Abstract
Background:
The length of postnatal hospital stay for healthy newborns remains controversial. Proponents of early hospital discharge claim that it is safe, decreases the risk of iatrogenic infection, promotes family bonding and attachment, and reduces hospitalization care and patient costs. Disadvantages include delayed breastfeeding, manifestation of new conditions affecting newborns after early discharge, and improper discharge planning.
Aim:
The main aim of the study was to compare early discharge versus late discharge with the risk of readmission.
Patients and Methods:
The length of hospital stay was recorded for all healthy newborns and infants and followed by investigation of any medical problem arising after discharge. Factors associated with readmission to the hospital were analyzed by Chi square and Mantel-Haenszel Common Odds Ratio Estimate (OR) with Confidence Limits (CL).
Results:
A total of 478 babies were enrolled, of which 307 were discharged ≤ 48 hours. The overall length of stay was 39 hours (1.6 days). Thirty-eight (7.9%) newborns were re-hospitalized, with the most common cause being neonatal jaundice. Factors associated with readmission for jaundice were breastfeeding (OR: 10.3 CL3.10to32.20) and length of stay ≤ 48 hours (OR: 13.8, CL4.04 to 47.05).
Conclusion:
Hospital discharge at any time ≤ 48 hours significantly increases the risk for readmission as well as the risk for readmission due to hyperbilirubinemia. Planning and implementing a structured program for follow up of infants who are discharged ≤ 48 hours are vital in order to decrease the risk for readmission, morbidity and neonatal mortality.
Keywords: Length of Postnatal Stay, Re-hospitalization after discharge, hyperbilirubinemia
Introduction
The length of hospital stay for newborns and mothers after uncomplicated deliveries has decreased and has become commonplace worldwide. In the United States, the mean length of stay reported in 1992 was 2.6 days and declined to 1.1 days in 1995 for vaginal deliveries[1]. This trend towards early newborn discharge has also been reported in 22 other countries[2].
Proponents of early discharge claim that it is safe, decreases the risk of iatrogenic infection, promotes family bonding and attachment, and reduces the hospitalization care and patients costs. However, concerns have also been expressed about potential disadvantages of early discharge: 1) breastfeeding is not established until the third or later postpartum day[3]; 2) a number of conditions do not manifest themselves until 2 or more days after delivery; 3) time is reduced for in-hospital teaching on breastfeeding, infant care and women's health. Braveman[4] concluded that “the currently available literature provides little scientific evidence to guide discharge planning for most apparently well newborns and their mothers”. Lee[5] recorded that shorter hospital stays were associated with increased number of readmission, within 14 days of life and the severity of these re-hospitalized infants was increased. Liu[6] found that discharging healthy infants within 30 hours of birth increased the risk of readmission within 28 days by 22%.
To our knowledge, no previous studies or published guidelines by the Lebanese Neonatal and Perinatal Societies exist that determine the optimal timing of discharge or follow-up period following early discharge. The main goal of this study was to compare early discharge versus late discharge with the risk of readmission. This study also examined the preventable causes of readmission, the mean cost of readmissions and the break-even point for preventing readmission.
Patients and Methods
A prospective study was conducted for a period of 7 months (September 2009 - March 2010). This study covered all healthy neonates after their discharge from the Nursery ward at Makassed General Hospital (MGH) in Beirut. On average, our hospital conducts 1200-1500 deliveries per annum. Infants were followed by investigating any medical problem arising after discharge by contacting their caregivers until the infants’ age of 14 days.
Newborn infants admitted to Neonatal Intensive Care Unit (NICU) for prematurity ≤ 34 weeks, intrauterine growth retardation (IUGR), respiratory distress, asphyxia, pathological hyperbilirubinemia, congenital malformations, and those requiring admission to NICU immediately after birth, were excluded from the study population. Data recorded for each subject included maternal factors (parity, mode of delivery, adequacy of antenatal check up, presence of maternal medical disease (e.g. chronic hypertension, diabetes mellitus, asthma and anemia), obstetric complications (e.g. gestational hypertension and diabetes, pre-eclampsia and eclampsia, lacerations, urgent cesarean section) and neonatal factors (such as birth weight and gestational age) .
