Abstract
Context:
Wandering spleen is an unusual condition characterized by the absence or maldevelopment of one or all of the ligaments securing the spleen in its normal position in the left upper abdomen. Pedicular tortion with a complete vascular disruption is a rare but known potential complication of this mostly congenital disorder. Spontaneous hemoperitoneum with acute abdomen however, is a life threatening situation that has not been adequately reported in the adult literature.
Case Report:
A forty four year old man presented to the emergency department with an acutely distended and rigid abdomen. His past medical history was only significant for mild mental retardation. The patient denies prior abdominal operation or recent trauma. On initial examination, he appeared to be anxious, pale, and tachycardic. Fullness in the midpelvic region was easily appreciated on palpation. An enlarged pelvic spleen and free intraperitoneal fluid consistent with blood were seen on a CT scan. The patient was promptly taken for an exploratory laparotomy where a large rush of blood was encountered upon entering the abdomen. A volvulus of the splenic pedicle with an infarcted spleen was found mandating a splenectomy.
Conclusions:
Abnormally located spleen, splenomegaly, and finding of hemoperitoneum are highly suggestive of wandering spleen with tortioned pedicle. Despite its life threatening presentation, immediate laparotomy and splenectomy invariably result in good outcome.
Keywords: Wandering spleen, pedicular tortion, hemoperitoneum, splenectomy
Introduction
Wandering spleen is an unusual condition characterized by an increased splenic mobility related to laxity or abscence of the splenogastric, splenorenal, or splenocolic ligaments. The first description of wandering spleen is credited to Van Horne during an autopsy in 1667[1]. It can occur at all ages but more commonly seen in reproductive aged women raising a suspicion that the splenic ligamentous laxity might be related to the hormonal effects of pregnancy[2]. This condition may present as an asymptomatic abdominal/pelvic mass, intermittent intestinal obstruction, or acute abdominal pain. Tortion of a wandering spleen is exceedingly rare with an incidence below 0.2%[3]. The authors report an unusual case of wandering spleen with pedicular tortion on a middle aged man presenting with large hemoperitoneum and abnormally located enlarged spleen.
Case Report
A forty four year old man presented to the Geisinger clinic emergency department for an evaluation of worsening abdominal pain associated with low grade fever, nausea and vomiting that had started one day prior to admission. The patient denied prior abdominal complaints, recent trauma, or changes in bowel habits. On the physical examination, he appeared to be anxious, mildy tachypneic and pale with heart rate of 132 beats per minute. An abdominal palpation showed moderate distention, diffuse rigidity with guarding, rebound tenderness, and hypoactive bowel sounds. Complete blood count showed a leukocytosis of 22.5 mg/dl, bandemia of 14%, hemoglobin of 9.6 mg/dl (baseline of 15 mg/dl). Liver function tests, pancreatic enzymes, and lactic acid were all within normal limits.
A CT scan showed an abnormally located spleen in the lower pelvis measured 15.7 × 10 × 9.2 cm (Figs. 1 and 2). The splenic artery descended inferiorly through the midabdomen and was markedly tortuous, suggesting a pedicular volvulus. The splenic parenchyma failed to enhance following intravenous contrast injection as what typically would have been seen in a normal spleen. The body and tail of the pancreas appeared to be coiled around the splenic vessels (Fig. 3). Significant volume of high density fluid consistent with hemoperitoneum was observed. No free air was identified.
Fig. 1.
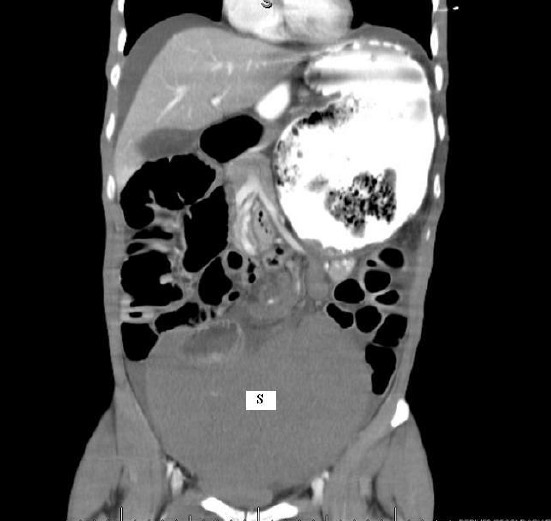
The enlarged spleen located in the pelvis with hemoperitoneum. S=Spleen
Fig. 2.
