Abstract
Purpose
This review explores the scientific evidence for clinical, functional and imaging outcomes after surgical management of Femoroacetabular Impingement (FAI) syndrome, and assesses the methodological quality of the published literature reporting this issue.
Methods
The medical literature databases of Pubmed, Medline, Ovid, Google Scholar and Embase were searched for articles published in English, Spanish, French and Italian, using a combination of the keywords ‘femoro-acetabular impingement syndrome’, ‘postoperative outcomes’, ‘open surgery’, and ‘arthroscopic management’. To address three main questions, we extracted data on demographic features, operative techniques, postoperative rehabilitation regimens, imaging features, pre and postoperative hip scores. Complications and conversion to arthroplasty were also investigated.
Results
Thirty-one studies published have reported clinical, functional and imaging outcomes after open and arthroscopic management of FAI syndrome. The modified Coleman methodology score (CMS) averaged 56.2 (range, 30–81). From extracted data, it was shown that arthroscopy, open surgery and arthroscopic surgery followed by mini open surgery are comparable for functional results, biomechanics, and return to sport. Progression of OA and conversion to hip arthroplasty are dependent on preoperative status of cartilage and osteoarthritis and type of management. Debridement and osteoplasty provide better results than debridement only. Significantly improved outcomes have been recorded in patients undergoing labral refixation than resection. The Coleman methodology score showed great heterogeneity in terms of study design and outcome assessment, and generally low methodological quality.
Conclusion
Although open and minimally invasive procedures allow athletes to return to professional sports activity, they are contraindicated in patients with severe osteoarthritis and cartilage degeneration.
Keywords: Medicine & Public Health, Orthopedics
Introduction
Femoroacetabular impingement syndrome (FAI) is the first cause of pain and discomfort in young active non-dysplastic patients [1, 2]. Two types of impingement, pincer and cam, respectively arising from an abnormal morphology of the femur and acetabulum, alter the biomechanics of the hip, and result in limited and painful range of motion, mostly in flexion and internal rotation. A minority (14%) presents pure femoroacetabular impingement, and most patients (86%) have a combination of both forms, the so called “mixed pincer and cam impingement”. The spectrum of abnormalities of the femur and acetabulum have been widely described [1, 3], but the knowledge about the long-term effects of this pathology is still scanty, and available studies, with short follow-ups, partially clarify this concern. In the short term, these abnormal configurations may become painful and symptomatic, impair functional and athletic performance, and induce young athletes to change level and/or type of sport, or even to retire early from sport activity. As cartilage damage and early osteoarthrosis may be developed [1, 4], early diagnosis and treatment are needed. In pincer impingement, common in dysplastic patients [5], the chronic abnormal loading of the acetabular rim (pincer-effect) results in early labral injury and long-term degenerative changes [6, 7] whereas in cam impingement, more frequent in non-dysplastic hips, the long-term evolution arises from an abnormal contact of the femoral neck against the acetabular rim (cam-effect). At present, the best line of management is still controversial, and there is no consensus on the efficacy of treatment. Hip dislocation and open osteochondroplasty have been the standard in the past [1], but favourable outcomes and reduced postoperative complications are increasingly observed in patients undergoing less invasive arthroscopic procedures [8, 9]. These emergent techniques avoid the trauma typically related to open procedures, and spare the soft tissues, with a complication rate less than 1.5%. We reviewed systematically the relevant evidence published on clinical and functional effects of open, arthroscopic, and combined mini-open and arthroscopic procedures for management of FAI syndrome. We wish to address the question of whether surgical treatment for FAI improves symptoms and functional outcomes and what is the standard surgical procedure.
As many systematic reviews have been published on this issue in the last year, we assessed the methodological quality of these papers using a validated and reliable scoring system, the modified Coleman methodology score (CMS) [10–17].
Methods
Search and study selection
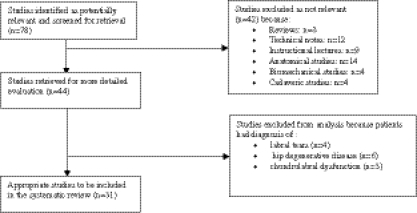
We searched for relevant studies published in Pubmed, Medline, Ovid, Google Scholar and Embase databases using the combined keywords ‘femoro-acetabular impingement syndrome’, ‘postoperative outcomes’, ‘open surgery’, and ‘arthroscopic management’, with no limit for year of publication. We included studies in English, Spanish, French and Italian, published in peer-reviewed journals, reporting data on clinical, functional and imaging outcomes of patients with femoroacetabular impingement syndrome who had undergone arthroscopic or open surgery. Biomechanical reports, studies on animals, cadavers, in vitro or animal studies, case reports, literature reviews, technical notes, letters to editors, and instructional courses were also excluded. Two authors (RP and ADB) independently assessed the abstract of each publication, selecting on the basis of its content, and excluding papers without abstract available. When the inclusion or exclusion were not possible from the abstract, we downloaded the full-text versions. The reference lists of the selected articles were fully reviewed by hand to identify articles not included at the first electronic search. Figure 1 summarises the significant steps of our search and explains the reasons for exclusion. Considering all the journals, we first identified the abstracts of 74 articles, but we downloaded the full text of 40, because they described the outcomes of patients who had undergone open and arthroscopic surgery. All the authors retrieved, reviewed, and discussed all the 40 articles, excluding 12 studies because they reported outcomes of patients without a defined diagnosis of FAI, and tested biomechanical and imaging methods of assessment. At the end of the study selection process, 31 relevant publications were included.
Fig. 1.
Schematics of inclusion and exclusion of studies
Quality assessment
Two investigators (RP and ADB) selected the studies, and separately evaluated the methodological quality of each article twice with the Coleman methodology score (CMS) [10]. The CMS is a ten-criteria scoring list with a final score from 0 to 100 (Table 1), which is a perfect score representing a study design that largely avoids the influence of chance, various biases, and confounding factors. The two investigators discussed scores where more than a two point difference was evident, until consensus was reached.
Table 1.
