Abstract
Objective
To identify women who are suffering from urinary incontinence but do not consult a physician and to identify reasons for this.
Design
Survey study as part of a randomized controlled trial that investigates the effects of a standardized assessment and evidence-based treatment on urinary incontinence in older women, the URINO project.
Setting
Female patients from general practices in the Northern part of the Netherlands.
Patients
A total of 225 women of 55 years and older suffering from urinary incontinence.
Main outcome measures
Number of patients with urinary incontinence who are not registered by their GP as suffering from this, factors associated with help-seeking behaviour, and reasons for not seeking help.
Results
Of the 225 patients, 143 (64%) were not registered by their GP as suffering from urinary incontinence. These women were more often younger and had lower levels of distress due to their urogynaecological symptoms. The most common reason for not consulting a GP was that patients considered their symptoms not to be serious enough.
Conclusion
The prevalence of older women with urinary incontinence who do not seek help is high. Help-seeking behaviour is associated with increasing age and higher levels of distress caused by the symptoms. Younger patients more often hesitate to consult their GP if they perceive their symptoms to be relatively mild.
Key Words: Family practice, female, patient acceptance of health care, primary health care, urinary incontinence
Introduction
Urinary incontinence is a very common health problem among older women: about one in three women suffers from it [1]. Though it is not a life-threatening condition, it can affect quality of life adversely. It may lead to social isolation, lack of self-confidence, shame, and feelings of depression [2–4]. Effective treatment options, such as pelvic floor physiotherapy, bladder training, and anticholinergic drugs, are available but underused, because only a minority of the affected patients seek help [5,6]. The main reasons for not seeking help are that the urinary incontinence is seen as a problem that must be self-managed and that it is a normal sequel of ageing which should be accepted [6–8]. Severity of the incontinence and a high impact of the symptoms on quality of life are identified as factors associated with seeking help [6–11].
The literature is equivocal regarding the role of age in help-seeking behaviour in urinary incontinence. Some authors found that older women are more likely to seek help than younger women, whereas others conclude the opposite [7,9,10]. Some factors potentially related to help-seeking behaviour have not been studied at all, for instance gender of the general practitioner (GP), frequency of contact with the GP, and comorbidity.
The aims of this study were to identify women who do not consult a professional for their incontinence symptoms, and to determine factors related to not seeking help and reasons for not seeking help.
Although effective treatment options for urinary incontinence in older women are available, only a minority of the patients seek help.
The main reason for not consulting is that patients consider their symptoms not serious enough.
Relatively young patients with low levels of distress hesitate to seek help.
Material and methods
Design
This survey study is part of the URINO project, a randomized controlled trial that investigates the effects of a standardized assessment and evidence-based treatment on urinary incontinence in older women.
Setting
The URINO project was conducted in 14 general practices in the northern part of the Netherlands and started in January 2008. In the Netherlands, the GP is a gatekeeper: patients may consult a medical specialist only after obtaining a referral from their GP.
Patients
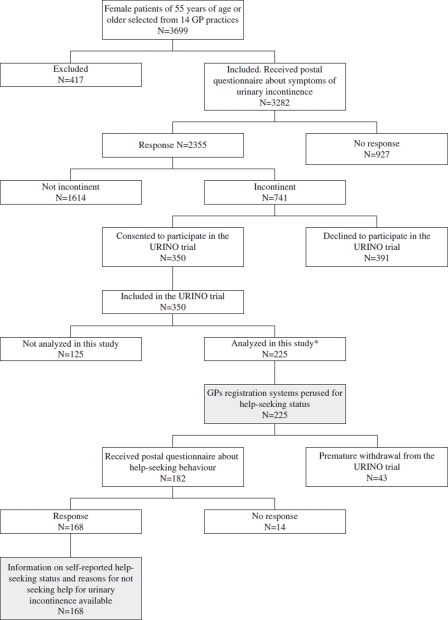
All female patients of 55 years and older were asked by their GP to complete a screening questionnaire on the presence of symptoms of urinary incontinence. Urinary incontinence was defined as involuntary leakage of urine once a month or more. Patients who reported urinary incontinence were invited to participate in the trial. They were included after they provided informed consent. For this study, data from the first 225 consecutive participants of the URINO project were analysed (Figure 1).