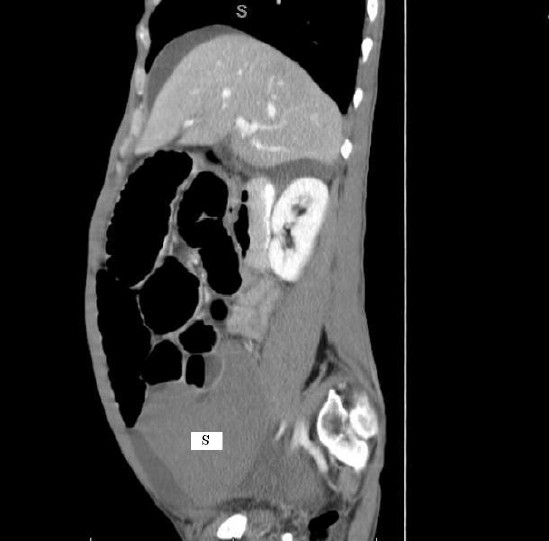
The sagittal section of enlarged spleen in the pelvis with hemoperitoneum. S=Spleen
Fig. 3.
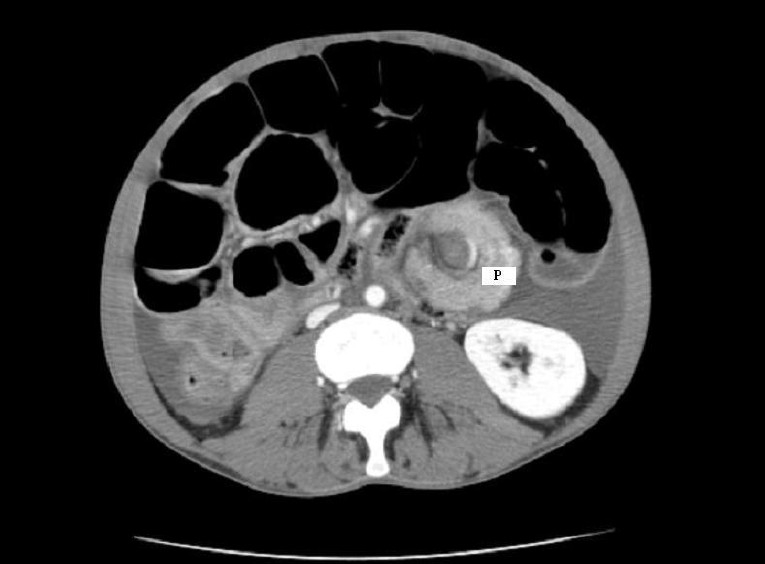
Tortion of the distal pancreas surrounding the splenic vessels. Notice an enhanced splenic artery after intravenous contrast injection. P=Pancreas
Exploratory laparotomy was promptly performed revealing a large rush of blood upon entering the peritoneal cavity. Once the midline incision was advanced inferiorly, a large mobile spleen was found in the pelvis which was easily brought up into the operative field. There was a volvulus of the splenic pedicle and distal pancreas. Following detortion and inspection, the spleen appeared to be permanently infarcted. A routine splenectomy was performed. Approximately one liter of blood was suctioned and the abdomen was thoroughly irrigated using three liters of normal saline. There was no other obvious pathology found.
Postoperatively, the patient was transferred to the postoperative care unit and medical-surgical floor in a stable condition. He made an uneventful recovery. Pathology report showed a congested spleen without other histopathologic abnormality. The patient was discharged to home on POD 4 after tolerating a regular diet. Pneumococcal, meningococcal and Hemophilus influenza vaccines were given.
