4 receptor in the paraventricular nucleus of the hypothalamus promotes high-fat diet-induced hyperphagia and obesity. J. Endocrinol. 2008;197:471–482. doi: 10.1677/JOE-08-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gearing K.L., Barnes A., Barnett J., Brown A., Cousens D., Dowell S., Green A., Patel K., Thomas P., Volpe F., Marshall F. Complex chimeras to map ligand binding sites of GPCRs. Protein Eng. 2003;16:365–372. doi: 10.1093/protein/gzg045. [DOI] [PubMed] [Google Scholar]
- 96.Ghamari-Langroudi M., Srisai D., Cone R.D. Multinodal regulation of the arcuate/paraventricular nucleus circuit by leptin. Proc. Natl. Acad. Sci. USA. 2011;108:355–360. doi: 10.1073/pnas.1016785108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ghate A., Befort K., Becker J.A., Filliol D., Bole-Feysot C., Demebele D., Jost B., Koch M., Kieffer B.L. Identification of novel striatal genes by expression profiling in adult mouse brain. Neuroscience. 2007;146:1182–1192. doi: 10.1016/j.neuroscience.2007.02.040. [DOI] [PubMed] [Google Scholar]
- 98.Gimpl G., Fahrenholz F. The oxytocin receptor system: structure, function, and regulation. Physiol. Rev. 2001;81:629–683. doi: 10.1152/physrev.2001.81.2.629. [DOI] [PubMed] [Google Scholar]
- 99.Gloriam D.E., Fredriksson R., Schiöth H.B. The G protein-coupled receptor subset of the rat genome. BMC Genom. 2007;8:338. doi: 10.1186/1471-2164-8-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Goke R., Larsen P.J., Mikkelsen J.D., Sheikh S.P. Distribution of GLP-1 binding sites in the rat brain: evidence that exendin-4 is a ligand of brain GLP-1 binding sites. Eur. J. Neurosci. 1995;7:2294–2300. doi: 10.1111/j.1460-9568.1995.tb00650.x. [DOI] [PubMed] [Google Scholar]
- 101.Gold S.J., Ni Y.G., Dohlman H.G., Nestler E.J. Regulators of G-protein signaling (RGS) proteins: region-specific expression of nine subtypes in rat brain. J. Neurosci. 1997;17:8024–8037. doi: 10.1523/JNEUROSCI.17-20-08024.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Goncharuk V., Zeng Z., Wang R., MacTavish D., Jhamandas J.H. Distribution of the neuropeptide FF1 receptor (hFF1) in the human hypothalamus and surrounding basal forebrain structures: immunohistochemical study. J. Comp. Neurol. 2004;474:487–503. doi: 10.1002/cne.20132. [DOI] [PubMed] [Google Scholar]
- 103.Gouarderes C., Quelven I., Mollereau C., Mazarguil H., Rice S.Q., Zajac J.M. Quantitative autoradiographic distribution of NPFF1 neuropeptide FF receptor in the rat brain and comparison with NPFF2 receptor by using [125I]YVP and [125I]EYF as selective radioligands. Neuroscience. 2002;115:349–361. doi: 10.1016/s0306-4522(02)00419-0. [DOI] [PubMed] [Google Scholar]
- 104.Gouzénes L., Sabatier N., Richard P., Moos F.C., Dayanithi G. V1a- and V2-type vasopressin receptors mediate vasopressin-induced Ca2+ responses in isolated rat supraoptic neurones. J. Physiol. 1999;517:771–779. doi: 10.1111/j.1469-7793.1999.0771s.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Grimsey N.L., Goodfellow C.E., Scotter E.L., Dowie M.J., Glass M., Graham E.S. Specific detection of CB1 receptors; cannabinoid CB1 receptor antibodies are not all created equal! J. Neurosci. Methods. 2008;171:78–86. doi: 10.1016/j.jneumeth.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 106.Grove K.L., Allen S., Grayson B.E., Smith M.S. Postnatal development of the hypothalamic neuropeptide Y system. Neuroscience. 2003;116:393–406. doi: 10.1016/s0306-4522(02)00668-1. [DOI] [PubMed] [Google Scholar]
- 107.Guastella A.J., Kenyon A.R., Alvares G.A., Carson D.S., Hickie IB I.B. Intranasal Arginine Vasopressin Enhances the Encoding of Happy and Angry Faces in Humans. Biol. Psychiat. 2010;67:1220–1222. doi: 10.1016/j.biopsych.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 108.Gurevich E.V., Joyce J.N. Distribution of dopamine D3 receptor expressing neurons in the human forebrain: comparison with D2 receptor expressing neurons. Neuropsychopharmacology. 1999;20:60–80. doi: 10.1016/S0893-133X(98)00066-9. [DOI] [PubMed] [Google Scholar]
- 109.Hadcock J.R., Wang H.Y., Malbon C.C. Agonist-induced destabilization of beta-adrenergic receptor mRNA. Attenuation of glucocorticoid-induced up-regulation of beta-adrenergic receptors. J. Biol. Chem. 1989;264:19928–19933. [PubMed] [Google Scholar]
- 110.Haley G.E., Flynn F.W. Agonist and hypertonic saline-induced trafficking of the NK3-receptors on vasopressin neurons within the paraventricular nucleus of the hypothalamus. Am. J. Physiol. Integr. Comp. Physiol. 2006;290:1242–1250. doi: 10.1152/ajpregu.00773.2005. [DOI] [PubMed] [Google Scholar]
- 111.Harmar A.J., Hills R.A., Rosser E.M., Jones M., Buneman O.P., Dunbar D.R., Greenhill S.D., Hale V.A., Sharman J.L., Bonner T.I., Catterall W.A., Davenport A.P., Delagrange P., Dollery C.T., Foord S.M., Gutman G.A., Laudet V., Neubig R.R., Ohlstein E.H., Olsen R.W., Peters J., Pin J.P., Ruffolo R.R., Searls D.B., Wright M.W., Spedding M. IUPHAR-DB: the IUPHAR database of G protein-coupled receptors and ion channels. Nucl. Acids Res. 2009;37:680–685. doi: 10.1093/nar/gkn728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Harrison C., Traynor J.R. The [35S]GTPγS binding assay: approaches and applications in pharmacology. Life Sci. 2003;74:489–508. doi: 10.1016/j.lfs.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 113.Hatae N., Aksentijevich N., Zemkova H.W., Kretschmannova K., Tomic M., Stojilkovic S.S. Cloning and functional identification of novel endothelin receptor type A isoforms in pituitary. Mol. Endocrinol. 2007;21:1192–1204. doi: 10.1210/me.2006-0343. [DOI] [PubMed] [Google Scholar]
- 114.Hatton G.I. Emerging concepts of structure–function dynamics in adult brain: the hypothalamo-neurohypophysial system. Prog. Neurobiol. 1990;34:437–504. doi: 10.1016/0301-0082(90)90017-b. [DOI] [PubMed] [Google Scholar]
- 115.Hatton G.I. Glial–neuronal interactions in the mammalian brain. Adv. Physiol. Educ. 2002;26:225–237. doi: 10.1152/advan.00038.2002. [DOI] [PubMed] [Google Scholar]
- 116.Hazell G.G., Yao S.T., Roper J.A., Prossnitz E.R., O’Carroll A-M., Lolait S.J. Localisation of GPR30, a novel G protein-coupled oestrogen receptor, suggests multiple functions in rodent brain and peripheral tissues. J. Endocrinol. 2009;202:223–236. doi: 10.1677/JOE-09-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Heinrichs S.C., Menzaghi F., Pich E.M., Hauger R.L., Koob G.F. Corticotropin-releasing factor in the paraventricular nucleus modulates feeding induced by neuropeptide Y. Brain Res. 1993;611:18–24. doi: 10.1016/0006-8993(93)91771-j. [DOI] [PubMed] [Google Scholar]
- 118.Heisler L.K., Pronchuk N., Nonogaki K., Zhou L., Raber J., Tung L., Yeo G.S., O’Rahilly S., Colmers W.F., Elmquist J.K., Tecott L.H. Serotonin activates the hypothalamic–pituitary–adrenal axis via serotonin 2C receptor stimulation. J. Neurosci. 2007;27:6956–6964. doi: 10.1523/JNEUROSCI.2584-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Herkenham M. Mismatches between neurotransmitter and receptor localizations in brain: observations and implications. Neuroscience. 1987;23:1–38. doi: 10.1016/0306-4522(87)90268-5. [DOI] [PubMed] [Google Scholar]
- 120.Herman J.P., Schäfer M.K., Watson S.J., Sherman T.G. In situ hybridization analysis of arginine vasopressin gene transcription using intron-specific probes. Mol. Endocrinol. 1991;5:1447–1456. doi: 10.1210/mend-5-10-1447. [DOI] [PubMed] [Google Scholar]
- 121.Hesketh S.A., Brennan A.K., Jessop D.S., Finn D.P. Effects of chronic treatment with citalopram on cannabinoid and opioid receptor-mediated G-protein coupling in discrete rat brain regions. Psychopharmacology. 2008;198:29–36. doi: 10.1007/s00213-007-1033-3. [DOI] [PubMed] [Google Scholar]
- 122.Hindmarch C., Fry, Smith P.M., Yao S.T., Hazell G.G., Lolait S.J., Paton J.F., Ferguson A.V., Murphy D. The transcriptome of the medullary area postrema: the thirsty rat the hungry rat and the hypertensive rat. Exp. Physiol. 2011;96:495–504. doi: 10.1113/expphysiol.2010.056515. [DOI] [PubMed] [Google Scholar]
- 123.Hindmarch C., Fry M., Yao S.T., Smith P.M., Murphy D., Ferguson A.V. Microarray analysis of the transcriptome of the subfornical organ in the rat: regulation by fluid and food deprivation. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008;295:1914–1920. doi: 10.1152/ajpregu.90560.2008. [DOI] [PubMed] [Google Scholar]
- 124.Hindmarch C., Yao S., Beighton G., Paton J., Murphy D. A comprehensive description of the transcriptome of the hypothalamoneurohypophyseal system in euhydrated and dehydrated rats. Proc. Natl. Acad. Sci. USA. 2006;103:1609–1614. doi: 10.1073/pnas.0507450103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hinks G.L., Poat J.A., Hughes J. Changes in hypothalamic cholecystokinin A and cholecysotkinin B receptor subtypes and associated neuropeptide expression in response to salt-stress in the rat and mouse. Neuroscience. 1995;68:765–781. doi: 10.1016/0306-4522(95)00148-c. [DOI] [PubMed] [Google Scholar]
- 126.Ho M.K., Su Y., Yeung W.W., Wong Y.H. Regulation of transcription factors by heterotrimeric G proteins. Curr. Mol. Pharmacol. 2009;2:19–31. doi: 10.2174/1874467210902010019. [DOI] [PubMed] [Google Scholar]