Coleman methodology scores and criteria
| Section score (maximum score) | Mean | Standard deviation | Range | Median |
|---|---|---|---|---|
| Part A | ||||
| Study size (10) | 5.5 | 3.8 | 0–10 | 4 |
| Mean duration of follow-up (10) | 3.5 | 1.8 | 0-5 | 5 |
| No. of surgical procedures (10) | 7.0 | 3.7 | 0–10 | 10 |
| Type of study (15) | 0.4 | 2.0 | 0–10 | 0 |
| Diagnostic certainty (5) | 4.4 | 1.0 | 2–5 | 5 |
| Description of surgical procedure (5) | 4.1 | 1.5 | 0–5 | 5 |
| Description of postoperative rehabilitation (10) | 5.1 | 3.6 | 0–10 | 6.5 |
| Part B | ||||
| Outcome measures (10) | 7.5 | 1.7 | 3–10 | 7 |
| Outcome assessment (15) | 8.8 | 1.5 | 5–12 | 9 |
| Selection process (15) | 9.8 | 2.4 | 4–15 | 10 |
| Total score (100) | 56.04 | 8.2 | 46–81 | 56 |
Data extraction
The data were extracted from each study included in our investigation, without contacting the author(s) to verify the accuracy of the extracted data and obtain further information. Extracted data, assessed by using different scales, allowed quantification of the postoperative good–excellent clinical results, the real entity of the improvement after surgery. Instrumental diagnostic methods (radiographs, MRI and CT) and classification radiographic systems were taken in account to report about imaging outcomes and, eventually, postoperative hip joint degenerative changes. We also extracted preoperative and postoperative alpha angle values to define whether impingement deformities had been biomechanically corrected.
Merle D’Aubignè hip scores [3, 18] ranging from 15 to 18 points and Harris hip rates higher than 80 points [19] were considered as good or excellent outcomes. Furthermore, rates of complications and conversion to arthroplasty were helpful to investigate safety, effectiveness, and reliability of both open and arthroscopic procedures. The intra-class correlation coefficient was calculated to quantify the agreement between the Coleman scores of the two independent assessors. Spearman correlation was used to assess correlation between the year of publication and the Coleman score. Correlation was calculated between Coleman score and good–excellent reported rates. Analysis was performed using SPSS software (version 16.0, Chicago, Illinois).
Results
Since 2004, 31 relevant studies have reported on clinical and imaging outcomes after open and arthroscopic hip surgery for femoroacetabular impingement. The total number of patients included in the various studies was 1713, with 1141 (67%) males and 562 (33%) females, and the numbers varied from five [20] to 200 [21]. Patients were operated upon at an average age ranging from 19.7 [22] to 47.3 years [23], after an average period from one month [24] to ten years [25] from the onset of symptoms. Based on extracted data, “cam type” impingement was found in 901 hips (57.9%), “pincer type” in 74 (4.8%), and “combined cam pincer” in 580 (37.3%). In total, 1230 patients underwent arthroscopy, 229 underwent open surgery, and 254 received arthroscopy followed by the open anterior approach.
Preoperative assessment
Standardised conventional antero-posterior pelvic and lateral cross-table radiographs supported the first clinical suspicion of FAI disease in almost all studies. In the scenario of FAI syndrome, if magnetic resonance with gadolinium arthrography is the standard to assess type of impingement, status and extent of labral and cartilage lesions [18–20, 26–33], thee-dimensional computed tomography reconstruction is used to map the bony architecture of suspected areas [19, 21, 25, 27, 29, 31, 34]. Ten [18, 20, 29, 35–37] studies reported on open surgical decompression, 18 studies [9, 19, 21, 23–28, 30, 34, 38–41] on arthroscopy, and three on arthroscopy followed by open anterior femoral osteoplasty [31–33]. Debridement and microfractures of cartilage lesions were made in 14 studies [9, 19, 23, 24, 27–30, 35, 38, 41, 42], a large femoral neck cyst was excised in one patient [26], and interthrocanteric and periacetabular osteotomy were carried out in seven patients [43]. The description of the postoperative rehabilitation program scored 6 points or more in 19 studies (59.3%) and 0 in four studies. Twenty-one of the 27 selected (78%) studies reported a satisfactory description of subject selection criteria and 25 (93%) used validated scoring systems with good reliability and sensitivity. The “outcome assessment” section scored adequately in 20 articles (64.5%). Seventeen studies [9, 19, 21, 24, 26, 32–34, 36–40, 42] used the modified Harris hip score, four studies the Merle d’Aubignè scale [3, 18, 25, 43], and five studies the WOMAC Index score [25, 27, 29, 30, 41]. The non arthritic hip score (NAHS) was used in four studies [9, 23, 28, 33], the hip outcome score was administered in two studies [22, 44], while VAS rating [26] and combined VAS and SF-12 criteria [19] were used in one study each. The average Coleman methodology scores for each item are given in Table 1, whereas the CMS of each article is listed in Table 2. Finally, five studies [20, 24, 35] rated outcomes in terms of return to sport activity and return to preoperative range of movement (internal and external rotation) (Table 3). The average modified Coleman methodology score was 56.2 (range from 30 [5] to 81.0 [28, 38]). The inter-class correlation coefficient of 0.73 showed a high correlation between the Coleman methodology scores awarded to each scientific article by each independent marker.
Table 2.