Figure 1.
The study population.
Note: *The first 225 participants in the URINO project.
Data collection
Data were derived from the GPs’ registration files and the baseline assessment of the URINO project. The GPs’ registration files were used to obtain information on whether the patients were known by their GP as suffering from urinary incontinence, their consultation behaviour in the three months preceding the inclusion, use of medication for chronic diseases, and comorbidity (the weighted Charlson Index) [12].
From the baseline measurement of the URINO project information was obtained on age, education level, and sexual activity. Also several validated questionnaires were used: the ICIQ-UI SF (Incontinence Consultation on Incontinence Questionnaire, which measures symptoms and impact of urinary incontinence), the ISI (Incontinence Severity Index, consisting of two questions regarding frequency and amount of leakage), UDI (Urogenital Distress Inventory) combined with the IIQ (Incontinence Impact Questionnaire) (which both measure health-related quality of life in multiple domains), EQ5D (EuroQol 5 Dimensions, for measuring general quality of life), and the GARS (Groningen Activity Restriction Scale, a two-domain questionnaire regarding functional status) [13–22].
For this survey, a questionnaire on help-seeking behaviour was developed. Patients were asked if they had consulted their GP for urinary incontinence. If a patient had not visited her GP for urinary incontinence, she was invited to explain her decision not to consult her GP for this problem (open question). Subsequently, she was asked to mark one or more of the reasons that are mentioned in Table III, a list of items derived from the literature [6,7,9].
Table III.
Reasons for not consulting the general practitioner for urinary incontinence.
| Total (n = 143) | |
| I think my involuntary loss of urine is not severe enough to consult my general practitioner; n (%) | 105 (73.4) |
| I have found a way to cope with it; n (%) | 82 (57.3) |
| I think involuntary loss or urine is a normal sequel of ageing; n (%) | 67 (46.9) |
| I think that there is no cure for my involuntary loss of urine; n (%) | 34 (23.8) |
| My general practitioner didn't ask me about involuntary loss of urine; n (%) | 29 (20.3) |
| I have other health problems which take priority; n (%) | 15 (10.5) |
| I feel uncomfortable at inconveniencing my general practitioner with involuntary loss of urine; n (%) | 17 (11.9) |
| I think my general practitioner would ignore my involuntary loss of urine; n (%) | 17 (11.9) |
| I am embarrassed to discuss involuntary loss of urine with my general practitioner; n (%) | 7 (4.9) |
| I think that the treatment options for involuntary loss of urine are too demanding on me; n (%) | 7 (4.9) |
| I think that my involuntary loss of urine is a transitory problem; n (%) | 5 (3.5) |
Statistical analysis
A multi-level analysis was conducted to address the factors related to help-seeking behaviour. In our data, individual patients (level 1) were nested within practices (level 2). Initially, univariate multi-level analysis was performed to determine the ORs of the several patient characteristics. Variables that showed a significant association in the univariate analysis were fitted in a subsequent multivariate multi-level logistic regression model. A best subset stepwise forward procedure was followed to develop a prediction model for not seeking help.
Information derived from the questionnaires was analysed with descriptive statistics. To identify women who did not seek help, the three most frequent reported reasons for not seeking help were identified and analysed in the same way as described for the help-seeking behaviour: initially the potential predictive factors were tested univariately and only a significant association between a factor and the outcome “seek help” led to fitting that variable in the multivariate model. Data were analysed by using SPSS 16.0 and MLwiN 2.19. A p-value of < 0.05 was considered statistically significant.
