Abstract
Exposure therapy, despite its demonstrated efficacy for chronic PTSD, remains underutilized across clinical settings. One suggested cause is that traumatized clients may not prefer exposure treatment. This paper reviews the current literature on factors associated with treatment preference for exposure therapy. Contrary to expectations, exposure-based therapy is not only perceived as a viable therapy but is well regarded among current therapy choices by potential clients. In particular, we highlight the central role of client beliefs about the need to talk about problems, the efficacy of treatment, and perceived need for help as crucial factors potentially impacting preference for exposure therapy. Importantly, fear of exposure treatment does not appear to play a significant role. To increase utilization, clinicians should provide clients information to address factors believed to increase preference for effective treatment.
Keywords: Exposure Therapy, Posttraumatic stress disorder, Preference
In the U.S. population, lifetime prevalence rates of posttraumatic stress disorder (PTSD) range from 7% to 8% (Kessler et al., 2005; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995) and 12-month rates approach 4% (Kessler, Chiu, Demler, & Walters, 2005). Prevalence rates among returning military veterans are estimated to reach as high as 19.9% (Hoge et al., 2004). Despite this high prevalence, only 7.1% of individuals with PTSD make treatment contact within the first year of trauma exposure (Wang, Berglund, Olfson, Pincus, Wells, & Kessler, 2005). Further, the median time to seek treatment for PTSD is twelve years after disorder onset, with only 65.3% eventually seeking treatment and only 34.4% seeing a mental health specialist (Wang et al., 2005). Thus, it is of paramount importance that we begin to better understand how to help individuals with PTSD seek clinically appropriate care.
The need for such care is likely to increase in coming years given the large number of active military conflicts and peace-keeping missions currently underway. Indeed, in order to address the expected increased numbers of veterans needing empirically-supported PTSD treatment (Hoge et al., 2004; Tanaelian & Jaycox, 2008), the United States Department of Defense (DoD) and the Veterans Administration (VA) have created Mental Health Centers of Excellence and funded large-scale initiatives aimed at training practitioners to deliver evidenced-based PTSD treatment. This training largely focuses on cognitive behavioral interventions such as exposure therapy. Although a number of psychotherapies have strong efficacy data (e.g., Bradley, Green, Russ, Dutra, & Westen, 2005), the recent Institute of Medicine (IOM, 2007) report on PTSD treatment concluded that the only sufficiently validated treatment for PTSD at the present time is exposure therapy. Indeed, the efficacy of exposure treatment has been strongly replicated across gender and types of trauma (e.g., Foa et al., 1991; 1999; 2005; Marks et al., 1998; Resick et al., 2003; Rothbaum et al., 2005; Schnurr et al., 2007; Tarrier et al., 1999; Taylor et al., 2003). Thus, exposure-based therapy is one of the treatments of choice for chronic PTSD.
Yet, both clients and therapists may be reluctant to choose this treatment. Despite exposure therapy’s proven benefits for PTSD, the treatment can be anxiety producing: clients are encouraged to directly and repeatedly approach the trauma memory (e.g., imaginal exposure) and trauma-related fears (e.g., in vivo exposure). Early commentators on the use of exposure therapy for PTSD voiced concerns about potentially retraumatizing the trauma survivor and increasing, rather than decreasing, his or her suffering. Specifically, Kilpatrick and Best (1984) suggested that high levels of anxiety during imaginal exposure may be a negative experience and result in an aversion to coming to therapy. Further, they suggested that some clients may exhibit more distress than they did before treatment and as a result, be less likely to seek treatment in the future. Although these fears have not been empirically supported, with exposure therapy failing to show more symptom worsening or treatment dropout (e.g., Foa, Zoellner, Feeny, Hembree, & Alvarez-Conrad, 2002; Hembree, Foa, Dorfan, Street, Kowlaski & Tu , 2004), concerns regarding the potential tolerability of exposure both for the therapist and for the client remain (e.g., Becker, Zayfert, & Anderson 2004; Tarrier et al., 1999; Pitman et al., 1991; 1996; Zayfert & Becker, 2000). Indeed, a recent survey of practitioners suggested that while lack of training in exposure therapy clearly plays a role in its under-utilization; even among therapists with such training fears about how the client will tolerate exposure appear to impact therapists’ willingness to use it (Becker et al., 2004). Thus, based on these fears, clients and/or therapists may choose not to utilize exposure treatment for chronic PTSD.
Importance of Preference in Treatment for PTSD
We may be better able to understand, and potentially improve, treatment seeking and utilization of evidence based treatments in people with PTSD by knowing more about individuals’ reactions to and preferences for exposure-based treatment. One of the main reasons to examine client treatment preferences is practical. Although clients in efficacy studies typically enter treatment passively through random assignment, clients in routine clinical practice see a treatment provider after actively shopping either for a type of treatment or a specific therapist (Seligman, 1995). Thus, although we have treatments with proven efficacy for PTSD, if this therapy is not available, or a client does not want this type of therapy, then the therapy is of limited practical utility (Zoellner, Feeny, & Rothbaum, 2005). Indeed, a National Institute of Mental Health workshop report (NIMH; Street, Niederehe, & Lebowitz, 2000) suggested the need for better understanding “whether providers should try to accommodate patient preferences for the type of treatment they wish to receive versus persuade them to accept one modality over another” (p. 130). If clients are unwilling to choose exposure therapy, then the next question is whether or not it is worthwhile to try to persuade them to accept this modality.
Another reason to examine treatment preferences is that they may lead to enhanced therapeutic outcome. The idea of trying to accommodate client preferences is not new. As far back as (1977), Cronbach and Snow suggested that matching treatments to client characteristics may enhance clinical outcomes, highlighting the role of what they termed aptitude by treatment interactions. Consistent with this, in a review article, Beutler and Bergan (1991) concluded, “. . .convergence of a client's attitudes and values on those of his or her counselor is linearly related to the benefit experienced by the patient.” Indeed, there is mounting evidence from other disorders that clients who agree with rationales for cognitive behavioral treatment improve more quickly and have better outcomes than those who do not (Addis & Carpenter, 1999; Addis & Jacobson, 2000; Bedi et al., 2000; Chilvers et al., 2001; Fennel & Teasdale, 1987; Ilardi & Craighead, 1994).
Thus, with regard to exposure therapy, the question that arises is whether or not there is a “match” between the rationale for the intervention and clients’ perceptions of the type of care they need. Will individuals with chronic PTSD choose exposure therapy? Does it match with their beliefs? We will attempt to address both questions. This paper will review the literature on the preference for exposure therapy, factors that influence traumatized individuals’ treatment preferences, and will suggest a model regarding how these factors contribute to clients’ preferences for exposure treatment. Understanding the factors that contribute to whether or not individuals are willing to enter exposure therapy may be critical to current efforts aimed at dissemination and improving its utilization by therapists.