Sample data
| Study | Date of publication | Sample size | Sample mean age (years) | Sex ratio (M:F) | Mean follow-up (months) | Management | Coleman score (CMS) |
|---|---|---|---|---|---|---|---|
| Bardakos et al. [39] | 2008 | 71 | 34.3 | 1.09 | NA | Arthroscopy | 56 |
| Beaulé et al. [29] | 2007 | 34 | 40.5 | 1.1 | 37.2 | Open surgery | 60 |
| Beck et al. [3] | 2004 | 19 | 36 | 2.8 | 56.4 | Open surgery | 61 |
| Bedi et al. [5] | 2011 | 10 | 25.9 | NA | 10.9 | Arthroscopy | 30 |
| Bizzini et al. [20] | 2007 | 5 | 21.4 | 5 | 32.4 | Open surgery | 55 |
| Byrd and Jones [21] | 2009 | 200 | 33.4 | 2.2 | 16 | Arthroscopy | 64 |
| Byrd and Jones [40] | 2009 | 26 | 46 | 1 | 120 | Arthroscopy | 49 |
| Clohisy et al. [48] | 2010 | 35 | 34 | 4 | 26.4 | Arthroscopy and open anterior approach | 53 |
| Espinosa et al. [18] | 2006 | 52 | 30 | 1.7 | 96 | Open surgery | 48 |
| Gedouin et al. [25] | 2010 | 110 | 31 | 2.4 | 10 | Arthroscopy | 53 |
| Gedouin et al. [41] | 2010 | 38 | 36 | 6.6 | 15.6 | Arthroscopy | 59 |
| Hartmann and Gunther [26] | 2009 | 33 | 31 | 1.06 | 15 | Arthroscopy | 60 |
| Haviv et al. [9] | 2010 | 166 | 37 | 3.9 | 22 | Arthroscopy | 73 |
| Haviv and O’Donnell [45] | 2010 | 82 | 29 | 4.5 | 26 | Arthroscopy | 67 |
| Horisberg et al. [28] | 2010 | 88 | 40.9 | 2.1 | 27.6 | Arthroscopy | 72 |
| Horisberg et al. [23] | 2010 | 20 | 47.3 | 4.0 | 36 | Arthroscopy | 49 |
| Ilizaliturri et al. [27] | 2007 | 13 | 30.6 | 1.2 | 30 | Arthroscopy | 43 |
| Ilizaliturri et al. [30] | 2008 | 19 | 34 | 1.4 | NA | Arthroscopy | 52 |
| Larson and Giveans [19] | 2008 | 96 | 34.7 | 1.3 | 9.9 | Arthroscopy | 59 |
| Larson and Giveans [34] | 2009 | 71 | 28.9 | 2.1 | 18.8 | Arthroscopy | 57 |
| Laude et al. [31] | 2009 | 91 | 33.4 | 1.1 | 58.3 | Arthroscopy and open anterior approach | 64 |
| Lincoln et al. [32] | 2009 | 14 | 37 | 2.5 | 24 | Arthroscopy and open anterior approach | 55 |
| Murphy et al. [43] | 2004 | 23 | 35.4 | 1.3 | 62.4 | Open surgery | 53 |
| Naal et al. [22] | 2011 | 22 | 19.7 | 22 | 45.1 | Open surgery | 57 |
| Nho et al. [44] | 2011 | 47 | 22.8 | 2.6 | 27 | Arthroscopy | 71 |
| Peters and Erickson [42] | 2006 | 29 | NA | 1.2 | 96 | Open surgery | 56 |
| Peters et al. [37] | 2010 | 94 | 28 | 1.4 | 26 | Open surgery | 59 |
| Philippon et al. [35] | 2007 | 45 | 31 | 14 | 19.2 | Open surgery | 46 |
| Philippon et al. [38] | 2009 | 112 | 40.6 | 1.24 | 27.6 | Arthroscopy | 81 |
| Philippon et al. [24] | 2010 | 28 | 27 | 28 | 24 | Arthroscopy | 56 |
| Yun et al. [36] | 2009 | 14 | 35.8 | 6 | 27.6 | Open surgery | 49 |
Table 3.
Success rate
| Author | Rate of success | Conversion to hip arthroplasty | Factors predisposing to hip arthroplasty |
|---|---|---|---|
| Bardakos et al. [39] | 59% in control group vs 83% in study group according to Harris hip score | – | |
| Beaulé et al. [29] | NA | – | |
| Beck et al. [3] | 54.2% had excellent good scores according to Merle d'Aubignè hip score | 5 patients (26.3%) open | Preoperative osteoarthritis, 1 with untreated ossified labrum |
| Bedi et al. [5] | – | ||
| Bizzini et al. [20] | 60% | – | |
| Byrd and Jones [21] | NA | 1 patient (0.5%) arthroscopy | Extensive grade IV acetabular and femoral cartilage lesions |
| Byrd and Jones [40] | NA | 8 patients (30.8%) arthroscopy | Preoperative osteoarthritis |
| Clohisy et al. [33] | 71% had excellent good scores according to Harris hip score | – | |
| Espinosa et al. [18] | 85% according to Merle d'Aubignè hip | – | |
| Gedouin et al. [25] | 77% overall satisfaction rate | 5 (4.5%) arthroscopy | Preoperative osteoarthritis |
| Gedouin et al. [41] | 79% overall satisfaction rate | – | |
| Hartmann and Gunther [26] | 78.8% | – | |
| Haviv et al. [9] | NA | – | |
| Haviv and O’Donnell [45] | – | ||
| Horisberg et al. [28] | NA | 9 hips (9%) arthroscopy | Five with preoperative Tonnis grade II and four with Tonnis grade I; grade 3 osteochondral lesion in four hips and five with grade 2. No difference in terms of alpha values |
| Horisberg et al. [23] | NA | 8 hips (40%) arthroscopy | Tonnis grades I-II osteoarthritis and marked advanced cartilage deterioration |
| Ilizaliturri et al. [27] | NA | ||
| Ilizaliturri et al. [30] | NA | 1 patient (5.3%) arthroscopy | Advanced osteoarthritis |
| Larson and Giveans [19] | 74.5% | ||
| Larson and Giveans [34] | 66.7% in debridement group vs 89.7% in refixed group according to Harris hip score | 1 patient (1.4%) arthroscopy | |
| Laude et al. [31] | NA | 9 patients (9.9%) arthroscopy and open anterior approach | Deep acetabular lesions (10.9 mm ), Beck grade 5 cartilage lesion and older age (40.3 years) |
| Lincoln et al. [32] | NA | 1 patient (7.1%) arthroscopy and open anterior approach | Tonnis grade II and a large (> 2 cm) chondral flap |
| Murphy et al. [43] | NA | – | |
| Naal et al. [22] | 86.4% | – | |
| Nho et al. [44] | NA | – | |
| Peters and Erickson [42] | NA | 3 patients (10.3%) open surgery | Progressive arthrosis; Outerbridge grade IV cartilage lesion of the acetabulum |
| Peters et al. [37] | NA | 5 patients (5.3%) open surgery | Four with severe acetabular articular cartilage delamination (Outerbridge Grade IV) and one with slipped capital femoral epiphysis |
| Philippon et al. [35] | 93% returned to sport activity | – | |
| Philippon et al. [38] | NA | 10 patients (8.9%) | Older age at the time of arthroscopy (58 vs 39 years, p = 0.001), significantly less joint space on all three weightbearing surfaces on their preoperative radiographs (p = 0.001), significantly lower mean preoperative modified HHS (47 vs 60, p = 0.026). Cartilage changes. Patients with microfracture on both the femoral head and the acetabulum were also more likely to undergo a THR (p = 0.001) |
| Philippon et al. [24] | 100% returned to sport activity | – | |
| Yun et al. [36] | NA | – |
The CMSs show no evidence of a statistically significant association with the publication year (r = 0.3; p = 0.23), demonstrating that more recent scientific articles did not score better than older studies.