- 127.Hoffman G.E., Smith M.S., Verbalis J.G. C-Fos and related immediate early gene products as markers of activity in neuroendocrine systems. Front. Neuroendocrinol. 1993;14:173–213. doi: 10.1006/frne.1993.1006. [DOI] [PubMed] [Google Scholar]
- 128.Hofmann K.P., Scheerer P., Hildebrand P.W., Choe H.W., Park J.H., Heck M., Ernst O.P. A G protein-coupled receptor at work: the rhodopsin model. Trends Biochem. Sci. 2009;34:540–552. doi: 10.1016/j.tibs.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 129.Holst B., Holliday N.D., Bach A., Elling C.E., Cox H.M., Schwartz T.W. Common structural basis for constitutive activity of the ghrelin receptor family. J. Biol. Chem. 2004;279:53806–53817. doi: 10.1074/jbc.M407676200. [DOI] [PubMed] [Google Scholar]
- 130.Hopkins A.L., Groom C.R. The druggable genome. Nat. Rev. Drug Discov. 2002;1:727–730. doi: 10.1038/nrd892. [DOI] [PubMed] [Google Scholar]
- 131.Howe H.E., Somponpon S.J., Sladek C.D. Role of neurokinin 3 receptors in supraoptic vasopressin and oxytocin neurons. J. Neurosci. 2004;24:10103–10110. doi: 10.1523/JNEUROSCI.3164-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Hurbin A., Boissin-Agasse L., Orcel H., Rabié A., Joux N., Desarménien M.G., Richard P., Moos F.C. The V1a and V1b, but not V2, vasopressin receptor genes are expressed in the supraoptic nucleus of the rat hypothalamus, and the transcripts are essentially colocalized in the vasopressinergic magnocellular neurons. Endocrinology. 1998;139:4701–4707. doi: 10.1210/endo.139.11.6320. [DOI] [PubMed] [Google Scholar]
- 133.Hurbin A., Orcel H., Alonso G., Moos F., Rabié A. The vasopressin receptors colocalize with vasopressin in the magnocellular neurons of the rat supraoptic nucleus and are modulated by water balance. Endocrinology. 2002;143:456–466. doi: 10.1210/endo.143.2.8643. [DOI] [PubMed] [Google Scholar]
- 134.Huynh J., Thomas W.G., Aguilar M.I., Pattenden L.K. Role of helix 8 in G protein-coupled receptors based on structure–function studies on the type 1 angiotensin receptor. Mol. Cell. Endocrinol. 2009;302:118–127. doi: 10.1016/j.mce.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 135.Hwang C.K., Song K.Y., Kim C.S., Choi H.S., Guo X.H., Law P.Y., Wei L.N., Loh H.H. Evidence of endogenous μ opioid receptor regulation by epigenetic control of the promoters. Mol. Cell. Biol. 2007;27:4720–4736. doi: 10.1128/MCB.00073-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Imaki T., Katsumata H., Miyata M., Naruse M., Imaki J., Minami S. Expression of corticotropin-releasing hormone type 1 receptor in paraventricular nucleus after acute stress. Neuroendocrinology. 2001;73:293–301. doi: 10.1159/000054646. [DOI] [PubMed] [Google Scholar]
- 137.Insel P.A., Tang C.M., Hahntow I., Michel M.C. Impact of GPCRs in clinical medicine: monogenic diseases, genetic variants and drug targets. Biochim. Biophys. Acta. 2007;1768:994–1005. doi: 10.1016/j.bbamem.2006.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Irani B.G., Donato J., Olson D.P., Lowell B.B., Sacktor T.C., Reyland M.E., Tolson K.P., Zinn A.R., Ueta Y., Sakata I., Zigman J.M., Elias C.F., Clegg D.J. Distribution and neurochemical characterization of protein kinase C-theta and -delta in the rodent hypothalamus. Neuroscience. 2010;170:1065–1079. doi: 10.1016/j.neuroscience.2010.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Itoi K., Horiba N., Tozawa F., Sakai Y., Sakai K., Abe K., Demura H., Suda T. Major role of 3′, 5′-cyclic adenosine monophosphate-dependent protein kinase A pathway in corticotropin-releasing factor gene expression in the rat hypothalamus in vivo. Endocrinology. 1996;137:2389–2396. doi: 10.1210/endo.137.6.8641191. [DOI] [PubMed] [Google Scholar]
- 140.Itoi K., Jiang Y.Q., Iwasaki Y., Watson S.J. Regulatory mechanisms of corticotropin-releasing hormone and vasopressin gene expression in the hypothalamus. J. Neuroendocrinol. 2004;16:348–355. doi: 10.1111/j.0953-8194.2004.01172.x. [DOI] [PubMed] [Google Scholar]
- 141.Izzo N.J., Seidman C.E., Collins S., Colucci W.S. Alpha 1-adrenergic receptor mRNA level is regulated by norepinephrine in rabbit aortic smooth muscle cells. Proc. Natl. Acad. Sci. USA. 1990;87:6268–6271. doi: 10.1073/pnas.87.16.6268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jaakola V.P., Griffith M.T., Hanson M.A., Cherezov V., Chien E.Y., Lane J.R., Ijzerman A.P., Stevens R.C. The 2.6 angstrom crystal structure of a human A2A adenosine receptor bound to an antagonist. Science. 2008;322:1211–1217. doi: 10.1126/science.1164772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Jhamandas J.H., Raby W., Rogers J., Buijs R.M., Renaud L.P. Diagonal band projection towards the hypothalamic supraoptic nucleus: light and electron microscopic observations in the rat. J. Comp. Neurol. 1989;282:15–23. doi: 10.1002/cne.902820103. [DOI] [PubMed] [Google Scholar]
- 144.Jhanwar-Uniyal M., Roland C.R., Leibowitz SF S.F. Diurnal rhythm of alpha 2-noradrenergic receptors in the paraventricular nucleus and other brain areas: relation to circulating corticosterone and feeding behavior. Life Sci. 1986;38:473–482. doi: 10.1016/0024-3205(86)90073-1. [DOI] [PubMed] [Google Scholar]
- 145.Jjamandas J.H., MacTavish D. Central administration of neuropeptide FF causes activation of oxytocin paraventricular hypothalamic neurones that project to the brainstem. J. Neuroendocrinol. 2003;15:24–32. doi: 10.1046/j.1365-2826.2003.00869.x. [DOI] [PubMed] [Google Scholar]
- 146.Joëls M., Baram T.Z. The neuro-symphony of stress. Nat. Rev. Neurosci. 2009;10:459–466. doi: 10.1038/nrn2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.John H.A., Birnstiel M.L., Jones K.W. RNA-DNA hybrids at the cytological level. Nature. 1969;223:582–587. doi: 10.1038/223582a0. [DOI] [PubMed] [Google Scholar]
- 148.Jones P.G., Nawoschik S.P., Sreekumar K., Uveges A.J., Tseng E., Zhang L., Johnson J., He L., Paulsen J.E., Bates B., Pausch M.H. Tissue distribution and functional analyses of the constitutively active orphan G protein coupled receptors, GPR26 and GPR78. Biochim. Biophys. Acta. 2007;1170:890–901. doi: 10.1016/j.bbagen.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 149.Jositsch G., Papadakis T., Haberberger R.V., Wolff M., Wess J., Kummer W. Suitability of muscarinic acetylcholine receptor antibodies for immunohistochemistry evaluated on tissue sections of receptor gene-deficient mice. Naunyn Schmiedebergs Arch. Pharmacol. 2009;379:389–395. doi: 10.1007/s00210-008-0365-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Joun H., Lanske B., Karperien M., Qian F., Defize L., Abou-Samra A. Tissue-specific transcription start sites and alternative splicing of the parathyroid hormone (PTH)/PTH-related peptide (PTHrP) receptor gene: a new PTH/PTHrP receptor splice variant that lacks the signal peptide. Endocrinology. 1997;138:1742–1749. doi: 10.1210/endo.138.4.5085. [DOI] [PubMed] [Google Scholar]
- 151.Kalra S.P., Kalra P.S. NPY and cohorts in regulating appetite, obesity and metabolic syndrome: beneficial effects of gene therapy. Neuropeptides. 2004;38:201–211. doi: 10.1016/j.npep.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 152.Kasai R.S., Suzuki K.G., Prossnitz E.R., Koyama-Honda I., Nakada C., Fujiwara T.K., Kusumi A. Full characterization of GPCR monomer–dimer dynamic equilibrium by single molecule imaging. J. Cell. Biol. 2011;192:463–480. doi: 10.1083/jcb.201009128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kastin A.J., Akerstrom V. Nonsaturable entry of neuropeptide Y into brain. Am. J. Physiol. 1999;276:479–482. doi: 10.1152/ajpendo.1999.276.3.E479. [DOI] [PubMed] [Google Scholar]
- 154.Kastin A.J., Akerstrom V. Orexin A but not orexin B rapidly enters brain from blood by simple diffusion. J. Pharmacol. Exp. Ther. 1999;289:219–223. [PubMed] [Google Scholar]
- 155.Katayama S., Tomaru Y., Kasukawa T., Waki K., Nakanishi M., Nakamura M., Nishida H., Yap C.C., Suzuki M., Kawai J., Suzuki H., Carninci P., Hayashizaki Y., Wells C., Frith M., Ravasi T., Pang K.C., Hallinan J., Mattick J., Hume D.A., Lipovich L., Batalov S., Engström P.G., Mizuno Y., Faghihi M.A., Sandelin A., Chalk A.M., Mottagui-Tabar S., Liang Z., Lenhard B., Wahlestedt C. Antisense transcription in the mammalian transcriptome. Science. 2005;309:1564–1566. doi: 10.1126/science.1112009. [DOI] [PubMed] [Google Scholar]
- 156.Katugampola S.D., Maguire J.J., Matthewson S.R., Davenport A.P. [(125)I]-(Pyr(1))Apelin-13 is a novel radioligand for localizing the APJ orphan receptor in human and rat tissues with evidence for a vasoconstrictor role in man. Br. J. Pharmacol. 2001;132:1255–1260. doi: 10.1038/sj.bjp.0703939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kawasaki M., Ponzio T.A., Yue C., Fields R.L., Gainer H. Neurotransmitter regulation of c-fos and vasopressin gene expression in the rat supraoptic nucleus. Exp. Neurol. 2009;219:212–222. doi: 10.1016/j.expneurol.2009.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kenakin T., Miller L.J. Seven transmembrane receptors as shapeshifting proteins: the impact of allosteric modulation and functional selectivity on new drug discovery. Pharmacol. Rev. 2010;62:265–304. doi: 10.1124/pr.108.000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Khositseth S., Pisitkun T., Slentz D.H., Wang G., Hoffert J.D., Knepper M.A., Yu M.J. Quantitative protein and mRNA profiling shows selective post-transcriptional control of protein expression by vasopressin in kidney cells. Mol. Cell. Proteomics. 2011;10 doi: 10.1074/mcp.M110.004036. M110.004036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kishi T., Aschkenasi C.J., Choi B.J., Lopez M.E., Lee C.E., Liu H., Hollenberg A.N., Friedman J.M., Elmquist J.K. Neuropeptide Y Y1 receptor mRNA in rodent brain: distribution and colocalization with melanocortin-4 receptor. J. Comp. Neurol. 2005;482:217–243. doi: 10.1002/cne.20432. [DOI] [PubMed] [Google Scholar]
