Abstract
Objective
To investigate to what extent a physician's place of graduation is associated with the physician choosing a career as a general practitioner (GP), and identify factors in the curriculum that could predict a general practice career.
Design
Cross-sectional study based on the membership database of the Norwegian Medical Association.
Setting
Physicians working in Norway who graduated from four domestic medical schools, five other countries, and three groups of countries. Physicians were categorized according to their main professional activity as GPs, hospital physicians, and researchers.
Subjects
A total of 2836 medical physicians who were working in Norway during 2010 and graduated from medical school between 2002 and 2005.
Main outcome measures
Percentage and odds ratio for subjects working as a GP in Norway during 2010. Descriptive data for pre-graduate general practice education in Norwegian medical schools were also analysed.
Results
Compared with the University of Oslo, there was a significantly higher proportion of GPs among physicians who had graduated from Denmark (OR 2.9, 95% CI 1.9–4.5), Poland (OR 2.0, 95% CI 1.4–2.9), Sweden (OR 1.8, 95% CI 1.0–3.1), and Trondheim (Norway) (OR 1.5, 95% CI 1.1–2.0). Across the four Norwegian medical schools, there were significant associations between choosing a general practice career and the sum of pre-graduate educational hours regarding general practice, general practice preceptorship, and the number of GP teachers.
Conclusion
The physician's place of graduation appears to be associated with career choice. The universities’ total contribution in pre-graduate general practice education may be associated with future GP career choice.
Key Words: General practice, hospital physician, medical education, research personnel
There is no documentation on how place of graduation for Norwegian physicians is associated with the likelihood of ending up practising as a GP.
This study found significant differences in the likelihood of working as GP based on where the physician graduated from medical school.
Universities’ total contribution to general practice teaching seems to be associated with its graduates’ future GP career choice.
Introduction
Norway has approximately 20 000 active physicians. Based on membership in the Norwegian medical association, these physicians can be categorized as general practitioners (GP), hospital physicians or researchers [1]. In the coming years, Norway will need more GPs.
Several factors affect the final career choice for physicians. The curriculum will be the same for all physicians from the same medical school, and this might partly explain different career choices among physicians educated at different universities. International studies have found associations between a medical school and its graduates’ career choices [2,3]. We could not identify any Scandinavian study investigating this association.
Based on a study population of all physicians working in Norway in 2010 who graduated during 2002–2005, our objectives for this study were to (1) estimate the prevalence of general practice, hospital, and researcher career choices among physicians who graduated from different universities in Norway and from different countries abroad, and (2) investigate whether descriptive data from Norwegian medical curricula could explain differences in the likelihood of graduates working in general practice.
Material and methods
The study's data were drawn from the membership database of the Norwegian Medical Association (NMA), which includes 95% of all physicians practicing in Norway. The database, which is based on input from each individual physician, lists the member's place and year of graduation, occupational branch, and PhD.
The independent predictor variable in this study was the physician's place of graduation. It was categorized into 12 groups: University of Oslo (Norway), University of Bergen (Norway), Norwegian University of Science and Technology, University of Tromsø (Norway), Sweden, Denmark, Germany, Hungary, Poland, Middle Europe (Slovakia, Czech Republic, Austria, Switzerland) and English-speaking countries (Australia, Canada, Ireland, Malta, Netherlands, United Kingdom), and other countries.
The University of Oslo educates the largest number of medical students in Norway; therefore we used it as the reference in variance analyses. Universities or countries that educated more than 100 Norwegian physicians during the study period were categorized separately. Due to general culture and medical curricula similarities, we split the remaining European countries into “Middle Europe” and “English-speaking countries”, including the Netherlands. The remaining “Other countries” consisted of 24 countries that each contributed < 10 Norwegian physicians during the study period (mean = 4). This mixed residual group will not be discussed further.
Tromsø in Norway started medical studies in 1973 and Trondheim in 1993. Oslo changed to a new curriculum in 1996. For data to be representative of today's medical curriculum in Norway, we included only physicians who started their medical education in 1996 or later.
