Abstract
Human dirofilariasis is a zoonotic infectious disease caused by the filarial nematodes of dogs Dirofilaria repens and Dirofilaria immitis. Depending on the species involved, human infections usually manifest as one cutaneous or visceral larva migrans that forms a painless nodule in the later course of disease. Dirofilariae are endemic in the Mediterranean, particularly in Italy. They are considered as emerging pathogens currently increasing their geographical range. We present one of the few known cases of human dirofilariasis caused by D. repens in Romania. The patient developed unusual and severe clinical manifestations that mimicked pathological conditions like cellulitis or deep venous thrombosis.
1. Introduction
Human dirofilariasis is a zoonotic infectious disease caused by parasites of the genus Dirofilaria [1–3]. Dirofilariae are a group of filarial nematodes infecting various carnivores as definitive hosts. The adult dirofilariae release microfilaria into the host's blood, which may be taken up by various mosquitoes that serve as intermediate hosts and transmit the disease. Humans may be infected as aberrant hosts, mainly by Dirofilaria (D.) immitis and D. repens. The definitive hosts of D. repens and D. immitis are dogs, but other animals have also been reported as reservoirs of the disease (cats, wolves, bears, foxes, etc.) [1, 3]. In human infections usually just one larva develops, which does not reach fertility [2, 3]. The larva wanders through the human body and finally forms a nodule. D. repens usually resides subcutaneously, while D. immitis frequently ends up in the human lung. In most cases parasites cause few symptoms. D. immitis infections in particular are therefore frequently detected only incidentally and are initially often confused with malignancies.
D. repens has been reported from various regions of the world with warm to moderate climate, but only very rarely from Romania [1, 4]. We report a human D. repens infection from Romania, which produced an atypical and severe clinical picture.
2. Case Presentation
A male, 31-years-old patient, with no significant medical history, presented in February 2011 with a cellulitis-like plaque on the right inner thigh (10 cm diameter) that, in about 12 hours, extended to almost the entire thigh. He was living in a Romanian suburban area (near Bucharest) and had a pet dog. The patient denied recent or past travel abroad, except for France (Paris) for a weekend, 4 months earlier (in October). The putative diagnosis at that time was cellulitis, and antibiotic treatment was started with amoxicillin-clavulanic acid (for 5 days). All symptoms subsided rapidly within 24–48 hours.
One week later the patient developed severe muscle pain in the lower right leg, and after a further two days he noticed a similar cellulitis-like plaque as before (red, edematous, warm with imprecise limits) in the popliteal region, with rapid extension to the adjacent areas, associated with impaired walking ability due to extensive edema. Doppler ultrasound showed no signs of thrombosis in the right leg. Laboratory investigations showed mild eosinophilia (7.2%; normal range 0–7%). All other investigations including complete blood count, sedimentation rate, urinalysis, and liver and renal function tests were normal. Because of the severity of symptoms, treatment with the macrolide antibiotic azithromycin and the low-molecular-weight heparin enoxaparin was administered for 7 days. Again the symptoms resolved quickly and completely.
After about two further weeks, the patient developed similar but less severe lesions on the lower right part of the abdomen that were again associated with muscle pain (Figure 1(a)).
Figure 1.