Will Clients Choose Exposure Therapy?
At a basic level, clients’ acceptance of exposure therapy may be largely influenced by their preference for psychotherapy in general. In a discussion of methods that could aid and speed dissemination efforts for psychological treatments, Barlow (2004) noted that there is a large body of evidence suggesting that when given the choice, the public generally prefers psychological treatments over pharmacological treatments. This literature spans a wide range of psychological disorders (panic disorder: Hazlett-Stevens et al., 2002; Hofmann et al., 1998; eating disorders: Mitchell et al., 1990; Wilson & Fairburn, 2002; PTSD: Zoellner, Feeny, Cochran & Pruitt, 2003; and depression: Bedi et al., 2000; Chilvers et al., 2001; Dwight-Johnson, Sherbourne, Liao & Wells, 2000; Goldstein & Roselli, 2003) and strongly suggests that individuals suffering from a psychological disorder prefer psychotherapy. The preference for psychotherapy in general may work in exposure therapy’s favor by predisposing clients to view any psychotherapy favorably.
A body of literature examining treatment preferences following trauma exposure and exposure therapy, in particular, is just starting to emerge. Studies to date have largely focused on trauma exposed (Roy-Byrne, Berliner, Russo, Zatzick & Pitman, 2003; Angelo, Miller, Zoellner & Feeny, 2008) or undergraduate samples (Becker, Darius, & Schaumberg, 2007; Tarrier, Liversidge, & Gregg, 2006; Zoellner, Feeny, Cochran, & Pruitt, 2003), with only subsamples pointing to preferences for individuals with chronic PTSD.
Two trials have explored preferences in trauma-exposed samples, one regarding therapy in general (Roy-Byrne et al., 2003) and the other specifically focusing on exposure therapy (Angelo et al., 2008). In a large preference trial, Roy-Byrne and colleagues (2003) explored the preference for medication, counseling, or combined treatment in 466 women seen in the emergency room after a physical or sexual assault. Although many women indicated an interest in both medication and counseling, more women preferred counseling (76%) than medication (62%). However, this study did not provide any detailed information about what these treatments would entail nor did it directly assess PTSD. In a smaller sample of trauma-exposed women (n = 74), Angelo and colleagues (2008) provided detailed treatment rationales for two empirically-supported treatments, prolonged exposure, a type of exposure therapy, and sertraline, a serotonergic medication. After viewing standardized therapist-delivered rationales, women were asked to choose among prolonged exposure therapy, sertraline, or no treatment. The vast majority of women preferred prolonged exposure (81.7%) to sertraline (12.7%) or no treatment (5.6%). Further, rates of choice did not change substantially when examining only those women who met PTSD diagnostic criteria: 78.9% chose prolonged exposure, 13.2% sertraline, and 7.9% no treatment (Feeny, Zoellner, Mavissakalian, & Roy-Byrne, 2008). Taken together, in trauma-exposed samples, there appears to be a preference for psychotherapy in general and this preference is also evident for exposure-based treatments.
In analogue studies, using undergraduate students and hypothetical scenarios, a similar preference pattern emerges (Becker et al., 2007; Tarrier et al., 2006; Zoellner et al., 2003). In the first study to directly examine preference for exposure therapy, Zoellner and colleagues explored choices of prolonged exposure and sertraline for the treatment of PTSD in a large sample of female undergraduates (n = 273) over half of whom had experienced a DSM-IV Criterion A trauma, and 18% of whom met diagnostic criteria for current PTSD. This analogue sample was asked to imagine that they had experienced an earlier sexual-assault and currently had PTSD-related symptoms, than they were presented with detailed treatment rationales for prolonged exposure (PE) and sertraline. The primary outcomes were perceived credibility of the treatment (e.g., how effective they believed the treatment to be in general) and personal reactions to the treatment (e.g., whether they believed the treatment would be effective for them personally). Participants rated the PE as more credible and had more positive personal reactions than the sertraline. When making a treatment choice, the majority of women (87.4%) chose PE, whereas only a minority chose sertraline (6.9%) or no treatment (5.7%). Of women who met criteria for PTSD, 74.1% chose PE, 22.2%, chose SER, and 3.1% chose no treatment. As might be expected, participants’ ratings of perceived treatment credibility and personal reactions to the rationales coincided with their treatment choices. This study further supports a general preference for psychotherapy over pharmacotherapy, and shows a specific preference for exposure therapy. However, both the forced choice nature of this study and lack of comparison to other treatment options raise questions about how well exposure therapy compares when compared to other psychotherapies for PTSD symptoms. That is, the preference shown for exposure therapy may result from the lack of other psychotherapy alternatives.
To address these limitations, Becker, Darius, and Schaumberg (2007) investigated preference for PTSD treatment in 160 undergraduate students comparing various treatment options including prolonged exposure, sertraline, and various psychotherapies and interventions with differing levels of empirical support (e.g., cognitive behavior therapy, eye movement desensitization reprocessing therapy, thought-field therapy). Similar to Zoellner et al. (2003), participants were given a hypothetical scenario and detailed treatment rationales for each choice. Even with an expanded range of psychotherapy treatments of varying empirical support, exposure therapy was still the most preferred treatment (51%), with the highest ratings of credibility. The next most preferred treatment was cognitive behavior therapy (22%). For those individuals who met criteria for PTSD (n = 11), exposure was once again the most preferred treatment (36%). This study suggests that the preference for exposure therapy found in previous studies was not solely an artifact of limited competition from other psychotherapy options. Importantly, the authors did not equate rationales for each treatment with respect to empirical support for the treatment because some psychotherapy alternatives had not been adequately researched. This potential difference across rationales highlights the question of the degree to which empirical support plays a role in treatment preference.
In a similar study, Tarrier, Liversidge, and Gregg (2006) further expanded this treatment preference paradigm and included fourteen different PTSD treatment options, with varied therapeutic models (e.g., psychoeducation, imaginal exposure, cognitive therapy, stress management) and methods of delivery (e.g., individual psychotherapy, groups, virtual reality, computers, e-therapy). Three-hundred and thirty undergraduates were given a hypothetical trauma scenario and treatment rationales designed to reflect the information clients would receive in real-world clinical settings. Among the 14 options, cognitive therapy was rated as the top choice treatment, cognitive therapy with exposure as the second highest ranked, and imaginal exposure as the third highest ranked treatment. Preference in individuals with PTSD was not directly examined in this sample. Notably, participants’ top five preferred treatments were the treatments with the strongest empirical evidence, suggesting that clients may well be educated consumers of psychotherapy and base their preference for treatment in part on empirical support.