As per our hospital policy, the mother-infant pair is discharged at the same time. A newborn was considered fit for discharge if he/she was on breast milk/bottle feeding, had urinated and passed meconium, with no physical abnormalities and normal vital signs (respiration<60/min, HR<100-160/min, rectal temperature 36-37C), had been vaccinated with hepatitis B vaccine, received vitamin K, and metabolic screen was taken. The mother and relatives are counseled regarding breastfeeding.
Length of stay (LOS) was defined as the interval between birth and discharge (in completed hours) and noted for all study subjects. Early discharge was defined as the postpartum length of stay at or before ≤ 48 hours, following the American Academy of Pediatrics (AAP) definition[7].The newborn was re-hospitalized if there was jaundice requiring intervention or any other major morbidity, including sepsis. The admitting diagnoses of such newborns were recorded. This study was approved by the Institutional Review Board (IRB) Committee of the Makassed General Hospital.
Statistical Analysis
Chi square and Mantel-Haenszel Common Odds Ratio Estimate (OR) with Confidence Limit (CL) were applied to determine the factors contributing to NICU readmission. Factors contributing significantly to readmission were included as independent variables. P<0.05 was considered significant.
Results
During the study period, a total of 686 deliveries were performed. Of these, 107 neonates required admission to NICU immediately after birth and were excluded. Five hundred seventy nine neonates were followed, of these 101 were lost for follow up; the remaining 478 newborns were enrolled in our study.
Two hundred sixty four (264) were born by normal vaginal delivery (NVD) and 214 by cesarean section (C-section). Figure 1 illustrates the subjects’ characteristics. Of the 478 neonates, 307 (64%) were discharged at or before ≤ 48 hours. While 171 neonates were discharged after 48 hours, the mean length of stay was 39 hours (1.6 days) of all deliveries. Total number of patients readmitted to NICU was 38 (7.9%), out of which 34 patients were early discharged ≤ 48 hours (Figures 2 & 3).
Fig. 1.
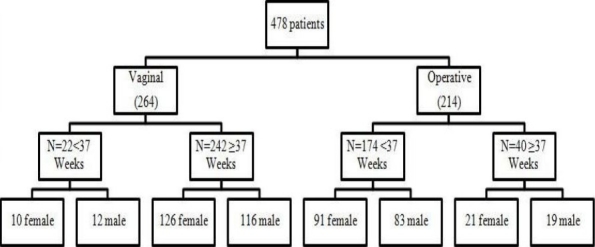
Patients characteristics. Data presented as numbers.
Fig. 2.
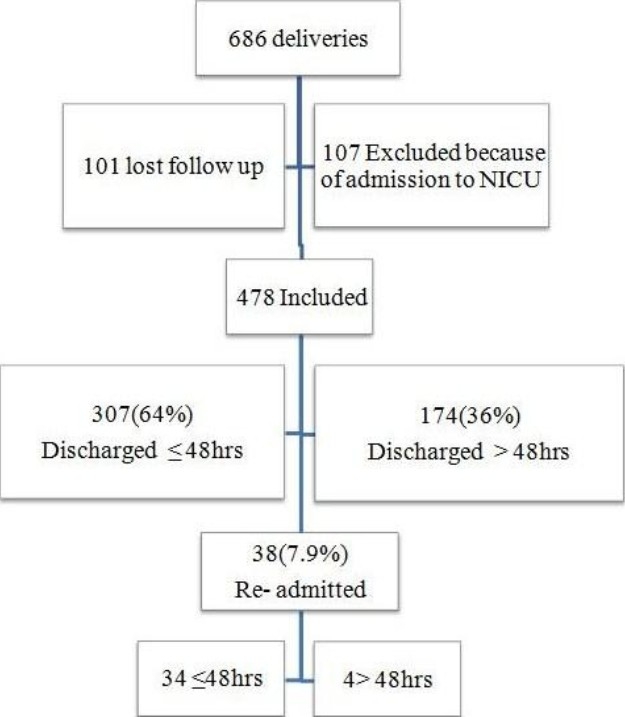
Study flow chart. Data presented as numbers and percentages.
