Abstract
Introduction:
Approximately 60%–70% of cigarette smokers who try to quit relapse by 2 weeks postcessation. We tested the efficacy of a front-loaded (FL) counseling intervention whose goal was to increase the likelihood of successful early abstinence and subsequent long-term abstinence.
Methods:
We randomized 278 adult smokers to an FL or weekly behavioral smoking cessation counseling schedule. The total number of sessions across treatment was the same for both groups. However, those assigned to the FL schedule received 6 counseling sessions in the first 2 weeks postcessation, while those in the weekly condition received 2 sessions. Participants in both groups also received standard nicotine patch treatment.
Results:
At 1 year postcessation, FL participants were significantly less likely to have relapsed when continuous abstinence was used as the definition of abstinence/relapse (11.7% abstinent vs. 6.3%, hazard ratio [HR] = 0.69, p = .007); and there were nonsignificant trends for FL subjects to have better outcomes when abstinence was defined as never smoking for 7 or more consecutive days nor for 7 or more consecutive episodes (18.4% abstinent vs. 14.8%, HR = 0.83, p = .20) and as point prevalence abstinence (15.6% abstinent vs. 12.9%, p = .11). The relationship between FL counseling treatment and continuous abstinence was partially mediated by higher postcessation levels of social support perceived from counseling and greater use of cessation-related coping strategies.
Conclusions:
We conclude that FL counseling is a promising treatment model that should be evaluated further, perhaps using modifications of the FL schedule used in this study.
Introduction
Approximately 60%–70% of cigarette smokers who try to quit relapse within two weeks of their quit dates (Garvey et al., 2000; Hughes, Keely, & Naud, 2004; Jorenby et al., 1995). Those who can remain abstinent for two weeks or more, however, have a 50% likelihood of remaining abstinent at one year postcessation (Hurt et al., 1994). If relapse could be prevented in the first two weeks postcessation, long-term success rates should seemingly be much higher (Zhu et al., 1996). The aim of the present study was to test the efficacy of a front-loaded (FL) counseling intervention designed to increase the likelihood of abstinence in the first two weeks of a quit attempt and subsequent long-term abstinence. This study provided the first experimental test to our knowledge regarding the effects of FL counseling on the outcome of a quit-smoking attempt. Our central hypothesis was that individuals randomly assigned to an FL counseling schedule, characterized by a greater number of counseling sessions in the first two weeks postcessation, would have a significantly greater likelihood of abstinence at one year postcessation compared with those assigned to a standard weekly counseling schedule.
We also examined mechanisms (mediators) through which FL counseling might enhance cessation rates. Our hypotheses were that participants receiving FL counseling would report higher levels of social support from counseling and greater use of cessation-related coping behavior in the first two weeks postcessation than would those receiving weekly counseling. We further believed that FL counseling would produce higher confidence, motivation, and effort levels in the first two weeks postquit compared with the weekly counseling condition.
In addition, we conducted moderation analyses to determine for whom FL counseling might be especially efficacious. The variables examined for interactions with treatment condition were gender (women expected to do better in the FL counseling condition), education level (those with lower education levels expected to have better outcomes with FL counseling), dependence level (more dependent smokers expected to do better if assigned to FL treatment), and depressive symptom level (those with more depressive symptomatology expected to have better outcomes with FL counseling). We expected the above subgroups to have better outcomes because of the greater volume of early social support and skills training provided by the FL counseling treatment.
Methods
Sample
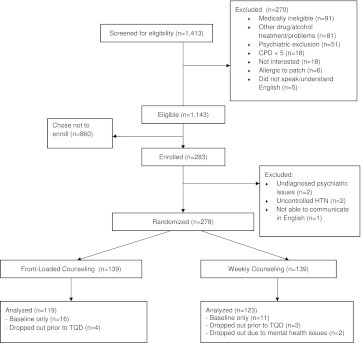
We recruited smokers using advertisements placed in Boston area newspapers. All participants smoked a minimum of 5 cigarettes/day (CPD), were motivated to quit, and reported good health. Medical exclusion criteria included uncontrolled hypertension, cardiovascular disease or symptoms, insulin-dependent diabetes, and pregnancy or lactation. Psychiatric exclusion criteria included history of schizophrenia, current severe depression (past three months), unstable bipolar disorder, substance use disorder (past twelve months), and/or hospitalization for psychiatric reasons in the past twelve months. We also excluded smokers taking antipsychotic medications for psychosis-related conditions. Institutional Review Board approval was obtained from the Harvard Medical School Committee on Human Studies and the Institutional Review Boards of Boston University and the University of Massachusetts Medical School. All participants gave written consent. Of the 283 people enrolled, 278 were randomized to FL or weekly counseling treatments (see Figure 1). Participants needed to attend both prequit-day counseling sessions in order to be included in statistical analyses (see Table 1). Thirty-six subjects were excluded from statistical analyses, the majority because they chose to drop out of the study before counseling treatment began. Hence, results are reported for 242 research participants.