- 161.Kiss J., Görcs T.J., Kuhn R., Knöpfel T., Csáky A., Halász B. Distribution of metabotropic glutamate receptor 1a in the rat hypothalamus: an immunocytochemical study using monoclonal and polyclonal antibody. Acta Biol. Hung. 1996;47:221–237. [PubMed] [Google Scholar]
- 162.Kistler-Heer V., Lauber M.E., Lichtensteiger W. Different developmental patterns of melanocortin MC3 and MC4 receptor mRNA: predominance of MC4 in fetal rat nervous system. J. Neuroendocrinol. 1998;10:133–146. doi: 10.1046/j.1365-2826.1998.00180.x. [DOI] [PubMed] [Google Scholar]
- 163.Kita I., Yoshida Y., Nishino S. An activation of parvocellular oxytocinergic neurons in the paraventricular nucleus in oxytocin-induced yawning and penile erection. Neurosci. Res. 2006;54:269–275. doi: 10.1016/j.neures.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 164.Klaasse E.C., Ijzerman A.P., de Grip W.J., Beukers M.W. Internalization and desensitization of adenosine receptors. Purinergic Signal. 2008;4:21–37. doi: 10.1007/s11302-007-9086-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kocsis K., Kiss J., Görcs T., Halász B. Metabotropic glutamate receptor in vasopressin, CRF and VIP hypothalamic neurones. NeuroReport. 1998;9:4029–4033. doi: 10.1097/00001756-199812210-00008. [DOI] [PubMed] [Google Scholar]
- 166.Kohout T.A., Lefkowitz R.J. Regulation of G protein-coupled receptor kinases and arrestins during receptor desensitization. Mol. Pharmacol. 2003;63:9–18. doi: 10.1124/mol.63.1.9. [DOI] [PubMed] [Google Scholar]
- 167.Konishi S., Kasagi Y., Katsumata H., Minami S., Imaki T. Regulation of corticotropin-releasing factor (CRF) type 1 receptor gene expression by CRF in the hypothalamus. Endocr. J. 2003;50:21–36. doi: 10.1507/endocrj.50.21. [DOI] [PubMed] [Google Scholar]
- 168.Koutcherov Y., Ashwell K.W., Paxinos G. The distribution of the neurokinin B receptor in the human and rat hypothalamus. Neuroreport. 2000;11:3127–3131. doi: 10.1097/00001756-200009280-00018. [DOI] [PubMed] [Google Scholar]
- 169.J Kovács K., Sawchenko P.E. Regulation of stress-induced transcriptional changes in the hypothalamic neurosecretory neurons. J. Mol. Neurosci. 1996;7:125–133. doi: 10.1007/BF02736792. [DOI] [PubMed] [Google Scholar]
- 170.Kubo T., Fukuda K., Mikami A., Maeda A., Takahashi H., Mishina M., Haga T., Haga K., Ichiyama A., Kangawa K. Cloning, sequencing and expression of complementary DNA encoding the muscarinic acetylcholine receptor. Nature. 1986;323:411–416. doi: 10.1038/323411a0. [DOI] [PubMed] [Google Scholar]
- 171.Kyrkouli S.E., Stanley B.G., Seirafi R.D., Leibowitz S.F. Stimulation of feeding by galanin: anatomical localization and behavioral specificity of this peptide’s effects in the brain. Peptides. 1990;11:995–1001. doi: 10.1016/0196-9781(90)90023-x. [DOI] [PubMed] [Google Scholar]
- 172.Lambert R.C., Dayanithi G., Moos F.C., Richard P. A rise in the intracellular Ca2+ concentration of isolated rat supraoptic cells in response to oxytocin. J. Physiol. 1994;478:275–287. doi: 10.1113/jphysiol.1994.sp020249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Landgraf R., Neumann I.D. Vasopressin and oxytocin release within the brain: a dynamic concept of multiple and variable modes of neuropeptide communication. Front. Neuroendocrinol. 2004;25:150–176. doi: 10.1016/j.yfrne.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 174.Lang K.M., Spritz R.A. In vitro splicing pathways of pre-mRNAs containing multiple intervening sequences? Mol. Cell. Biol. 1987;7:3428–3437. doi: 10.1128/mcb.7.10.3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Larsen P.J., Tang-Christensen M., Jessop D.S. Central administration of glucagon-like peptide-1 activates hypothalamic neuroendocrine neurons in the rat. Endocrinology. 1997;138:4445–4455. doi: 10.1210/endo.138.10.5270. [DOI] [PubMed] [Google Scholar]
- 176.Latchford K.J., Ferguson A.V. ANG II-induced excitation of paraventricular nucleus magnocellular neurons: a role for glutamate interneurons. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004;286:894–902. doi: 10.1152/ajpregu.00603.2003. [DOI] [PubMed] [Google Scholar]
- 177.Lee N.H., Earle-Hughes J., Fraser C.M. Agonist-mediated destabilization of m1 muscarinic acetylcholine receptor mRNA. Elements involved in mRNA stability are localized in the 3′-untranslated region. J. Biol. Chem. 1994;269:4291–4298. [PubMed] [Google Scholar]
- 178.Lee S.Y., Kang J.S., Song G.Y., Myung C.S. Stress induces the expression of heterotrimeric G protein beta subunits and the phosphorylation of PKB/Akt and ERK1/2 in rat brain. Neurosci. Res. 2006;56:180–192. doi: 10.1016/j.neures.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 179.Lee S.P., So C.H., Rashid A.J., Varghese G., Cheng R., Lança A.J., O’Dowd B.F., George S.R. J. Biol. Chem. 2004;279:35671–35678. doi: 10.1074/jbc.M401923200. [DOI] [PubMed] [Google Scholar]
- 180.Lee T.T., Redila V.A., Hill M.N., Gorzalka B.B. 5-HT(2A) receptor mediated neuronal activation within the paraventricular nucleus of the hypothalamus is desensitized following prolonged glucocorticoid treatment. Eur. J. Pharmacol. 2009;602:54–57. doi: 10.1016/j.ejphar.2008.11.035. [DOI] [PubMed] [Google Scholar]
- 181.Lefkowitz R.J., Shenoy S.K. Transduction of receptor signals by beta-arrestins. Science. 2005;308:512–517. doi: 10.1126/science.1109237. [DOI] [PubMed] [Google Scholar]
- 182.Lein E.S., Hawrylycz M.J., Ao N., Ayres M., Bensinger A., Bernard A., Boe A.F., Boguski M.S., Brockway K.S., Byrnes E.J. Genome-wide atlas of gene expression in the adult mouse brain. Nature. 2007;445:168–176. doi: 10.1038/nature05453. [DOI] [PubMed] [Google Scholar]
- 183.Lein E.S., Zhao X., Gage F.H. Defining a molecular atlas of the hippocampus using DNA microarrays and high-throughput in situ hybridization. J. Neurosci. 2004;24:3879–3889. doi: 10.1523/JNEUROSCI.4710-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.M.D. Lemonick, D. Cray, A. Park, C.B. Thomas, D. Thompson, Brave New Pharmacy, Time magazine, US 157, January 15, 2001.
- 185.Leng G., Brown C., Sabatier N., Scott V. Population dynamics in vasopressin cells. Neuroendocrinology. 2008;88:160–172. doi: 10.1159/000149827. [DOI] [PubMed] [Google Scholar]
- 186.Lenkei Z., Palkovits M., Corvol P., Llorens-Cortes C. Distribution of angiotensin type-1 receptor messenger RNA expression in the adult rat brain. Neuroscience. 1998;82:827–841. doi: 10.1016/s0306-4522(97)00328-x. [DOI] [PubMed] [Google Scholar]
- 187.Levoye A., Dam J., Ayoub M.A., Guillaume J.L., Jockers R. Do orphan G-protein-coupled receptors have ligand-independent functions? New insights from receptor heterodimers. EMBO Rep. 2006;7:1094–1098. doi: 10.1038/sj.embor.7400838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Li D.P., Atnip L.M., Chen S.R., Pan H.L. Regulation of synaptic inputs to paraventricular-spinal output neurons by α2 adrenergic receptors. J. Neurophysiol. 2005;93:393–402. doi: 10.1152/jn.00564.2004. [DOI] [PubMed] [Google Scholar]
- 189.Li X., Fan M., Shen L., Cao Y., Zhu D., Hong Z. Excitatory responses of cardiovascular activities to urocortin3 administration into the PVN of the rat. Auton. Neurosci. 2010;154:108–111. doi: 10.1016/j.autneu.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 190.Li D.P., Pan H.L. Increased group I metabotropic glutamate receptor activity in paraventricular nucleus supports elevated sympathetic vasomotor tone in hypertension. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;299:552–561. doi: 10.1152/ajpregu.00195.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Liang J.J., Cockett M., Khawaja X.Z. Immunohistochemical localization of G protein beta1, beta2, beta3, beta4, beta5, and gamma3 subunits in the adult rat brain. J. Neurochem. 1998;71:345–355. [PubMed] [Google Scholar]
- 192.Licatalosi D.D., Darnell R.B. RNA processing and its regulation: global insights into biological networks. Nat. Rev. Genet. 2010;11:75–87. doi: 10.1038/nrg2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Lichtensteiger W., Hanimann B., Siegrist W., Eberle A.N. Region- and stage-specific patterns of melanocortin receptor ontogeny in rat central nervous system, cranial nerve ganglia and sympathetic ganglia. Brain Res. Dev. Brain Res. 1996;91:93–110. doi: 10.1016/0165-3806(95)00167-0. [DOI] [PubMed] [Google Scholar]
- 194.Lightman S.L. The neuroendocrine paraventricular hypothalamus: receptors, signal transduction, mRNA and neurosecretion. J. Exp. Biol. 1988;139:31–49. doi: 10.1242/jeb.139.1.31. [DOI] [PubMed] [Google Scholar]
- 195.Lin S.H., Leslie F.M., Civelli O. Neurochemical properties of the prolactin releasing peptide (PrRP) receptor expressing neurons: evidence for a role of PrRP as a regulator of stress and nociception. Brain Res. 2002;952:15–30. doi: 10.1016/s0006-8993(02)03183-9. [DOI] [PubMed] [Google Scholar]