Fig. 3.
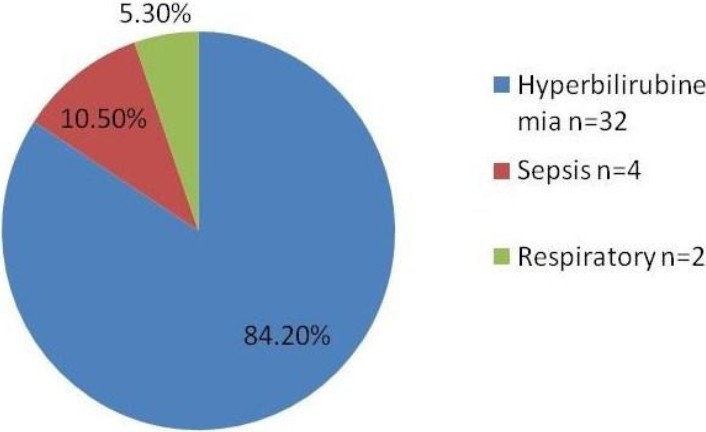
Number and percentages of admissions according to the etiology.
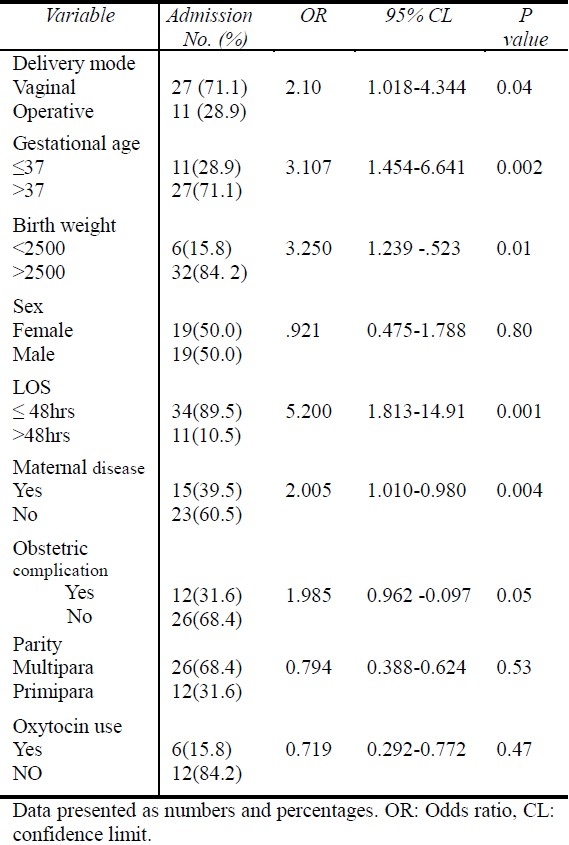
Factors associated with increased risk of readmission to the hospital were: 1) Vaginal delivery (OR: 2.10; CL 1.08 to 4.34), 2) Birth weight < 2500 gram (OR: 3.25 CL 1.23 to 8.52), 3) Pre-existing maternal complications (OR: 2.0 CL 1.01 to 3.98), and 4) Gestational age≤ 37 weeks (OR: 3; CL 1.45 to 6.64 (Table 1).
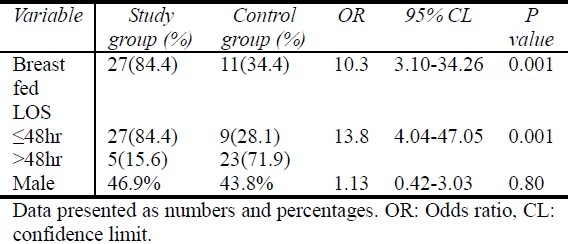
Table 1.