Discussion
During embriogenesis, the spleen begins its development in the fifth week of gestation from the mesenchymal cells in the dorsal mesogastrium[4]. This dorsal mesogastrium is also responsible for the formation of the peritoneum, greater omentum and peritoneal folds including the major splenic ligaments[2]. It was proposed that abnormal laxity and elongated hilum allow the spleen to freely migrate and become hypermobile in the abdomen. The incidence of wandering spleen is 15 times greater in women compared to that in men, especially in women between 20 and 40 years of age suggesting the role hormonal factor[5]. Etiology of wandering spleen is most likely multifactorial, including both congenital and acquired. Splenomegaly from any causes may predispose to the wandering spleen, however by itself is unlikely to play a significant role since there is no increased incidence of wandering spleen in geographic regions with endemic splenomegaly from infectious origin[4,6].
Clinical presentation is widely variable. Sixty percent of patients experience abdominal pain or discomfort, while the remainders are asymptomatic[5]. Even though the pain is mostly acute indicating an acute torsion, volvulus of the spleen resulting in splenic vessels obstruction and parenchymal infarction may also be chronic and intermittent from repeated tortion-detortion[4].
Diagnosis usually made by an ultrasound or a CT scan with intravenous contrast. When pancreatic tail is involved, a whorl of normal appearing pancreatic and fat tissues at the medial border of the displaced spleen may be seen. Doppler studies can also be employed to evaluate the status of the vascular flow. The presence of an abdominal or pelvic mass, abnormally located bowel loops, findings of gastrointestinal obstruction, and elevated left kidney are sometimes seen on plain film[7]. Laboratory findings of leukocytosis, thrombocytopenia, and anemia may be present however they are nonspecific as well as nondiagnostic.
A unique presentation of acute gastric hemorrhage secondary to wandering spleen has also been reported by Angeras et al[8]. In that case, a pedicular tortion resulted in impaired blood return via the splenic vein. As the consequence, collateral circulations then built through the short gastric vessels leading to a formation of isolated gastric varices and ultimately bleeding from the stomach fundus. Differential vascular compression has also led to a splenic congestion and platelet sequestration. Another unusual presentation of hypermobile spleen which resulted in recurrent episodes of acute pancreatitis was reported by Choi YH et al[9]. In this case, the recurrent pancreatitis was attributable to a counterclockwise rotation of the pancreatic tail resulting in intermittent kinking/obstruction of the pancreatic duct which then subsequently led to mechanical pancreatitis.
The treatment options for hypermobile spleen include observation, splenopexy, and splenectomy. Watchful management has been found to lead to splenic torsion and infarction in more than half of the patients, therefore an elective operation is recommended[10]. The splenopexy and splenectomy can be performed either with open or laparoscopic approach.
In the case of open splenectomy, access to the left upper quadrant can be obtained either through a midline or left subcostal incision. Splenic detortion and hilar transection must be performed carefully to avoid rupture/bleeding and injury to the pancreatic tail respectively. The later complication may further lead to an acute pancreatitis and pancreatic fistula formation. Majority of patients however were successfully managed using conservative approach which entail bowel rest with or without total parenteral nutrition until resolution of their hyperlipasemia or fistulae. Pancreatic injuries did not occur more often in patients with large spleens. Other potential complications include postoperative hemorrhage requiring reoperation, subphrenic abscess, and incisional wound complications. Nowadays, abdominal drain is not used routinely anymore after a splenectomy due to the increased incidence of intraabdominal infection/abscess.
In children, splenic preservation is always preferred in order to minimize the risk of infection, especially with encapsulated organisms. In this young population, the risk of developing postsplenectomy septicemia is 4%, with fatality rate of 1.8%. In adults, they are slightly less, 1.9% and 1.1% respectively. The more rarely seen overwhelming postsplenectomy sepsis however, has a fatality rate of 60%[11].
Several authors have therefore described conservative management of this condition with various techniques of laparoscopic splenopexy. It has been well known that the laparoscopic approach offers benefits such as shorter hospital stay, less immune system attennuation, earlier return of bowel function and quicker postoperative recovery. The laparoscopic splenopexy can be performed via creation of an extra/retroperitoneal pocket to house the spleen, direct suture fixation of the splenic hilum to the splenic bed, colonic displacement in front of the spleen followed by a gastropexy to the anterior abdominal wall, or creation of an intraperitoneal pocket using absorbable mesh and omentum[12–17]. All patients should receive pneumococcus, meningococcus and Hemophilus influenzae vaccines in the case of splenectomy.