- 196.Lincoln D.W., Wakerley J.B. Electrophysiological evidence for the activation of supraoptic neurones during the release of oxytocin. J. Physiol. 1974;242:533–554. doi: 10.1113/jphysiol.1974.sp010722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Little K.Y., Duncan G.E., Breese G.R., Stumpf W.E. Beta-adrenergic receptor binding in human and rat hypothalamus. Biol. Psychiat. 1992;32:512–522. doi: 10.1016/0006-3223(92)90219-p. [DOI] [PubMed] [Google Scholar]
- 198.Liu F., Wan Q., Pristupa Z.B., Yu X.M., Wang Y.T., Niznik H.B. Direct protein–protein coupling enables cross-talk between dopamine D5 and gamma-aminobutyric acid A receptors. Nature. 2000;403:274–280. doi: 10.1038/35002014. [DOI] [PubMed] [Google Scholar]
- 199.Losel R.M., Falkenstein E., Feuring M., Schultz A., Tillmann H.C., Rossol-Haseroth K., Wehling M. Nongenomic steroid action: controversies, questions, and answers. Physiol. Rev. 2003;83:965–1016. doi: 10.1152/physrev.00003.2003. [DOI] [PubMed] [Google Scholar]
- 200.Lu B., Yang X.J., Chen K., Yang D.J., Yan J.Q. Dietary sodium deprivation evokes activation of brain regional neurons and down-regulation of angiotensin II type 1 receptor and angiotensin-convertion enzyme mRNA expression. Neuroscience. 2009;164:1303–1311. doi: 10.1016/j.neuroscience.2009.08.064. [DOI] [PubMed] [Google Scholar]
- 201.Lu X.Y., Barsh G.S., Akil H., Watson S.J. Interaction between α-melanocyte-stimulating hormone and corticotropin-releasing hormone in the regulation of feeding and hypothalamo-pituitary–adrenal responses. J. Neurosci. 2003;23:7863–7872. doi: 10.1523/JNEUROSCI.23-21-07863.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Ludwig M. Dendritic release of vasopressin and oxytocin. J. Neuroendocrinol. 1998;10:881–895. doi: 10.1046/j.1365-2826.1998.00279.x. [DOI] [PubMed] [Google Scholar]
- 203.Ludwig M., Leng G. Autoinhibition of supraoptic nucleus vasopressin neurons in vivo: a combined retrodialysis/electrophysiological study in rats. Eur. J. Neurosci. 1997;9:2532–2540. doi: 10.1111/j.1460-9568.1997.tb01682.x. [DOI] [PubMed] [Google Scholar]
- 204.Ludwig M., Leng G. Dendritic peptide release and peptide-dependent behaviours. Nat. Rev. Neurosci. 2006;7:126–136. doi: 10.1038/nrn1845. [DOI] [PubMed] [Google Scholar]
- 205.Lundstrom K. Latest development in drug discovery on G protein-coupled receptors. Curr. Protein Pept. Sci. 2006;7:465–470. doi: 10.2174/138920306778559403. [DOI] [PubMed] [Google Scholar]
- 206.Luo X., Kiss A., Makara G., Lolait S.J., Aguilera G. Stress-specific regulation of corticotropin releasing hormone receptor expression in the paraventricular and supraoptic nuclei of the hypothalamus in the rat. J. Neuroendocrinol. 1994;6:689–696. doi: 10.1111/j.1365-2826.1994.tb00636.x. [DOI] [PubMed] [Google Scholar]
- 207.Luther J.A., Daftary S.S., Boudaba C., Gould G.C., Halmos K.C., Tasker J.G. Neurosecretory and non-neurosecretory parvocellular neurones of the hypothalamic paraventricular nucleus express distinct electrophysiological properties. J. Neuroendocrinol. 2002;14:929–932. doi: 10.1046/j.1365-2826.2002.00867.x. [DOI] [PubMed] [Google Scholar]
- 208.Lutz-Bucher B., Monnier D., Koch B. Evidence for the presence of receptors for pituitary adenylate cyclase-activating polypeptide in the neurohypophysis that are positively coupled to cyclic AMP formation and neurohypophyseal hormone secretion. Neuroendocrinology. 1996;64:153–161. doi: 10.1159/000127113. [DOI] [PubMed] [Google Scholar]
- 209.Ma D., Tao B., Warashina S., Kotani S., Lu L., Kaplamadzhiev D.B., Mori Y., Tonchev A.B., Yamashima T. Expression of free fatty acid receptor GPR40 in the central nervous system of adult monkeys. Neurosci. Res. 2007;58:394–401. doi: 10.1016/j.neures.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 210.Macova M., Pavel J., Saavedra J.M. A peripherally administered, centrally acting angiotensin II AT2 antagonist selectively increases brain AT1 receptors and decreases brain tyrosine hydroxylase transcription, pituitary vasopressin and ACTH. Brain Res. 2009;1250:130–140. doi: 10.1016/j.brainres.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Maejima Y., Sedbazar U., Suyama S., Kohno D., Onaka T., Takano E., Yoshida N., Koike M., Uchiyama Y., Fujiwara K., Yashiro T., Horvath T.L., Dietrich M.O., Tanaka S., Dezaki K., Oh-I S., Hashimoto K., Shimizu H., Nakata M., Mori M., Yada T. Nesfatin-1-regulated oxytocinergic signaling in the paraventricular nucleus causes anorexia through a leptin-independent melanocortin pathway. Cell Metab. 2009;10:355–365. doi: 10.1016/j.cmet.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 212.Mahan L.C., Insel P.A. Expression of beta-adrenergic receptors in synchronous and asynchronous S49 lymphoma cells. I. Receptor metabolism after irreversible blockade of receptors and in cells traversing the cell division cycle. Mol. Pharmacol. 1986;29:7–15. [PubMed] [Google Scholar]
- 213.Marion S., Weiner D.M., Caron M.G. RNA editing induces variation in desensitization and trafficking of 5-hydroxytryptamine 2c receptor isoforms. J. Biol. Chem. 2004;279:2945–2954. doi: 10.1074/jbc.M308742200. [DOI] [PubMed] [Google Scholar]
- 214.Markovic D., Challiss R.A. Alternative splicing of G protein-coupled receptors: physiology and pathophysiology. Cell. Mol. Life Sci. 2009;66:3337–3352. doi: 10.1007/s00018-009-0093-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Marroni S.S., Nakano F.N., Gati C.D.C., Oliveira J.A.C., Antunes-Rodrigues J., Garcia-Cairasco N. Neuroanatomical and cellular substrates of hypergrooming induced by microinjection of oxytocin in central nucleus of amygdala, an experimental model of compulsive behaviour. Mol. Psychiat. 2007;12:1103–1117. doi: 10.1038/sj.mp.4002015. [DOI] [PubMed] [Google Scholar]
- 216.Marshall F.H., Foord S.M. Heterodimerization of the GABAB receptor-implications for GPCR signaling and drug discovery. Adv. Pharmacol. 2010;58:63–91. doi: 10.1016/S1054-3589(10)58003-7. [DOI] [PubMed] [Google Scholar]
- 217.Matsuda L.A., Bonner T.I., Lolait S.J. Localization of cannabinoid receptor mRNA in rat brain. J. Comp. Neurol. 1993;327:535–550. doi: 10.1002/cne.903270406. [DOI] [PubMed] [Google Scholar]
- 218.Matsumoto M., Maruyama M., Noguchi J., Horikoshi Y., Fujiwara K., Kitada C., Hinuma S., Onda H., Nishimura O., Inoue K., Fujino M. Stimulation of corticotropin-releasing hormone-mediated adrenocorticotropin secretion by central administration of prolactin-releasing peptide in rats. Neurosci. Lett. 2000;285:234–238. doi: 10.1016/s0304-3940(00)01077-6. [DOI] [PubMed] [Google Scholar]
- 219.Maudsley S., Martin B., Luttrell L.M. The origins of diversity and specificity in g protein-coupled receptor signalling. J. Pharmacol. Exp. Ther. 2005;314:485–494. doi: 10.1124/jpet.105.083121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.McIntosh H.H., Song C., Howlett A.C. CB1 cannabinoid receptor: cellular regulation and distribution in N18TG2 neuroblastoma cells. Brain Res. Mol. Brain Res. 1998;53:163–173. doi: 10.1016/s0169-328x(97)00294-5. [DOI] [PubMed] [Google Scholar]
- 221.McKenzie D.N., Leng G., Dyball R.E. Electrophysiological evidence for mutual excitation of oxytocin cells in the supraoptic nucleus of the rat hypothalamus. J. Physiol. 1995;485:485–492. doi: 10.1113/jphysiol.1995.sp020744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Meister B., Broberger C., Villar M.J., Hökfelt T. Cholecystokinin B receptor gene expression in hypothalamic neurosecretory neurons after experimental manipulations. Neuroendocrinology. 1994;60:458–469. doi: 10.1159/000126782. [DOI] [PubMed] [Google Scholar]
- 223.Michael R.P. Oestrogens in the central nervous system. Br. Med. Bull. 1965;21:87–90. doi: 10.1093/oxfordjournals.bmb.a070363. [DOI] [PubMed] [Google Scholar]
- 224.Michel M.C., Wieland T., Tsujimoto G. How reliable are G-protein-coupled receptor antibodies? Naunyn Schmiedebergs Arch. Pharmacol. 2009;379:385–388. doi: 10.1007/s00210-009-0395-y. [DOI] [PubMed] [Google Scholar]
- 225.Milligan G. G protein-coupled receptor hetero-dimerization: contribution to pharmacology and function. Br. J. Pharmacol. 2009;158:5–14. doi: 10.1111/j.1476-5381.2009.00169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ming G.L., Song H.J., Berninge B., Holt C.E., Tessier-Lavigne M., Poo M.M. cAMP-dependent growth cone guidance by netrin-1. Neuron. 1997;19:1225–1235. doi: 10.1016/s0896-6273(00)80414-6. [DOI] [PubMed] [Google Scholar]
- 227.Mons N., Cooper D.M. Adenylyl cyclase mRNA expression does not reflect the predominant Ca2+/calmodulin-stimulated activity in the hypothalamus. J. Neuroendocrinol. 1994;6:665–671. doi: 10.1111/j.1365-2826.1994.tb00633.x. [DOI] [PubMed] [Google Scholar]
- 228.Moore-Morris T., Varrault A., Mangoni M.E., Le Digarcher A., Negre V., Dantec C., Journot L., Nargeot J., Couette B. Identification of potential pharmacological targets by analysis of the comprehensive G protein-coupled receptor repertoire in the four cardiac chambers. Mol. Pharmacol. 2009;75:1108–1116. doi: 10.1124/mol.108.054155. [DOI] [PubMed] [Google Scholar]
- 229.M. Mori, H. Eguchi, Screening method of nesfatin-1-action regulating substance or nesfatin-1-like action substance with the use of receptor protein selected from the group consisting of gpr3, gpr6 and gpr12. Patent USPTO#20090155833, 2009.