Clinical outcomes
Methods of assessment and relative values have been reported in detail in Table 4. One hundred forty-two of 181 (78.5%) arthroscopically managed patients [19, 34, 39] and 135 of 169 patients (80%) [3, 18, 20, 33, 35] undergoing open surgical dislocation and hip decompression reported good or excellent results. As reported in Table 5, in all studies postoperative scores were significantly improved compared to preoperative scores, regardless of the procedure performed. Mean improvement in modified HHS score after surgery was 24 for arthroscopy, 19.7 for open surgical dislocation, and 19.1 for the combined approach. With regard to arthroscopy, combined debridement and osteoplasty provide better, though not significant, outcomes than debridement only [39]. When performing arthroscopic femoral osteoplasty for treatment of cam FAI, additional microfracturing for grades III/IV cartilage lesions does not change outcomes [21]. A recent study on patients undergoing bilateral arthroscopy for bilateral cam type impingement has shown that there is no significant difference in outcomes between patients with bilateral and unilateral hip pain at presentation, with higher improvement after their second operation than the first [45].
Table 4.
Preoperative and postoperative outcome scores
| Author | Surgery | Score | Preoperative | Postoperative | p value |
|---|---|---|---|---|---|
| Bardakos et al. [39] | Arthroscopy | Modified Harris hip score | Control group 55 (37–72) | Control group 77 (59–87) | 0.11 (NS, intergroup difference) |
| Study group 59 (52–64) | Study group 83 (75–87) | ||||
| Beaulé et al. [29] | Open surgery | WOMAC score | 61.2 ±20 | 81.4 ± 16 | < 0.001 |
| Beck et al. [3] | Open surgery | Merle d’Aubignè score | 14.1 | 16.5 | 0.015 |
| Bedi et al. [5] | Arthroscopy | Modified Harris hip score | 65.9 | 89.1 | |
| Bizzini et al. [20] | Open surgery | NA | |||
| Byrd and Jones [21] | Arthroscopy | Modified Harris hip score | |||
| Byrd and Jones [40] | Arthroscopy | Modified Harris hip score | 52 | 81 | < 0.001 |
| Clohisy et al. [48] | Arthroscopy and Open anterior | Modified Harris hip score | 63.8 (35–85) | 87.9 (54–100) | <0.0001 |
| Espinosa et al. [18] | Open surgery | Merle d’Aubignè score | Gr 1: 12 (8–13) | Gr 1: 15 (10–18) | 0.0009 |
| Gr 2: 12 (5–16) | Gr 2: 17 (13–18) | <0.0001 | |||
| 0.01: Intergroup difference | |||||
| Gedouin et al. [25] | Arthroscopy | WOMAC score | 60.3 (32–96) | 83 (37–100) | < 0.001 |
| Gedouin et al. [41] | Arthroscopy | Merle d’Aubignè score | 14.6 (11–18) | 17.2 (12–18) | < 0.001 |
| Hartmann and Gunther [26] | Arthroscopy | Modified Harris hip score | 63.9 | 85.1 | < 0.001 |
| (31–83) | (64–100) | ||||
| Haviv et al. [9] | Arthroscopy | Modified Harris hip score | 70.7 (26–100) | 86.1 (36–100) | < 0.001 |
| Haviv and O’Donnell [45] | Arthroscopy | Modified Harris hip score | Gr 1: 77 | Gr 1: 94 | |
| Gr 2: 67 | Gr 2: 93 | ||||
| Horisberg et al. [28] | Arthroscopy | Non Arthritic hip score (NAHS) | 56.8 (15–92.5) | 84.6.(47.5–100) | < 0.001 |
| Horisberg et al. [23] | Arthroscopy | Non Arthritic hip score (NAHS) | 47.15 (23.75–66.25) | 78.3(63.75–95.0) | 0.004 |
| Ilizaliturri et al. [27] | Arthroscopy | WOMAC score | 77.7 (74–82) | 87.4 (80–94) | 0.0001 |
| Ilizaliturri et al. [30] | Arthroscopy | WOMAC score | NA | NA | |
| Larson and Giveans [19] | Arthroscopy | Modified Harris hip score | 60.8 | 82.7 | < 0.001 |
| Larson and Giveans [34] | Arthroscopy | Modified Harris hip score | NA | NA | < 0.01 intergroup difference |
| Laude et al. [31] | Arthroscopy and Open anterior approach | Non arthritic hip score (NAHS) | 54.8 ± 12 | 83.9 ± 16 | <0.000001 no difference (p = 0.13) at the last follow-up between patients with refixation (86 ± 11) and without refixation (82 ± 19) |
| Lincoln et al. [32] | Arthroscopy and Open anterior approach | Modified Harris hip score | 63.8 ± 5.1 | 76.1 ± 4.8 | 0.01 |
| Murphy et al. [43] | Open surgery | Merle d’Aubignè score | 13.2 (11–15) | 16.9 (13–18) | < 0.001 |
| Naal et al. [22] | Open surgery | Hip outcome score | 94.5 (activity of daily living subscale) | ||
| 89.1 (sport subscale) | |||||
| Nho et al. [44] | Arthroscopy | Modified Harris hip score | 68.6 | 88.5 | 0.002 |
| Peters and Erickson [42] | Open surgery | Modified Harris hip score | 70 | 87 | < 0.0001 |
| Peters et al. [37] | Open surgery | Modified Harris hip score | 67 (43–87) | 91 (48–100) | < 0.0001 |
| Philippon et al. [35] | Open surgery | NA | NA | NA | NA |
| Philippon et al. [38] | Arthroscopy | Modified Harris hip score | 58 | 84.3 | |
| Philippon et al. [24] | Arthroscopy | Modified Harris hip score | 70 (57–100) | 95 (74–100) | 0.001 |
| Yun et al. [36] | Open surgery | Modified Harris hip score | 76 (72–81) | 93 (87–98) | NA |
NA not available
Table 5.