Results
Patient characteristics
Of the 225 participants, 143 (64%, 95% CI 57.3–69.9) were not registered by their GP as suffering from urinary incontinence. The mean age of these women was 63.81 (SD 7.24), whereas among women with known urinary incontinence the mean age was 69.93 (SD 9.57) (Table I). The women with known urinary incontinence more often had a male GP in a rural practice area; the women who were not known more often had a female GP and were living in an urban area.
Table I.
Baseline characteristics of the study population (known and unknown by the GP as having urinary incontinence).
| Known (n = 82) | Not known (n = 143) | |
| Age at baseline in years; mean (SD) | 69.39 (9.57) | 63.81 (7.24) |
| Education level | ||
| Low; n (%) | 29 (35.4) | 31 (21.8) |
| Average; n (%) | 35 (42.7) | 64 (45.1) |
| High; n (%) | 18 (22.0) | 47 (33.1) |
| Difference in age between patient and GP; mean (SD) | 23.2 (11.1) | 18.2 (11.5) |
| Male GP; n (%) | 56 (68.3) | 70 (49.0) |
| Location practice rural; n (%) | 55 (67.1) | 81 (56.6) |
| Self-reported type of incontinence: | ||
| Stress incontinence; n (%) | 11 (14.7) | 48 (36.6) |
| Urge incontinence; n (%) | 20 (26.7) | 20 (15.3) |
| Mixed incontinence; n (%) | 44 (58.7) | 63 (48.1) |
| Severity of the incontinence according to the ISI score:* | ||
| Slight; n (%) | 12 (16.0) | 43 (32.3) |
| Moderate; n (%) | 33 (44.0) | 68 (51.1) |
| Severe and very severe; n (%) | 30 (40.0) | 22 (16.5) |
| Urinary incontinence during sexual intercourse; n (%) | 9 (31.0) | 14 (21.5) |
| Number of medications for chronic diseases; median (IQR) | 2 (0–5) | 1 (0–3) |
| Total number of consultations; median (IQR) | 11 (7–19) | 9 (4–16) |
| Number of home visits; median (IQR) | 0 (0–1) | 0 (0–0) |
| Charlson index for comorbidity; median (IQR) | 0 (0–1) | 0 (0–1) |
| UDI score for distress caused by urogynaecological symptoms; median (IQR)* | 15.9 (8.0–28.0) | 9.6 (6.9–15.1) |
| IIQ score for psychological impact of urinary incontinence; median (IQR)* | 0.0 (0.0– 4.8) | 0.0 (0.0– 0.0) |
| EQ5D score for health outcome and utilities; median (IQR)* | 0.8 (0.7– 0.9) | 0.8 (0.8– 1.0) |
| GARS score for functional status; median (IQR)* | 20.0 (18.0–24.0) | 18.0 (18.0–21.0) |
Notes: *ISI: Incontinence Severity Index; UDI: Urogenital Distress Inventory; IIQ: Incontinence Impact Questionnaire; EQ5D: EuroQol 5 Dimension; GARS: Groningen Activity Restriction Scale.
Factors associated with help-seeking behaviour
A younger age of the patient (OR 0.91; 95% CI 0.87–0.96) and lower levels of distress due to the urogynaecological symptoms (UDI score OR 0.95; 95% CI 0.92–0.98) proved to be significant predictors for not being known by the GP as suffering from urinary incontinence (Table II).
Table II.
Factors related to not seeking help for urinary incontinence.