Risk for readmission by the age of 14 days
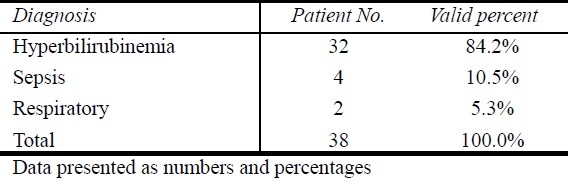
Thirty-two subjects (84.2%) were readmitted due to hyperbilirubinemia, four (10.5%) with a diagnosis of “rule out sepsis” and two (5.3%) for respiratory distress. Discharge diagnoses among thirty-two hyperbilirubinemic patients included two with Rhesus (Rh) hemolytic disease, eight with ABO hemolytic disease and 22 with idiopathic jaundice; 16 (72%) were breast fed. The mean bilirubin level in infants readmitted for phototherapy was 16.3 mg/dL (range 14.5 to 19mg/dL). Hyperbilirubinemia accounted for the majority of readmissions. Since this is potentially preventable, we compared 32 infants readmitted for jaundice with a randomly selected group who were not readmitted. The factors associated with readmission for jaundice in these infants are shown in Table 3. All infants admitted for hyperbilirubinemia received phototherapy; none of the cases needed exchange transfusion.
Table 3.
Factors associated with readmission for jaundice
All four cases of sepsis were early discharged ≤ 48 hours and were readmitted to NICU within 1.5 days following discharge. These neonates underwent septic screen and received antibiotic therapy ranging from 3 to 10 days according to biological parameters (complete blood count and differential, C-reactive protein and blood culture results). All re-hospitalized infants were discharged within 4 to 12 days (Table 2).
Table 2.
Diagnoses in 38 infants readmitted within 14 days of discharge
Discussion
This study showed that early discharge ≤ 48 hours was associated with increased likelihood of readmission during the first 2 weeks of life as compared with later discharge. The average length of stay for healthy newborn infants for all hospital deliveries was 39 hours (1.6 days) and readmission rate was 7.9%. Our findings are similar to the study done by Gupta[2] in India where the mean length of stay was reported to be 46 hours (1.9 days) and the readmission rate was 8.3%. This is in contrast to other studies that had been conducted in developed countries, such as the United States and Canada, where the mean length of stay was 62 hours (2.6 days)[1] and 64 hours (2.7 days)[5], with a readmission rate of 0.8% and 2.7%, respectively.
In our study, the readmission rate is 10 times greater than that in developed countries. This difference is due to insufficient education provided to lactating mothers, and mainly due to lack of post-discharge home nursing visits that assess the infant's general health, hydration, jaundice and feeding problems. Therefore, hospital readmission rates are reduced among infants who receive early follow-up visits or home visits[8–10]. In addition to discharge timing, other factors were found to be associated with the increased risk of readmission.
One of the most contributing factors to the significant rise in readmission is vaginal delivery. 94% of all healthy vaginally delivered are routinely discharged at or before ≤48 hours, and more than 8.7% were readmitted to NICU. Vaginal delivery increases the probability of readmission as compared to neonates who were delivered by cesarean section. Soskolne and Kring[11,12] reported that vaginal delivery is a risk factor for readmission. Anthony[13] found that the most strongly associated factor with a decreased likelihood of readmission for jaundice was cesarean delivery. Bragg[14] found that implementation of a structured program for early neonatal discharge does not have an association with increased risk of neonatal readmission to the hospital.
Late preterms are physiologically and metabolically immature. They are at higher risk than term infants to develop medical complications and are more likely than term infants to be admitted to NICU[15]. Several case control studies designed to evaluate risk factors for neonatal hospital readmission after birth have identified late preterm birth as a significant risk factor[11,15,16]. In our study, we found that late preterms were re-hospitalized 2.7 times more than term infants, similar to Anthony et al. who concluded that late preterm gestation was associated with ≤ 3 times increase in the risk of readmission[13]. Our results concerning late preterm risk of re-hospitalization were 1.5 times more than those presented by Tomashek et al.[16].