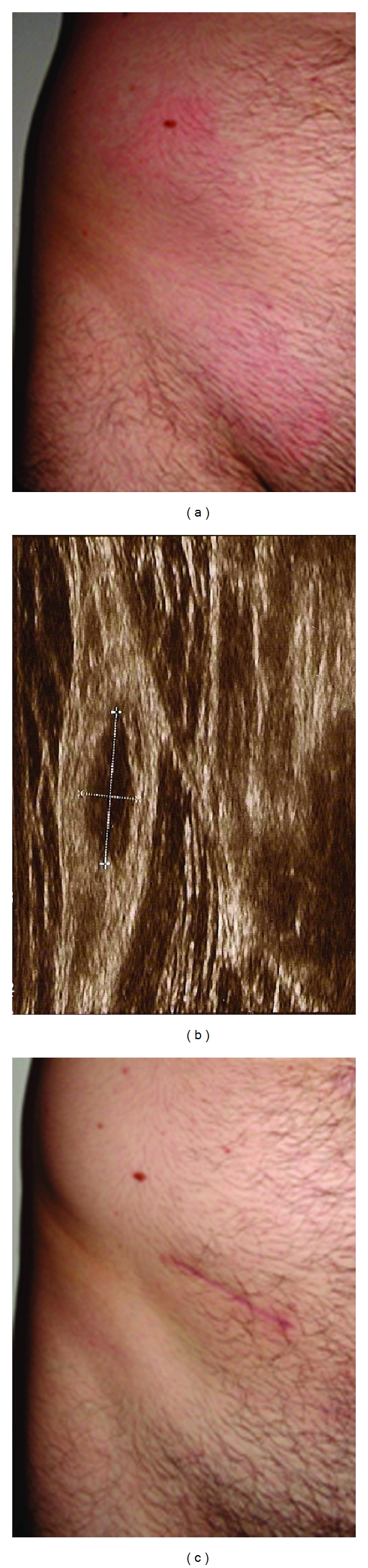
Clinical picture before and after surgery. Before the removal of the parasite, the patient showed erythematous plaques with mild edema in the lower right abdominal region (a). The ultrasound revealed a well-defined cystic lesion of 11.9 mm × 4.8 mm above muscular layer, which is seen on the right (b). After excision of the nodule the wound healed without complications and all symptoms resolved. The scar reveals the final location of the parasite (c).
Infectious disease screening was performed and showed positive serology for Echinococcus (E.) granulosus IgG (ELISA) and negative tests for Borrelia burgdorferi, Toxoplasma gondii, Toxocara canis, Trichinella spiralis, EBV, CMV, HBV, HCV, and HIV. Abdominal ultrasound and chest radiography were normal.
Because of the eosinophilia and the positive E. granulosus serology, a parasitological cause was suspected and albendazole treatment was started (800 mg/day). During antiparasitic therapy, the inflammatory abdominal plaque resolved, but a nodule developed deep in the subcutaneous tissue (Figure 1(b)). The nodule was excised, and all signs of infection including the eosinophilia subsided, and no further symptoms developed (Figure 1(c)).
The excised material was investigated histopathologically using hematoxylin-eosin (HE), Giemsa, and Masson's trichrome stains, periodic acid-Schiff reaction, and immunohistochemistry for IgE (Figure 2). The histopathology was similar to that described for subcutaneous dirofilariasis in previous reports [5, 6]. The parasite showed the typical features of a nongravid female D. repens. The most indicative structures were the external longitudinal ridges, leading to a cogwheel-like appearance in the transverse sections (Figures 2(a), 2(b), and 2(c)). Further typical features were the thick cuticula and the well-developed musculature (Figures 2(a) and 2(c)). Around the parasite a marked inflammatory reaction had developed (Figures 2(d) and 2(e)). The histological slides showed numerous eosinophils, neutrophils, lymphocytes, plasma cells, and macrophages. (Figures 2(d) and 2(e)). Occasionally, eosinophils and neutrophils, partly with pycnotic nuclei, were seen on the surface of the parasite (Figures 2(d) and 2(e)). Many IgE-positive plasma cells were present in the infiltration and near to the surface of the parasite (Figure 2(f)).
Figure 2.
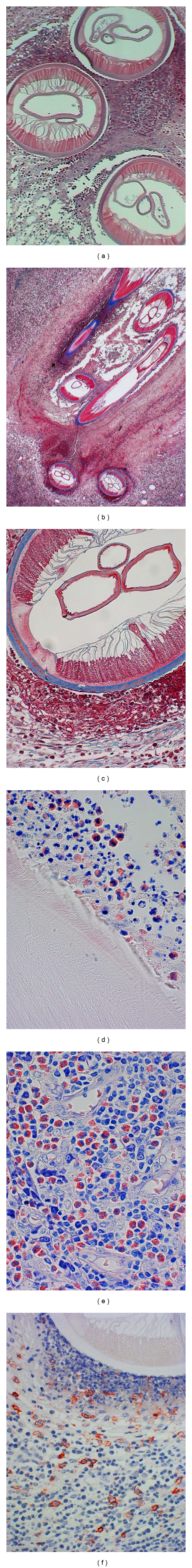
Histological sections of the parasite. Sections were stained using hematoxylin-eosin (HE) (a), Masson's trichrome stain (b, c), Giemsa (d, e), and periodic acid-Schiff reaction and immunohistochemistry for IgE (f). Typical features of D. repens are the external longitudinal ridges, the thick cuticula, and the well-developed musculature (a, b, c). Around the parasite a marked inflammatory reaction with numerous eosinophils, neutrophils, lymphocytes, plasma cells, and macrophages is seen (d, e). Many IgE-positive plasma cells are present in the infiltration and near to the surface of the parasite (f).