| Univariate multilevel analysis |
Multivariate multilevel analysis |
||||
| OR (95% CI) | p | OR (95% CI) | p | ||
| * | Age at baseline | 0.93 (0.89– 0.96) | < 0.01 | 0.91 (0.87–0.96) | < 0.01 |
| UDI score for distress caused by urogynaecological symptoms§ | 0.95 (0.92– 0.98) | < 0.01 | 0.95 (0.92–0.98) | < 0.01 | |
| † | Age of patient minus age of GP | 0.94 (0.91– 0.97) | < 0.01 | ||
| Education level: | |||||
| Low | 1 | ||||
| Average | 1.66 (0.84– 3.26) | 0.14 | |||
| High | 2.50 (1.16– 5.37) | 0.02 | |||
| Gender GP | |||||
| Male | 1 | 0.01 | |||
| Female | 2.25 (1.27– 3.97) | ||||
| Self-reported type of incontinence: | |||||
| Stress incontinence | 1 | ||||
| Urge incontinence | 0.24 (0.10–0.60) | < 0.01 | |||
| Mixed incontinence | 0.34 (0.16–0.72) | < 0.01 | |||
| Number of prolonged medications | 0.88 (0.80– 0.98) | 0.01 | |||
| Total consultations | 0.96 (0.94– 0.99) | 0.01 | |||
| IIQ score for psychological impact of urinary incontinence§ | 0.95 (0.91– 0.99) | 0.01 | |||
| EQ5D score for health outcome and utilities§ | 4.34 (1.02–18.42) | 0.05 | |||
| GARS score for functional status§ | 0.92 (0.87– 0.97) | < 0.01 | |||
| ‡ | Severity of incontinence according to the ISI score:§ | 1 | |||
| Slight | 0.64 (0.29–1.38) | 0.25 | |||
| Moderate | 0.22 (0.09–0.51) | < 0.01 | |||
| Severe and very severe | |||||
Notes: *Variables included in the multivariate multilevel model; †variables removed from the multivariate multilevel model; ‡variables not included in the multivariate multilevel analysis; §UDI: Urogenital Distress Inventory; IIQ: Incontinence Impact Questionnaire; EQ5D: EuroQol 5 Dimension; GARS: Groningen Activity Restriction Score; ISI: Incontinence Severity Index.
Reasons for not seeking help
The most frequently mentioned reason for not consulting the GP for urinary incontinence was that the symptoms were not severe enough (n = 105, 73.4%) (Table III). Severity of the incontinence (moderate: OR 0.14; 95% CI 0.03–0.72 and (very) severe: OR 0.14; 95% CI 0.02–0.81) and distress from the incontinence symptoms (UDI score OR 0.93; 95% CI 0.88–0.98) were associated with this reason for not seeking help (Table IV).
Table IV.
Factors related to the top three reasons for not seeking help.
| Urinary incontinence is not severe enough |
|||
| OR (95%CI) | p-value | ||
| * | Severity of incontinence according to the ISI score:‡ |
||
| Slight | 1 | 0.02 | |
| Moderate | 0.14 (0.03–0.72) | 0.03 | |
| Severe and very severe | 0.14 (0.02–0.81) | ||
| UDI score for distress caused by urogynaecological symptoms‡ |
0.93 (0.88–0.98) | 0.01 | |
| † | Age at baseline | ||
| Charlson index for comorbidity | |||
| Home visits | |||
| IIQ score for psychological impact of urinary incontinence‡ |
|||
| Education level | |||
| |
Age of GP at baseline |
||
| I have found a way to cope with it |
|||
| |
|
OR (95%CI) |
p-value |
| * | Age of GP at baseline | 1.09 (1.02– 1.15) | 0.01 |
| Urinary incontinence during sexual intercourse | 5.22 (1.15–23.60) | 0.03 | |
| † |
Self-reported type of incontinence |
|
|
| Urinary incontinence is a normal sequel of ageing |
|||
| |
|
OR (95%CI) |
p-value |
| * | Age at baseline | 1.07 (1.02–1.11) | 0.01 |
| Location of practice: | |||
| urban | 1 | ||
| rural | 0.38 (0.15–0.96) | 0.04 | |
| † | Self-reported type of incontinence | ||
Notes: *Variables included in the multivariate multilevel model; †variables removed from the multivariate multilevel model; ‡ISI: Incontinence Severity Index; UDI: Urogenital Distress Inventory; IIQ: Incontinence Impact Questionnaire.
