Abstract
Background:
A large number of women undergo caesarean section throughout the world. These women pass through a period of post operative pain and a morbidity period. These women translate into a substantial portion of population and hence there is a load on the financial resources of healthcare system. Use of the appropriate technique to approximate the wound after caesarean section would not only avoid financial load but also help in early recovery of the patient.
Aim:
The aim of this study is to compare the effects of alternative techniques for closure of subcutaneous fat and skin on maternal health and use of healthcare resources in caesarean section.
Materials and Methods:
Patients undergoing Caesarean section were divided in two groups of one thousand patients each. Patients with hematological disorders or a malignancy, diabetes, septicemia or chorioamnionitis were excluded from the study. In all the patients, after stitching the uterus, the rectus sheath was stitched with thread vicryl No.1 (synthetic absorbable braided sutures with polyglycolic acid, polycaprolactone and calcium stearate coating), using a round body needle. Then the patients were divided into two groups. In group I, vicryl No.1 thread used in stitching of the rectus sheath was continued into the skin with application of subcuticular stitches, after securing the edges with a knot. In group II, after stitching the rectus sheath with vicryl No. 1, the thread was cut and interrupted sutures were applied in subcutaneous fat with thread vicryl No. 2. Skin was stitched with subcuticular stitches using proline 2, a non-absorbable propylene suture. The two groups of patients were observed for the duration of surgery, post-operative pain in stitches, patient satisfaction about removal of stitches, evidence of wound infection or seroma, and cosmetic results.
Results:
It was noted that the duration of surgery in group I was on average 7.5 minutes less as compared to the duration in group II. Patients in group I were more satisfied with the results of the surgery and were relieved to know that their stitches did not need to be removed.
Conclusion:
Although no difference was found in the rates of wound infection and formation of scar tissue between the group I and group II, the duration of surgery was less and the patients were more satisfied in group I.
Keywords: Subcuticular stitches, intradermal stitches, suture material
Introduction
The goals of wound closure include obliteration of dead space, even distribution of tension along deep suture lines, and maintenance of tensile strength across the wound. It is intended to achieve adequate tissue tensile strength after approximation and eversion of its epithelial portion. Methods employed for mechanical wound closure include staples, tape, adhesives, and sutures. Each method has specific indications, advantages and disadvantages. Suture closure permits primary wound healing as tissue is held in proximity until enough healing has occurred to withstand stress without mechanical support. Suture material being a foreign body implanted in the human tissue elicits a foreign body tissue reaction. During wound closure, a sterile field and a meticulous aseptic technique are critical to minimize the risk of wound infection. Complications of wound healing such as hypertrophic scars, wide scars and wound dehiscence can result from patient factors, such as nutritional status, incorrect suture selection or a technique which causes excessive tension across the wound.
Monofilament suture is made of a single strand, a structure that is relatively more resistant to harboring microorganisms. The monofilament sutures experience less resistance to passage through tissue than multifilament suture. Great care must be taken in handling and tying a monofilament suture because crushing or crimping can nick or weaken the suture leading to premature suture failure. A multifilament suture is composed of several filaments twisted or braided together. Although this material is less stiff, it has a higher coefficient of friction. Multifilament suture generally has greater tensile strength, better pliability and flexibility than monofilament suture. This type of suture ties well. Since multifilament materials have more capillarity, the resultant increased absorption of fluid may act as a tract for the introduction of pathogens.
Caesarean section is one of the most commonly performed abdominal operations on women in most countries of the world. Its rate has increased markedly in recent years, and is about 20–25% of all child-births in most developed countries[1,2]. The rates in other parts of the world vary widely, from 1.6% of all child-births in Haiti to 59% in Chilean private hospitals[3]. A variety of surgical techniques for all elements of the caesarean section operation are in use[4]. Many of these have not yet been rigorously evaluated in randomized controlled trials, and it is not known whether or not they are associated with better outcomes. There is not enough evidence to say whether any particular technique for closing the abdominal wall during caesarean section is better than the others[5]. Because of the large number of women that undergo caesarean section, even small differences in post-operative morbidity rates due to different techniques could translate into improved health for a substantial number of women and significant savings of cost and health services resources.