- 230.Morisset S., Rouleau A., Ligneau X., Gbahou F., Tardivel-Lacombe J., Stark H., Schunack W., Ganellin C.R., Schwartz J.C., Arrang J.M. High constitutive activity of native H3 receptors regulates histamine neurons in brain. Nature. 2000;408:860–864. doi: 10.1038/35048583. [DOI] [PubMed] [Google Scholar]
- 231.Morris J.F., Christian H., Ma D., Wang H. Dendritic secretion of peptides from hypothalamic magnocellular neurosecretory neurones: a local dynamic control system and its functions. Exp. Physiol. 2000;85:131–138. doi: 10.1111/j.1469-445x.2000.tb00016.x. [DOI] [PubMed] [Google Scholar]
- 232.Morris A.J., Malbon C.C. Physiological regulation of G protein-linked signalling. Physiol. Rev. 1999;79:1373–1430. doi: 10.1152/physrev.1999.79.4.1373. [DOI] [PubMed] [Google Scholar]
- 233.Murgatroyd C., Patchev A.V., Wu Y., Micale V., Bockmühl Y., Fischer D., Holsboer F., Wotjak C.T., Almeida O.F., Spengler D. Dynamic DNA methylation programs persistent adverse effects of early-life stress. Nat. Neurosci. 2009;12:1559–1566. doi: 10.1038/nn.2436. [DOI] [PubMed] [Google Scholar]
- 234.Nakamura K., Kaneko T., Yamashita Y., Hasegawa H., Katoh H., Negishi M. Immunohistochemical localization of prostaglandin EP3 receptor in the rat nervous system. J. Comp. Neurol. 2000;421:543–569. doi: 10.1002/(sici)1096-9861(20000612)421:4<543::aid-cne6>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 235.Negoescu A., Labat-Moleur F., Lorimier P., Lamarcq L., Guillermet C., Chambaz E., Brambilla E. F(ab) secondary antibodies: a general method for double immunolabeling with primary antisera from the same species. Efficiency control by chemiluminescence. J. Histochem. Cytochem. 1994;42:433–437. doi: 10.1177/42.3.7508473. [DOI] [PubMed] [Google Scholar]
- 236.Neuhaus E.M., Zhang W., Gelis L., Deng Y., Noldus J., Hatt H. Activation of an olfactory receptor inhibits proliferation of prostate cancer cells. J. Biol. Chem. 2009;284:16218–16225. doi: 10.1074/jbc.M109.012096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Ni Y.G., Gold S.J., Iredale P.A., Terwilliger R.Z., Duman R.S., Nestler E.J. Region-specific regulation of RGS4 (regulator of G-protein-signaling protein type 4) in brain by stress and glucocorticoids: in vivo and in vitro studies. J. Neurosci. 1999;19:3674–3680. doi: 10.1523/JNEUROSCI.19-10-03674.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Nichol K.A., Morey A., Couzens M.H., Shine J., Herzog H., Cunningham A.M. Conservation of expression of neuropeptide Y5 receptor between human and rat hypothalamus and limbic regions suggests an integral role in central neuroendocrine control. J. Neurosci. 1999;19:10295–10304. doi: 10.1523/JNEUROSCI.19-23-10295.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Nijenhuis W.A., Oosterom J., Adan R.A. AgRP(83-132) acts as an inverse agonist on the human-melanocortin-4 receptor. Mol. Endocrinol. 2001;15:164–171. doi: 10.1210/mend.15.1.0578. [DOI] [PubMed] [Google Scholar]
- 240.Niswender C.M., Conn P.J. Metabotropic glutamate receptors: physiology, pharmacology, and disease. Annu. Rev. Pharmacol. Toxicol. 2010;50:295–322. doi: 10.1146/annurev.pharmtox.011008.145533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Nuyt A.M., Lenkei Z., Corvol P., Palkovits M., Llorens-Cortés C. Ontogeny of angiotensin II type 1 receptor mRNAs in fetal and neonatal rat brain. J. Comp. Neurol. 2001;440:192–203. doi: 10.1002/cne.1379. [DOI] [PubMed] [Google Scholar]
- 242.O’Carroll A.-M., Lolait S.J. Regulation of rat APJ receptor messenger ribonucleic acid expression in magnocellular neurones of the paraventricular and supraopric nuclei by osmotic stimuli. J. Neuroendocrinol. 2003;15:661–666. doi: 10.1046/j.1365-2826.2003.01044.x. [DOI] [PubMed] [Google Scholar]
- 243.O’Carroll A.-M., Selby T.L., Palkovits M., Lolait S.J. Distribution of mRNA encoding B78/apj, the rat homologue of the human APJ receptor, and its endogenous ligand apelin in brain and peripheral tissues. Biochim. Biophys. Acta. 2000;1492:72–80. doi: 10.1016/s0167-4781(00)00072-5. [DOI] [PubMed] [Google Scholar]
- 244.Oka T., Oka K., Scammell T.E., Lee C., Kelly J.F., Nantel F., Elmquist J.K., Saper C.B. Relationship of EP1–4 prostaglandin receptors with rat hypothalamic cell groups involved in lipopolysaccharide fever responses. J. Comp. Neurol. 2000;428:20–32. doi: 10.1002/1096-9861(20001204)428:1<20::aid-cne3>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 245.Oldfield B.J., Davern P.J., Giles M.E., Allen A.M., Badoer E., McKinley M.J. Efferent neural projections of angiotensin receptor (AT1) expressing neurones in the hypothalamic paraventricular nucleus of the rat. J. Neuroendocrinol. 2001;13:139–146. doi: 10.1046/j.1365-2826.2001.00597.x. [DOI] [PubMed] [Google Scholar]
- 246.Oldham W.M., Hamm H.E. Heterotrimeric G protein activation by G-protein-coupled receptors. Nat. Rev. Mol. Cell. Biol. 2008;9:60–71. doi: 10.1038/nrm2299. [DOI] [PubMed] [Google Scholar]
- 247.Ostrowski N.L., Young W.S., Knepper M.A., Lolait S.J. Expression of vasopressin V1a and V2 receptor messenger ribonucleic acid in the liver and kidney of embryonic, developing, and adult rats. Endocrinology. 1993:1849–1859. doi: 10.1210/endo.133.4.8404628. [DOI] [PubMed] [Google Scholar]
- 248.Palczewski K., Kumasaka T., Hori T., Behnke C.A., Motoshima H., Fox B.A., Le Trong I., Teller D.C., Okada T., Stenkamp R.E., Yamamoto M., Miyano M. Crystal structure of rhodopsin: a G protein-coupled receptor. Science. 2000;289:739–745. doi: 10.1126/science.289.5480.739. [DOI] [PubMed] [Google Scholar]
- 249.Park J.H., Scheerer P., Hofmann K.P., Choe H.W., Ernst O.P. Crystal structure of the ligand-free G-protein-coupled receptor opsin. Nature. 2008;454:183–187. doi: 10.1038/nature07063. [DOI] [PubMed] [Google Scholar]
- 250.Parker K.J., Buckmaster C.L., Schatzberg A.F., Lyons D.M. Intranasal oxytocin administration attenuates the ACTH stress response in monkeys. Psychoneuroendocrinology. 2005;30:924–929. doi: 10.1016/j.psyneuen.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 251.Parkes D., Rivest S., Lee S., Rivier C., Vale W. Corticotropin-releasing factor activates c-fos, NGFI-B, and corticotropin-releasing factor gene expression within the paraventricular nucleus of the rat hypothalamus. Mol. Endocrinol. 1993;7:1357–1367. doi: 10.1210/mend.7.10.8264665. [DOI] [PubMed] [Google Scholar]
- 252.Pazos A., Probst A., Palacios J.M. Serotonin receptors in the human brain – III. Autoradiographic mapping of serotonin-1 receptors. Neuroscience. 1987;21:97–122. doi: 10.1016/0306-4522(87)90326-5. [DOI] [PubMed] [Google Scholar]
- 253.Pertwee R.G., Howlett A.C., Abood M.E., Alexander S.P., Di Marzo V., Elphick M.R., Greasley P.J., Hansen H.S., Kunos G., Mackie K., Mechoulam R., Ross R.A. International union of basic and clinical pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB1 and CB2. Pharmacol. Rev. 2010;62:588–631. doi: 10.1124/pr.110.003004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Pierce K.L., Premont R.T., Lefkowitz R.J. Seven-transmembrane receptors. Nat. Rev. Mol. Cell. Biol. 2002;3:639–650. doi: 10.1038/nrm908. [DOI] [PubMed] [Google Scholar]
- 255.Poulain D.A., Wakerley J.B. Electrophysiology of hypothalamic magnocellular neurones secreting oxytocin and vasopressin. Neuroscience. 1982;7:773–808. doi: 10.1016/0306-4522(82)90044-6. [DOI] [PubMed] [Google Scholar]
- 256.Pradidarcheep W., Labruyère W.T., Dabhoiwala N.F., Lamers W.H. Lack of specificity of commercially available antisera: better specifications needed. J. Histochem. Cytochem. 2008;56:1099–1111. doi: 10.1369/jhc.2008.952101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Price C.J., Hoyda T.D., Samson W.K., Ferguson A.V. Nesfatin-1 influences the excitability of paraventricular nucleus neurones. J. Neuroendocrinol. 2008;20:245–250. doi: 10.1111/j.1365-2826.2007.01641.x. [DOI] [PubMed] [Google Scholar]
- 258.Price C.J., Scott R., Rusakov D.A., Capogna M. GABA(B) receptor modulation of feedforward inhibition through hippocampal neurogliaform cells. J. Neurosci. 2008;28:6974–6982. doi: 10.1523/JNEUROSCI.4673-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Pyner S. Neurochemistry of the paraventricular nucleus of the hypothalamus: implications for cardiovascular regulation. J. Chem. Neuroanat. 2009;38:197–208. doi: 10.1016/j.jchemneu.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 260.Qiu D.L., Chu C.P., Tsukino H., Shirasaka T., Nakao H., Kato K., Kunitake T., Katoh T., Kannan H. Neuromedin U receptor subtype-2 mRNA and HCN channels mRNA expression NMU-sensitive neurons in rat hypothalamic paraventricular nucleus. Neurosci. Lett. 2005;374:69–72. doi: 10.1016/j.neulet.2004.10.033. [DOI] [PubMed] [Google Scholar]
- 261.Quitterer U., AbdAlla S., Jarnagin K., Müller-Esterl W. Na+ ions binding to the bradykinin B2 receptor suppress agonist-independent receptor activation. Biochemistry. 1996;35:13368–13377. doi: 10.1021/bi961163w. [DOI] [PubMed] [Google Scholar]
- 262.Raison C.L., Miller A.H. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am. J. Psychiat. 2003;160:1554–1565. doi: 10.1176/appi.ajp.160.9.1554. [DOI] [PubMed] [Google Scholar]
- 263.Rasmussen S.G., Choi H.J., Rosenbaum D.M., Kobilka T.S., Thian F.S., Edwards P.C., Burghammer M., Ratnala V.R., Sanishvili R., Fischetti R.F., Schertler G.F., Weis W.I., Kobilka B.K. Crystal structure of the human beta2 adrenergic G-protein-coupled receptor. Nature. 2007;450:383–387. doi: 10.1038/nature06325. [DOI] [PubMed] [Google Scholar]