The second most frequently mentioned reason was that women had found a way to cope with their symptoms of incontinence (n = 82, 57.3%). These women more often had an older GP (OR 1.09; 95% CI 1.02–1.15) and more often experienced urinary incontinence during sexual intercourse (OR 5.22; 95% CI 1.15–23.60) as compared with women reporting other reasons, although the last result must be interpreted with caution because of the relatively high number of missing values concerning the intercourse variable.
Considering urinary incontinence as a normal sequel of ageing was reported by 67 women (46.9%); these women were more often older (OR 1.07; 95% CI 1.02–1.11) than the women who did not give that reason. Their GP practice was less often located at a rural region (OR 0.38; 95% CI 0.15–0.96).
The fourth most mentioned reason for not seeking help was “I think there is no cure”.
Discussion
Principal findings
Help-seeking behaviour of older women in primary care with urinary incontinence was studied in women of 55 years and older who were participating in a RCT. In total, 64% (95% CI: 57.3–69.9) of the participating patients with urinary incontinence were not known by their GP as suffering from this problem. These women were younger and had relatively low levels of distress. Although GP characteristics such as age, gender, and urbanization grade showed an association with help-seeking behaviour in the univariate analyses, in the final multivariate analysis these variables disappeared from the model. The main reason given for not seeking help was: “The symptoms are not severe enough”.
Strengths and limitations
Although help-seeking behaviour of women with urinary incontinence has been frequently studied, we found that to the best of our knowledge this is the first study that matches information from the patient with the GPs’ registration systems. This could lead to new insights, because it uses information both from a doctor's perspective (“Urinary incontinence should be the main reason for consultation”) and from a patient's perspective (“I have raised this problem”).
A possible limitation of this study is that the study population is not a random sample of the total population of older women with urinary incontinence, since it included women willing to participate in a trial. However, with a response rate of 72% on the screening questionnaire (2355 out of 3282 forms were returned) and 92% on the questionnaire about help-seeking behaviour (168 out of 182), we are confident that our data are robust.
Comparison with existing literature
In this study, we found that 64% (95%-CI 57.3–69.9) of the women had never discussed their problem of urinary incontinence with their GP. Peters et al. found a prevalence of undiagnosed urinary incontinence in women of 65 years and older of 86% (95% CI: 80.7–90.6), while Dugan et al. found a prevalence of 70% (95% CI: 62.4–78.2) in women of 60 years and older [8,9]. An explanation for these varying prevalences might be that the definition of urinary incontinence in studies differs, especially concerning the time-period in which symptoms occurred, as well as the definition of help-seeking behaviour, the way women were recruited, and the age categories of the study populations.
Although not new – it has been reported by others – it is still puzzling that women as they become older are more likely to be known by their GP as having urinary incontinence. A good explanation has not been found so far [9,23–25]. It could be explained by an unidentified interaction effect with age, like severity of the incontinence. However, no evidence of such interaction was present in our final regression model. Another explanation could be that a GP has a higher index of suspicion of urinary incontinence in older women and as a consequence may ask more frequently for symptoms.
Less unexpected is our finding that women with relatively low levels of distress due to their symptoms are less likely to seek help. This corresponds with the results of previous studies [6,7,9].
In our study, the most frequently reported reason for not seeking help for urinary incontinence was that the symptoms were considered not severe enough. Teunissen et al. reported the same finding [11]. That urinary incontinence is a normal sequel of ageing was reported by almost half of the patients as a reason for not seeking help. Commercials about absorbent products, in which remarkably happy older women experience virtually no discomfort from urinary incontinence, are not contributing to a change in the perception of this problem. It is surprising that a quarter of our study population assumed that urinary incontinence cannot be cured. This means that informing women that urinary incontinence can be treated effectively is still very important.