The above studies demonstrate convincingly that there is a preference for psychotherapy treatments for trauma-related difficulties and, despite questions to the contrary, an acceptance of and preference for exposure treatment. This preference was found whether participants were offered a forced choice between exposure therapy and a medication or offered a wide range of psychotherapies to determine their preference of treatment. Yet, none of the studies to date include treatment-seeking samples with chronic PTSD. How ever, in both the Angelo et al. (2008) and Zoellner et al. (2003), rates of preference for those with PTSD were comparable to the larger sample. Nevertheless, preferences may be different when individuals are making actual treatment choices. These studies also start to highlight factors that may underlie treatment preference for exposure, including the potential importance of beliefs or knowledge about empirical evidence. In the following section, we will review the role of client-related beliefs, comorbid psychopathology and symptom severity, and demographic factors that may underlie preference for exposure therapy.
Factors Associated With Treatment Preference for Exposure
Client's Beliefs about Psychosocial Treatment
Thus far, across the research on treatment preference and choice of exposure, one of the strongest factors associated with whether individuals will choose exposure treatment for PTSD is the individual’s beliefs about treatment (Angelo, Miller, Zoellner & Feeny, 2008; Cochran, Pruitt, Fukuda, Zoellner & Feeny, 2008; Zoellner, et al., 2003). In particular, an individual’s beliefs about the mechanism of treatment action (e.g., “You need to talk about the trauma”), treatment’s effectiveness (e.g., “therapy gets to the root of the problem and does not just cover up the symptoms”), and the perceived need for therapy (e.g., “Something this big can’t be dealt with alone”) appear to be salient factors influencing treatment preference for exposure-based therapies (Angelo et al., 2008; Cochran et al., 2008). Each will be reviewed below.
Treatment mechanism: The importance of talking about problems
One of the most commonly cited reasons for choosing exposure therapy is a belief regarding the importance of talking through problems as a way of healing. In Cochran et al.’s (p. 283, 2008) qualitative analysis of reasons underlying treatment preference, one undergraduate wrote, “I think that it is important to talk about your problems and figure out what is causing them.” Another also reiterated the same point suggesting that, “Talking about problems makes me feel better.” Indeed, of the reasons given for choosing a treatment, 41% highlighted a need to talk about a problem and 28.2% highlighted a need to directly confront problems (Cochran et al., 2008). These rates were comparable in their trauma-exposed and PTSD subsamples. Of note, women who stated positive feelings about talking were 7.01 times more likely to choose exposure therapy over sertraline or no treatment. Angelo et al. (2008), in their trauma-exposed sample, a high percentage of primary reasons given for choosing a treatment (49.3%) highlighted a similar construct and women who cited this construct were 2.63 times more likely to choose exposure therapy. Thus, as might be expected, individuals who believe that talking about their trauma is critical to recovery overwhelmingly choose exposure therapy.
This strong emphasis on the need to talk about problems is telling and may reflect a more generalized belief about the need to talk about psychological difficulties and recovery (Hayes, Kohlenberg & Melancon, 1989; Hayes & Wilson, 1993). This dovetails well with a large body of research noting the beneficial effects of talking about emotional events (Campbell & Pennebaker, 2003; Groom & Pennebaker 2002, Pennebaker, Mehl, & Niederhoffer 2003). Alternatively, this perceived need to talk about problems may be crucial in PTSD-related treatment because of the presence of an external event. PTSD provides a unique scenario for questions of mechanism, as it is one of the only disorders that requires an external event for the etiology of the disorder (Davidson & Foa, 1991). This can be contrasted with depression where the etiology or cause of the disorder is often argued to be more biological, and consequently internal nature (Shelton, Hollon, Purdon, & Loosen, 1991). This importance of beliefs about mechanism suggests that individuals are thinking carefully about the relationship between their current difficulties and possible treatments that might address these difficulties. These beliefs about how problems are handled and confronted may already be in place well before an individual experiences a traumatic event. Overall, beliefs about treatment mechanism may play one of the largest roles influencing a client’s treatment preference. That is, the match between a treatment and an individual’s beliefs about how a treatment might work, may be critical to understanding preferences.
Perceived effectiveness of therapy
As suggested above (Tarrier et al., 2006), the degree to which individuals believe that a treatment is efficacious most likely influences their willingness to undergo treatment, and indeed, this belief is also strongly associated with treatment choice (Zoellner et al., 2003). In particular, this belief appears to include ideas such as therapy getting to the root of the underlying problem and producing long-lasting effects (Cochran et al., 2008). Zoellner et al. (2003) found that 36% of their sample reported that perceived effectiveness of the treatment was the primary reason for their choice of treatment. Similarly, Angelo et al. (2008) reported that 22.5% cited this as their primary reason for their choice of treatment. In the Cochran et al. (2008) sample, this reason was the most commonly given among all the reasons (73.6%) for choosing a treatment and increased the likelihood of choosing exposure therapy by 4.56 times. This is all the more striking, as in this Cochran et al. (2008) study, the wording regarding the effectiveness of exposure and sertraline was actually identical. Although the perceived effectiveness of a treatment clearly plays an important role in individuals’ choice of treatment, its ability to predict choice was actually not as strong as beliefs about the mechanism of treatment in the Angelo et al. (2008) sample. Though we would expect that individuals are more likely to choose treatments they feel will be helpful at addressing their symptoms, the importance of efficacy suggests that clients are conscientious consumers who when provided relevant information, are carefully weighing their treatment options before choosing.
Perceived need for help
A related belief that may potentially play a more important role among those with chronic PTSD than in analogue samples is the perceived need for outside help. Typical reasons given include statements like “Something that big can’t be dealt with alone,” and “Treatment is absolutely necessary.” (p. 284, Cochran et al., 2008). Yet, of all reasons given, only 22.3% of women cited this as one of their reasons for treatment choice; however, when given, it was a strong predictor of preference for type of treatment (Cochran et al., 2008). Notably, in this study though, this reason was more about the role of medications than it was about exposure. That is, one interpretation is that the more severe the problem is perceived the more there is a belief regarding the need for medication intervention. In general, although psychotropic medications may be generally disapproved of, the severity of the problem may underlie how much medication is perceived to be needed (Benkert et al., 1997). Across studies, though, this belief has not been as systematically studied as either beliefs about perceived mechanism or perceived effectiveness.
