Abstract
Purpose
Hip hemiarthroplasty dislocation is a serious complication in treatment of displaced intracapsular hip fractures. We investigated factors associated with an increased risk of dislocation after cemented hip hemiarthroplasty following the posterolateral approach.
Methods
Between January 2002 and December 2008, 602 hip fractures were treated with cemented unipolar hip hemiarthroplasty. A registry-based analysis was carried out to determine the total number of hemiarthroplasty dislocations in these patients. A control group of 96 patients without dislocation was randomly selected. Logistic regression analysis was performed to evaluate clinical and operative factors associated with dislocation.
Results
Thirty-four patients (5.6%) experienced at least one dislocation. Most were the result of a fall and occurred within two months after surgery. There was a trend for increased dislocation in patients who had been operated on more than 48 hours after admission and in patients who had a longer operative time. Smaller centre-edge angle and hip offset were observed in patients with dislocation. Recurrent dislocation was a significant problem, as 18 patients (62%) experienced multiple dislocations.
Conclusions
The risk of hemiarthroplasty dislocation following the posterolateral surgical approach may be reduced by prompt surgical treatment and fall prevention in the early postoperative period. Patients with smaller acetabular coverage seem more predisposed to dislocation after the posterolateral approach and may be more suitable for other surgical approaches.
Keywords: Medicine & Public Health, Orthopedics
Introduction
The treatment of choice for displaced fractures of the femoral neck in elderly patients is hemiarthroplasty [1, 2]. The benefits of this treatment modality are immediate full weight bearing and decreased reoperation rate, which both reduce postoperative morbidity rates [3]. Although rare, hemiarthroplasty dislocation can lead to multiple hospital admissions and a possible revision arthroplasty. Furthermore, early dislocation is associated with an increased mortality rate [4, 5]. Hemiarthroplasty dislocation may be related to surgical approach, patient-related factors and implant malpositioning, yet there are several inconsistent findings in the literature with respect to these predisposing factors [6–8]. An increased risk of dislocation has been shown for the posterolateral surgical approach compared with lateral approaches [6, 7, 9, 10]. This increased risk may be reduced by posterior capsule repair and short external rotator reattachment [11, 12]. In one study, gender and mental impairment were shown to be significant clinical risk factors for dislocation [5]. Failure to achieve an anatomical offset, and excessive residual femoral neck, may also influence the dislocation rate [5, 7].
Although there is no consensus on the optimal surgical approach, the posterior approach is still commonly used in hip hemiarthroplasty despite the higher dislocation rate. Previous studies focused primarily on evaluating predisposing factors for dislocation in the light of different surgical approaches. Therefore, this study was designed to determine the clinical and radiographic factors leading to an increased risk of dislocation when using the posterolateral approach in cemented hip hemiarthroplasty.
Materials and methods
Between January 2002 and December 2008, 575 consecutive patients were treated in our department with a cemented unipolar hemiarthroplasty for displaced femoral-neck fracture. No other treatment modalities were used in this patient group. Twenty-seven patients fractured both hips during this period. Thus, the total number of hip fractures was 602. A retrospective registry-based analysis was carried out in December 2009 to determine the total number of hemiarthroplasty dislocations in these patients. We identified 34 patients (5.6 %) who experienced at least one dislocation (Fig. 1). Of the 34 patients with a dislocation, 31 were alive at six months and 28 at one year after surgery. A control group of 96 patients (approximately 1:3 ratio of cases to controls) without a hemiarthroplasty dislocation was randomly selected from the 575 patients. All control patients were alive at least two years after hemiarthroplasty. The study was approved by the local ethical committee.
Fig. 1.