To confirm the morphological diagnosis, DNA was isolated from the tissue sample embedded in paraffin wax and a PCR targeting the mitochondrial 12S rRNA was performed as described before [7, 8]. Sequence analysis of the PCR product showed the highest similarity to Italian isolates of D. repens, thus confirming the morphological identification of our isolate as D. repens.
Serum samples were investigated retrospectively for antifilarial antibodies using an ELISA composed of D. immitis antigen. The test was positive as expected. In addition, the presence of antibodies against E. granulosus was confirmed by ELISA and indirect hemagglutination, but not by a western blot confirmation test. The patient was thoroughly screened for signs of an Echinococcus infection by sonography and CT scans, but no indications of a hydatid cyst were found.
In order to exclude the patient's dog as a source of (further) D. repens infections, blood samples were obtained and investigated for microfilaria using Giemsa stain and PCR. No microfilaria or filarial DNA was found.
3. Discussion
We present a case of human D. repens infection with an atypical presentation that was most likely acquired in Romania. Human infection with D. repens usually presents as larva migrans and later in the course of infection as a subcutaneous nodule [2, 3]. However, infection may cause a wide variety of symptoms depending on the site of infection [2, 3]. In our case D. repens infection was associated with an unusual clinical presentation, namely, signs of cellulitis and deep venous thrombosis. We cannot definitively say what caused the symptoms in our case and cannot exclude any cause of the symptoms other than D. repens. It seems extremely unlikely that an Echinococcus infection was responsible for the symptoms since we did not find any sign of Echinococcus infection. It could not be clarified whether the positive reactions with the E. granulosus tests were caused by an asymptomatic previous contact with Echinococcus or just by unspecific cross-reactions. The finding of Echinococcus antibodies with ELISA must be interpreted as an incidental finding without relevance for the described case.
The facts that the symptoms developed close to the site of the D. repens worm and that all symptoms subsided only when the D. repens was removed strongly suggest that the worm was the true cause of the symptoms. Most probably the worm initially wandered in the subcutaneous tissue and provoked a local immune response. It may be speculated that the antibiotic treatment contributed to the temporary resolution of symptoms. A possible mechanism would be by attack on the endosymbiont Wolbachia, which contributes to the immune reaction of the host [9]. Equally, the worm may have wandered to another less sensitive place, and the temporary resolution of symptoms after antibiotic treatment might have been coincidental. However, the antiparasitic treatment most likely had an effect and indeed led to the arrest of the worm, allowing its subsequent removal. Because usually only one infertile parasite is present, removal of the worm is sufficient. However, it is scarcely possible to locate and surgically remove a subcutaneously wandering worm, because the main signs of infection are present in the region that the parasite has just vacated. As long as the worm is not wandering through the subconjunctiva, where it can be precisely located, surgery should not be performed before the worm has stopped its journeying. As our case shows, an anthelmintic treatment can be used to stop the worm. Such anthelmintic therapy leading to the arrest of a wandering worm and allowing removal of the worm has successfully been applied before (G. Just-Nuebling, Frankfurt, personal communication, 2011).
The exact source of infection of our patient could not be determined. We did not find signs of infection with D. repens in the patient's dog. Considering the longevity of the worm in its final host, the dog, it is unlikely but not impossible that the patient's dog was the source of its owner's infection. It is highly unlikely that the patient acquired the infection during the short trip to Paris because the disease is hardly present in French urban dogs and there are only very low numbers of mosquitoes in Paris in October. The infection was therefore most likely acquired in the region of residence (near Bucharest) in Romania. Only a few cases of human infection with D. repens have so-far been described in Romania [4]. It is well known that D. repens occurs in moderate climatic zones of Europe, with a hot spot in northern Italy [2, 3]. Recently, increasing numbers of human dirofilariasis cases have been reported from France and Greece, and first cases have even been found north of the Alps, in countries such as the Czech Republic, Hungary, Russia, and Austria [1, 10–13]. It has been suggested that D. repens is an emerging disease that is spreading under the influence of global climate warming [14]. D. repens is thus probably more frequent in Romania than the so-far sparse case reports imply, and the number of cases might be increasing.