Type of management and outcome improvement
| Variable | Arthroscopy | Open surgery | Combined arthroscopy and mini open approach |
|---|---|---|---|
| mHHS | |||
| Articles | 10 | 4 | 3 |
| Mean preoperative score | 64.1 | 71 | 63,9 |
| Mean postoperative score | 88.1 | 90.7 | 83 |
| Mean improvement | 24 | 19.7 | 19,1 |
| WOMAC | |||
| Articles | 4 | 1 | – |
| Mean preoperative score | 68.75 | 61.2 | – |
| Mean postoperative score | 83.6 | 81.4 | – |
| Mean improvement | 14.85 | 20.2 | – |
| Merle D’Abignè Score | |||
| Articles | 1 | 2 | |
| Mean preoperative score | 14.6 | 12.6 | |
| Mean postoperative score | 17.2 | 16.5 | |
| Mean improvement | 2.6 | 2.9 | |
| NAHS | |||
| Articles | 2 | – | 1 |
| Preop | 52 | 75.1 | |
| Postoperative score (mean) | 81.5 | 90.2 | |
| Mean improvement | 29.5 | 15.1 | |
With regard to management of labral tears, labral re-fixation provides significantly higher scores than debridement alone (p < .0.01), with higher success rates (94%) after open acetabular trimming and femoral osteochondroplasty [18] than arthroscopic procedure [34] (89.7%). While debridement alone improves pain score two years after surgery, labral repair relieves symptoms at one year. In arthroscopy, labral repair provides higher modified Harris hip scores than labral debridement alone, with no significant difference (87 vs 81, p = 0.10) [38] (Table 4). From a multivariable analysis, preoperative score, joint space narrowing ≥ 2 mm, and labral repair rather than debridement are predictors of higher postoperative scores [38].
Range of motion and biomechanics
Arthroscopy significantly improves hip flexion, from 111.2° at baseline to 119.9° postoperatively, and internal rotation at 90° of hip flexion, from 11.5° to 23.9°. After arthroscopy and open surgery, hip flexion improved from 94.1° to 110° and internal rotation from 7.1° to 12.3°. Concerning open approach we did not find any data.
Biomechanically, alpha angle decreased from a mean of 72.9 to a mean of 48.8 after arthroscopy, from an average value of 69.3 to an average value of 43.4 after open surgical decompression, and from a mean of 64.5 to 43.3 for patients who had undergone arthroscopy followed by a mini open anterior approach. Biomechanically, by comparing these procedures, we found no significant differences.
Return to sport activity
Among five ice hockey players undergoing open surgical decompression for FAI syndrome, three athletes were fully reintegrated in the team and two played for farm teams [20]. In another study including 45 patients managed by open surgical decompression, of 42 (93%) athletes who had returned to professional sport activity, 35 (78%) were still active at a professional level at an average 1.6-year follow-up. Of five patients requiring a further operation, three benefitted from arthrolysis of the adhesions and returned to professional play, whereas two retired because of signs and symptoms of osteoarthritis [35]. At a mean of 45.1 months from open dislocation for combined impingement, 21 of 22 patients (95.5%) still competed professionally, one gave up his career and participated in recreational sports only. Nineteen of these 21 patients (90.5%) maintained their pre-symptomatic level, and two were active in minor leagues but still played professionally. Nineteen patients (86.4%) were satisfied with their sports ability. Thirteen patients (59.1%) had improved their sports ability; six (27.2%) indicated no change; and three (13.6%) experienced a deterioration [22]. Philippon et al. [24] reported on return to sports activity after arthroscopy in 28 professional hockey players, all of them returned to skating/hockey drills at an average period of 3.8 months (range, one to five) from the operation, playing an average number of 94 NHL games (range, 3–252). Two players required another hip arthroscopy after a new injury. The time to return to play was not associated with age (p = 0.4), preoperative (p =0.1) and postoperative scores (p = 0.2), or time from injury to surgery (p = 0.8). Age was negatively related to the number of games played (r = −0.48; p = 0.009), whereas time from injury to surgery influenced significantly the time to return to play, i.e. players who received surgery within one year from the time of injury returned to sport earlier than patients who waited more than one year. Indeed, time from injury to surgery had no relationship with pre- or postoperative Harris hip scores. As shown by Nho et al., 79% of patients returned to play at a mean of 9.4 months (range, four to 26 months) from arthroscopy. Almost all these patients achieved the same level of competition and were still active at two years [44].
Radiographic classification, hip osteoarthritis and conversion to total hip arthroplasty
Radiographic features of degenerative joint disease changes were classified according to the Tonnis grading system [46] in 18/31 (58.1%) studies [3, 18, 19, 23, 25, 28, 31–35, 41–43], to the Kellgren Lawrence classification [47] in one study [26] and non specifically in two studies [30, 40]. On the other hand, articular cartilages have been assessed intraoperatively in 19 studies, according to the Outerbridge and Beck classifications. From extracted data, progression of OA and conversion to hip arthroplasty depend on preoperative status of cartilage and osteoarthritis, and type of management. Although microfractures for high grade cartilage lesions relieve symptoms and improve hip function in the short term [3], these patients may deteriorate over time, with clinical and imaging progression of OA, or even the need for hip arthroplasty [42]. The progressive development of arthritis, often symptomatic, may result in significantly worse outcomes than those observed in patients with an history of trauma, in the absence of arthritic changes [40]. However, surgery improves baseline symptoms [41].
As reported by Horisberg et al. [23], patients with preoperative severe degenerative changes (higher Tönnis grades), regardless of cartilage grade degeneration, are more likely to worsening in hip scores, pain and range of motion, and to undergo total hip arthroplasty (p = 0.03). Labral resection and labral repair result in significant radiographic differences. After resection, the average Tonnis grade changed from 0.6 at baseline to 1.2 at one year, and 1.3 at two years. On the other hand, once the labrum had been reattached, Tonnis grade did not change at one year (0.5) and increased to 0.8 after two years [18].
Late complications
As reported in Table 6, heterotopic ossification is the most frequent complication [19, 21, 29, 31, 34, 48]. Many patients underwent a new arthroscopy in the index hip for persistent symptoms, further debridement, lysis of adhesions, management of mechanical symptoms, inadequate decompression, and advanced osteoarthritis [21]. A few patients had neurapraxia of the sciatic, pudendal, and lateral femoral cutaneous nerves [19, 21, 34, 40]. All these patients recovered within a few months.