Postoperative radiograph after hip hemiarthroplasty due to a displaced femoral neck fracture in a 79-year old female (left). The patient suffered a fall five weeks postoperatively and was unable to walk. The radiographs showed a hemiartroplasty dislocation (right)
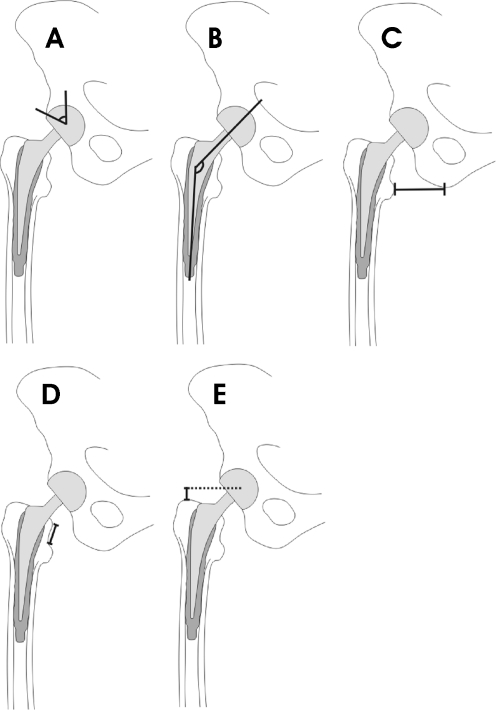
Hemiarthroplasty was performed using the posterolateral approach in all patients, as this is the standard technique in our department. Furthermore, a single implant design with a high-offset stem was used (LPP-EcoFit, Implantcast, GmbH). As our hospital is a teaching hospital, surgery was performed by a resident, a specialist, or both together. After surgery, standard anteroposterior and lateral radiographs were taken, and full weight bearing was started as soon as possible. Clinical data regarding patient demographics, medical comorbidities and surgical procedure details were collected from patient and operative records (Table 1). Postoperative radiographs were analysed to evaluate stem position and degree of acetabular dysplasia. Radiographic measurements performed included the centre-edge angle of Wiberg, prosthesis neck/femoral shaft angle, residual femoral neck length, offset measured as the distance between the the lesser trochanter tip and the ischial tuberosity and distance between the greater trochanter tip and centre of prosthesis head (Fig. 2) [7]. All radiographic measurements were performed in a blinded fashion by an experienced radiologist.
Table 1.
Patient demographics
| Patients with dislocation (n = 34) | Controls (n = 96) | |
|---|---|---|
| Age in yearsa | 78.5 (53–95) | 78.2 (48–97) |
| Genderb | ||
| Male | 7 (21) | 27 (28) |
| Female | 27 (79) | 69 (72) |
| BMIa | 24.3 (16.2–40.0) | 24.2 (17.2–35.2) |
| Sideb | ||
| Left | 18 (53) | 51 (53) |
| Right | 16 (47) | 45 (47) |
| Diseasesb | ||
| Dementia | 7 (21) | 23 (24) |
| Alcoholism | 4 (12) | 6 (6) |
| Living conditionsb | ||
| Home | 25 (74) | 65 (68) |
| Assisted living | 9 (26) | 31 (32) |
| Use of walking aidsb | 12 (35) | 43 (45) |
| Time from arrival to surgery hoursa | 39.4 (2.9–131.3) | 34.8 (2.2–141.2) |
| Surgery duration minutesa | 91 (25–236) | 88 (43–200) |
| Time of surgeryb | ||
| Working hours (8 a.m. to 3 p.m.) | 23 (68) | 64 (67) |
| Outside working hours (3 p.m. to 8 a.m.) | 11 (32) | 32 (33) |
| ASA classb | ||
| 1 and 2 | 6 (18) | 24 (25) |
| 3 and 4 | 28 (82) | 72 (75) |
| Component sizea | ||
| Head (mm) | 47 (42–58) | 47 (42–56) |
| Stem | 7.7 (5.0–12.5) | 7.7 (5.0–12.5) |
BMI body mass index, ASA American Society of Anesthesiologists
aValues gives as mean with range in parentheses.
bValues represent number of patients with percentage of total given in parentheses.
Fig. 2.
Measurements from postoperative radiographs. a Centre-edge angle of Wiberg, b prosthesis neck/femoral shaft angle, c offset, d residual femoral neck length, e distance between the tip of the greater trochanter and the centre of the prosthesis head
Categorical data is presented as absolute numbers and percentages. Continuous data is presented as mean values and ranges. Binary logistic regression analysis was performed to evaluate clinical and operative factors associated with dislocation. Comparisons between patients with a dislocation and controls are shown using odds ratios (OR) with 95% confidence intervals (CI). Student’s t test for independent samples was used to compare radiological parameters between groups. A p value of <0.05 was considered statistically significant. All analyses were performed using the SAS system for Windows version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
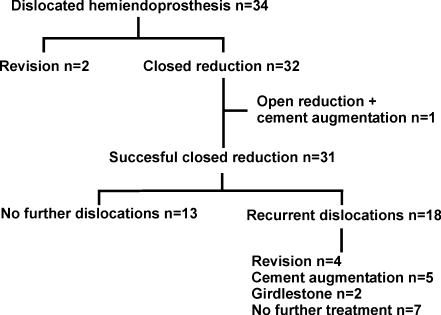
Mean time from surgery to the first dislocation was 35 days (range 1−408 days). Dislocations occurred within the first eight weeks of surgery, except for two late dislocations which occurred at three and 13 months . The most common cause for dislocation was a same-level fall (59%). In 26% of patients, dislocation occurred without trauma, and in 15%, the mechanism of dislocation was unknown. Closed reduction of the dislocation was successful in 94% of cases. Thirty eight percent experienced one dislocation during the follow-up period, and 62% had recurrent dislocations (Fig. 3). Patients with multiple dislocations underwent either revision arthroplasty (n = 4), cement augmentation of the acetabulum (n = 5) or the Girdlestone procedure (n = 2). In seven patients with more than one dislocation, no operative treatment was performed. One patient with multiple dislocations refused operative treatment.