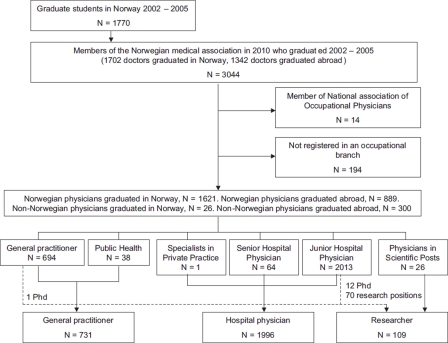
All the 3044 physicians in the NMA membership database who had graduated between 2002 and 2005 and who worked in Norway in 2010 were eligible. The NMA has seven occupational branches. We categorized the branches into three groups; these represent the dependent outcome variables in this study (Figure 1). Group A, GPs, combines the members of General Practitioners and Public Health groups, as physicians organized in Public Health have a long tradition of being GPs. Group B, Hospital physicians, combines Junior Hospital Physicians, Senior Hospital Physicians and Specialists in Private Practice. Group C, Researchers, initially consisted of Physicians in Scientific Posts. All physicians who had a PhD or who were registered in NMA with research position were re-categorized as researchers. Physicians who were organized as Occupational Physicians were excluded. A total of 194 physicians were excluded because of missing data on occupational branch membership. The total study population consisted of 2836 physicians (Figure 1). This article focuses mainly on GPs.
Figure 1.
Participants in the study.
To identify simple associations between university curriculum and a career as a GP, quantitative descriptive information regarding pre-graduate general practice education was obtained from the Norwegian universities (teaching hours on subjects relevant to general practice, the number of general practice teachers, and the hours of preceptorship in general practice). Each variable was ranked from 1 (lowest) to 4 (highest) and the rankings were summed.
The NMA membership database held information on the members’ age, sex, and citizenship. Age was categorized into three groups, with one-third of the study population in each group. Citizenship was categorized as Norwegian or non-Norwegian/immigrant. Confounding was evaluated by multivariate logistic regression and crosstab analyses of these variables according to occupation. Multivariate logistic regression adjusted for confounding. In multistratified analyses for sex, age, citizenship, and origin of education, only the results for the occupational choice by physicians graduated in Norway were considered.
We treated independent variables as categorical. Rankings of descriptive data had a Gaussian distribution and were treated as continuous variables in logistic regression analyses. We evaluated the assumption of linear trend between working as a GP and descriptive ranking through model comparison using a chi-squared test. The assumption of linearity could not be rejected (p > 0.05).
Results are presented as absolute number, mean, percentage, and adjusted odds ratio (OR) for appropriate confounders with 95% confidence intervals (CI). P-values < 5% were considered statistically significant and referred to as significant findings. SPSS 15.0 for Windows (SPSS Inc., Chicago, IL) was used for the statistical analyses.
Results
The study population consisted of 2836 physicians: 731 GPs (26%), 1996 hospital physicians (70%), and 109 researchers (4%) (see Figure 1). A total of 1189 physicians (42%) had graduated abroad; of these, 300 (25%) held foreign citizenship. Germany contributed the most immigrant physicians (242), while Denmark, Sweden, Iceland, and Finland contributed 115, 67, eight, and one physicians, respectively. The study population consisted of 1494 women (53%) and 1342 men (47%). The subjects’ mean age in 2010 was 33.7 years.
General practitioners
Compared with physicians who graduated from Oslo, physicians who graduated in Denmark (OR 2.9), Poland (OR 2.0), Sweden (OR 1.8), and from Trondheim (OR 1.5) were significantly more likely to have chosen a GP career (Table I). Age ≥ 35 years was an independent predictor significantly associated with working as a GP (OR 1.5, 95% CI 1.2–1.9). Among physicians who graduated in Norway, the likelihood of working as a GP was highest among Norwegian women ≥ 35 years who graduated from Trondheim (15/35; 43%).
Table I.
OR for occupation as general practitioner, hospital physician, or researcher based on origin of education.