Table 6.
Postoperative complications
| Author | Surgery | Postoperative complication |
|---|---|---|
| Bardakos et al. [39] | Arthroscopy | – |
| Beaulé et al. [29] | Open surgery | One patient had failed trochanteric fixation; 1 patient had Brooker grade IV heterotopic ossification; 9 hips persistent bursitis; 6 patients had unsatisfactory outcomes cartilage damage |
| Beck et al. [3] | Open surgery | |
| Bedi et al. [5] | Arthroscopy | |
| Bizzini et al. [20] | Open surgery | |
| Byrd and Jones [21] | Arthroscopy | Three patients underwent new arthroscopy for mechanical symptoms; 1 neuroapraxia of pudendal nerve; 1 partial neuroapraxia of lateral femoral cutaneous; 1 heterotopic ossification |
| Byrd and Jones [40] | Arthroscopy | – |
| Clohisy et al. [48] | Arthroscopy and open anterior | One superficial infection; 1 deep vein thrombosis (in the popliteal vein proximal to the calf); asymptomatic Brooker grade-I heterotopic ossification in 4 hips |
| Espinosa et al. [18] | Open surgery | – |
| Gedouin et al. [25] | Arthroscopy | Three patients developed ectopic ossification; 1 patient showed femoral neurapraxia; 1 pudendal neurapraxia and 1 labium majus skin necrosis; 1 patient had a non-displaced stress fracture of the femoral head/neck junction |
| Gedouin et al. [41] | Arthroscopy | – |
| Hartmann and Gunther [26] | Arthroscopy | – |
| Haviv et al. [9] | Arthroscopy | Ten patients underwent re-operation because of persistent symptoms |
| Haviv and O’Donnell [45] | Arthroscopy | Eight patients underwent reoperation because of persistent symptoms at a mean interval of 33.8 months from the second operation. Of these, 6 were on the first operated side and 2 on the second (contralateral) side |
| Horisberg et al. [28] | Arthroscopy | 12 hips (11%): Dysesthesia/hypesthesia of pudendal and lateral cutaneous femoral nerves in 9, sciatic nerve neurapraxia with hypesthesia of the instep region in 2, a superficial tear of labia minora |
| Horisberg et al. [23] | Arthroscopy | Two cases (10%) of temporal hypesthesia in the area of nervus cutaneus femoris lateralis |
| Ilizaliturri et al. [27] | Arthroscopy | – |
| Ilizaliturri et al. [30] | Arthroscopy | – |
| Larson and Giveans [19] | Arthroscopy | One partial sciatic nerve neurapraxia; 6 hips (6%) had heterotopic bone formation |
| Larson and Giveans [34] | Arthroscopy | Four hips (11.1%) in gr 1, and 3 hips (7.7%) in gr 2; 3 patients heterotopic ossification in gr 1 and 0 in gr 2; 2 revision femoral osteochondroplasty for inadequate initial decompression in gr 1; 1 failure of labral anchor suture in 1 patient in gr 2 |
| Laude et al. [31] | Arthroscopy and open anterior approach | One femoral neck fracture; 2 deep infection treated with surgical debridement and antibiotics; 1 revision for heterotopic ossification |
| Lincoln et al. [32] | Arthroscopy and open anterior approach | One had transient anesthesia in the perineum (hip distraction), 6 had transient anesthesia in the proximal lateral area of innervation of the lateral femoral cutaneous nerve |
| Murphy et al. [43] | Open surgery | Three early failures: 1 had circumferential osteophyte formation, 2 untreated acetabular dysplasia |
| Naal et al. [22] | Open surgery | – |
| Nho et al. [44] | Arthroscopy | – |
| Peters and Erickson [42] | Open surgery | Four hips (13%) were considered as failure because of pain and or progressive arthrosis |
| Peters et al. [37] | Open surgery | Two complications related to fixation of the greater trochanter: one early failure of fixation due to failure to acquire cortical screw purchase distally in a female patient and one nonunion in a male patient |
| Philippon et al. [35] | Open surgery | Five patients required reoperation: 3 underwent lysis of adhesions and 2 had symptomatic treatment of extensive OA |
| Philippon et al. [38] | Arthroscopy | – |
| Philippon et al. [24] | Arthroscopy | – |
| Yun et al. [36] | Open surgery | Three cases of nonunion of the trochanteric osteotomy site, which were treated with internal fixation using a trochanteric plate |
After arthroscopic management, some patients had traction related complications, such as nerve numbness, nerve palsies, dysesthesia, and transient anesthesia. All resolved within a few months.
Discussion
Over the years, increasingly sophisticated imaging techniques have allowed better definition of FAI syndrome, which was otherwise unknown until a few decades ago. In the literature, the pathological, anatomical, imaging and surgical aspects of pincer and cam types have been widely investigated [49], but knowledge about the long-term evolution of this disease is scanty. The trend to prefer conservative measures, reserving surgery to symptomatic patients [50, 51], pushes us to clarify the best management and the role of surgery in management of FAI syndrome. Surgery not only relieves symptoms and encourages the return to sport activity, but also improves prognosis of concomitant and pre-existing degenerative joint disease [20, 35]. Pooling the data from several studies [9, 35, 52–54], open labral debridement and osteoplasty have been recognised as successful procedures, with highly satisfactory and favourable Harris hip and Merle d’Aubignè scores [3, 18, 29, 42, 43], whereas arthroscopy is less traumatic for soft tissues and more encouraging in terms of rapid recovery and return to sport activity [35, 55], allowing 93% of patients to return to their pre-injury sport and 78% to remain active at the last follow-up [35]. Arthroscopy is more technically demanding, and anterolateral and anterior portals are close to the femoral neurovascular bundle [56]. In a recent study on 37 subjects undergoing revision arthroscopy for persistence of groin pain, findings of FAI were still evident at imaging and surgery, probably because they were not or were inadequately addressed at the index surgery [8]. This demonstrates that checking the head sphericity after osteochondroplasty may be problematic [31], especially in the early stages of the learning curve, when some arthroscopic osteochondroplasty procedures may be incomplete. Therefore, at the beginning of this practice, fluoroscopic control and specially-designed spherometer gauges can be helpful to improve femoral assessment and favour an adequate osteochondroplasty. In cam type impingement, a combined arthroscopic and modified open approach could improve the quality of the osteoplasty of femoral head and neck [33].