Fig. 3.
Outcome in patients with dislocation
A delay of more than 48 hours and a prolonged operative time (>90 min) were the most important factors associated with a trend for increased dislocation risk (Table 2). Additionally, the use of walking aids prior to hip fracture seemed to be a protective factor against dislocation. Age, gender, body mass index, dementia, alcoholism, living conditions, American Society of Anesthesiologists (ASA) class, time of surgery and surgeon experience did not significantly increase dislocation risk.
Table 2.
Logistic regression analysis of patient-related factors for dislocation
| OR (95% CI) | P value | |
|---|---|---|
| Gender | ||
| Male | 0.66 (0.26-1.70) | 0.39 |
| Female | 1 | |
| Age (years) | ||
| >80 | 1.39 (0.63-3.04) | 0.41 |
| <80 | 1 | |
| BMI | ||
| >25 | 1.00 (0.44-2.31) | 0.99 |
| <25 | 1 | |
| Dementia | ||
| Yes | 0.78 (0.30-2.01) | 0.60 |
| No | 1 | |
| Alcoholism | ||
| Yes | 2.00 (0.53-7.57) | 0.31 |
| No | 1 | |
| Living conditions | ||
| Assisted living | 0.76 (0.32-1.81) | 0.53 |
| Home | 1 | |
| Use of walking aids | ||
| No | 1.72 (0.71-4.21) | 0.23 |
| Yes | 1 | |
| Time from arrival in hospital to surgery | ||
| >48 | 2.02 (0.79-5.15) | 0.14 |
| <48 | 1 | |
| ASA class | ||
| 3 and 4 | 1.56 (0.58-4.21) | 0.38 |
| 1 and 2 | 1 | |
| Time of surgery | ||
| Outside working hours | 0.96 (0.42-2.20) | 0.92 |
| Working hours | 1 | |
| Duration of surgery (min) | ||
| >90 | 1.85 (0.84-4.08) | 0.13 |
| <90 | 1 | |
| Surgeon experience | ||
| Resident | 1.06 (0.37-3.01) | 0.92 |
| Resident and specialist | 1 | |
OR odds ratio, CI confidence interval, ASA American Society of Anesthesiologists, BMI body mass index
Patients with a dislocation had a smaller centre-edge angle of Wiberg (42° vs. 47°, p = 0.029), shorter residual femoral neck (13 mm vs. 16 mm, p = 0.029) and a smaller offset (41 mm vs. 45 mm, p = 0.026). The prosthesis neck / femoral shaft angle (143° vs. 141°, p = 0.15), and distance between the greater trochanter tip and the centre of prosthesis head (0.4 mm vs. -0.7 mm, p = 0.44) were not significantly different between the groups.
Discussion
The study evaluated risk factors associated with hip hemiarthroplasty dislocation following the posterolateral surgical approach. The dislocation rate of 5.6% found in this study is comparable with previous reports when the posterolateral surgical approach was used [10, 13, 14], although dislocation rates as high as 16% have been reported [7]. Lower dislocation rates have been associated with the Hardinge approach in patients following hemiarthroplasty for hip fracture [7]. However, the Hardinge approach may be associated with problems related to hip-abductor dysfunction, leading to altered gait and a positive Trendelenburg sign [15]. This may hinder the postoperative rehabilitation process, leading to increased morbidity. Nevertheless, the Hardinge approach seems more appropriate in patients with high dislocation risk, such as those with a hip-flexion contracture or marked acetabular dysplasia.