Implications of the study and future research
In this study, the most common reason for not consulting a GP was that patients considered their symptoms not to be severe enough. This knowledge may be useful. Information campaigns about urinary incontinence, initiated from the general practice or publicly funded, might make patients more aware about this problem and the available good treatment options, even when their symptoms are relatively mild.
This study also demonstrates that women who do not seek help for urinary incontinence are relatively young with lower levels of distress. As a consequence, GPs should be more attentive to the presence of urinary incontinence in relatively young women, as this group may not easily consult a GP for incontinence but could benefit from treatment, and also to prevent further deterioration of symptoms. Perhaps all women above 55 years should be systematically screened for urinary incontinence, as already suggested by Rohr et al. [26]. The effectiveness of a proactive approach towards older women, for example by using a single question intended to gather information on the presence of urinary incontinence during routine medical check-ups of elderly women in general practice, should be subject to further investigation. In this study we describe the characteristics of the women who hesitate to seek help. An intervention study that has already started will have to show which women will profit from treatment of their incontinence and should be encouraged to seek help.
Ethical approval
The URINO project was approved by the Medical Ethical Committee of the University of Groningen, the Netherlands.
Funding support
The Health Research and Development Council (ZonMW) in the Netherlands funded the URINO-project (grant number 170882301).
Conflicts of interest
All authors declare they have no conflicts of interest.
References
- 1.Anger JT, Saigal CS, Litwin MS. The prevalence of urinary incontinence among community dwelling adult women: Results from the National Health and Nutrition Examination Survey. J Urol. 2006;175:601–4. doi: 10.1016/S0022-5347(05)00242-9. [DOI] [PubMed] [Google Scholar]
- 2.Ko Y, Lin SJ, Salmon JW, Bron MS. The impact of urinary incontinence on quality of life of the elderly. Am J Manag Care. 2005;11:S103–S111. [PubMed] [Google Scholar]
- 3.Lagro–Janssen T, Smits A, Van Weel C. Urinary incontinence in women and the effects on their lives. Scand J Prim Health Care. 1992;10:211–16. doi: 10.3109/02813439209014063. [DOI] [PubMed] [Google Scholar]
- 4.Teunissen D, Van den Bosch W, Van Weel C, Lagro-Jansen T. “It can always happen”: The impact of urinary incontinence on elderly men and women. Scand J Prim Health Care. 2006;24:166–73. doi: 10.1080/02813430600739371. [DOI] [PubMed] [Google Scholar]
- 5.Fonda D, Woodward M, D'Astoli M, Chin WF. Sustained improvement of subjective quality of life in older community-dwelling people after treatment of urinary incontinence. Age Ageing. 1995;24:283–86. doi: 10.1093/ageing/24.4.283. [DOI] [PubMed] [Google Scholar]
- 6.Teunissen D, Van Weel C, Lagro-Janssen T. Urinary incontinence in older people living in the community: Examining help-seeking behaviour. Br J Gen Pract. 2005;55:776–82. [PMC free article] [PubMed] [Google Scholar]
- 7.Kinchen KS, Burgio K, Diokno AC, Fultz NH, Bump R, Obenchain R. Factors associated with women's decisions to seek treatment for urinary incontinence. J Womens Health (Larchmt) 2003;12:687–98. doi: 10.1089/154099903322404339. [DOI] [PubMed] [Google Scholar]
- 8.Peters TJ, Horrocks S, Stoddart H, Somerset M. Factors associated with variations in older people's use of community-based continence services. Health Soc Care Community. 2004;12:53–62. doi: 10.1111/j.1365-2524.2004.00468.x. [DOI] [PubMed] [Google Scholar]