In pincer impingement, debridement only is appropriate to manage degenerative changes in the over-coverage region of the labrum [32], but an additional labral refixation, when indicated, provides earlier recovery and superior clinical and radiographic outcomes compared to labral excision [18, 19, 31, 39]. Open acetabular trimming and femoral osteochondroplasty [18] seem to provide success rates higher than those observed after arthroscopic procedures [34], but we could not compare the data given the heterogeneity of the scores. However, as evident from the extracted data, arthroscopy, open surgery and arthroscopic followed by mini open surgery are comparable for functional results (Table 5), biomechanics, and return to sport [56]. According to available data, we can not state if surgery modifies the evolution of osteoarthritis in young patients and contributes to prevent the development of OA. Few methods have been used to assess pre-existing osteoarthritis and cartilage status, allowing determination of homogeneity in study findings. Postoperative failure and subsequent conversion to total hip arthroplasty are influenced by preoperative clinical and imaging findings [56]. Open dislocation and debridement show a higher rate of conversion to total hip arthroplasty, particularly in patients with pre-existing severe osteoarthritis and cartilage lesions [3, 23, 37, 43]. Concomitant cartilage lesions and degenerative changes result in lower clinical and functional scores [9], short-term pain relief, no evidence of long-term satisfactory outcomes, higher failure rate, and even conversion to total hip arthroplasty [23]. However, almost all information on cartilage status have been extracted from studies in which arthroscopy was performed. Young patients are the best candidates. Though providing high return to professional sport activity level [24, 35], there is no evidence to propose a surgical procedure to patients with concomitant advanced osteoarthrosis and cartilage deterioration [23].
Conclusions and perspectives for the future
Most studies of level III-IV of evidence include small numbers of participants and, importantly, have limited long-term follow-ups. Therefore, randomised trials should be the next logical step for research in this field. We are unable to draw any definitive conclusions about which management is most effective because the long-term consequences of residual bony impingement and secondary degeneration usually appear at mid- and long-term assessments. From the published studies, it appears that these three procedures are grossly equivalent, but more data focusing on preoperative cartilage status and type of impingement are essential. Given the present state of the art on this particular issue, we cannot draw any definitive evidence-based conclusions on the best surgery for management of FAI. Apart from assessing preoperative status of cartilage and grading of osteoarthritis, age at surgery, duration of symptoms before surgery, sex, type of sport and daily activities, and preoperative alpha angle measures could be investigated as predictive factors for good functional outcomes or predisposing to development or deterioration of osteoarthritis.
Acknowledgments
Conflicts of interest
All the authors disclose no conflicts of interest. No benefit in any form has been received or will be received from a commercial party related directly or indirectly to the subject of this paper.
Contributor Information
Rocco Papalia, Email: r.papalia@unicampus.it.
Angelo Del Buono, Email: a.delbuono@unicampus.it.
Francesco Franceschi, Email: f.franceschi@unicampus.it.
Andrea Marinozzi, Email: a.marinozzi@unicampus.it.
Nicola Maffulli, Phone: +44-20-82238839, FAX: +44-20-82238930, Email: n.maffulli@qmul.ac.uk.
Vincenzo Denaro, Email: denaro@unicampus.it.
References
- 1.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. doi: 10.1097/00003086-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 5.Bedi A, Dolan M, Hetsroni I, Magennis E, Lipman J, Buly R, Kelly BT. Surgical treatment of femoroacetabular impingement improves hip kinematics: a computer-assisted model. Am J Sports Med. 2011;39(Suppl):43S–9S. doi: 10.1177/0363546511414635. [DOI] [PubMed] [Google Scholar]
- 6.Dorrell JH, Catterall A. The torn acetabular labrum. J Bone Joint Surg Br. 1986;68:400–403. doi: 10.1302/0301-620X.68B3.3733805. [DOI] [PubMed] [Google Scholar]
- 7.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 8.Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 9.Haviv B, Singh PJ, Takla A, O'Donnell J. Arthroscopic femoral osteochondroplasty for cam lesions with isolated acetabular chondral damage. J Bone Joint Surg Br. 2010;92:629–633. doi: 10.1302/0301-620X.92B5.23667. [DOI] [PubMed] [Google Scholar]
- 10.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 11.Jakobsen RB, Engebretsen L, Slauterbeck JR. An analysis of the quality of cartilage repair studies. J Bone Joint Surg Am. 2005;87:2232–2239. doi: 10.2106/JBJS.D.02904. [DOI] [PubMed] [Google Scholar]
- 12.Del Buono A, Papalia R, Khanduja V, Denaro V, Maffulli N (2011) Management of the greater trochanteric pain syndrome: a systematic review. Br Med Bull. Sep 4. [Epub ahead of print] [DOI] [PubMed]
- 13.Papalia R, Buono A, Osti L, Denaro V, Maffulli N. Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull. 2011;99:89–106. doi: 10.1093/bmb/ldq043. [DOI] [PubMed] [Google Scholar]
- 14.Papalia R, Franceschi F, Buono A, Maffulli N, Denaro V. Results of surgical management of symptomatic shoulders with partial thickness tears of the rotator cuff. Br Med Bull. 2011;99:141–154. doi: 10.1093/bmb/ldq040. [DOI] [PubMed] [Google Scholar]
- 15.Papalia R, Osti L, Del Buono A, Denaro V, Maffulli N Tibial inlay for posterior cruciate ligament reconstruction: a systematic review. Knee 17: 264–269 [DOI] [PubMed]
- 16.Papalia R, Osti L, Buono A, Denaro V, Maffulli N. Management of combined ACL-MCL tears: a systematic review. Br Med Bull. 2010;93:201–215. doi: 10.1093/bmb/ldp044. [DOI] [PubMed] [Google Scholar]
- 17.Papalia R, Osti L, Buono A, Denaro V, Maffulli N. Glenohumeral arthropathy following stabilization for recurrent instability. Br Med Bull. 2010;96:75–92. doi: 10.1093/bmb/ldq009. [DOI] [PubMed] [Google Scholar]
- 18.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935. doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 19.Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540–546. doi: 10.1016/j.arthro.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 20.Bizzini M, Notzli HP, Maffiuletti NA. Femoroacetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35:1955–1959. doi: 10.1177/0363546507304141. [DOI] [PubMed] [Google Scholar]