In our study, dislocation occurred almost exclusively within the first eight weeks of surgery, and the most common mechanism was a fall. The redislocation rate was 62%, which was slightly higher than in previous studies, which ranged from 31–57% [6, 16, 17]. This highlights the fact that a majority of these patients will go on to experience chronic hemiendoprosthesis instability. In the early postoperative period, the stabilising effect of posterior soft tissue structures is still deficient, and even minor trauma is more likely to predispose to dislocation. It is evident that more attention should be paid to preventing falls in the early recovery period in this patient population. This issue is multifaceted and may include reducing psychotropic medications, appropriate use of walking aids and possibly home alterations to reduce the risk of falls. The study also showed a tendency for dislocation in patients who had not used any walking aids prior to fracture. This may be explained by the higher physical activity and hence associated with a potentially higher number of events predisposing to dislocation. Furthermore, it is possible that living conditions are suboptimal for the walking aids required during rehabilitation.
It is recommended that a hip fracture should be operatively treated within 24 hours [18]. A delay in surgery usually leads to increased morbidity and increases the risk for pressure sores, concomitant infections and thromboembolic events [19]. These factors combined hinder the early mobilisation process, which is crucial in these elderly patients. In our study, a delay of over 48 hours was associated with a trend for increased dislocation. The delays were generally due to operating-room capacity, and in some cases, patient-related factors requiring medical treatment. Poor physical condition prior to hemiarthroplasty may increase the risk of falling and hence dislocation following the procedure. On the other hand, the delay per se usually leads to deterioration in the patient’s physical condition. This result also supports prompt surgical treatment. This study also demonstrated a trend for increased dislocation in patients with prolonged operative time, probably linked to the experience of the operating surgeon or due to technical difficulties encountered during the procedure.
It is noteworthy that the time of day when surgery was performed had no effect on dislocation risk. Furthermore, the dislocation risk was not higher in hemiarthroplasties performed by residents alone. Enocson et al. also found that surgeon experience was not a predisposing factor [6]. In the current study, the residents who performed the hemiarthroplasties unassisted by an orthopaedic surgeon had previously gathered sufficient training and experience with the procedure. It has been shown that excess length of the residual femoral neck following Thompson hemiarthroplasty predisposes to dislocation [7]. Our study found no increased dislocation rate in patients with excess residual femoral neck. This may be explained by the lack of a collar in the stem design used in patients in our study, and therefore, the stem can be placed at a suitable level regardless of femoral-neck resection level. As expected, patients with dislocation had a smaller offset than controls. Also, the centre-edge angle of Wiberg was smaller in patients with dislocation, reflecting mild acetabular dysplasia.
Our study had some limitations. Previous studies show mental dysfunction to be an important risk factor for dislocation [5, 6], which was not confirmed in our study. This result should be interpreted with caution since information regarding mental capacity and alcohol consumption may only be partially accurate; these factors were not quantified using standardised questionnaires. Second, patient coordination and therefore susceptibility to falls could have been tested using coordination and muscle tests. Third, surgeon experience was classified according to educational level rather than on the actual number of hemiarthroplasties performed annually. Finally, an age- and sex-matched control group was not used, as this would have eliminated two possible factors that might influence the dislocation rate. However, age and sex distribution of both groups were similar (Table 1). Strengths of the study are the use of a single prosthesis design and offset, a single standardised surgical approach and a large number of patients from a single centre.