Figure 1.
Participation flow diagram. CPD indicates cigarettes per day, HTN indicates hypertension, and TQD is target quit day.
Table 1.
Schedule of Counseling Sessions
| Days postcessation | −4 | −2 | 0 | 2 | 4 | 7 | 10 | 14 | 21 | 28 | 35 | 42 | 49 | 56 | 84 | 180 | 270 | 365 |
| Front-loaded counseling condition | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Weekly counseling condition | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
Note. X = counseling session. Day 0 is quit day. Day 84 (12 weeks) is end of nicotine patch treatment.
Procedure
Participants were randomly assigned after their baseline visits to receive either an FL or weekly counseling schedule (see Table 1). Participants in both conditions received 2 prequit and 12 postquit individual counseling sessions. The counseling was in-person and individual. Those assigned to FL treatment received 6 of the 12 postquit counseling sessions in the first two weeks following their quit days, while participants assigned to the weekly counseling schedule received 2 of the 12 sessions in the first two postquit weeks. Counselors were trained to deliver a manual-based cognitive–behavioral smoking cessation therapy developed for the study (manual available upon request). In developing the manualized protocol, we followed the principles and techniques detailed in the Public Health Service Clinical Practice Guideline (Fiore et al., 2008). Major elements of the counseling protocol involved the development of an individualized coping plan for preventing smoking in high-risk situations, re-working of the coping plan as needed, and provision of counseling support. The counseling protocol also included discussions of issues, such as guarding against rationalizations, the abstinence violation effect, proactive versus reactive coping, and developing a nonsmoker identity.
All counselors had earned a master's or bachelor’s degree in Psychology. Counselors provided counseling to participants in both conditions. Counselors received three full days of training from the second author (Dr. Kalman) prior to being assigned any cases. Training included demonstrations and extensive role-plays of all sessions. Training also consisted of discussions of a variety of counseling scenarios, including how to manage participant ambivalence about quitting, participants who have difficulty staying on topic in the session, and lapses and relapses. Following training, the second author met with counselors for 2–3 hr in supervision at least biweekly for several months and then on a monthly basis. He was also available on an as needed basis for supervision throughout the trial. All sessions were audio taped, and Dr. Kalman reviewed at least two randomly selected taped sessions per month for each counselor to monitor for fidelity and competence and to prevent drift. Excerpts from these tapes were also played and discussed in supervision.
Length of time for counseling sessions varied. The two prequit counseling sessions were approximately 45 min each. Postquit counseling sessions averaged 20–30 min per session. These sessions consisted of review of experiences since the previous session, review of previously discussed material, introduction of new material, and revision of coping plans as needed. Variations in postquit session counseling length were dependent on the participant level of difficulties encountered and degree of coping plan modification needed.
Participants were assigned a counselor based on schedule availability, and participants continued to work primarily with that counselor throughout their participation (in the event of sickness, vacations, etc., one of the other counselors would fill in to maintain schedule adherence, though this was a very rare occurrence). No blinding was done. All personnel involved in the study were told that we were conducting a research study and that we did not know a priori whether those assigned to FL counseling or those assigned to the weekly counseling schedule would have the better outcomes. Randomization was done using a 12-block block-randomization model so as to ensure with every block of 12 subjects that 6 would be assigned to FL and 6 to weekly counseling; randomization occurred at the end of the baseline visit following the consenting process and administration of baseline measures. The approximate sample size needed was estimated to be 132 participants per treatment group by assuming a 33% quit rate at the end of 1 year for those assigned to FL counseling and an 18% quit rate for those assigned to weekly counseling using the p = .05 level (two-sided) and power = 0.80.