Conclusions
Wandering spleen is a rare entity that should be considered in patients presenting with acute abdomen and an abnormal palpable mass. The clinical presentation ranges from asymptomatic condition to a surgical emergency requiring splenectomy. The risks and benefits of various treatment options should be discussed and tailored to the individual patients.
References
- 1.Lane TM, South LM. Management of wandering spleen. J R Soc Med. 1999;92(2):84–85. doi: 10.1177/014107689909200211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen KB, Gay BB, Skandalakis JE. Wandering spleen: Anatomic and radiologic consideration. South Med J. 1992;85:976–984. doi: 10.1097/00007611-199210000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Fernandez EM L, Gonzales IA, Malagon AM, et al. An unusual case of hemoperitoneum owing to acute splenic tortion in a child with imunoglobulin deficiency. J Postgrad Med. 2006;52:41–42. [PubMed] [Google Scholar]
- 4.Lewis GA, Byrne MP. Wandering spleen. Ann Surg. 1981;47:275–277. [PubMed] [Google Scholar]
- 5.Desai DC, Hebra A, Davidoff AM, et al. Wandering spleen: A challenging diagnosis. South Med J. 1997;90:439–443. doi: 10.1097/00007611-199704000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Carswell JW. Wandering spleen. 11 cases from Uganda. BR J Surg. 1974;61:495–497. doi: 10.1002/bjs.1800610620. [DOI] [PubMed] [Google Scholar]
- 7.Beuhner M, Baker MS. The wandering spleen. Surg Gynecol Obstet. 1992 Oct;175(4):373–387. [PubMed] [Google Scholar]
- 8.Angeras U, Almskog B, Lukes P, et al. Acute gastric hemorrhage secondary to wandering spleen. Dig Dis Sci. 1984;29:1159–1163. doi: 10.1007/BF01317093. [DOI] [PubMed] [Google Scholar]
- 9.Choi YH, Menken FA, Jacobson IM, et al. Recurrent acute pancreatitis : An additional manifestation of the wandering spleen syndrome. Am J Gastroenterol. 1996;91(5):1034–1038. [PubMed] [Google Scholar]
- 10.Thomson JS, Ross RJ, Pizzaro ST. The wandering spleen in infancy and childhood. Clin Pediatr (Phila) 1980;19:221–224. doi: 10.1177/000992288001900309. [DOI] [PubMed] [Google Scholar]
- 11.Dalpe C, Cunningham M. Wandering spleen as an asymptomatic pelvic mass. Obstet Gynecol. 2003;101(5 Pt 2):1102–1104. doi: 10.1016/s0029-7844(02)02618-2. [DOI] [PubMed] [Google Scholar]
- 12.Cohen MS, Soper NF, Underwood RA, et al. Laparoscopic splenopexy for wandering (pelvic) spleen. Surg Laparosc Endosc. 1998;8:286–290. [PubMed] [Google Scholar]
- 13.Caracciolo F, Bonatti PL, Castrucci G, et al. Wandering spleen: treatment with colonic displacement. J R Coll Surg Edinb. 1986;31:242–244. [PubMed] [Google Scholar]
- 14.Martinez-Ferro M, Elmo G, Laje P. Laparoscopic pocket splenectomy for wandering spleen. A case report. J Pediatr Surg. 2005;40:882–884. doi: 10.1016/j.jpedsurg.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 15.Lacreuse I, Moog R, Kauffmann I, et al. Laparoscopic splenopexy for a wandering spleen in a child. J Laparoendosc Adv Surg Tech A. 2007;17(2):255–257. doi: 10.1089/lap.2006.0005. [DOI] [PubMed] [Google Scholar]
- 16.Tan H, Ooi LP, Tan D, et al. Recurrent abdominal pain in a woman with a wandering spleen. Singapore Med J. 2007;48(4):e122. [PubMed] [Google Scholar]
- 17.Fukuzawa H, Urushihara N, Ogura K, et al. Laparoscopic splenopexy for wandering spleen: extraperitoneal pocket splenopexy. Pediatr Surg Int. 2006;22(11):931–934. doi: 10.1007/s00383-006-1760-2. [DOI] [PubMed] [Google Scholar]