Conclusions
The posterolateral approach resulted in a dislocation rate less than 6%. We believe that this could be further reduced by influencing the risk factors observed in this study. Prompt surgical treatment and fall prevention in the early postoperative period are key factors in treating femoral-neck fractures in elderly patients who undergo hip hemiarthroplasty. Redislocation is a significant problem, and this subgroup of patients should be the main focus of prospective studies.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Gjertsen JE, Vinje T, Engesaeter LB, Lie SA, Havelin LI, Furnes O, Fevang JM. Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Joint Surg Am. 2010;92:619–628. doi: 10.2106/JBJS.H.01750. [DOI] [PubMed] [Google Scholar]
- 2.Iorio R, Schwartz B, Macaulay W, Teeney SM, Healy WL, York S. Surgical treatment of displaced femoral neck fractures in the elderly: A survey of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2006;21:1124–1133. doi: 10.1016/j.arth.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76:15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Petersen MB, Jørgensen HL, Hansen K, Duus BR. Factors affecting postoperative mortality of patients with displace femoral neck fracture. Injury. 2006;37:705–711. doi: 10.1016/j.injury.2006.02.046. [DOI] [PubMed] [Google Scholar]
- 5.Ninh CC, Sethi A, Hatahet M, Les C, Morandi M, Vaidya R. Hip dislocation after modular unipolar hemiarthroplasty. J Arthroplasty. 2009;24:768–774. doi: 10.1016/j.arth.2008.02.019. [DOI] [PubMed] [Google Scholar]
- 6.Enocson A, Tidermark J, Törnkvist H, Lapidus LJ. Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop. 2008;79:211–217. doi: 10.1080/17453670710014996. [DOI] [PubMed] [Google Scholar]
- 7.Pajarinen J, Savolainen V, Tulikoura I, Lindahl J, Hirvensalo E. Factors predisposing to dislocation of the Thompson hemiarthroplasty. Acta Orthop. 2003;74:45–48. doi: 10.1080/00016470310013644. [DOI] [PubMed] [Google Scholar]
- 8.Enocson A, Hedbeck CJ, Törnkvist H, Tidermark J, Lapidus LJ (2011) Unipolar versus bipolar Exeter hip hemiarthroplasty: a prospective cohort study on 830 consecutive hips in patients with femoral neck fractures. Int Orthop. doi:10.1007/s00264-011-1326-3 [DOI] [PMC free article] [PubMed]
- 9.Keene GS, Parker MJ. Hemiarthroplasty of the hip – the anterior or posterior approach ? A comparison of surgical approaches. Injury. 1993;24:611–613. doi: 10.1016/0020-1383(93)90125-P. [DOI] [PubMed] [Google Scholar]
- 10.Bush JB, Wilson MR. Dislocation after hip hemiarthroplasty: anterior versus posterior capsular approach. Orthopedics. 2007;30:138–144. doi: 10.3928/01477447-20070201-05. [DOI] [PubMed] [Google Scholar]
- 11.Suh KT, Park BG, Choi YJ. A posterior approach to primary hip arthroplasty with soft tissue repair. Clin Orthop. 2004;418:162–167. doi: 10.1097/00003086-200401000-00026. [DOI] [PubMed] [Google Scholar]
- 12.Ko CK, Law SW, Chiu KH. Enhanced soft tissue repair using locking loop stich after posterior approach for hip hemiarthroplasty. J Arthroplasty. 2001;16:207–211. doi: 10.1054/arth.2001.20539. [DOI] [PubMed] [Google Scholar]
- 13.Varley J, Parker MJ. Stability of hip hemiarthroplasties. Int Orthop. 2004;28:274–277. doi: 10.1007/s00264-004-0572-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sierra RJ, Schleck CD, Cabanela ME. Dislocation of bipolar hemiarthroplasty: rate, contributing factors, and outcome. Clin Orthop. 2006;442:230–238. doi: 10.1097/01.blo.0000183741.96610.c3. [DOI] [PubMed] [Google Scholar]
- 15.Ramesh M, O’Byrne JM, McCarthy N, Jarvis A, Mahalingham K, Cashman WF. Damage to the superior glutal nerve after the Hardinge approach to the hip. J Bone Joint Surg Br. 1996;78:903–906. doi: 10.1302/0301-620X78B6.1289. [DOI] [PubMed] [Google Scholar]
- 16.Barnes CL, Berry DJ, Sledge CB. Dislocation after bipolar hemiarthroplasty of the hip. J Arthroplasty. 1995;10:667–669. doi: 10.1016/S0883-5403(05)80213-X. [DOI] [PubMed] [Google Scholar]
- 17.Noon AP, Hockings M, Warner JG. Dislocated Thompson hemiarthroplasty - the management of the recurrent dislocator. Injury. 2005;36:618–621. doi: 10.1016/j.injury.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 18.Maggi S, Siviero P, Wetle T, Besdine RW, Saugo M, Crepaldi G. A multicenter survey on profile of care for hip fracture: predictors of mortality and disability. Osteoporos Int. 2010;21:223–231. doi: 10.1007/s00198-009-0936-8. [DOI] [PubMed] [Google Scholar]
- 19.Leung F, Lau TW, Kwan K, Chow SP, Kung AW. Does timing of surgery matter in fragility hip fractures? Osteoporosis Int. 2010;21:S529–S534. doi: 10.1007/s00198-010-1391-2. [DOI] [PMC free article] [PubMed] [Google Scholar]