Participants in both treatment conditions received transdermal nicotine patches. The patches used were Nicoderm CQ Patches (GlaxoSmithKline) in 21-, 14-, and 7-mg doses. Participants who reported smoking 10 or more CPD at baseline were given the 21-mg patch for 8 weeks and then were reduced to 14 mg for 2 weeks and 7 mg for 2 weeks. Participants who reported smoking fewer than 10 CPD were provided the 14-mg patch for 8 weeks and then reduced to 7 mg for 4 weeks. Nicotine patches were distributed at the second prequit counseling session, and participants were instructed to start wearing the patches the morning of their target quit days. At each subsequent office visit, subjects were given enough patches to last until their next visit.
Data Collection and Analysis
At their baseline visits, participants filled out questionnaires concerning demographics, smoking history, levels of confidence and motivation for quitting, and level of effort that they would devote to the quit attempt. Confidence, motivation, and effort were assessed using single-item 0–10 rating scales like those used in our previous studies (e.g., Garvey et al., 2000). The Fagerstrom Test of Nicotine Dependence (FTND) was used to assess level of nicotine dependence (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991). Severity of depressive symptoms was measured using the Center for Epidemiological Studies Depression Scale (CES-D; Anda, Williamson, & Escobedo, 1990). Carbon monoxide (CO) level was obtained as an index of cigarette exposure using a Vitalograph Breath CO Instrument (Lenexa, KS). Ambient CO levels were subtracted from expired CO values for each participant.
In the postcessation period, we reassessed variables measured in the precessation period that were likely to change, for example, motivation, confidence, and effort levels, depressive symptom level. We also assessed support level perceived from counseling and ratings of the degree of coping skills utilization using single-item 0–10 rating scales. Postcessation measures were obtained at “common” office visits, that is, those attended both by FL and weekly participants, such as visits at postcessation Days 7, 14, 28, etc (see Table 1). CO levels were also assessed in the postquit period to provide biochemical verification of self-reported abstinence. Verified abstinence was defined as a CO level of <8 ppm.
Cox regression (proportional hazards) and generalized estimating equations (GEE) were the principal procedures used to assess the statistical significances of treatment and covariate effects on outcomes. Analysis of variance (ANOVA) and chi-square analyses were used to assess possible differences between the two counseling conditions on demographics and smoking history variables. ANOVA was used for assessing treatment group differences in number of counseling sessions attended in the first two weeks postcessation and for assessing treatment group differences in perceived counseling support, use of coping strategies, as well as differences in motivation, confidence, and effort levels in the postcessation period. Data analyses were conducted using SAS software (Version 9.2).
We used three definitions of abstinence/relapse suggested by Hughes et al. (2003) in analyzing our outcome data. Continuous abstinence was defined as not even a puff smoked at any point during the period of follow-up. The definition of abstinence developed originally by the National Heart, Lung, and Blood Institute (NHLBI) was also used; NHLBI abstinence was defined as never smoking for seven or more consecutive days nor for seven or more consecutive episodes (e.g., weekend smoking; Ossip-Klein et al., 1986). Day of relapse was defined as the day postcessation that began the regular pattern of smoking, a definition we have used in our previous studies (e.g., Garvey et al., 2000). Hence, for example, if the person's first day of seven or more consecutive days of smoking began on Day 3, then he/she was credited with two days abstinence and as relapsed by Day 3. For continuous abstinence and NHLBI abstinence, the outcome (dependent variable) was survival time (i.e., time to relapse). Point prevalence abstinence was defined as no smoking for a week or more before an office visit at which chemical verification of abstinence was assessed.
FL counseling treatment was coded as 1, and weekly counseling as 0 in all analyses. Participants lost to follow up sometime after their quit days (N = 17) were coded as censored. For example, if a person did not participate further than three months beyond his/her quit day and was confirmed abstinent at the Month 3 visit, then that person would be considered as abstinent at three months and as censored thereafter. For mediation analyses, we followed the guidelines suggested by Baron and Kenny (1986) and MacKinnon and Luecken (2011). Essentially, evidence for mediation is provided if the following conditions are shown to be valid: (a) the independent variable is significantly related to the outcome (dependent) variable, (b) the independent variable is significantly related to the mediator, (c) the mediator is significantly related to the outcome variable, and (d) the effect of the independent variable on the outcome variable is less with the mediator in the model. Evidence for complete mediation is obtained if the independent variable is no longer statistically significant once the mediator is in the model, while partial mediation is evidenced if the effect of the independent variable is reduced with the mediator in the model, even if the independent variable remains statistically significant.