| General practitioner |
Hospital physician |
Researcher |
|||||||||||
| Origin of education | n | (%) | OR1 | 95% CI | n | (%) | OR2 | 95% CI | n | (%) | OR1 | 95% CI | n |
| Oslo | 114 | 22 | Ref | 367 | 71 | Ref | 36 | 7 | Ref | 517 | |||
| Bergen | 132 | 25 | 1.2 | 0.9–1,6 | 380 | 71 | 1.0 | 0.8–1.3 | 22 | 4 | 0.5 | 0.3–0.9* | 534 |
| Trondheim | 92 | 29 | 1.5 | 1.1–2.0* | 217 | 68 | 0.9 | 0.6–1.2 | 12 | 4 | 0.5 | 0.2–0.4* | 321 |
| Tromsø | 75 | 27 | 1.3 | 0.9–1.9 | 192 | 70 | 0.9 | 0.7–1.3 | 8 | 3 | 0.4 | 0.2–0.9* | 275 |
| Sweden | 23 | 34 | 1.8 | 1.0–3.1* | 42 | 63 | 0.7 | 0.4–1.2 | 2 | 3 | 0.4 | 0.1–1.8 | 67 |
| Denmark | 54 | 47 | 2.9 | 1.9–4.5* | 59 | 51 | 0.5 | 0.3–0.7* | 2 | 2 | 0.3 | 0.1–1.1 | 115 |
| Germany | 33 | 13 | 0.5 | 0.4–0.8* | 200 | 83 | 2.0 | 1.3–2.9* | 9 | 4 | 0.5 | 0.3–1.1 | 242 |
| Hungary | 58 | 26 | 1.3 | 0.9–1.8 | 159 | 72 | 1.0 | 0.7–1.5 | 5 | 2 | 0.3 | 0.1–0.8* | 222 |
| Poland | 78 | 36 | 2.0 | 1.4–2.9* | 139 | 63 | 0.7 | 0.5–1.0* | 3 | 1 | 0.2 | 0.1–0.5* | 220 |
| Middle Europe | 10 | 24 | 1.2 | 0.6–2.5 | 30 | 73 | 1.1 | 0.6–2.3 | 1 | 2 | 0.3 | 0.1–2.3 | 41 |
| English-speaking countries | 37 | 20 | 1.0 | 0.6–1.5 | 140 | 77 | 1.3 | 0.9–1.9 | 8 | 4 | 0.5 | 0.2–1.1 | 185 |
| Other countries | 25 | 26 | 1.2 | 0.8–2.0 | 71 | 73 | 1.2 | 0.7–2.0 | 1 | 1 | 0.1 | 0.1–1.0* | 97 |
| Total | 731 | 26 | 1996 | 70 | 109 | 4 | 2836 | ||||||
Notes: 1Adjusted for age, 2adjusted for citizenship, *p < 0.05.
When curriculum type and descriptive variables of pre-graduate GP education were analyzed separately, there were no significant associations with a GP career. However, when descriptive data were ranked from 1 (lowest) to 4 (highest) and summed, Oslo's ranking sum was 5 while Trondheim's ranking sum was 10 (Table II). GPs had a significantly higher ranking sum than non-GPs (mean difference 0.2, 95% CI 0.03–0.4). There was a significant adjusted linear trend towards an increasing proportion of GPs with increasing ranking sum of the total contribution of pre-graduate education in general practice (OR 1.08, 95% CI 1.02–1.15).
Table II.
Descriptive data on number of graduated students, type of curriculum, and pre-graduate general practice education in Norwegian universities, ranked from 1 (lowest) to 4 (highest).
| UiO | UiB | UiT | NTNU | |||||
| Number of graduated students 2002–2005 | 601 | 553 | 291 | 325 | ||||
| Type of curriculum: | ||||||||
| PBL and integrated organ-based curriculum | X | X | X | |||||
| Traditional curriculum |
|
|
|
X |
|
|
|
|
| From Table 1: OR for working as a GP |
|
Ref |
|
1.2 |
|
1.3 |
|
1.5 |
| Descriptive data: | Ranking | Ranking | Ranking | Ranking | ||||
| Hours of preceptorship in general practice | 252 | 2 | 158 | 1 | 300 | 3 | 345 | 4 |
| Curriculum hours in general practice1 | 133 | 1 | 158 | 3 | 293 | 4 | 150 | 2 |
| General practice teachers/total positions | 8/6 | 2 | 15/8 | 3 | 15/5 | 1 | 25/11 | 4 |
| Sum ranking | 5 | 7 | 8 | 10 |
Notes: PBL = problem–based learning. UiO = University of Oslo, Norway. UiB = University of Bergen, Norway. UiT = University of Tromsø, Norway. NTNU = Norwegian University of Science and Technology. 1Based on total hours in general practice curriculum (lectures, seminars, communication training, GP skills training etc.). Does not include PBL hours.
Hospital physicians
Among all physicians from Norway, physicians who graduated from Oslo or Bergen were most likely to be working as a hospital physician. Physicians who graduated from Germany were significantly the highest in this respect (OR 2.0), while physicians who graduated from Denmark were lowest (OR 0.5) (see Table I). Norwegian citizenship was an independent predictor significantly associated with working as a hospital physician in Norway (OR 1.7, 95% CI 1.3–2.2). Among physicians who graduated in Norway, the probability of working as a hospital physician was highest among Norwegian males < 33 years who graduated from the University of Oslo (61/78; 78%).
Researchers
Compared with Oslo, the proportion of researchers was lower for physicians from all other origins (see Table I). Among physicians who graduated in Norway, the probability of working as a researcher was highest among Norwegian females < 33 years who graduated in Oslo (12/90; 13%).