Fear of exposure
Notably, fear of exposure (“This sounds like a difficult treatment.”), though commonly thought of as a reason for not choosing exposure, does not systematically emerge as a predictor of choice. More specifically, in our work, this reason consistently fails to be one of the key reasons given underlying choice (< 25%; Angelo et al., 2008; Cochran et al., 2008; Zoellner et al., 2003). When wariness of treatment is more consistently mentioned, it is more often about wariness of medications, or about not wanting any psychiatric treatment at all (e.g., “My faith will heal me.”), and not necessarily about exposure therapy (Angelo, et al., 2008, Cochran et al., 2007). That said, none of these studies directly asked about fear of exposure. Instead, participants were asked to describe the reasons underlying their preference. With this method, we can easily conclude that this fear appears not to be a highly salient issue, but we cannot conclude that fear is not a concern.
If fears of exposure-related distress are indeed a concern, anxiety sensitivity, or fear of fear, should consistently predict not choosing exposure. Yet, it does not predict choosing or not choosing exposure (Angelo et al., 2008) nor is it associated with lower personal reactions and credibility of exposure (Zoellner et al., 2003). Further, given that individuals are willing to choose exposure therapy even in the midst of other viable treatments (e.g., Becker et al., 2007; Tarrier et al., 2006), and even though they note associated discomfort (Tarrier et al., 2006), this further argues that, even if this is an issue for some individuals, other factors may be more directly affecting treatment choice. That is, even though some individuals may be afraid of exposure, they still appear willing to enter exposure treatment, perhaps because their belief that talking about the event is necessary to recover from it is stronger than their fears.
Summary regarding importance of beliefs
Importantly, beliefs about the nature of treatment appear to be some of the strongest predictors of treatment choice, almost always outperforming demographic and psychopathology factors further discussed below. These beliefs are likely not a unitary construct, with some factors being more important than others. Specifically, beliefs about the mechanism of treatment, including the importance of talking about a problem and the etiology of PTSD-related symptom, are consistently some of the strongest predictors for exposure treatment preference. Beliefs about the efficacy of treatment also predict exposure treatment preference, suggesting that preference is also determined by a belief that a given treatment will work. Perceived need for help also appears to be a salient issue, potentially more so for those with more severe symptoms. Finally, despite arguments in the literature that fear of exposure should play a large role in treatment preference, there is a striking lack of evidence that would suggest that individuals are avoiding choosing exposure as a result of their fear of the arousal that accompanies it.
Symptom Severity and Diagnostic Co-occurrence
Though preexisting client beliefs are some of the strongest predictors of treatment preference, there are other factors that may play a role as well. One such factor is symptom severity, which modestly predicts not choosing exposure therapy in PTSD. Indeed, Zoellner, Feeny and Bittinger (2008) showed that severity of psychopathology (depression or PTSD) may be directly associated with a greater likelihood of choosing pharmacotherapy, albeit at a low level. One possible reason for this preference is that higher levels of symptoms may make individuals have doubts about their ability to fully participate in exposure therapy. Consistent with this interpretation, higher state anxiety has been mildly associated with lower personal reactions to exposure therapy in an analogue sample (r = −.17; Zoellner et al., 2003) and the presence of co-occurring depression leads to a higher preference for pharmacotherapy over exposure than for those individuals without depression (Feeny et al., 2008), though exposure therapy is still preferred. Alternatively, individuals with more severe symptoms may choose other treatment options such as medications for immediate relief of their psychological distress (Feeny et al., 2008). Taken together, high symptom severity or the presence of comorbidity may be somewhat associated with less receptivity to exposure therapy.
Prior Treatment History
Another possible factor contributing to treatment preference is prior history of treatment. Though we would expect prior experience with any form of psychotherapy or pharmacotherapy to be potentially associated with treatment preference, the results to date have been mixed. Two studies report small associations between past experience and treatment preference (Roy-Byrne et al., 2003; Tarrier et al., 2006), with positive past therapy experience or knowledge predicting preference for psychotherapy (Tarrier et al., 2006). However, prior therapy experience or medication experience were not substantially associated with choice or exposure therapy and sertraline (Angelo et al., 2008; Feeny et al., 2008; Zoellner et al., 2003) or ratings of personal reactions and credibility of exposure or sertraline (Angelo et al. 2008). It may be that, even among those with prior therapy experience, exposure therapy is perceived a “new” therapy possibility and accordingly, experience with other therapies does not directly affect its preference. Thus, past treatment experience may play a small but potentially unstable role in treatment preference, though the current studies are not sufficient to fully determine the relationship between the two.
Demographic Factors
Across a range of demographic factors including age, education, income, ethnicity, history of trauma exposure, at this time, only three factors have consistently emerged as being associated with treatment preference in PTSD: education (Angelo et al., 2008), cultural background (Zoellner et al., 2008), and gender (Roy-Bryne et al., 2003). Yet, in these findings, these factors appear to be associated with modest, at best, predictive value of treatment preference.
Because beliefs about treatment strongly predict exposure therapy preference, there are a number of reasons why we might expect education to be similarly related. Indeed, in a community sample of women with a history of trauma, higher levels of education predicted choosing exposure therapy (Angelo et al., 2008), though this finding has not be seen in other studies (Zoellner et al., 2008) and was not examined in others (e.g., Becker et al., 2007; Roy-Bryne et al., 2003; Tarrier et al., 2008). Regardless, it may be that this relationship when seen speaks to a more general association between education and preference for psychotherapy often seen in the literature (Olfson & Pincus, 1994) rather than anything overtly specific to exposure therapy.
Other demographic variables such as ethno-cultural factors may influence treatment preference for exposure. Indeed, in several preference studies (Dwight-Johnson et al., 2000; Hazlett-Stevens et al., 2002; Wagner et al., 2005), ethnic minorities indicated being less receptive to medication than Caucasians. However, this has not been replicated in trauma exposed samples (Angelo et al., 2008; Roy-Byrne et al., 2003), or in one study which found a small effect of ethnic minorities’ preference for pharmacotherapy over psychotherapy (Zoellner et al., 2008). Given the evidence that ethnic minorities are less likely to seek mental health services (Wyatt, 1992), it is all the more important to better understand specific cultural factors in choosing treatment for mental health issues. As suggested by Wong and colleagues (2003) credibility of treatment options may be moderated by cultural identity and self-construals rather than broad categorizations of group membership. Clearly, at this time, better studies are needed to examine the influence factors such as cultural identity and self-construal on treatment preferences in PTSD and exposure therapy specifically.