Results
The mean age of participants in our study was 46.9 years (SD = 11.5, range = 19–78), 52.9% were female, 73.6% were White, 39.3% were married, 57% had less than a 4-year college degree, and 73.1% were employed. Participants smoked 17.9 CPD on average (SD = 7.9, range = 5–45), the mean baseline CO level was 21.0 ppm (SD = 11.0, range = 1–64), and the mean FTND score was 4.9 (SD = 2.3, range = 0–10). The mean FTND value indicates that, on average, smokers enrolled in the study were moderately dependent, though the whole range of dependency was represented in our sample. Participants in the two counseling treatment groups did not differ significantly in age, gender, race, marital status, education, CPD, FTND, or CO (all p values > .05, range = 0.12–0.89). There was a marginally significant relationship between treatment condition and percent employed (p = .04; FL, 79.0% employed; weekly, 67.2%). However, percent employed was unrelated to outcomes (e.g., p = .31 for the continuous abstinence definition at one year postcessation). Also, controlling for percent employed had little effect on the relationship between treatment condition and outcomes at 1 year (e.g., p = .007 for the continuous abstinence definition with percent employed not controlled vs. p = .009 with percent employed controlled), and the interaction of treatment group and percent employed was not significant (p = .37). Hence, we did not control for percent employed in subsequent analyses.
The mean number of counseling sessions attended in the first two weeks postcessation differed significantly, as expected, by counseling condition. FL participants attended significantly more sessions in the first two weeks postcessation compared with those assigned to weekly counseling (FL: M = 4.9 sessions attended of a scheduled six sessions, SD = 1.8, median = 6; weekly: M = 1.6 sessions of a scheduled two sessions, SD = 0.8, median = 2 [p < .0001 from ANOVA]). Thus, it was clear that FL participants as a group displayed excellent compliance to the FL counseling schedule.
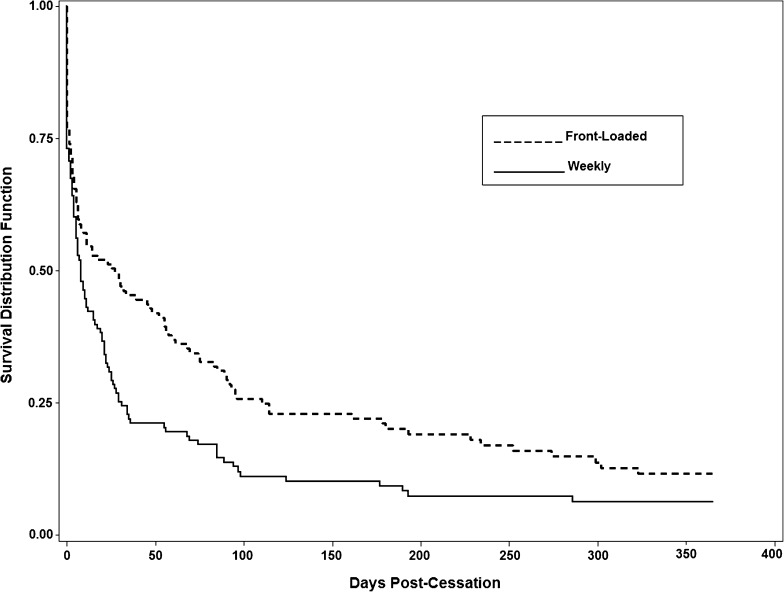
We found support for our principal hypothesis that those assigned to the FL counseling schedule would have better outcomes at one year postcessation, though the statistical significances of associations differed depending on the definition used to classify participants as abstinent or relapsed (see Figures 2–4). From Figure 2, using continuous abstinence as the definition of abstinence/relapse, it can be seen that those in the FL condition had a significantly lower likelihood of failure (relapse) over the course of the 1-year follow-up period than did those assigned to weekly counseling (11.7% abstinent vs. 6.3%, hazard ratio [HR] = 0.69 [0.53–0.90], p = .007). Surprisingly, no striking differences in outcomes between the FL and weekly conditions were observed in the first two weeks postcessation. A test of the interaction between counseling condition and time period (Baseline—2 weeks, 2+ weeks—12 weeks, 12+ weeks—52 weeks) was not significant (p = .15). Thus, for the continuous abstinence definition of abstinence/relapse, we can conclude that there was a consistent statistically significant effect over the entire course of the 1-year period of follow-up for those in the FL condition to have the lower likelihood of relapse.