Discussion
We found significant associations between the place of medical education and working as a GP. We could not identify any single variable from the Norwegian curriculums that could predict a GP outcome, but each university's total contribution to a general practice curriculum might be associated with the graduate's future choice of a general practice career.
A major strength of this study is that it includes almost all Norwegian physicians in the relevant cohorts. The study population represents 96% (1702/1770) of all physicians who graduated from medical schools in Norway from 2002 to 2005. The database had valid information regarding place of education and occupation as of September 2010. All physicians who graduated from the same university had the same curriculum programmes, teaching personnel and methods, leadership, and curricular context experience [4]. This represents a shared background that makes it possible to find differences between universities in their graduates’ career choices. No prior Scandinavian study has investigated the association between place of pre-graduate education and career choice among all Norwegian physicians.
One weakness of our study is that the NMA database did not have information on how far the physicians had progressed toward specialization, or whether they had changed occupational branch after graduation. Another weakness is that the study examined the physicians’ occupations during the first 5–8 years after graduation. At this point, a physician could still opt to change career. A Norwegian study found that 11% of Norwegian physicians change career to become GPs 5–10 years after graduation [5]. Another report found that 50% of all Norwegian physicians start their speciality program within 2.2 years after graduation [6]. By following physicians ≥ 5 years after graduation, we believed it reasonable that our study population represented their final occupational branch.
Unfortunately, the NMA's database is incomplete regarding members who hold PhD degrees and research positions. We have merged previous and present research to estimate the interest in research. Due to incomplete data and the small number of researchers, our results are not necessarily predictive of graduates choosing a future career in research.
Many factors are associated with a physician's choice of career, including career opportunities [5], working hours [7–9], on-duty hours [7,8], payment [2,7,8], prestige [10], and family situation [10]. The NMA's database did not record information on these factors. Personal preferences are likely to be independent of the place where a physician graduated, but we cannot rule out that some universities might attract a group of students with certain personal career preferences, biasing the results. Magnus investigated the mobility among students who graduated from Tromsø, and found that 56% of the physicians stayed in that same part of Norway [11]. This can be a confounder, because job opportunities for GPs might vary between parts of the country. We explored potential confounders and adjusted appropriately. However, as many factors influence career choice, we cannot rule out residual confounding.
It is difficult to conduct research on the effects of medical education [4]. There are mixed conclusions on how medical curricula influence choice of a general practice career [12]. In our study, curriculum type (problem-based learning [PBL] teaching) among the Norwegian medical schools was not associated with increasing proportions of GPs. Studies have found that role models [12], location of the university and work [13], and the use of excellent clinical teachers [14] appear to influence career choice. Evidence for the positive role of GPs and general practice in medical education is growing [15]. Differences between medical schools in the proportion of graduates choosing to be GPs have been partly associated in a meta-analysis with the number of required weeks’ study in family practice, and with each school's mission and funding sources [16]. Data on the quality of teaching, preceptorship, and role models in medical universities are hard to obtain. We obtained data on the quantitative variables “curriculum hours in general practice”, “general practice teachers”, and “hours of preceptorship in general practice” from the universities. They represent three important components in the general practice curriculum and we believe they shed light on the Norwegian universities’ resources, effort, and focus on general practice. These variables showed that the Norwegian universities with the highest ranking sum had the highest proportions of GPs. The results might indicate that it is not a single factor, but rather the universities’ total quantitative contribution in pre-graduate general practice education that might be associated with graduates’ choice of a general practice career.
The new health sector reform in Norway, the Coordination Reform, that will be initiated in January 2012 [17] makes the results of our survey particularly interesting. Norway needs to increase the proportion of GPs to meet the objectives of the reform, but political and administrative determination are required in order to accomplish this goal [18]. It might be necessary to import GPs if Norwegian universities cannot meet future demands for GPs. Our results give some indication that allocating more resources to pre-graduate GP education in medical schools could increase the proportion of GPs.
In conclusion, differences exist between universities in the proportion of physicians who choose a GP career after graduation. Many factors are linked to career preferences, yet the universities’ total contribution to general practice teaching appears to be associated with encouraging graduates to choose a career as a GP.
Ethics
The study was not based on identifiable data from individuals. The data were anonymous and did not contain sensitive information. Therefore, the Regional Ethics Committee for Medical Research was not involved.
Wesnes has received a grant from the Western Norway Regional Health Authority.
Wesnes and Bærheim are both employees at the University of Bergen and engaged in general practice teaching. Wesnes is presently also working as a GP; Bærheim formerly worked as a GP. Aasland is employed by the Norwegian Medical Association.