We found a significantly increased risk of readmission for low birth weight (<2500 gram) newborns of 2.8 times greater than that of normal birth weight. This is similar to the results published in California by Beate[3] and Anthony[13].
The presence of maternal complications was also associated with increased risk of readmission. Our results were comparable to Beate[3]. In this study, male sex was not found to be an associated factor in increased readmission rate. Of all of the conditions found to account for readmission to the hospital within 14 days, only hyperbilirubinemia is susceptible to a type of intervention that might prevent readmission. In our data, we found that neonatal jaundice is the first cause of re-hospitalization, accounting for 84% of all admissions. A similar cause of readmission was reported in the literature, in which jaundice accounted for 50% of the subjects[2,12,17] .We more closely examined the factors associated with readmission for jaundice as shown in Table 3. LOS≤ 48 hours was an important factor associated with the risk of readmission, the same significance was found for breastfeeding, similar to the results published by Jeffrey et al[12]. In fact, breastfeeding is not established until the third or later postpartum day[3], and it is likely that mothers discharged early do not have the opportunity to establish proper lactation on the first postpartum day under the guidance of nursing staff and lactation counselors[12]. In addition, Eidelman et al. have demonstrated that women on the first postpartum day score significantly lower than non-pregnant women on standardized tests of cognitive function, and these mothers will not be able to reliably integrate information given to them by caregivers, which could have an impact on the infant's well-being in the next several days[18]. To evaluate the possible effects of inadequate nursing, we observed the weight loss of infants readmitted for hyperbilirubinemia in the first 7 days. There were 20 such infants and we compared them with 15 infants who had been readmitted within 7 days for reasons other than jaundice, dehydration, or failure to thrive. The jaundiced babies had a mean weight loss (from birth weight) of 2.6% versus 0.1% in the non-jaundiced babies (with a difference of 2.5%; CL:10.7 to 3.5; P=0.0001). The difference between the two groups suggests less adequate fluid and caloric intake in the jaundiced group, which is consistent with previous observations[12].
Moreover, the practice recognized by our population, mainly replacing breastfeeding with glucose water solution, causes constipation and subsequently increases the enterohepatic circulation that leads to an increase in jaundice. Another common practice is covering of the infant with a yellow scarf instead of appropriate management. Recent data suggest the readmission rate for breastfeeding problems is approximately 0.3% to 2% of term or near term infants[6]. Hall[19] confirm that short hospital stays are risk factors for readmission of insufficiently breastfed infants with hyperbilirubinemia.
Attempts to decrease the risk of hyperbilirubinemia should be directed at the early establishment of effective lactation, as well as closer surveillance for those infants who have risk factors for readmission. These include vaginal delivery, gestation <37 weeks, length of stay ≤48 hours, and birth weight <2500 gr.
In our study, the increased rate of readmission due to sepsis is 0.8% versus 0.2% as shown by Jeffrey[12]. This is secondary to poor prenatal care, and lack of group B streptococcus (GBS) screening. Saoud and Yunis[20] found that pregnant women in Lebanon appear to have a relatively high prevalence of GBS colonization with no identifiable risk factors for its acquisition. These results could provide a basis for a national policy for universal maternal GBS screening in order to reduce neonatal morbidity and mortality.
Decreases in the length of hospital stay for newborns may result in a substantial increase in the readmission rate[21]. Lee and colleagues found that with a decrease in length of stay from 4.5 to 2.7 days, there was an associated increase in the rate of hospital readmission[5]. In our study, we compared the group discharged early and the group discharged after 48 hours. We found that the former is at higher risk of readmission. At this point, several disadvantages are related to readmission: 1) the psychological effect of mother - newborn pair separation and parental anxiety; 2) the risk of nosocomial infection that can be acquired during hospitalization with increased infant mortality and morbidity, in addition to the complications of hyperbilirubinemia (kernicterus); and 3) elevated expenses due to breast milk replacement by bottle formula.