- 264.Re M., Pampillo M., Savard M., Dubuc C., McArdle C.A., Millar R.P., Conn P.M., Gobeil F., Bhattacharya M., Babwah A.V. The human gonadotropin releasing hormone type I receptor is a functional intracellular GPCR expressed on the nuclear membrane. PLoS One. 2010;5:11489. doi: 10.1371/journal.pone.0011489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Renaud L.P., Bourque C.W. Neurophysiology and neuropharmacology of hypothalamic magnocellular neurons secreting vasopressin and oxytocin. Prog. Neurobiol. 1991;36:131–169. doi: 10.1016/0301-0082(91)90020-2. [DOI] [PubMed] [Google Scholar]
- 266.Revankar C.M., Cimino D.F., Sklar L.A., Arterburn J.B., Prossnitz E.R. A transmembrane intracellular estrogen receptor mediates rapid cell signalling. Science. 2005;307:1625–1630. doi: 10.1126/science.1106943. [DOI] [PubMed] [Google Scholar]
- 267.Rhodes C.H., Morrell J.I., Pfaff D.W. Immunohistochemical analysis of magnocellular elements in rat hypothalamus: distribution and numbers of cells containing neurophysin, oxytocin, and vasopressin. J. Comp. Neurol. 1981;198:45–64. doi: 10.1002/cne.901980106. [DOI] [PubMed] [Google Scholar]
- 268.Richards D.S., Villalba R.M., Alvarez F.J., Stern J.E. Expression of GABAB receptors in magnocellular neurosecretory cells of male, virgin female and lactating rats. J. Neuroendocrinol. 2005;17:413–423. doi: 10.1111/j.1365-2826.2005.01324.x. [DOI] [PubMed] [Google Scholar]
- 269.Ritter S.L., Hall R.A. Fine-tuning of GPCR activity by receptor-interacting proteins. Nat. Rev. Mol. Cell. Biol. 2009;10:819–830. doi: 10.1038/nrm2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Rivkees S.A., Lachowicz J.E. Functional D1 and D5 dopamine receptors are expressed in the suprachiasmatic, supraoptic, and paraventricular nuclei of primates. Synapse. 1997;26:1–10. doi: 10.1002/(SICI)1098-2396(199705)26:1<1::AID-SYN1>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 271.Robertson A., Gonzalez A.M., Stopa E., Leadbeater W., Coimbra R., Johanson C., Eliceiri B., Baird A. Immunohistochemical evidence that Argillin, the product of the ECRG4 gene, encodes a novel neuroendocrine peptide. Soc. Endocrinol. 2009;19:OC16. (Endocrine Abstracts) [Google Scholar]
- 272.Rogers K.V., Dunn C.K., Hebert S.C., Brown E.M. Localization of calcium receptor mRNA in the adult rat central nervous system by in situ hybridization. Brain Res. 1997;744:47–56. doi: 10.1016/s0006-8993(96)01070-0. [DOI] [PubMed] [Google Scholar]
- 273.Roper J., O’Carroll A.M., Young W., Lolait S. The vasopressin Avpr1b receptor: molecular and pharmacological studies. Stress. 2011;14:98–115. doi: 10.3109/10253890.2010.512376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Rosenbaum D.M., Rasmussen S.G., Kobilka B.K. The structure and function of G-protein-coupled receptors. Nature. 2009;459:356–363. doi: 10.1038/nature08144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Rosin D.L., Robeva A., Woodward R.L., Guyenet P.G., Linden J. Immunohistochemical localization of adenosine A2A receptors in the rat central nervous system. J. Comp. Neurol. 1998;401:163–186. [PubMed] [Google Scholar]
- 276.Sabatier N., Caquineau C., Dayanithi G., Bull P., Douglas A.J., Guan X.M., Jiang M., Van der Ploeg L., Leng G. α-Melanocyte-stimulating hormone stimulates oxytocin release from the dendrites of hypothalamic neurons while inhibiting oxytocin release from their terminals in the neurohypophysis. J. Neurosci. 2003;23:10351–10358. doi: 10.1523/JNEUROSCI.23-32-10351.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Sabatier N., Leng G. Presynaptic action of endocannabinoids mediate α-MSH-induced inhibition of oxytocin cells. Am. J. Physio. Integr. Comp. Physiol. 2006;290:577–584. doi: 10.1152/ajpregu.00667.2005. [DOI] [PubMed] [Google Scholar]
- 278.Sakaue M., Hoffman B.B. Glucocorticoids induce transcription and expression of the alpha 1B adrenergic receptor gene in DTT1 MF-2 smooth muscle cells. J. Clin. Invest. 1991;88:385–389. doi: 10.1172/JCI115315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Samson W.K., Zhang J.V., Avsian-Kretchmer O., Cui K., Yosten G.L., Klein C., Lyu R.M., Wang Y.X., Chen X.Q., Yang J., J Price C., Hoyda T.D., Ferguson A.V., Yuan X.B., Chang J.K., Hsueh A.J. Neuronostatin encoded by the somatostatin gene regulates neuronal, cardiovascular, and metabolic functions. J. Biol. Chem. 2008;283:31949–31959. doi: 10.1074/jbc.M804784200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Sands S.A., Morilak D.A. Expression of alpha1D adrenergic receptor messenger RNA in oxytocin- and corticotropin-releasing hormone-synthesizing neurons in the rat paraventricular nucleus. Neuroscience. 1999;91:639–649. doi: 10.1016/s0306-4522(98)00616-2. [DOI] [PubMed] [Google Scholar]
- 281.Sato K., Numata T., Saito T., Ueta Y., Okada Y. V2 receptor-mediated autocrine role of somatodendritic release of AVP in rat vasopressin neurons under hypo-osmotic conditions. Sci. Signal. 2011;4:ra5. doi: 10.1126/scisignal.2001279. [DOI] [PubMed] [Google Scholar]
- 282.Saunders C., Limbird L.E. Disruption of microtubules reveals two independent apical targeting mechanisms for G-protein-coupled receptors in polarized renal epithelial cells. J. Biol. Chem. 1997;272:19035–19045. doi: 10.1074/jbc.272.30.19035. [DOI] [PubMed] [Google Scholar]
- 283.Sawchenko P.E. Toward a new neurobiology of energy balance, appetite, and obesity: the anatomists weigh in. J. Comp. Neurol. 1998;402:435–441. [PubMed] [Google Scholar]
- 284.Schrader L.A., Tasker J.G. Presynaptic modulation by metabotropic glutamate receptors of excitatory and inhibitory synaptic inputs to hypothalamic magnocellular neurons. J. Neurophysiol. 1997;77:527–536. doi: 10.1152/jn.1997.77.2.527. [DOI] [PubMed] [Google Scholar]
- 285.Schwartz M.W., Woods S.C., Porte D., Seeley R.J., Baskin D.G. Central nervous system control of food intake. Nature. 2000;404:661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- 286.Shaw J.L., Gackenheimer S.L., Gehlert D.R. Functional autoradiography of neuropeptide Y Y1 and Y2 receptor subtypes in rat brain using agonist stimulated [35S]GTPgammaS binding. J. Chem. Neuroanat. 2003;26:179–193. doi: 10.1016/j.jchemneu.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 287.Shen B., Harrison-Bernard L.M., Fuller A.J., Vanderpool V., Saifudeen Z., El-Dahr S.S. The Bradykinin B2 receptor gene is a target of angiotensin II type 1 receptor signaling. J. Am. Soc. Nephrol. 2007;18:1140–1149. doi: 10.1681/ASN.2006101127. [DOI] [PubMed] [Google Scholar]
- 288.Shi B., Bhat G., Mahesh V.B., Brotto M., Nosek T.M., Brann D.W. Bradykinin receptor localization and cell signaling pathways used by bradykinin in the regulation of gonadotropin-releasing hormone secretion. Endocrinology. 1999;140:4669–4676. doi: 10.1210/endo.140.10.7069. [DOI] [PubMed] [Google Scholar]
- 289.Shibuya I., Noguchi J., Tanaka K., Harayama N., Inoue U., Kabashima N., Ueta Y., Hattori Y., Yamashita H. PACAP increases the cytosolic Ca2+ concentration and stimulates somatodendritic vasopressin release in rat supraoptic neurons. J. Neuroendocrinol. 1998;10:31–42. doi: 10.1046/j.1365-2826.1998.00168.x. [DOI] [PubMed] [Google Scholar]
- 290.Shibuya I., Setiadji S.V., Ibrahim N., Harayama N., Maruyama T., Ueta Y., Yamashita H. Involvement of postsynaptic EP4 and presynaptic EP3 receptors in actions of prostaglandin E2 in rat supraoptic nucleus. J. Neuroendocrinol. 2002;14:64–72. doi: 10.1046/j.1365-2826.2002.00741.x. [DOI] [PubMed] [Google Scholar]
- 291.Shrestha Y.B., Wickwire K., Giraudo S. Effect of reducing ghrelin receptor gene expression on energy balance. Peptides. 2009;30:1336–1341. doi: 10.1016/j.peptides.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Shuey D.J., Betty M., Jones P.G., Khawaja X.Z., Cockett M.I. RGS7 attenuates signal transduction through the G(alpha q) family of heterotrimeric G proteins in mammalian cells. J. Neurochem. 1998;70:1964–1972. doi: 10.1046/j.1471-4159.1998.70051964.x. [DOI] [PubMed] [Google Scholar]
- 293.Shughrue P.J., Lane M.V., Merchenthaler I. Glucagon-like peptide-1 receptor (GLP1-R) mRNA in the rat hypothalamus. Endocrinology. 1996;137:5159–5162. doi: 10.1210/endo.137.11.8895391. [DOI] [PubMed] [Google Scholar]
- 294.Siegel R.E., Young W.S. Detection of preprocholecystokinin and preproenkephalin A mRNAs in rat brain by hybridization histochemistry using complementary RNA probes. Neuropeptides. 1985;6:573–580. doi: 10.1016/0143-4179(85)90121-0. [DOI] [PubMed] [Google Scholar]
- 295.Simmons D.M., Swanson L.W. Comparison of the spatial distribution of seven types of neuroendocrine neurons in the rat paraventricular nucleus: toward a global 3D model. J. Comp. Neurol. 2009;516:423–441. doi: 10.1002/cne.22126. [DOI] [PubMed] [Google Scholar]
- 296.Simonnet G., Rodriguez F., Fumoux F., Czernichow P., Vincent J.D. Vasopressin release and drinking induced by intracranial injection of angiotensin II in monkey. Am. J. Physiol. 1979;237:20–25. doi: 10.1152/ajpregu.1979.237.1.R20. [DOI] [PubMed] [Google Scholar]
- 297.Sklar L.A., Hyslop P.A., Oades Z.G., Omann G.M., Jesaitis A.J., Painter R.G., Cochrane C.G. Signal transduction and ligand-receptor dynamics in the human neutrophil. Transient responses and occupancy-response relations at the formyl peptide receptor. J. Biol. Chem. 1985;260:11461–11467. [PubMed] [Google Scholar]
- 298.C.D. Sladek, Antidiuretic Hormone: Synthesis and Release. Handbook of Physiology, The Endocrine System, Endocrine Regulation of Water and Electrolyte Balance, American Physiological Society, 2000.