There is also little known on the relationship of treatment preference to gender in PTSD. In general, women are more likely to engage in psychotherapy (Kushner & Sher, 1991) whereas men are less willing for reasons potentially related to being socialized as self-reliant and avoiding self-disclosure (Nadler, Maler & Friedman, 1984), suggesting that gender may differentially impact treatment preference. One study with sexual assault survivors showed that being female was predictive of preferring either medication and psychotherapy (Roy-Bryne et al., 2003), suggesting a general inclination in women for seeking help of any kind. Studies by Zoellner et al. (2003) and Angelo et al. (2008) utilized female only samples, and, accordingly, rates of choice in these samples may actually reflect gender effects. Other preference studies have included primarily females as well (62%; Becker et al 2007; 64%; Tarrier et al., 2006) and have not investigated the impact of gender on choice.
Taken together, our current understanding of the influence of psychopathology, prior treatment history, demographic variables on treatment preference for exposure therapy is relatively limited. Some of these limitations are largely due to samples with limited ranges of these factors such as undergraduates and lack of diversity of individuals with prior treatment experiences, varying ethnic backgrounds, or genders. There is some preliminary evidence that higher symptom severity is associated with choosing pharmacotherapy over exposure therapy, though it looks to be a small effect. In general, demographic factors such as education, ethnicity, and gender show low or inconsistent predictive ability in exposure treatment preference, potentially reflecting a smaller causal role than treatment beliefs.
A Proposed Belief-based Model of Preference for Exposure Therapy for Chronic PTSD
In the treatment choice and preference studies reviewed above, exposure treatment was consistently one of the most frequently chosen treatments for PTSD (Angelo et al., 2008; Becker et al., 2007; Feeny et al., 2008; Tarrier et al., 2006; Zoellner et al., 2003). Though this preference for exposure therapy may reflect a general preference for psychotherapy over pharmacotherapy (Barlow, 2004; Becker et al., 2007), research on the choice of exposure therapy for PTSD suggests a more complex picture. The evidence reviewed above suggests that perhaps the most critical determining factor for treatment choice is individual’s beliefs about treatment. Indeed, individuals may have a complicated range of beliefs about the match between exposure treatment and PTSD (Cochran et al., 2008), including beliefs about the importance of talking about events, including the etiology and external nature of PTSD, beliefs about the effectiveness of treatment, and their perceived need for treatment.
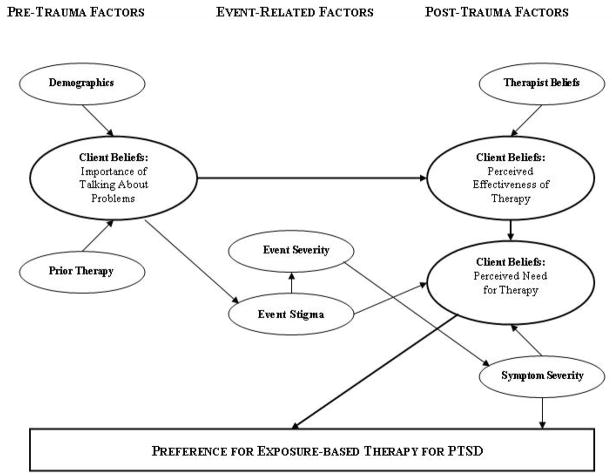
Though the current treatment preference literature is weak in certain areas (e.g., demographic factors), it highlights a number of factors that potentially play an important role in treatment preference for exposure. In order to provide a conceptual framework for further research into preference for exposure therapy, we have proposed a belief-based model that incorporates what we believe to be potentially key empirically-supported factors that may influence exposure treatment preference. Figure 1 presents this belief-based model. This model includes the relationship between the factors discussed above and the hypothesized roles that they play in the prediction of treatment preference, highlighting both proposed direct and indirect effects. In interpreting this figure, the relative size of the ovals denoting key constructs and thickness of the lines denoting key associations are potentially indicative of stronger more consistent associations.
Figure 1.
A Beliefs-based Model for Preference for Exposure Therapy for Chronic PTSD.
Notably, this model is broken into pre-trauma, event-related, and post-trauma factors. Prior to trauma exposure, it is likely that individuals have thought about what it would be like to have experienced a traumatic event (e.g., rape, combat, etc.) and already have some beliefs in place about how to handle certain types of problems and, in particular, beliefs about the importance of talking about problems. We propose that various demographic factors, such as education, cultural identity, and gender may exert their influence on preference largely through a general belief about how psychological treatments work, that is, the believed key treatment mechanism. In addition, other demographic factors such as prior trauma history may also exert their influence through this belief, though at present this is unstudied. Further, prior experience with either psychotherapy or pharmacotherapy for psychological problems may also exert its influence on treatment preference through pre-existing beliefs about treatment mechanism.
We have included two specific event-related factors, neither of which has proposed direct effects on preference for exposure. Obviously, the severity of a traumatic event is consistently associated with severity of post-trauma reactions and thus is included specifically in that regard (Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey & West, 2003). We have also included a variable we term “event stigma”, referring to the individual’s perception of societal or self stigma of the event. This is a factor has not been previously explored. However, we deem it potentially important for whether or not individuals will perceive a need for treatment. Indeed, given the focus of previous studies on more homogeneous samples, it may be that certain types of events or event characteristics are perceived as more stigmatizing than others (e.g., Frazier & Berman, 2008; Hoge et al. 2004; Ullman, 1996); and, accordingly, individuals will be less likely to perceive a need or have a willingness to seek treatment.
Finally, we have included a variety of post-event factors. Of primary note, key factors here are beliefs about the effectiveness of therapy and one’s perceived need for treatment. Given that providers have pre-existing beliefs about the effectiveness of exposure for their particular clients (e.g., Becker, Zayfert & Anderson, 2004), we have included this as a factor associated with whether or not an individual will perceive exposure therapy as an effective treatment. Further, event stigma, current symptom severity, and beliefs about the effectiveness of treatment are hypothesized to impact a belief about the need for treatment. We also have included a direct link between severity and choice of exposure, as individuals with higher symptom severity may be less likely to choose exposure therapy (Zoellner et al., 2008). Notably, as discussed above, fear of exposure itself does not appear to deter people from preferring exposure in general; and accordingly, it is not included as a central construct in this beliefs model.
Many areas of the proposed model have yet to be thoroughly investigated, but the model incorporates and synthesizes key factors found to date to play a role in treatment preference for exposure and provides an initial framework for their interaction. Obviously, our current knowledge of preference for exposure needs to be expanded to include much larger samples and various groups of trauma survivors with PTSD; and accordingly, this model should only be viewed as preliminary. Of particular note in this model is a shift away from focusing on demographic factors in predicting treatment preference to more specifically understanding individual’s belief systems about treatment seeking both in general and more specifically about exposure for the treatment of chronic PTSD. Ultimately, we believe that what individual’s believe about themselves and treatment will most dramatically influence their preference for or against a treatment. This may also have a profound influence on treatment adherence, dropout, and clinical outcome, reflecting either a good or poor aptitude by treatment match.