Figure 2.
Survival distribution function by treatment condition where survival is defined based on the continuous abstinence definition of abstinence/relapse (p = .007 from Cox regression).
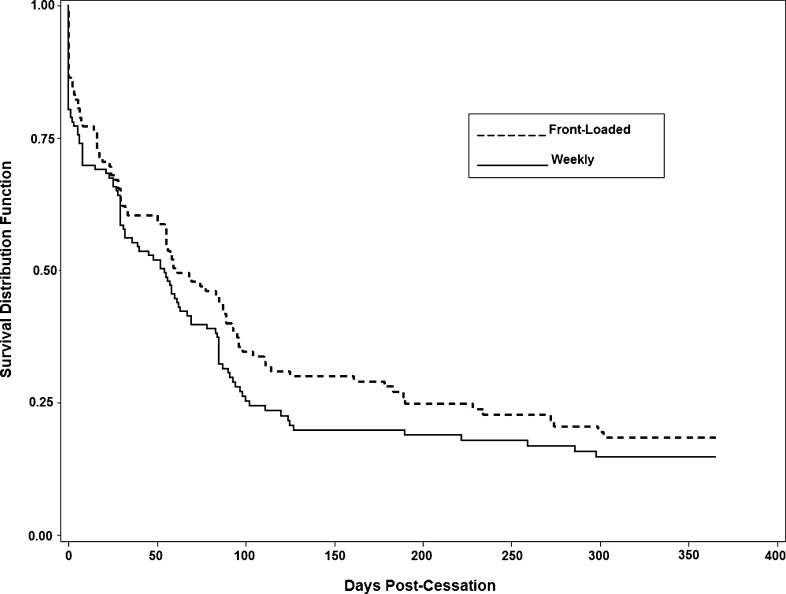
Figure 3.
Survival distribution function by treatment condition where survival is defined based on the National Heart, Lung, and Blood Institute (NHLBI) definition of abstinence/relapse. NHLBI abstinence is defined as never smoking for more than seven consecutive days nor for more than seven consecutive episodes (Ossip-Klein et al., 1986; p = .20 from Cox regression).
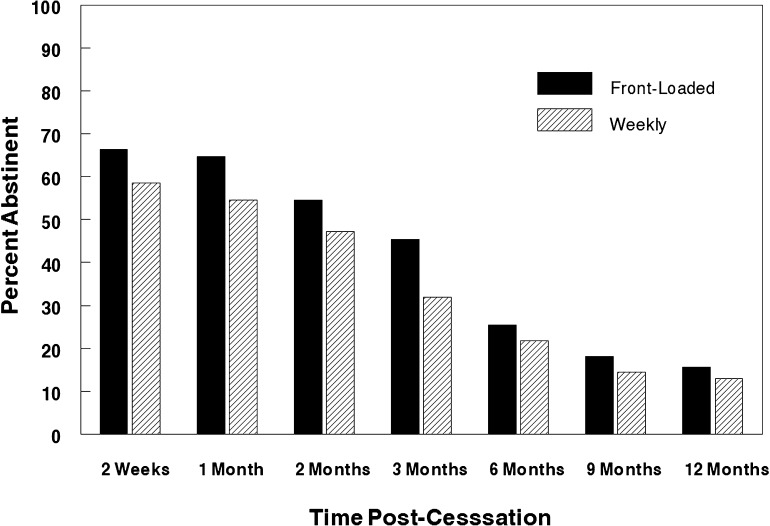
Figure 4.
Percent abstinent by treatment group across 1 year of follow-up using point prevalence abstinence as the dependent variable (p = .11 from generalized estimating equations analysis).