The decrease in length of stay leads to a higher risk for re-hospitalization unless there is a change in post discharge care, such as home visits by healthcare professionals and early follow-up. Kotagal et al[22] found that reductions in length of stay for full-term Medicaid newborns in Ohio have not resulted in an increase in re-hospitalization rates in the immediate postnatal period. This was explained by changing patterns of post discharge care, such as home visits, to encourage optimal lactation and the use of home phototherapy. The risk profiles and sheer numbers of births should encourage hospitals to consider the cost-effectiveness of preventive strategies. If the hospital stay is increased by an additional day, the number of readmissions can be decreased from 8.7% to 2.3%, and the cost from 174 million Lebanese Pounds (LP) to 121 million LP per 1000 infants discharged.
Conclusion
This study may provide an important aspect on the quality of care implications of current discharge policies and practices. We conclude that the major reason for hospital readmission in the first 2 weeks of life is hyperbilirubinemia - the most common cause which is potentially susceptible to intervention in the first few days of life. Attempts to decrease the risk of hyperbilirubinemia should be directed at the early establishment of effective lactation.
Recommendations
It is cost-effective and efficient to prolong hospitalizations in at-risk patients for readmission, particularly those born prematurely, having low birth weight <2500 gram and infants developing jaundice in the nursery.
To establish a structured strategic plan for the infants discharged ≤48 hours; this includes changing the patterns of post discharge care such as home visits by healthcare professionals or early follow-up.
To encourage and to educate lactating mothers by healthcare professionals.
Maternal GBS screening to reduce neonatal sepsis and related morbidity and mortality.
Finally, we suggest that morbidity and mortality resulting from early neonatal discharge can be markedly decreased and managed by following appropriate national guidelines.
Acknowledgement
The authors would like to thank Zouhair Naja, MD., Aouni Alameddine, MD., and Fouad Ziade, PhD. for their support and assistance in this work.
References
- 1.Centers for Disease Control and Prevention. Trends in Length of Stay for Hospital Deliveries - United States, 1970-1992. MMWR. 1995;44:335–337. [PubMed] [Google Scholar]
- 2.Gupta P, Malhotra S, Singh DK, Dua T. Length of hospital stay in healthy newborn re-hospitalization following their early discharge. Ind J Pediatrics. 2006;73:897–900. doi: 10.1007/BF02859282. [DOI] [PubMed] [Google Scholar]
- 3.Danielson B, Castles AG, Damberg CL, Gould JB. Newborn discharge timing and readmission, 1992-1995. Pediatrics. 2000;106:31–39. doi: 10.1542/peds.106.1.31. [DOI] [PubMed] [Google Scholar]
- 4.Braveman P, Egerter S, Pearl M, Machi K, Miller C. Early discharge of newborns and mothers: a critical review of the literature. Pediatrics. 1995;96:716–726. [PubMed] [Google Scholar]
- 5.Lee KS, Perlman M, Ballantyne M, Elliot J, To T. Association between duration of neonatal hospital stay and readmission rate. J Pediatrics. 1995;127:758–766. doi: 10.1016/s0022-3476(95)70170-2. [DOI] [PubMed] [Google Scholar]
- 6.Liu LL, Clemens CJ, Shay DK, Davis RL, Novack AH. The safety of newborn discharge; the Washington State experience. JAMA. 1997;278:293–298. [PubMed] [Google Scholar]