- 299.Smith M.J., Wise P.M. Localization of kappa opioid receptors in oxytocin magnocellular neurons in the paraventricular and supraoptic nuclei. Brain Res. 2001;898:162–165. doi: 10.1016/s0006-8993(01)02154-0. [DOI] [PubMed] [Google Scholar]
- 300.Sofroniew M.V. Projections from vasopressin, oxytocin, and neurophysin neurons to neural targets in the rat and human. J. Histochem. Cytochem. 1980;28:475–478. doi: 10.1177/28.5.7381192. [DOI] [PubMed] [Google Scholar]
- 301.Song Z., Gomes D.A., Stevens W., Sladek C.D. Multiple α1 adrenergic receptor subtypes support synergistic stimulation of vasopressin and oxytocin release by ATP and phenylephrine. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;299:1529–1537. doi: 10.1152/ajpregu.00532.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Song Z., Vijayaraghavan S., Sladek C.D. ATP increases intracellular calcium in supraoptic neurons by activation of both P2X and P2Y purinergic receptors. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007;292:423–431. doi: 10.1152/ajpregu.00495.2006. [DOI] [PubMed] [Google Scholar]
- 303.Sóvágó J., Dupuis D.S., Gulyás B., Hall H. An overview on functional receptor autoradiography using [35S]GTPgammaS. Brain Res. Brain Res. Rev. 2001;38:149–164. doi: 10.1016/s0165-0173(01)00106-0. [DOI] [PubMed] [Google Scholar]
- 304.Springael J.Y., Urizar E., Costagliola S., Vassart G., Parmentier M. Allosteric properties of G protein-coupled receptor oligomers. Pharmacol. Ther. 2007;115:410–418. doi: 10.1016/j.pharmthera.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 305.Stankova J., Turcotte S., Harris J., Rola-Pleszczynski M. Modulation of leukotriene B4 receptor-1 expression by dexamethasone: potential mechanism for enhanced neutrophil survival. J. Immunol. 2002;168:3570–3576. doi: 10.4049/jimmunol.168.7.3570. [DOI] [PubMed] [Google Scholar]
- 306.Stern J.E. Nitric oxide and homeostatic control: an intercellular signalling molecule contributing to autonomic and neuroendocrine integration? Prog. Biophys. Mol. Biol. 2004;84:197–215. doi: 10.1016/j.pbiomolbio.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 307.Stern J.E., Zhang W. Cellular sources, targets and actions of constitutive nitric oxide in the magnocellular neurosecretory system of the rat. J. Physiol. 2005;562:725–744. doi: 10.1113/jphysiol.2004.077735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Stewart L., Hindmarch C.C., Qiu J., Tung Y.C., Yeo G.S., Murphy D. Hypothalamic transcriptome plasticity in two rodent species reveals divergent differential gene expression but conserved pathways. J. Neuroendocrinol. 2011;23:177–185. doi: 10.1111/j.1365-2826.2010.02093.x. [DOI] [PubMed] [Google Scholar]
- 309.Storm E.E., Tecott L.H. Social circuits: peptidergic regulation of mammalian social behaviour. Neuron. 2005;47:483–486. doi: 10.1016/j.neuron.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 310.Stofkova A., Skurlova M., Kiss A., Zelezna B., Zorad S., Jurcovicova J. Activation of hypothalamic NPY, AgRP, MC4R, AND IL-6 mRNA levels in young Lewis rats with early-life diet-induced obesity. Endocr. Regul. 2009;43:99–106. [PubMed] [Google Scholar]
- 311.Stricker E.M., Sved A.F. Controls of vasopressin secretion and thirst: similarities and dissimilarities in signals. Physiol. Behav. 2002;77:731–736. doi: 10.1016/s0031-9384(02)00926-5. [DOI] [PubMed] [Google Scholar]
- 312.Succu S., Sanna F., Melis T., Boi A., Argiolas A., Melis M.R. Stimulation of dopamine receptors in the paraventricular nucleus of the hypothalamus of male rats induces penile erection and increases extra-cellular dopamine in the nucleus accumbens: involvement of central oxytocin. Neuropharmacology. 2007;52:1034–1043. doi: 10.1016/j.neuropharm.2006.10.019. [DOI] [PubMed] [Google Scholar]
- 313.Sun Y., Huang J., Xiang Y., Bastepe M., Jüppner H., Kobilka B.K., Zhang J.J., Huang X.Y. Dosage-dependent switch from G protein-coupled to G protein-independent signaling by a GPCR. EMBO J. 2007;26:53–64. doi: 10.1038/sj.emboj.7601502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Swaab D.F. The human hypothalamo-neurohypophysial system in health and disease. Prog. Brain Res. 1998;119:577–618. doi: 10.1016/s0079-6123(08)61594-0. [DOI] [PubMed] [Google Scholar]
- 315.Swaab D.F., Pool C.W., Van Leeuwen F.W. Can specificity ever be proved in immunocytochemical staining. J. Histochem. Cytochem. 1977;25:388–391. doi: 10.1177/25.5.325124. [DOI] [PubMed] [Google Scholar]
- 316.Swanson L.W., Sawchenko P.E. Hypothalamic integration: organization of the paraventricular and supraoptic nuclei. Annu. Rev. Neurosci. 1983;6:269–324. doi: 10.1146/annurev.ne.06.030183.001413. [DOI] [PubMed] [Google Scholar]
- 317.Szarek E., Cheah P.S., Schwartz J., Thomas P. Molecular genetics of the developing neuroendocrine hypothalamus. Mol. Cell. Endocrinol. 2010;323:115–123. doi: 10.1016/j.mce.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 318.Tadross J.A., Patterson M., Suzuki K., Beale K.E., Boughton C.K., Smith K.L., Moore S., Ghatei M.A., Bloom S.R. Augurin stimulates the hypothalamo-pituitary–adrenal axis via the release of corticotrophin-releasing factor in rats. Br. J. Pharmacol. 2010;159:1663–1671. doi: 10.1111/j.1476-5381.2010.00655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Takahashi A., Ishimaru H., Ikarashi Y., Kishi E., Maruyama Y. Opposite regulation of body temperature by cholinergic input to the paraventricular nucleus and supraoptic nucleus in rats. Brain Res. 2001;909:102–111. doi: 10.1016/s0006-8993(01)02642-7. [DOI] [PubMed] [Google Scholar]
- 320.Takano Y., Nakayama Y., Matsumoto T., Saito R., Kamiya H.O. The mechanism of central pressor actions of tachykinin NK-3 receptor in the paraventricular nucleus of the hypothalamus in rats. Regul. Peptides. 1993;46:360–363. doi: 10.1016/0167-0115(93)90086-n. [DOI] [PubMed] [Google Scholar]
- 321.Tanaka S., Ishii K., Kasai K., Yoon S.O., Saeki Y. Neural expression of G protein-coupled receptors GPR3, GPR6, and GPR12 up-regulates cyclic AMP levels and promotes neurite outgrowth. J. Biol. Chem. 2007;282:10506–10515. doi: 10.1074/jbc.M700911200. [DOI] [PubMed] [Google Scholar]
- 322.Tasker J.G., Di S., Boudaba C. Functional synaptic plasticity in hypothalamic magnocellular neurons. Prog. Brain Res. 2002;139:113–119. doi: 10.1016/s0079-6123(02)39011-3. [DOI] [PubMed] [Google Scholar]
- 323.Tasker J.G., Dudek F.E. Electrophysiological properties of neurones in the region of the paraventricular nucleus in slices of rat hypothalamus. J. Physiol. 1991;434:271–293. doi: 10.1113/jphysiol.1991.sp018469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Tauchi M., Zhang R., D’Alessio D.A., Stern J.E., Herman J.P. Distribution of glucagon-like peptide-1 immunoreactivity in the hypothalamic paraventricular and supraoptic nuclei. J. Chem. Neuroanat. 2008;36:144–149. doi: 10.1016/j.jchemneu.2008.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Tiao J.Y., Bradaia A., Biermann B., Kaupmann K., Metz M., Haller C., Rolink A.G., Pless E., Barlow P.N., Gassmann M., Bettler B. The sushi domains of secreted GABA(B1) isoforms selectively impair GABA(B) heteroreceptor function. J. Biol. Chem. 2008;283:31005–31011. doi: 10.1074/jbc.M804464200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Tobin A.B., Butcher A.J., Kong K.C. Location, location, location site-specific GPCR phosphorylation offers a mechanism for cell-type-specific signalling. Trends Pharmacol. Sci. 2008;29:413–420. doi: 10.1016/j.tips.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Tobin V.A., Bull P.M., Arunachalam S., O’Carroll A.-M., Ueta Y., Ludwig M. The effects of apelin on the electrical activity of hypothalamic magnocellular vasopressin and oxytocin neurons and somatodendritic peptide release. Endocrinology. 2008;149:6136–6145. doi: 10.1210/en.2008-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Toshinai K., Nakazato M. Neuroendocrine regulatory peptide-1 and -2: novel bioactive peptides processed from VGF. Cell. Mol. Life Sci. 2009;66:1939–1945. doi: 10.1007/s00018-009-8796-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Toyooka M., Tujii T., Takeda S. The N-terminal domain of GPR61, an orphan G-protein-coupled receptor, is essential for its constitutive activity. J. Neurosci. Res. 2009;87:1329–1333. doi: 10.1002/jnr.21955. [DOI] [PubMed] [Google Scholar]
- 330.Tran T.M., Friedman J., Qunaibi E., Baameur F., Moore R.H., Clark R.B. Characterization of agonist stimulation of cAMP-dependent protein kinase and G protein-coupled receptor kinase phosphorylation of the beta2-adrenergic receptor using phosphoserine-specific antibodies. Mol. Pharmacol. 2004;65:196–206. doi: 10.1124/mol.65.1.196. [DOI] [PubMed] [Google Scholar]
- 331.Ulrich-Lai Y.M., Herman J.P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 2009;10:397–409. doi: 10.1038/nrn2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Valentino R.J., Page M., Van Bockstaele E., Aston-Jones G. Corticotropin-releasing factor innervation of the locus coeruleus region: distribution of fibers and sources of input. Neuroscience. 1992;48:689–705. doi: 10.1016/0306-4522(92)90412-u. [DOI] [PubMed] [Google Scholar]
- 333.van den Burg E.H., Neumann I.D. Bridging the Gap between GPCR activation and behaviour: oxytocin and prolactin signalling in the hypothalamus. J. Mol. Neurosci. 2011;43:200–208. doi: 10.1007/s12031-010-9452-8. [DOI] [PubMed] [Google Scholar]
- 334.Vassilatis D.K., Hohmann J.G., Zeng H., Li F., Ranchalis J.E., Mortrud M.T., Brown A., Rodriguez S.S., Weller J.R., Wright A.C., Bergmann J.E., Gaitanaris G.A. The G protein-coupled receptor repertoires of human and mouse. Proc. Natl. Acad. Sci. USA. 2003;100:4903–4908. doi: 10.1073/pnas.0230374100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Veening J.G., Barendregt H.P. The regulation of brain states by neuroactive substances distributed via the cerebrospinal fluid; a review. Cerebrospinal Fluid Res. 2010;7:1–16. doi: 10.1186/1743-8454-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Wainford R.D., Kapusta D.R. Hypothalamic paraventricular nucleus G alpha q subunit protein pathways mediate vasopressin dysregulation and fluid retention in salt-sensitive rats. Endocrinology. 2010;151:5403–5414. doi: 10.1210/en.2010-0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Wakerley J.B., Poulain D.A., Brown D. Comparison of firing patterns in oxytocin- and vasopressin-releasing neurones during progressive dehydration. Brain Res. 1978;148:425–440. doi: 10.1016/0006-8993(78)90730-8. [DOI] [PubMed] [Google Scholar]
- 338.Wakerley J.B., Poulain D.A., Dyball R.E., Cross B.A. Activity of phasic neurosecretory cells during haemorrhage. Nature. 1975;258:82–84. doi: 10.1038/258082a0. [DOI] [PubMed] [Google Scholar]
- 339.Wang Z., Gerstein M., Snyder M. RNA-Seq: a revolutionary tool for transcriptomics. Nat. Rev. Genet. 2009;10:57–63. doi: 10.1038/nrg2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Wang S.S., Kamphuis W., Huitinga I., Zhou J.N., Swaab D.F. Gene expression analysis in the human hypothalamus in depression by laser microdissection and real-time PCR: the presence of multiple receptor imbalances. Mol. Psychiat. 2008;13:786–799. doi: 10.1038/mp.2008.38. [DOI] [PubMed] [Google Scholar]
- 341.Wang T., Palkovits M., Rusnak M., Mezey E., Usdin T.B. Distribution of parathyroid hormone 2 receptor-like immunoreactivity and messenger mRNA in the rat nervous system. Neuroscience. 2000;100:629–649. doi: 10.1016/s0306-4522(00)00282-7. [DOI] [PubMed] [Google Scholar]
- 342.Watson A.M., McKinley M.J., May C.N. Effect of central urotensin II on the heart rate, blood pressure and brain fos immunoreactivity in conscious rats. Neuroscience. 2008;155:241–249. doi: 10.1016/j.neuroscience.2008.05.032. [DOI] [PubMed] [Google Scholar]
- 343.Wayte J., Buckingham J.C., Cowell A.M. The role of phospholipase C in arginine vasopressin secretion by rat hypothalami in vitro. Neuroreport. 1997;8:1277–1282. doi: 10.1097/00001756-199703240-00044. [DOI] [PubMed] [Google Scholar]
- 344.Weekes M.P., Antrobus R., Lill J.R., Duncan L.M., Hör S., Lehner P.J. Comparative analysis of techniques to purify plasma membrane proteins. J. Biomol. Tech. 2010;21:108–115. [PMC free article] [PubMed] [Google Scholar]
- 345.Wei K., Eubanks J.H., Francis J., Jia Z., Snead O.C. Cloning and tissue distribution of a novel isoform of the rat GABA(B)R1 receptor subunit. Neuroreport. 2001;12:833–837. doi: 10.1097/00001756-200103260-00042. [DOI] [PubMed] [Google Scholar]
- 346.Wei S.G., Yu Y., Zhang Z.H., Felder R.B. Angiotensin II upregulates hypothalamic AT1 receptor expression in rats via the mitogen-activated protein kinase pathway. Am. J. Physiol. Heart Circ. Physiol. 2009;296:1425–1433. doi: 10.1152/ajpheart.00942.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Weil T.T., Parton R.M., Davis I. Making the message clear: visualizing mRNA localization. Trends Cell. Biol. 2010;20:380–390. doi: 10.1016/j.tcb.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.H.G. Wendelboe, K. Bisgaard, Education Guide: Immunohistochemical (IHC) Staining Methods, 5th ed., Dako North America, California, 2009.