Materials and Methods
This study was conducted on two thousand patients undergoing primary caesarean section; these patients were divided into two equal groups. Only patients with a transverse incision during an elective or emergency caesarean section were included in this study. Patients with established or gestational diabetes, coagulation defects, hemodynamic instability, septicemia or chorioamnionitis were excluded. Patients on cytotoxic drugs or anticoagulants and those with hematological disorders or malignancy were also excluded from the study. The subject study was carried out in Military Hospital, Rawalpindi, Pakistan. This study was given approval through an internal mechanism of military; involving the relevant specialist and administrative staff giving ethical approval. Written informed consent was taken from all patients.
In group I, after stitching the uterus, the rectus sheath was stitched with thread vicryl No.1 on a round body needle; after securing the edges with a knot, the thread of rectus sheath was continued into the skin with application of subcuticular stitches. In group II, after stitching the rectus sheath with vicryl No. 1, the thread was cut and interrupted sutures were applied in subcutaneous fat with vicryl 2/0. Skin was stitched by subcuticular stitches with proline 2/0. Prophylactic antibiotics were given for 24 hours. All surgeries were performed by consultants or residents with at least two years of training. Only round body needles were used in these surgeries. All the surgeries were done under regional spinal analgesia.
Dressing was opened on the second post-operative day. Patients were discharged from the hospital and called back between 8th and 12th post operative days. The patients in group I did not require removal of stitches while the stitches of patients in group II were removed between 8th and 12th post operative days. The two groups of cases were observed for the duration of surgery and were followed up for post-operative pain in stitches, patient's satisfaction about removal of stitches, evidence of wound infection or seroma and cosmetic results. The data was collected in the Operation Theater immediately following the surgery, at discharge from the hospital, at first post-natal visit and six weeks after delivery. To allow a comparable assessment of pain, Visual Analogue Scale (VAS) was used with a 10 cm line labeled at ‘0’ with ‘no pain’ and ‘10’ with ‘worst pain’. The line was marked at a point corresponding to the assessment of the pain. The distance of the mark from zero was measured (Fig. 1).
Fig. 1.
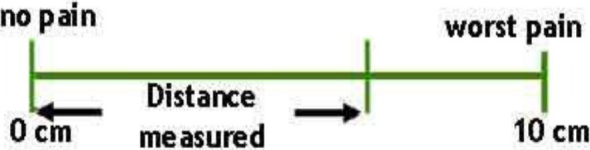
Visual analogue scale (VAS) used to assess post-operative pain.
Results
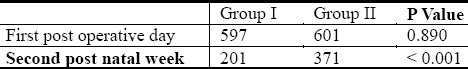
Table 1 shows the average duration of surgery. It is to be noted that the duration of surgery in group I on the average was 7.5 minutes less as compared to patients in group II. The degree of pain was assessed on the basis of Visual Analogue Scale (VAS) with significant pain as more than 5/10. The data was analysed on SPSS. P value was calculated to be less than 0.05. Data was presented as proportion and percentages. Pain was significantly less in group I (Table 2).
Table 1.
Duration of surgery
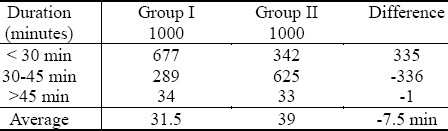
Table 2.
Post operative pain in Visual Analogue Scale
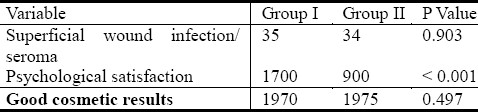
Patients in group I were more satisfied with the results of the surgery; and they were relieved to know that their stitches did not need to be removed. There were no patients in either group with a morbid wound infection. Few cases of superficial wound infection and seroma were found in both groups which did not require any treatment except a few dressings. Cosmetic results in both groups were equally good (Table 3).
Table 3.
Other post operative variables.