Clinical Implications
Importantly, contrary to some clinicians’ beliefs, the studies reviewed above strongly show that individual will choose exposure when given an empirically sound rationale for it. Further, treatment beliefs play a critical role in exposure treatment preference and therefore should routinely be addressed and incorporated in treatment rationales. The presentation of treatment rationales is the primary opportunity for clinicians to understand beliefs that clients have. Clinicians should be prepared to offer clients seeking treatment for PTSD a menu of empirically-supported treatments and, importantly, be able to offer rationales that include information about key areas potentially affecting choice, namely the hypothesized underlying mechanism of treatment and information regarding the research supporting its effectiveness.
In this process, clinicians should assess clients’ treatment-related beliefs and incorporate these beliefs into treatment rationales, in an effort to not only enhance confidence in their treatment choice but potentially also to enhance treatment adherence. For instance, if a client already has a strong belief that talking about their traumatic event is important to their recovery, highlighting this aspect of exposure treatment may foster a better aptitude by treatment match for exposure. Conversely, if a client believes that psychotherapy treatment that does not focus on talking about the event is just as likely to be beneficial, the clinician may devote more of the rationale to discussion the empirical basis for talking about the traumatic event. Alternatively, in the instances where a good “match” cannot be achieved, it is important to remember that there are a number of other empirically-supported treatments for trauma-related PTSD (Foa, Keane, & Friedman, 2000). Thus, by actively assessing the clients’ beliefs during the treatment contemplation phase, the clinician can tailor their treatment rationales to result in the greatest likelihood of the client choosing a “good match.”
It is important to note, however, that client’s beliefs about treatments may well be inaccurate, and therefore may contribute to an unwillingness to participate in effective treatments. For example, clients may believe that revisiting traumatic events can only serve to further upset them and therefore that exposure therapy cannot address their symptoms. Or, a client may believe that there are no differences in the empirical support between various psychotherapies and therefore feel any treatment may be as helpful. In these instances, the clinician must be able to highlight the incorrect portions of the client’s treatment beliefs and to provide corrective information. Lastly, though clinicians can present clients with the important information regarding the therapies they are considering, a clinician’s ability to influence the client’s choice, even by drastically altering information they may provide, may be limited (Feeny, Zoellner, & Kahana, 2008). That is, clients may come into treatment with strong pre-existing preferences regarding what will be helpful to them and these beliefs may be highly resistant to change.
Though exposure therapy generally appears to be considered a viable treatment option, the current underutilization of exposure suggests that there is still much work to be done. Namely, any efforts that prove helpful at increasing clients’ preference for effective PTSD treatment, in any form, are clearly in the client’s best interest. One interesting area of PTSD research that may prove influential in enhancing client utilization of exposure is its adaptation to virtual reality (VR) environments (Difede, Cukor, Patt, Giosan, & Hoffman, 2006; Rothbaum, 2006). Though VR includes the same components of typical exposure therapy, the addition of VR may well make this treatment more palatable to some clients and therapists. In particular, VR may be a large selling point for young male and female military veterans with PTSD. The use of technological may make therapy more like playing a therapeutic “video game” and remove some of the stigma or embarrassment associated with psychotherapy (Rothbaum, Hodges, Ready, Graap & Alarcon, 2001). Garcia-Palacios and colleagues (2002) found that among undergraduate students, virtual reality exposure treatment for spider phobia was greatly preferred to traditional in-vivo exposure (Garcia-Palacios, Hoffman, Carlin, Furness, & Botella, 2002). However, it should be noted that when included as options for PTSD treatment, exposure with VR was rated as one of the five lowest preferred treatments (Tarrier, et al., 2006). Other efforts to increase the utilization of exposure might be aimed at clinicians themselves. Insufficient training in the delivery of exposure therapy appears to be one, but perhaps not the most important reason for therapist underutilization (Becker et al., 2004). Clinicians who are concerned about the well being of their patients may be reassured that not only is exposure therapy acceptable to many individuals, it is in fact, preferred.
In summary, despite concerns to the contrary, the current treatment preference literature shows that exposure treatment is a well accepted and preferred treatment for trauma-related difficulties. Across a number of studies, whether given a forced choice between treatments or allowed to rank preference among a number of treatments, exposure therapy is consistently rated as one of the more preferred treatment options. Despite this preference, exposure therapy remains underutilized, and efforts to increase utilization must examine the factors that contribute to treatment preference. The studies reviewed above show that the strongest predictor of treatment preference for exposure are client beliefs. This suggests that treatment-seeking clients enter a clinician’s office with clearly thought out beliefs about how treatment will work, if treatment will work, and whether or not they need treatment. Each of these types of beliefs affects treatment preference in powerful ways and should be incorporated into treatment rationales by clinicians to facilitate good treatment matches for clients.
Acknowledgments
This work was supported in part by grants from the National Institutes of Mental Health, F31 MH077483 (PI: Jaeger), R01 MH066347 (PI: Zoellner) and R01 MH066348 (PI: Feeny).