- 7.Committee on Fetus and Newborn. American Academy of Pediatrics. Hospital stay for healthy term newborns. Pediatrics. 2004;113:1434–1436. doi: 10.1542/peds.113.5.1434. [DOI] [PubMed] [Google Scholar]
- 8.Meara E, Kotagal UR, Atherton HD, Lieu TA. Impact of early newborn discharge legislation and early follow up visits on infant outcomes in a state of Medicaid problems. Pediatrics. 2004;113:1619–1627. doi: 10.1542/peds.113.6.1619. [DOI] [PubMed] [Google Scholar]
- 9.Escobar GJ, Green JD, Hulac P, Kincannon E, Bischoff K, Gardner MN. Rehospitalization after birth hospitalization: Patterns among infants of all gestations. Arch Dis Child. 2005;90:125–131. doi: 10.1136/adc.2003.039974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Welt SI, Cole JS, Myers MS, Sholes DM, Jr, Jelovsek FR. Feasibility of postpartum rapid hospital discharge: a study from a community hospital population. Am J Perinatol. 1993;10(5):384–387. doi: 10.1055/s-2007-994768. [DOI] [PubMed] [Google Scholar]
- 11.Soskolne El, Schumackher R, Fyock C, Young Ml, Schork A. The effects of early discharge and other factors on readmission rates of newborns. Arch Pediatr Adolesc Med. 1996;150(4):373–379. doi: 10.1001/archpedi.1996.02170290039006. [DOI] [PubMed] [Google Scholar]
- 12.Maisels MJ, Kring E. Length of stay, jaundice, and hospital readmission. Pediatrics. 1998;101:995–998. doi: 10.1542/peds.101.6.995. [DOI] [PubMed] [Google Scholar]
- 13.Burgos AE, Schmitt SK, Stevenson DK, Phibbs CS. Readmission for Neonatal Jaundice in California, 1991-2000: Trends and Implications. Pediatrics. 2008;121:e864–869. doi: 10.1542/peds.2007-1214. [DOI] [PubMed] [Google Scholar]
- 14.Bragg E, Rosenn BM, Khoury JC, Miodovnik M, Siddiqi TA. The effect of early discharge after vaginal delivery on neonatal readmission rates. Obstet Gynecol. 1997;89:930–933. doi: 10.1016/s0029-7844(97)85764-x. [DOI] [PubMed] [Google Scholar]
- 15.Engle W, Tomashek KM, Wallman C. and the Committee on Fetus and Newborn. Academy of Pediatrics. “Late preterm” population at risk. Pediatrics. 2007;129:1390–1401. doi: 10.1542/peds.2007-2952. [DOI] [PubMed] [Google Scholar]
- 16.Tomashek KM, Shaipora-Mendoza C, Weiss J, et al. Early discharge among late preterm and term newborns and risk of neonatal morbidity. Semin Perinatol. 2006;30:61–68. doi: 10.1053/j.semperi.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 17.Luca D, Carnielli Virgilio P, Paollilo P. Neonatal hyperbilirubinemia and early discharge from maternity ward. Eur J Pediatr. 2009;68:1025–1030. doi: 10.1007/s00431-009-0969-1. [DOI] [PubMed] [Google Scholar]
- 18.Eidelman Al, Hoffmann NW, Kaitz M. Cognitive deficits in women after childbirth. Obstet Gynecol. 1993;82(5):764–767. [PubMed] [Google Scholar]
- 19.Hall RT, Simon S, Smith M. Readmission of breast fed infants in the first 2 weeks of life. J Perinatol. 2000;20:432–437. doi: 10.1038/sj.jp.7200418. [DOI] [PubMed] [Google Scholar]
- 20.Soud M, Nassar AH, Zalloua P, et al. Prenatal and Group B screening and serotyping in Lebanon incidence and implications. Acta Obster Gyneco Scand. 2010;89(3):399–403. doi: 10.3109/00016340903560008. [DOI] [PubMed] [Google Scholar]
- 21.Lock M, Ray JG. Higher neonatal morbidity after routine early hospital discharge: Are we sending newborns home too early? CMAJ. 1999;161(3):249–253. [PMC free article] [PubMed] [Google Scholar]
- 22.Kotagal UR, Atherton HD, Eshett R. Safety of early discharge for Medicaid newborns. JAMA. 1999;282(12):1150–1156. doi: 10.1001/jama.282.12.1150. [DOI] [PubMed] [Google Scholar]