Discussion
Absorbable sutures provide temporary wound support, until the wound heals well enough to withstand the normal stress. The absorbable surgical sutures are made from either “natural” or synthetic polymers. Natural polymers include collagen, surgical gut and chromic. Their absorption occurs by enzymatic degradation. Synthetic sutures are chemical polymers absorbed by hydrolysis and cause a lesser degree of tissue reaction following placement. These sutures include Polyglactin 910 (Vicryl): Poliglecaprone 25 (Monocryl): Polysorb and Polydioxanone.
The first stage of absorption has a linear rate lasting for several days to weeks. The second stage is characterized by a loss of suture mass and this stage overlaps the first stage. The loss of suture mass occurs as a result of leukocytic cellular responses that remove cellular debris and suture material from the line of tissue approximation. Chemical treatments such as chromic salts lengthen the absorption time. Accelerated absorption may occur in patients with fever, infection or protein deficiency and may lead to an excessively rapid decline in tensile strength. Accelerated absorption may also occur in a body cavity that is moist, filled with fluid or if the sutures become wet or moist during handling prior to implantation.
Non-absorbable sutures elicit a tissue reaction that results in encapsulation of the suture material by fibroblasts. Non-absorbable sutures are natural (surgical silk) or synthetic (nylon, Polypropylene-Prolene). Prolene, a monofilament suture, is an isostatic crystalline stereoisomer of a linear propylene polymer; it permits little or no saturation. The material does not adhere to tissues and is useful as a pull-out suture (e.g., subcuticular closure). Polypropylene also holds knot better than other monofilament synthetic material. This material is biologically inert and elicits minimal tissue reaction. Prolene is not subject to degradation or weakening and maintains tensile strength for up to 2 years. This material is useful in contaminated and infected wounds, minimizing the chances of sinus formation and suture extrusion.
Much of the process regarding suture selection depends on the surgeon's training and preference. A wide variety of suture materials are available for each surgical location and surgical requirement. Generally the surgeon selects the smallest suture that can adequately hold the healing wound edges and is able to achieve a tension-free closure. The tensile strength of the suture should never exceed the tensile strength of the tissue. As the wound heals, the relative loss of suture strength over time should be slower than the gain of tissue tensile strength. Aesthetic concerns are at a premium in women. Sutures are no longer needed when a wound has reached maximum strength. Therefore, non-absorbable suture are considered in skin, fascia and tendons (slowly healing tissues), while mucosal wounds (rapidly healing tissues) may be closed with absorbable sutures. Wound closure and healing is affected by the initial tissue injury caused by needle penetration and subsequent suture passage. Needle selection, surface characteristics of the suture (e.g. coefficient of friction) and suture-coating material are important factors that must be considered by the surgeon.
Ideal surgical needle characteristics include high-quality stainless steel, smallest possible diameter, stability in the grasp of needle holder, capability of implanting suture material through tissue with minimal trauma, sharpness enough to penetrate tissue with minimal resistance, sterile and corrosion-resistance to prevent introduction of microorganisms or foreign materials into the wound. Taper-point (round) needle penetrates and passes through tissues by stretching without cutting. A sharp tip at the point flattens to an oval/rectangular shape. Curved needle has a predictable path through tissue and requires less space for maneuvering than a straight needle. The semicircular path is the optimal course for sutures through tissue and provides an even distribution of tension. The main consideration in needle selection is to minimize trauma. A taper needle is sufficient for tissues that are easy to penetrate. The ideal suture should be biologically inert and cause no tissue reaction. It should be very strong but simply dissolve in body fluids and lose strength at the same rate that the tissue gains strength. It should be easy for the surgeon to handle the suture and knot it reliably. It should neither cause nor promote complications. While there have been great improvements in suture materials in the recent past and the modern sutures are very close to the above ideal, no single suture is ideal in all situations. Different tissues have different requirement for suture support, some need only a few days of support such as muscle, subcutaneous tissue, and skin; while others require weeks or even months such as fascia and tendon. Healing of wounds is delayed by a range of factors such as infection, debility, respiratory problems, obesity, collagen disorders, malnutrition, malignancy, and drugs such as cytotoxics and steroids. The surgeon wants to ensure that a suture will retain its strength until the tissue regains enough strength to prevent separation. Subjective preferences such as familiarity with the material and availability are also to be taken into account. It could be said that it is always best to use an absorbable suture unless there is a good reason not to use it. When used for skin closure, non-absorbable suture must be removed or they will lead to chronic sepsis.