Using the NHLBI definition of abstinence, those in the FL condition again had a lower likelihood of relapse, though effects were not significant over the 1-year period of follow-up (18.4% abstinent vs. 14.8%, HR = 0.83 [0.63–1.10], p = .20; Figure 3). As with outcomes involving the continuous abstinence definition, results were not dramatic in the first two weeks postcessation. For point prevalence abstinence (Figure 4), there were trends for FL participants to have better outcomes at every postcessation checkpoint. However, a GEE analysis assessing the significance of treatment on point prevalence abstinence over the 1-year follow-up period was not significant (p = .11).
We also assessed treatment effects using prolonged abstinence as the definition of outcome. Prolonged abstinence was defined as never smoking for seven or more consecutive days, nor seven or more consecutive episodes, after a grace period of two weeks duration during which some smoking was allowed (Hughes et al., 2003). Results were essentially the same as, and not substantively different from, those reported above for the NHLBI definition of abstinence. Hence, we did not present results using the prolonged abstinence definition.
Mediator Effects
Since counseling treatment group was significantly related to abstinence/relapse using the continuous abstinence definition, we examined possible mediators of this relationship. As stated in our Introduction section, the variables hypothesized as mediators were social support, degree of utilization of coping strategies, and levels of motivation, confidence, and effort devoted to the quit attempt. No other variables were considered for the mediation analyses. Mediator information was collected at Week 2 postcessation. We thus examined the effects of the hypothesized mediators from Weeks 2 to 12 (3 months) postcessation as our primary analyses. We chose Weeks 2–12 because we believed that the effects of the mediators would be most apparent in the early weeks after the data on mediators were obtained. For completeness, we also examined mediator effects from Weeks 2 to 52 (1 year). Because mediation analyses assume that the mediator is assessed before the outcome is attained and that therefore the outcome cannot be a cause of the mediator (Baron & Kenny, 1986; MacKinnon & Luecken, 2011), only subjects who were abstinent at Week 2 were included in the mediation analyses. The sample size for the mediation analyses was therefore reduced to N = 111.
At two weeks postcessation, those assigned to FL counseling, compared with weekly participants, perceived significantly more social support from counseling (M = 8.5, SD = 2.0 vs. M = 7.4, SD = 2.0, p = .006) and reported significantly greater usage of coping strategies to resist smoking (M = 8.1, SD = 2.4 vs. M = 6.8, SD = 2.4, p = .004). There were no significant differences between the counseling treatment groups, however, in reported levels of motivation, confidence, or effort at two weeks postquit (p values = .48, .09, and .56, respectively). Hence, we did not consider the variables motivation, confidence, and effort further as mediators given that they did not meet a criterion required of mediators, that is, that they be significantly related to the independent variable.
We next examined the effects of perceived social support and use of coping strategies at Week 2 as mediators of the relationship between counseling treatment and continuous abstinence during the period from 2 to 12 weeks. Using procedures suggested by Baron and Kenny (1986) and MacKinnon and Luecken (2011), we looked first at the effects of perceived social support as a mediator using three proportional hazards models (Cox regression). In the first model, counseling treatment condition was the predictor variable. The second model had perceived counseling support as the predictor variable, and the third model had both counseling treatment condition and perceived counseling support as independent variables.
Both counseling treatment (p = .008, HR = 0.49 [0.28–0.83]) and perceived counseling support (p = .019, HR = 0.86 [0.79–0.98]) were significant in univariate models. When both variables were entered as predictors, the p value for treatment declined (p = .026, HR = 0.54 [0.31–0.93]), as did the effect of perceived counseling support (p = .069, HR = 0.89 [0.78–1.01]). The percent decline in the regression weight for counseling treatment with social support in the model was 14.0%. Hence, following the suggestions of Baron and Kenny (1986) and MacKinnon and Luecken (2011), we can conclude that there was partial mediation of the treatment effect by the mediator, perceived social support, though the effect was relatively small.
Identical models were employed for assessing degree of utilization of coping strategies as a mediator. Similar to results involving perceived social support from counseling, counseling treatment group declined in significance when use of coping strategies was also entered in a Cox regression model. Both counseling treatment (p = .008, HR = 0.49 [0.28–0.83]) and use of coping strategies (p = .018, HR = 0.89 [0.81–0.98]) were significant in univariate models. When both variables were entered as predictors, the effect of counseling treatment declined (p = .033, HR = 0.55 [0.31–0.95]), as did the effect of utilization of coping strategies (p = .087, HR = 0.92 [0.83–1.01]). The percent decline in the regression weight for treatment group when use of coping strategies entered the model was 16.2%. Thus, as for perceived social support, we can conclude that there was partial mediation of the counseling treatment effect by the mediator utilization of coping strategies and that the mediation effect was relatively small.