References
- Addis ME, Carpenter KM. The treatment rational in cognitive behavioral therapy: psychological mechanisms and clinical guidelines. Cognitive and Behavioral Practice. 1999;7:147–156. [Google Scholar]
- Addis ME, Jacobson NS. A closer look at the treatment rationale and homework compliance in cognitive therapy for depression. Cognitive Therapy and Research. 2000;24:313–326. [Google Scholar]
- Angelo FN, Miller HE, Zoellner LA, Feeny NC. “I need to talk about it”: A qualitative analysis of trauma-exposed women’s reasons for treatment choice. Behavior Therapy. 2008;39:13–21. doi: 10.1016/j.beth.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH. Psychological treatments. American Psychologist. 2004;59:869–878. doi: 10.1037/0003-066X.59.9.869. [DOI] [PubMed] [Google Scholar]
- Becker CB, Darius E, Schaumberg K. An analog study of patient preferences for exposure versus alternative treatments for posttraumatic stress disorder. Behaviour Research and Therapy. 2007;45:2861–28.73. doi: 10.1016/j.brat.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Becker CB, Zayfert C, Anderson E. A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy. 2004;42:277–292. doi: 10.1016/S0005-7967(03)00138-4. [DOI] [PubMed] [Google Scholar]
- Benkert O, Graf-Morgenstern M, Hillert A, Sandmann J, et al. Public opinion on psychotropic drugs: An analysis of the factors influencing acceptance or rejection. Journal of Nervous and Mental Disease. 1997;185(3):151–158. doi: 10.1097/00005053-199703000-00004. [DOI] [PubMed] [Google Scholar]
- Bedi N, Chilvers C, Churchill R, Dewey M, Duggan C, Fielding K, Gretton V, Miller P, Harrison G, Lee A, Williams I. Assessing effectiveness of treatment of depression in primary care. British Journal of Psychiatry. 2000;177:312–318. doi: 10.1192/bjp.177.4.312. [DOI] [PubMed] [Google Scholar]
- Beutler LE, Bergan J. Value change in counseling and psychotherapy: A search for scientific credibility. Journal of Consulting Psychology. 1991;38:16–24. [Google Scholar]
- Bradley R, Green J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68(5):748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Campbell R, Pennebaker J. The secret life of pronouns: flexibility in writing style and physical health. Psychological Science. 2003;14(1):60–65. doi: 10.1111/1467-9280.01419. [DOI] [PubMed] [Google Scholar]
- Chilvers C, Dewey M, Fielding K, Gretton V, Miller P, Palmer B, Weller D, Churchill R, Williams I, Bedi N, Duggan C, Lee A, Harrison G. British Medical Journal. 2001;322:1–5. doi: 10.1136/bmj.322.7289.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran B, Pruitt L, Fukuda S, Zoellner L, Feeny N. Reasons underlying treatment preference: An exploratory study. Journal of Interpersonal Violence. 2007;23:276–291. doi: 10.1177/0886260507309836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper L, Gonzales J, Gallo J, Rost K, Meredith L, Rubenstein L, Wang N, Ford D. The acceptability of treatment for depression among African-American, Hispanic, and White primary care patients. Medical Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ, Snow RE. Aptitudes and instructional methods. New York: Wiley; 1977. [Google Scholar]
- Davidson J, Foa E. Diagnostic issues in posttraumatic stress disorder: Considerations for the DSM-IV. Journal of Abnormal Psychology. 1991;100:346–355. doi: 10.1037//0021-843x.100.3.346. [DOI] [PubMed] [Google Scholar]
- Difede J, Cukor J, Patt I, Giosan C, Hoffman H. The application of virtual reality to the treatment of PTSD following the WTC attack. In: Yehuda R, editor. Psychobiology of posttraumatic stress disorders: A decade of progress. Malden, MA: Blackwell Publishing; 2006. pp. 500–501. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment preferences among depressed primary care patients. Journal of General Internal Medicine. 2000;15:527–534. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeny N, Zoellner L, Mavissakalian, Roy-Byrne What would you choose? Sertraline or prolonged exposure for chronic PTSD. 2008 doi: 10.1002/da.20588. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeny N, Zoellner L, Kahana S. Does what we say matter? A manipulation of the content of treatment rationales regarding PTSD treatment options. 2008 Manuscript submitted for publication. [Google Scholar]
- Fennel MJV, Teasdale JD. Cognitive therapy for depression: Individual differences and the process of change. Cognitive Therapy and Research. 1987;11:253–271. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67(2):194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, Yadin E. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive–behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. New York: Guilford Press; 2000. [Google Scholar]
- Foa EB, Zoellner LA, Feeny NC, Hembree EA, Alvarez-Conrad J. Does imaginal exposure exacerbate PTSD symptoms? Journal of Consulting and Clinical Psychology. 2002;70:1022–1028. doi: 10.1037//0022-006x.70.4.1022. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Berman MI. Posttraumatic growth following sexual assault. In: Joseph S, Linley PA, editors. Trauma, recovery, and growth: Positive psychological perspectives on posttraumatic stress. Hoboken NJ: John Wiley; 2008. pp. 161–181. [Google Scholar]
- Garcia-Palacios A, Hoffman H, Carlin A, Furness TA, III, Botella C. Virtual reality in the treatment of spider phobia: a controlled study. Behaviour Research and Therapy. 2002;40:983–993. doi: 10.1016/s0005-7967(01)00068-7. [DOI] [PubMed] [Google Scholar]
- Goldstein B, Rosselli F. Etiological paradigms of depression: The relationship between perceived causes, empowerment, treatment preferences, and stigma. Journal of Mental Health. 2003;12(6):551–563. [Google Scholar]
- Groom C, Pennebaker J. Words. Journal of Research in Personality. 2002;36(6):615–621. [Google Scholar]
- Hayes SC, Kohlenberg BS, Melancon SM. Avoiding and altering rule-control as a strategy of clinical intervention. In: Hayes SC, editor. Rule-governed behavior: Cognition, contingencies, and instructional control. New York: Plenum Press; 1989. pp. 359–385. [Google Scholar]
- Hayes SC, Wilson KG. Some applied implications of contemporary behavior-analytic account of verbal events. The Behavior Analyst. 1993;16:301–383. doi: 10.1007/BF03392637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazlett-Stevens H, Craske M, Roy-Bryne P, Sherbourne CD, Stein MB, Bystritsky A. Predictors of willingness to consider medication and psychosocial treatment for panic disorder in primary care patients. General Hospital Psychiatry. 2002;24:316–321. doi: 10.1016/s0163-8343(02)00204-9. [DOI] [PubMed] [Google Scholar]
- Hembree E, Foa E. Interventions for trauma-related emotional disturbances in adult victimes of crime. Journal of Traumatic Stress. 2003;16(2):187–199. doi: 10.1023/A:1022803408114. [DOI] [PubMed] [Google Scholar]
- Hembree EA, Foa EB, Dorfan NM, Street GP, Kowlaski J, Tu X. Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress. 2004;16:555–62. doi: 10.1023/B:JOTS.0000004078.93012.7d. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Barlow DH, Papp LA, Detweiler MF, Ray SE, Shear MK, et al. Pretreatment attrition in a comparative treatment outcome study on panic disorder. American Journal of Psychiatry. 1998;155:43–47. doi: 10.1176/ajp.155.1.43. [DOI] [PubMed] [Google Scholar]