Declaration of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Acknowledgements
The authors would like to thank Elin Olaug Rosvold at the University of Oslo, Randi Oen at the University of Bergen, Siri Forsmo at the University of Trondheim, and Knut Holtedahl at the University of Tromsø for contributing descriptive data on the general practice curriculum hours, preceptorship, and GP teachers at their respective institutions.
References
- 1.Taraldset A. Oslo: Norwegian Medical Association; 2010. [Statistics on physicians in the Norwegian Medical Association per 1.1.2010] Available at: http://www.legeforeningen.no. [Google Scholar]
- 2.Hutt R, Parsons D, Pearson R. The timing of and reasons for doctors’ career decisions. Health Trends. 1981;13:17–20. [PubMed] [Google Scholar]
- 3.Roussel F, Gehanno JF, Ladner J, Benichou J. Do teaching faculty resources affect the choice of medical career? Med Teach. 2006;28:734–41. doi: 10.1080/01421590601047664. [DOI] [PubMed] [Google Scholar]
- 4.Baerheim A. Doing research on medical education. Scand J Prim Health Care. 2006;24:65–6. doi: 10.1080/02813430600699971. [DOI] [PubMed] [Google Scholar]
- 5.Aasland OG, Røvik JO, Wiers-Jenssen J. [Motives for choice of specialty during and after medical school] Tidsskr Nor Legeforen. 2008;128:1833–7. [PubMed] [Google Scholar]
- 6.Gjerberg E, Aasland O. Oslo: Research Institute of the Norwegian Medical Association; 1999. [Do doctors use too much time for post-graduate education (specialisation)?] [Google Scholar]
- 7.Thornton J, Esposto F. How important are economic factors in choice of medical specialty? Health Econ. 2003;12:67–73. doi: 10.1002/hec.682. [DOI] [PubMed] [Google Scholar]
- 8.McKay NL. The economic determinants of specialty choice by medical residents. J Health Econ. 1990;9:335–57. doi: 10.1016/0167-6296(90)90050-d. [DOI] [PubMed] [Google Scholar]
- 9.Harris MG, Gavel PH, Young JR. Factors influencing the choice of specialty of Australian medical graduates. Med J Aust. 2005;183:295–300. doi: 10.5694/j.1326-5377.2005.tb07058.x. [DOI] [PubMed] [Google Scholar]
- 10.Wiers-Jenssen J, Aasland OG. [Changes in career plans of medical students during the first half of medical school] Tidsskr Nor Legeforen. 1999;119:2858–64. [PubMed] [Google Scholar]
- 11.Magnus JH, Tollan A. Rural doctor recruitment: Does medical education in rural districts recruit doctors to rural areas? Med Educ. 1993;27:250–3. doi: 10.1111/j.1365-2923.1993.tb00264.x. [DOI] [PubMed] [Google Scholar]
- 12.Bunker J, Shadbolt N. Choosing general practice as a career: The influences of education and training. Aust Fam Physician. 2009;38:341–4. [PubMed] [Google Scholar]
- 13.Wilkinson D, Laven G, Pratt N, Beilby J. Impact of undergraduate and postgraduate rural training, and medical school entry criteria on rural practice among Australian general practitioners: National study of 2414 doctors. Med Educ. 2003;37:809–14. doi: 10.1046/j.1365-2923.2003.01596.x. [DOI] [PubMed] [Google Scholar]
- 14.Griffith CH, 3rd, Georgesen JC, Wilson JF. Specialty choices of students who actually have choices: The influence of excellent clinical teachers. Acad Med. 2000;75:278–82. doi: 10.1097/00001888-200003000-00020. [DOI] [PubMed] [Google Scholar]
- 15.Thistlethwaite JE, Kidd MR, Hudson JN. General practice: A leading provider of medical student education in the 21st century? Med J Aust. 2007;187:124–8. doi: 10.5694/j.1326-5377.2007.tb01160.x. [DOI] [PubMed] [Google Scholar]
- 16.Bland CJ, Meurer LN, Maldonado G. Determinants of primary care specialty choice: A non-statistical meta-analysis of the literature. Acad Med. 1995;70:620–41. doi: 10.1097/00001888-199507000-00013. [DOI] [PubMed] [Google Scholar]
- 17.HOD. Oslo: Ministry of Health and Care Services; 2009. [Report no. 47 to the Storting: The Coordination Reform. Proper treatment – at the right place at the right time] [Google Scholar]
- 18.Eklund-Gronberg A, Stange P. News from the Nordic colleges of general practitioners: The future is approaching. Scand J Prim Health Care. 2006;24:193–5. doi: 10.1080/02813430601017009. [DOI] [PubMed] [Google Scholar]