We also performed mediation analyses entering both social support and utilization of coping strategies in the same model. These two variables were moderately correlated, r = .59, p < .0001. With both variables in the model, neither social support nor utilization of coping strategies were significant by themselves (p = .213 and p = .193, respectively) as predictors of outcome. However, when they were both in the model along with treatment group, they reduced the treatment effect somewhat more than when they entered singly (treatment effect p = .041, HR = 0.56 [0.32–0.98], percent decline in the treatment effect regression coefficient = 19.6%).
We next performed identical sets of mediation analyses as those described above, this time considering the period from 2 to 52 weeks. Neither perceived social support nor use of coping strategies were significantly related to outcome at 1 year (p = .101 and p = .128, respectively). Since the criterion that a mediator be significantly related to the outcome was not satisfied, we did not pursue the analyses further (Baron & Kenny, 1986; MacKinnon & Luecken, 2011). We can conclude that the partial mediation effects of perceived social support and utilization of coping strategies were most evident in the period from 2 to 12 weeks postcessation and that these effects were weaker when the longer period from Weeks 2 to 52 was considered.
Moderator Effects
There were no statistically significant interactions between treatment condition and any of the potential moderator variables examined. There were nonsignificant trends, but only when using the continuous abstinence definition of abstinence/relapse, for women in the FL condition to have better outcomes than men in the FL condition at two weeks postcessation (interaction effect, p = .10; within-FL counseling gender p value = .10), at twelve weeks postcessation (interaction effect, p = .07; within-FL counseling gender p value = .04), and at 1 year of follow-up (interaction effect, p = .19; within-FL counseling gender p value = .13). When the NHLBI definition of abstinence/relapse was used, however, there were no trends for women in the FL condition to do better than men receiving the FL treatment at any follow-up timepoint (all interaction p values > .52). Likewise, using point prevalence abstinence/relapse, there were no trends for women in the FL condition to do better than men in this condition (all interaction p values > .63).
For education level (coded as less than college graduate vs. college graduate), interaction effects with treatment condition were nonsignificant (all p values > .64). There were also no significant interaction effects of dependence level, indexed by the FTND, with counseling treatment condition (all p values > .72). Likewise, those with more depressive symptomatology, as indexed by the CES-D, did not do better with FL treatment (all interaction p values > .82).
Discussion
We found consistent evidence for the efficacy of FL counseling, though treatment effects were statistically significant only when using the continuous abstinence definition of abstinence/relapse. We had expected a more striking difference in quit rates between the FL and weekly counseling treatments in the first two weeks postcessation given that FL participants received 3 times as many sessions as weekly subjects in this period (six sessions vs. two). It is possible that the provision of two prequit counseling sessions may have prepared all participants reasonably well for the early portion of the quit attempt, thereby muting or dampening, the expected differences in abstinence rates between the FL and weekly counseling conditions in the first two weeks postcessation. On the other hand, the tripling of counseling sessions during the first two weeks for those in the FL condition, with assumed accelerated learning and implementation both of initial coping plans and refinements of these coping plans, as well as the greater volume of social support received from counseling may have better prepared FL participants to maintain abstinence after this early 2-week period. FL participants did in fact report significantly higher levels of social support from counseling and greater use of coping plans at two weeks postcessation; and we found evidence that perceived social support and greater use of coping strategies were partial mediators of the significant relationship between FL counseling treatment and continuous abstinence.
We should reiterate that treatment outcomes and interactions of other variables with treatment differed somewhat depending on the definition of abstinence/relapse used. It seems very important, therefore, that treatment studies use multiple definitions of abstinence/relapse in order to get a more balanced perspective regarding the interpretation of treatment outcomes. For example, counseling treatment group was significantly related to continuous abstinence outcomes, but while trends favoring FL counseling were in the same direction for NHLBI abstinence and point prevalence abstinence, these trends were nonsignificant. Had only NHLBI abstinence, for example, been used as the outcome, the conclusion might have been that FL counseling treatment has little promise as a potential treatment. On the other hand, had data based on continuous abstinence been the only outcome reported, conclusions regarding the promise of FL counseling would likely have been overly optimistic.