- Hoge C, Castro C, Messer S, et al. Combat duty in Iraq and Afghanistan, mental health problems and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology Science and Practice. 1994;1:138–156. [Google Scholar]
- Institute of Medicine. Treatment of PTSD: An assessment of the evidence. Washington, DC: National Academies Press; 2007. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Study. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Best CL. Some cautionary remarks on treating sexual assault victims with implosion. Behavior Therapy. 1984;15(4):421–423. [Google Scholar]
- Kushner MG, Sher KJ. The relation of treatment fearfulness and psychological service utilization: An overview. Professional Psychology: Research and Practice. 1991;22:196–203. [Google Scholar]
- Mitchell J, Bray G. Emergency Services Stress. Guidelines for preserving the health and careers of emergency services personnel. Edgewood Cliffs, NJ: Prentice Hall; 1990. [Google Scholar]
- Marks IM, Baer L, Greist JH, Park J, Bachofen M, Nakagawa A, Wenzel KW, Parkin JR, Manzo PS, Dottl SL, Mantle JM. Home self-assessment of obsessive-compulsive disorder: Use of a manual and a computer-conducted telephone interview: Two UK-US studies. British Journal of Psychiatry. 1998;172:406–412. doi: 10.1192/bjp.172.5.406. [DOI] [PubMed] [Google Scholar]
- Nadler A, Maler S, Friedman A. Effects of helper's sex, subject's sex, subject's androgyny, and self-evaluation on male's and female's willingness to seek and receive help. Sex Roles. 1984;10:327–339. [Google Scholar]
- Olfson M, Pincus H. Outpatient psychotherapy in the United States, I: volume, costs, and user characteristics. American Journal of Psychiatry. 1994;151(9):1281–1288. doi: 10.1176/ajp.151.9.1281. [DOI] [PubMed] [Google Scholar]
- Ozer E, Best S, Lipsey T, Weiss D. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Pennebaker J, Mehl M, Niederhoffer K. Psychological aspects of natural language use: Our words, our selves. Annual Review of Psychology. 2003;54:547–577. doi: 10.1146/annurev.psych.54.101601.145041. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Altman B, Greenwald E, Longpre RE, Macklin ML, Poire RE, Steketee GS. Psychiatric complication during flooding therapy for posttraumatic stress diosorder. Journal of Clinical Psychiatry. 1991;52:17–20. [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Altman B, Longpre RE, Poire RE, Macklin ML. Emotional processing and outcome of imaginal flooding therapy in Vietnam Veterans with chronic posttraumatic stress disorder. Comprehensive Psychiatry. 1996;37(6):409–418. doi: 10.1016/s0010-440x(96)90024-3. [DOI] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Griffin MG. How well does cognitive behavioral therapy treat symptoms of complex PTSD? An examination of child sexual abuse survivors within a clinical trial. CNS Spectrums. 2003;8:340–355. doi: 10.1017/s1092852900018605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum B, Astin MC, Marstellar F. Prolonged exposure versus eye movement desensitisation (EMDR) for PTSD rape victims. Journal of Traumatic Stress. 2005;18:607–616. doi: 10.1002/jts.20069. [DOI] [PubMed] [Google Scholar]
- Rothbaum BO. Virtual reality in the treatment of psychiatric disorders. CNS Spectrums. 2006;11(1):34. [Google Scholar]
- Rothbaum BO, Hodges LF, Ready D, Graap K, Alarcon RD. Virtual reality exposure treatment for Vietnam Veterans with posttraumatic stress disorder. Journal of Clinical Psychiatry. 2001;62(8):617–622. doi: 10.4088/jcp.v62n0808. [DOI] [PubMed] [Google Scholar]
- Roy-Bryne P, Berliner L, Russo J, Zatzick D, Pitman RK. Treatment preferences and determinants in victims of sexual and physical assault. The Journal of Nervous and Mental Disease. 2003;191(3):161–165. doi: 10.1097/01.NMD.0000055343.62310.73. [DOI] [PubMed] [Google Scholar]
- Schnurr P, Friedman M, Engel C. Cognitive behavioral therapy for posttraumatic stress disorder in women. The Journal of the American Medical Association. 2007;297:820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Seligman MEP. The effectiveness of psychotherapy: The Consumer Reports study. American Psychologist. 1995;50:956–974. doi: 10.1037//0003-066x.50.12.965. [DOI] [PubMed] [Google Scholar]
- Shelton R, Hollon S, Purdon S, Loosen P. Biological and psychological aspects of depression. Behavior Therapy. 1991;22:201–228. [Google Scholar]
- Street LL, Niederehe G, Lebowitz BD. Toward greater public health relevance for psychotherapeutic intervention research: An NIMH workshop report. Clinical Psychology: Science and Practice. 2000;7(2):127–137. [Google Scholar]
- Tanielian T, Jaycox L. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery [Monograph] Santa Monica, CA: RAND Corporation; 2008. [Google Scholar]
- Tarrier N, Pilgrim H, Sommerfield C, Fragher B, Reynolds M, Graham E, Barrowclough C. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67:13–18. doi: 10.1037//0022-006x.67.1.13. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Liversidge T, Gregg L. The acceptability and preference for the psychological treatment of PTSD. Behavior Research and Therapy. 2006;44:1643–1656. doi: 10.1016/j.brat.2005.11.012. [DOI] [PubMed] [Google Scholar]
- Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, Ogrodniczuk J. Comparative efficacy, speed and adverse effects of three PTSD treatments: Exposure therapy, EMDR, relaxation training. Journal of Consulting and Clinical Psychology. 2003;71(2):330–338. doi: 10.1037/0022-006x.71.2.330. [DOI] [PubMed] [Google Scholar]
- Ullman S. Correlates and consequences of adult sexual disclosure. Journal of Interpersonal Violence. 1996;11:554–571. [Google Scholar]
- Wilson G, Fairburn C. Treatments for eating disorders. In: Nathan P, Gorman J, editors. A guide to treatments that work. Oxford: University Press; 2002. [Google Scholar]
- Wang P, Berglund P, Olfson M, Pincus H, Wells K, Kessler R. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Wong E, Kim B, Zane N, Kim I, Huang J. Examining culturally based variables associated with ethnicity: Influences on credibility perceptions of empirically supported interventions. Cultural Diversity and Ethnic Minority Psychology. 2003;9(1):88–96. doi: 10.1037/1099-9809.9.1.88. [DOI] [PubMed] [Google Scholar]
- Wyatt GE. The sociocultural context of African American and White American women's rape. Journal of Social Issues. 1992;48:77–91. [Google Scholar]
- Zayfert C, Becker CB. Implementation of empirically supported treatments for PTSD: Obstacles and innovations. The Behavior Therapist. 2000;23:161–168. [Google Scholar]
- Zoellner L, Feeny N, Cochran B, Pruitt L. Treatment choice for PTSD. Behavior Research and Therapy. 2003;41:879–886. doi: 10.1016/s0005-7967(02)00100-6. [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Feeny NC, Rothbaum BO. Dissemination: Transforming care through transforming lives. Journal of Traumatic Stress. 2005;19:567–569. doi: 10.1002/jts.20172. [DOI] [PubMed] [Google Scholar]