- 9.Dugan E, Roberts CP, Cohen SJ, Preisser JS, Davis CC, Bland DR, et al. Why older community-dwelling adults do not discuss urinary incontinence with their primary care physicians. J Am Geriatr Soc. 2001;49:462–5. doi: 10.1046/j.1532-5415.2001.49094.x. [DOI] [PubMed] [Google Scholar]
- 10.Hagglund D, Walker-Engstrom ML, Larsson G, Leppert J. Quality of life and seeking help in women with urinary incontinence. Acta Obstet Gynecol Scand. 2001;80:1051–5. [PubMed] [Google Scholar]
- 11.Teunissen D, Lagro-Jansen T. Urinary incontinence in community dwelling elderly: Are there sex differences in help-seeking behaviour? Scand J Prim Health Care. 2004;22:209–16. doi: 10.1080/02813430410006666. [DOI] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23:322–30. doi: 10.1002/nau.20041. [DOI] [PubMed] [Google Scholar]
- 14.D'Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders, I: The acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract. 1994;11:260–6. doi: 10.1093/fampra/11.3.260. [DOI] [PubMed] [Google Scholar]
- 15.Kempen GIJM, Miedema I, Ormel J, Molenaar W. The assessment of disability with the Groningen Activity Restriction Scale. Conceptual framework and psychometric properties. Soc Sci Med. 1996;43:1601–10. doi: 10.1016/s0277-9536(96)00057-3. [DOI] [PubMed] [Google Scholar]
- 16.Kempen GIJM, Brilman EI, Heyink JW, Ormel J. [Measurement of general health with the MOS Short-Form General Health Survey (SF-20). A manual] Groningen: Northern Center for Health Issues; 1995. [Google Scholar]
- 17.Lamers LM, Stalmeier PF, McDonnell J, Krabbe PF, Van Busschbach JJ. [Measuring the quality of life in economic evaluations: the Dutch EQ-5D tariff] Ned Tijdschr Geneeskd. 2005;149:1574–8. [PubMed] [Google Scholar]
- 18.Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12) Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:164–8. doi: 10.1007/s00192-003-1063-2. [DOI] [PubMed] [Google Scholar]
- 19.Sandvik H, Espuna M, Hunskaar S. Validity of the incontinence severity index: Comparison with pad-weighing tests. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:520–4. doi: 10.1007/s00192-005-0060-z. [DOI] [PubMed] [Google Scholar]
- 20.Thirlaway K, Fallowfield L, Cuzick J. The Sexual Activity Questionnaire: A measure of women's sexual functioning. Qual Life Res. 1996;5:81–90. doi: 10.1007/BF00435972. [DOI] [PubMed] [Google Scholar]
- 21.Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: The Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn. 1995;14:131–9. doi: 10.1002/nau.1930140206. [DOI] [PubMed] [Google Scholar]
- 22.Van der Vaart CH, De Leeuw JRJ, Roovers JPWR, Heintz APM. Measuring health-related quality of life in women with urogenital dysfunction: The urogenital distress inventory and incontinence impact questionnaire revisited. Neurourol Urodyn. 2003;22:97–104. doi: 10.1002/nau.10038. [DOI] [PubMed] [Google Scholar]
- 23.Hannestad YS, Rortveit G, Hunskaar S. Help-seeking and associated factors in female urinary incontinence. The Norwegian EPINCONT Study: Epidemiology of Incontinence in the County of Nord-Trondelag. Scand J Prim Health Care. 2002;20:102–7. [PubMed] [Google Scholar]
- 24.Koch LH. Help-seeking behaviors of women with urinary incontinence: An integrative literature review. J Midwifery Women's Health. 2006;51:e39–44. doi: 10.1016/j.jmwh.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 25.O'Donnell M, Lose G, Sykes D, Voss S, Hunskaar S. Help-seeking behaviour and associated factors among women with urinary incontinence in France, Germany, Spain and the United Kingdom. Eur Urol. 2005;47:385–92. doi: 10.1016/j.eururo.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 26.Rohr G, Stovring H, Christensen K, Gaist D, Nybo H, Kragstrup J. Characteristics of middle-aged and elderly women with urinary incontinence. Scand J Prim Health Care. 2005;23:203–8. doi: 10.1080/02813430500362803. [DOI] [PubMed] [Google Scholar]