- 349.Wess J. Mutational analysis of muscarinic acetylcholine receptors: structural basis of ligand/receptor/G protein interactions. Life Sci. 1993;53:1447–1463. doi: 10.1016/0024-3205(93)90618-d. [DOI] [PubMed] [Google Scholar]
- 350.Wheatley M., Hawtin S.R. Glycosylation of G-protein-coupled receptors for hormones central to normal reproductive functioning: its occurrence and role. Hum. Reprod. Update. 1999;4:356–364. doi: 10.1093/humupd/5.4.356. [DOI] [PubMed] [Google Scholar]
- 351.Wheatley M., Hawtin S.R., Wesley V.J., Howard H.C., Simms J., Miles A., McEwan K., Parslow R.A. Agonist binding to peptide hormone receptors. Biochem. Soc. Trans. 2003;31:35–39. doi: 10.1042/bst0310035. [DOI] [PubMed] [Google Scholar]
- 352.Whitnall M.H. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog. Neurobiol. 1993;40:573–629. doi: 10.1016/0301-0082(93)90035-q. [DOI] [PubMed] [Google Scholar]
- 353.Wilson M.H., Limbird L.E. Mechanisms regulating the cell surface residence time of the alpha 2A-adrenergic receptor. Biochemistry. 2000;39:693–700. doi: 10.1021/bi9920275. [DOI] [PubMed] [Google Scholar]
- 354.Windle R.J., Gamble L.E., Kershaw Y.M., Wood S.A., Lightman S.L., Ingram C.D. Gonadal steroid modulation of stress-induced hypothalamo-pituitary–adrenal activity and anxiety behavior: role of central oxytocin. Endocrinology. 2006;147:2423–2431. doi: 10.1210/en.2005-1079. [DOI] [PubMed] [Google Scholar]
- 355.Woehler A., Ponimaskin E.G. G protein-mediated signaling: same receptor, multiple effectors. Curr. Mol. Pharmacol. 2009;2:237–248. doi: 10.2174/1874467210902030237. [DOI] [PubMed] [Google Scholar]
- 356.Wong L.F., Harding T., Uney J., Murphy D. cAMP-dependent protein kinase A mediation of vasopressin gene expression in the hypothalamus of the osmotically challenged rat. Mol. Cell. Neurosci. 2003;24:82–90. doi: 10.1016/s1044-7431(03)00123-4. [DOI] [PubMed] [Google Scholar]
- 357.Wren A.M., Small C.J., Abbott C.R., Jethwa P.H., Kennedy A.R., Murphy K.G., Stanley S.A., Zollner A.N., Ghatei M.A., Bloom S.R. Hypothalamic actions of neuromedin U. Endocrinology. 2002;143:4227–4234. doi: 10.1210/en.2002-220308. [DOI] [PubMed] [Google Scholar]
- 358.Wu Q., Law P.Y., Wei L.N., Loh H.H. Post-transcriptional regulation of mouse μ opioid receptor (MOR1) via its 3′ untranslated region: a role for microRNA23b. FASEB J. 2008;22:4085–4095. doi: 10.1096/fj.08-108175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Wu M., Tang M., Adriaensen D., Depoortere I., Peeters T.L., Timmermans J.P. Central, but not peripheral application of motilin increases c-Fos expression in hypothalamic nuclei in the rat brain. Histochem. Cell Biol. 2005;123:139–145. doi: 10.1007/s00418-005-0763-8. [DOI] [PubMed] [Google Scholar]
- 360.Wu Y.H., Zhou J.N., Balesar R., Unmehopa U., Bao A., Jockers R., Van Heerikhuize J., Swaab D.F. Distribution of MT1 melatonin receptor immunoreactivity in the human hypothalamus and pituitary gland: colocalization of MT1 with vasopressin, oxytocin, and corticotropin-releasing hormone. J. Comp. Neurol. 2006;499:897–910. doi: 10.1002/cne.21152. [DOI] [PubMed] [Google Scholar]
- 361.Xie G.X., Meuser T., Pietruck C., Sharma M., Palmer P. Presence of opioid receptor-like (ORL1) receptor mRNA splice variants in peripheral sensory and sympathetic neuronal ganglia. Life Sci. 1999;64:2029–2037. doi: 10.1016/s0024-3205(99)00150-2. [DOI] [PubMed] [Google Scholar]
- 362.Yamada T., Mochiduki A., Sugimoto Y., Suzuki Y., Itoi K., Inoue K. Prolactin-releasing peptide regulates the cardiovascular system via corticotrophin-releasing hormone. J. Neuroendocrinol. 2009;21:586–593. doi: 10.1111/j.1365-2826.2009.01875.x. [DOI] [PubMed] [Google Scholar]
- 363.Yamaguchi H., Sasaki K., Satomi Y., Shimbara T., Kageyama H., Mondal M.S., Toshinai K., Date Y., González L.J., Shioda S., Takao T., Nakazato M., Minamino N. Peptidomic identification and biological validation of neuroendocrine regulatory peptide-1 and -2. J. Biol. Chem. 2007;282:26354–26360. doi: 10.1074/jbc.M701665200. [DOI] [PubMed] [Google Scholar]
- 364.Yokoi H., Arima H., Kondo K., Murase T., Iwasaki Y., Yang H.Y., Oiso Y. Antiserum against neuropeptide FF augments vasopressin release in conscious rats. Peptides. 1998;19:393–395. doi: 10.1016/s0196-9781(97)00375-6. [DOI] [PubMed] [Google Scholar]
- 365.Young W.S., Kuhar M.J. A new method for receptor autoradiography: [3H]opioid receptors in rat brain. Brain Res. 1979;179:255–270. doi: 10.1016/0006-8993(79)90442-6. [DOI] [PubMed] [Google Scholar]
- 366.Young W.S., Li J., Wersinger S.R., Palkovits M. The vasopressin 1b receptor is prominent in the hippocampal area CA2 where it is unaffected by restraint stress or adrenalectomy. Neuroscience. 2006;143:1031–1039. doi: 10.1016/j.neuroscience.2006.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Young L.J., Nilsen R., Waymire K.G., MacGregor G.R., Insel T.R. Increased affiliative response to vasopressin in mice expressing the V1a receptor from a monogamous vole. Nature. 1999;400:766–768. doi: 10.1038/23475. [DOI] [PubMed] [Google Scholar]
- 368.Young W.S., Shepard E.A., Burch R.M. Plasma hyperosmolality increases G protein and 3′,5′-cyclic adenosine monophosphate synthesis in the paraventricular and supraoptic nuclei. Mol Endocrinol. 1987;1:884–888. doi: 10.1210/mend-1-12-884. [DOI] [PubMed] [Google Scholar]
- 369.Yue C., Mutsuga N., Sugimura Y., Verbalis J., Gainer H. Differential kinetics of oxytocin and vasopressin heteronuclear RNA expression in the rat supraoptic nucleus in response to chronic salt loading in vivo. J. Neuroendocrinol. 2008;20:227–232. doi: 10.1111/j.1365-2826.2007.01640.x. [DOI] [PubMed] [Google Scholar]
- 370.Zhang Y., Gray T.S., D’Souza D.N., Carrasco G.A., Damjanosk K.J., Dudas B., Garcia F., Zainelli G.M., Sullivan Hanley N.R., Battaglia G., Muma N.A., Van de Kar L.D. Desensitization of 5-HT1A receptors by 5-HT2A receptors in neuroendocrine neurons in vivo. J. Pharmacol. Exp. Ther. 2004;310:59–66. doi: 10.1124/jpet.103.062224. [DOI] [PubMed] [Google Scholar]
- 371.Zheng H., Loh H.H., Law P.Y. Agonist-selective signaling of G protein-coupled receptor: mechanisms and implications. IUBMB Life. 2010;62:112–119. doi: 10.1002/iub.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Zheng H., Zeng Y., Zhang X., Chu J., Loh H.H., Law P.Y. μ-Opioid receptor agonists differentially regulate the expression of miR-190 and NeuroD. Mol. Pharmacol. 2010;77:102–109. doi: 10.1124/mol.109.060848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Zhong M.K., Shi Z., Zhou L.M., Gao J., Liao Z.H., Wang W., Gao X.Y., Zhu G.Q. Regulation of cardiac sympathetic afferent reflex by GABA(A) and GABA(B) receptors in paraventricular nucleus in rats. Eur. J. Neurosci. 2008;27:3226–3232. doi: 10.1111/j.1460-9568.2008.06261.x. [DOI] [PubMed] [Google Scholar]
- 374.Zhou X.J., Yang J., Yan F.L., Wang D.X., Li X.Y., Fan X.Q., Hao F., Yan X.Q., Li X.P., Li H., Liu W.Y., Lin B.C. Norepinephrine plays an important role in antinociceptive modulation of hypothalamic paraventricular nucleus in the rat. Int. J. Neurosci. 2010;120:428–438. doi: 10.3109/00207450802333649. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
GPCR signal transduction components detected in the PVN by DNA microarrays.
GPCR signal transduction components detected in the SON by DNA microarrays.
GPCRs detected in the rat PVN and SON by receptor ARG.
GPCRs in the paraventricular nucleus (PVN) and supraoptic nucleus (SON) of the rat hypothalamus: a summary of the literature.
GPCRs noted as present in rat PVN arrays.
GPCRs noted as present in rat SON arrays.
Orphan GPCRs in the rat PVN & SON.
Examples of GPCR regulation in the PVN and SON.
Some functions of GPCRs in the rat PVN/SON.
References for Supplementary Tables.