As another example, when we used the continuous abstinence definition of abstinence/relapse, there were some, though not statistically significant, treatment-by-gender interaction trends indicating that women assigned to FL counseling treatment did somewhat better than men assigned to FL treatment. However, no trends at all were observed regarding gender interactions with treatment when NHLBI abstinence or when point prevalence abstinence were the outcome measures used. Had only continuous abstinence been used as the outcome variable, potentially spurious, nonrobust trends for gender to moderate the effects of treatment might unknowingly have been reported.
We conclude that FL counseling is a promising treatment approach whose efficacy should be examined further. We used essentially an “every other day” counseling schedule in the first two weeks postcessation, and this schedule yielded significant effects when continuous abstinence was used as the definition of abstinence/relapse. Other FL schedules should also be investigated, for example, seeing a person each business day for the first week or first two weeks, or alternating daily in-office and phone sessions in the first two to three weeks. It is possible that other, perhaps more intensive, FL schedules could yield even better outcomes than did our schedule.
Funding
This study was supported by grant 5 R01 DA016739 from the National Institute on Drug Abuse of the National Institutes of Health. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Declaration of Interests
No competing financial interests exist.
Acknowledgments
The authors wish to thank Christine D. Armour, B.A., Sarah A. Kupper, B.A., and Sybil Copp, L.S.W. for their helpful suggestions with regard to improving the manuscript. We also wish to thank Emily Wood, M.A. for her assistance in collection of data analyzed in the study.
References
- Anda RF, Williamson DF, Escobedo LG. Depression and the dynamics of smoking: A national perspective. Journal of the American Medical Association. 1990;264:1541–1545. doi:10.1001/jama.264.12.1541. [PubMed] [Google Scholar]
- Baron RH, Kenny DA. The moderation-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. doi:10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008. [Google Scholar]
- Garvey AJ, Kinnunen T, Nordstrom BL, Utman CH, Doherty K, Rosner B. Effects of nicotine gum dose by level of nicotine dependence. Nicotine & Tobacco Research. 2000;2:53–63. doi: 10.1080/14622200050011303. doi:10.1080/14622200050011303. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. doi:10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99:29–38. doi: 10.1111/j.1360-0443.2004.00540.x. doi:10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: Issues and recommendations. Nicotine & Tobacco Research. 2003;5:13–25. doi:10.1080/146222003/000070552. [PubMed] [Google Scholar]
- Hurt RD, Dale LC, Fredrickson PA, Caldwell CC, Lee GA, Offord KP, et al. Nicotine patch therapy for smoking cessation combined with physician advice and nurse follow-up: One-year outcome and percentage of nicotine replacement. Journal of the American Medical Association. 1994;271:596–600. doi:10.1001/jama.271.8.595. [PubMed] [Google Scholar]
- Jorenby DE, Smith SS, Fiore MC, Hurt RD, Offord KP, Croghan IT, et al. Varying nicotine patch dose and type of smoking cessation counseling. Journal of the American Medical Association. 1995;274:1347–1352. doi:10.1001/jama.274.17.1347. [PubMed] [Google Scholar]
- MacKinnon DP, Luecken LJ. Statistical analysis for identifying mediating variables in public health dentistry interventions. Journal of Public Health Dentistry. 2011;71:S37–S46. doi: 10.1111/j.1752-7325.2011.00252.x. doi:10.1111/j.1752-7325.2011.00252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ossip-Klein DJ, Bigelow G, Parker SR, Curry S, Hall S, Kirkland S. Classification and assessment of smoking behavior. Health Psychology. 1986;9(Suppl.):3–11. doi:10.1037/0278-6133.5.Suppl.3. [PubMed] [Google Scholar]
- Zhu SH, Stretch V, Balabanis M, Rosbrook B, Sadler G, Pierce JP. Telephone counseling for smoking cessation: Effects of single-session and multiple-session interventions. Journal of Consulting and Clinical Psychology. 1996;64:202–211. doi: 10.1037//0022-006x.64.1.202. doi:10.1037//0022-006X.64.1.202. [DOI] [PubMed] [Google Scholar]