Caesarean section is a common operation with no agreed standards on operative techniques and materials to use. There is no conclusive evidence about how the skin should be closed after a caesarean section. Questions regarding the best closure technique, material used and the outcome associated with each remain unanswered. The appearance and strength of the scar following caesarean section is important to women and the choice of technique and materials should be made by women in consultation with their obstetrician based on the limited information that is currently available. There is not enough evidence to say whether any particular technique for closing the abdominal wall during a caesarean section is better than the others[5]. No substantial differences in strength of incision closure or cosmetic outcome were found in the different techniques involving an intradermal suture with non-reabsorbable thread, metallic clips and 2-octyl-cyanoacrylate (2-OCA) glue[6]. The subcutaneous fat (between the sheath and the skin) may be left to heal without suturing, or can be closed using a variety of techniques. Closing the subcutaneous fat may reduce the risk of some wound complications (haematoma and seroma) but further research is needed to investigate how these outcomes affect the well being and recovery of the patient concerned[5].
The aim of our study was to examine two specific aspects of techniques used in caesarean section to help determine which method can lead to a better outcome for women and health care resources. It was a randomized trial making comparison of (a) suture used for closure of subcutaneous fat versus none, and (b) suture materials used for closure of skin.
The risk of hematoma or seroma was reduced with fat closure as compared with non closure. No difference in the risk of wound infection alone or other short-term outcomes was found[5]. There was no case of death or maternal infectious morbidity in any group. Patients were observed for six weeks after delivery and there was no operative procedure on wound, blood transfusion or primary post partum hemorrhage. It is important that caesarean section operations are performed as safely and effectively as possible and that methodologically rigorous randomized controlled trials are performed to establish the effectiveness of different surgical techniques.
Conclusion
The best way of closing the mother's skin layer after caesarean section is not known. Improvements in health from optimizing caesarean section techniques are likely to be more significant in developing countries because the rates of postoperative morbidity in these countries tend to be higher. More women could therefore benefit from improvements in techniques. Given the very high number of caesarean sections performed, even small differences may be important for the cost of health services or the population's health. Although duration of operation was documented as variable, it may have no correlation with maternal or neonatal outcome. There was wide variation in the surgical techniques used by obstetricians for caesarean section operations. There is an urgent need for future research to evaluate many aspects of caesarean section operations on substantive short- and long-term outcomes[4].
Acknowledgement
Dr. Ambreen Ehsan collected data.
References
- 1.Menacker F, Curtin SC. Trends in cesarean birth and vaginal birth after previous cesarean, 1991-99. Natl Vital Stat Rep. 2001;49(13):1–16. [PubMed] [Google Scholar]
- 2.Thomas J, Paranjothy S. The National Sentinel Caesarean Section Audit report. London: Royal College of Obstetricians and Gynecologists; 2001. [Google Scholar]
- 3.Belizan J, Althabe F, Barros F, Alexander S. Rates and implication of cesarean sections in Latin America: ecological study. BMJ. 1999;319:1397–1402. doi: 10.1136/bmj.319.7222.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tully L, Gates S, Brocklehurst P, Ayers S, McKenzie-McHarg K. Surgical techniques used in caesarean section operations in the UK: a survey of current practice. Eur J Obstet Gynecol Reprod Biol. 2002;102:120–126. doi: 10.1016/s0301-2115(01)00589-9. [DOI] [PubMed] [Google Scholar]
- 5.Anderson ER, Gates S. Techniques and materials for closure of the abdominal wall in caesarean section. Cochrane Database of Systematic Reviews. 2004;4:CD004663. doi: 10.1002/14651858.CD004663.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Croce P, Frigoli A, Perotti D, Di Mario M. Cesarean section, techniques and skin suture materials. Minerva Gynecol. 2007;59(6):595–599. [PubMed] [Google Scholar]