Human doctors as well as veterinarians should therefore be prepared to come across cases of dirofilariasis in Romania, as well as in other European countries regarded nonendemic so far. As our case illustrates, infection should even be considered in patients with signs of parasitic infection that do not exactly correspond to the description of dirofilariasis in the text books.
Acknowledgments
The authors thank the patient for his cooperation and his approval to publish this case report. They thank Rolf Horstmann, Egbert Tannich, and Bernhard Fleischer from the Board of Directors of the Bernhard Nocht Institute for their support.
References
- 1.Genchi C, Kramer LH, Rivasi F. Dirofilarial Infections in Europe. Vector Borne and Zoonotic Diseases. Larchmont, NY, USA: 2011. [DOI] [PubMed] [Google Scholar]
- 2.Pampiglione S, Rivasi F, Angeli G, et al. Dirofilariasis due to Dirofilaria repens in Italy, an emergent zoonosis: report of 60 new cases. Histopathology. 2001;38(4):344–354. doi: 10.1046/j.1365-2559.2001.01099.x. [DOI] [PubMed] [Google Scholar]
- 3.Pampiglione S, Rivasi F. Human dirofilariasis due to Dirofilaria (Nochtiella) repens: an update of world literature from 1995 to 2000. Parassitologia. 2000;42(3-4):231–254. [PubMed] [Google Scholar]
- 4.Mǎnescu R, Bǎrǎscu D, Mocanu C, et al. Subconjunctival nodule with Dirofilaria repens. Chirurgia. 2009;104(1):95–97. [PubMed] [Google Scholar]
- 5.Brattig NW, Racz P, Hoerauf A, Büttner DW. Strong expression of TGF-beta in human host tissues around subcutaneous Dirofilaria repens. Parasitology Research. 2011;108:1347–1354. doi: 10.1007/s00436-010-2028-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ratnatunga N, Wijesundera MDS. Histopathological diagnosis of subcutaneous Dirofilaria repens infection in humans. Southeast Asian Journal of Tropical Medicine and Public Health. 1999;30(2):375–378. [PubMed] [Google Scholar]
- 7.Casiraghi M, Bain O, Guerrero R, et al. Mapping the presence of Wolbachia pipientis on the phylogeny of filarial nematodes: evidence for symbiont loss during evolution. International Journal for Parasitology. 2004;34(2):191–203. doi: 10.1016/j.ijpara.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Poppert S, Hodapp M, Krueger A, et al. Dirofilaria repens infection and concomitant meningoencephalitis. Emerging Infectious Diseases. 2009;15(11):1844–1846. doi: 10.3201/eid1511.090936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grandi G, Morchon R, Kramer L, Kartashev V, Simon F. Wolbachia in Dirofilaria repens, an agent causing human subcutaneous dirofilariasis. Journal of Parasitology. 2008;94(6):1421–1423. doi: 10.1645/GE-1575.1. [DOI] [PubMed] [Google Scholar]
- 10.Auer H, Susani M. The first autochthonous case of subcutaneous dirofilariosis in Austria. Wiener Klinische Wochenschrift. 2008;120(4):104–106. doi: 10.1007/s00508-008-1031-4. [DOI] [PubMed] [Google Scholar]
- 11.Ondriska F, Lengyel D, Miterpáková M, Lengyelová B, Strehárová A, Dubinský P. Human dirofilariosis in the Slovak Republic—a case report. Annals of Agricultural and Environmental Medicine. 2010;17(1):169–171. [PubMed] [Google Scholar]
- 12.Kartashev V, Batashova I, Kartashov S, et al. Canine and human dirofilariosis in the rostov region (Southern Russia) Veterinary Medicine International. 2011;2011 doi: 10.4061/2011/685713. Article ID 685713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fodor E, Fok E, Maka E, Lukats O, Toth J. Recently recognized cases of ophthalmofilariasis in Hungary. European Journal of Ophthalmology. 2009;19(4):675–678. doi: 10.1177/112067210901900424. [DOI] [PubMed] [Google Scholar]
- 14.Genchi C, Mortarino M, Rinaldi L, Cringoli G, Traldi G, Genchi M. Changing climate and changing vector-borne disease distribution: the example of Dirofilaria in Europe. Veterinary Parasitology. 2011;176(4):295–299. doi: 10.1016/j.vetpar.2011.01.012. [DOI] [PubMed] [Google Scholar]