- 21.Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739–746. doi: 10.1007/s11999-008-0659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naal FD, Miozzari HH, Wyss TF, Notzli HP. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med. 2011;39:544–550. doi: 10.1177/0363546510387263. [DOI] [PubMed] [Google Scholar]
- 23.Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoral acetabular impingement in patients with preoperative generalized degenerative changes. Arthroscopy. 2010;26:623–629. doi: 10.1016/j.arthro.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38:99–104. doi: 10.1177/0363546509346393. [DOI] [PubMed] [Google Scholar]
- 25.Gedouin JE, Duperron D, Langlais F, Thomazeau H. Update to femoroacetabular impingement arthroscopic management. Orthop Traumatol Surg Res. 2010;96:222–227. doi: 10.1016/j.otsr.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Hartmann A, Gunther KP. Arthroscopically assisted anterior decompression for femoroacetabular impingement: technique and early clinical results. Arch Orthop Trauma Surg. 2009;129:1001–1009. doi: 10.1007/s00402-008-0806-4. [DOI] [PubMed] [Google Scholar]
- 27.Ilizaliturri VM, Jr, Nossa-Barrera JM, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of femoroacetabular impingement secondary to paediatric hip disorders. J Bone Joint Surg Br. 2007;89:1025–1030. doi: 10.1302/0301-620X.89B8.19152. [DOI] [PubMed] [Google Scholar]
- 28.Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoroacetabular impingement of the hip: a new technique to access the joint. Clin Orthop Relat Res. 2010;468:182–190. doi: 10.1007/s11999-009-1005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beaule PE, Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 30.Ilizaliturri VM, Jr, Orozco-Rodriguez L, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty. 2008;23:226–234. doi: 10.1016/j.arth.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 31.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467:747–752. doi: 10.1007/s11999-008-0656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lincoln M, Johnston K, Muldoon M, Santore R. Combined arthroscopic and modified open approach for cam femoroacetabular impingement: a preliminary experience. Arthroscopy. 2009;25:392–399. doi: 10.1016/j.arthro.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 33.Clohisy JC, Zebala LP, Nepple JJ, Pashos G. Combined hip arthroscopy and limited open osteochondroplasty for anterior femoroacetabular impingement. J Bone Joint Surg Am. 2010;92:1697–1706. doi: 10.2106/JBJS.I.00326. [DOI] [PubMed] [Google Scholar]
- 34.Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 35.Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908–914. doi: 10.1007/s00167-007-0332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yun HH, Shon WY, Yun JY. Treatment of femoroacetabular impingement with surgical dislocation. Clin Orthop Surg. 2009;1:146–154. doi: 10.4055/cios.2009.1.3.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peters CL, Schabel K, Anderson L, Erickson J. Open treatment of femoroacetabular impingement is associated with clinical improvement and low complication rate at short-term followup. Clin Orthop Relat Res. 2010;468:504–510. doi: 10.1007/s11999-009-1152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 39.Bardakos NV, Vasconcelos JC, Villar RN. Early outcome of hip arthroscopy for femoroacetabular impingement: the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br. 2008;90:1570–1575. doi: 10.1302/0301-620X.90B12.21012. [DOI] [PubMed] [Google Scholar]
- 40.Byrd JW, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25:365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 41.Gedouin JE, May O, Bonin N, Nogier A, Boyer T, Sadri H, Villar RN, Laude F. Assessment of arthroscopic management of femoroacetabular impingement. A prospective multicenter study. Orthop Traumatol Surg Res. 2010;96:S59–S67. doi: 10.1016/j.otsr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am. 2006;88:1735–1741. doi: 10.2106/JBJS.E.00514. [DOI] [PubMed] [Google Scholar]
- 43.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 44.Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39:14S–19S. doi: 10.1177/0363546511401900. [DOI] [PubMed] [Google Scholar]
- 45.Haviv B, O'Donnell J. Arthroscopic treatment for symptomatic bilateral cam-type femoroacetabular impingement. Orthopedics. 2010;33:874. doi: 10.3928/01477447-20101021-14. [DOI] [PubMed] [Google Scholar]
- 46.Tonnis D, Heinecke A, Nienhaus R, Thiele J. Predetermination of arthrosis, pain and limitation of movement in congenital hip dysplasia. Z Orthop Ihre Grenzgeb. 1979;117:808–815. [PubMed] [Google Scholar]
- 47.Kellgren JH, Lawrence JS. Radiological assessment of rheumatoid arthritis. Ann Rheum Dis. 1957;16:485–493. doi: 10.1136/ard.16.4.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res. 2010;468:555–564. doi: 10.1007/s11999-009-1138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Banerjee P, McLean CR. Femoroacetabular impingement: a review of diagnosis and management. Curr Rev Musculoskelet Med. 2011;4:23–32. doi: 10.1007/s12178-011-9073-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93:580–586. doi: 10.2106/JBJS.J.00875. [DOI] [PubMed] [Google Scholar]
- 51.Emara K, Samir W, Motasem H, Ghafar KA. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong) 2011;19:41–45. doi: 10.1177/230949901101900109. [DOI] [PubMed] [Google Scholar]
- 52.Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15:132–137. doi: 10.1053/ar.1999.v15.015013. [DOI] [PubMed] [Google Scholar]
- 53.McCarthy JC, Lee JA. Arthroscopic intervention in early hip disease. Clin Orthop Relat Res. 2004;429:157–162. doi: 10.1097/01.blo.0000150118.42360.1d. [DOI] [PubMed] [Google Scholar]
- 54.Santori N, Villar RN. Acetabular labral tears: result of arthroscopic partial limbectomy. Arthroscopy. 2000;16:11–15. doi: 10.1016/S0749-8063(00)90121-X. [DOI] [PubMed] [Google Scholar]
- 55.Khanduja V, Villar RN. The arthroscopic management of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1035–1040. doi: 10.1007/s00167-007-0319-7. [DOI] [PubMed] [Google Scholar]
- 56.Imam S, Khanduja V. Current concepts in the diagnosis and management of femoroacetabular impingement. Int Orthop. 2011;35:1427–1435. doi: 10.1007/s00264-011-1278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]