Abstract
AIM: To study the therapeutic efficacy of a new transnasal ileus tube advanced endoscopically for adhesive small bowel obstruction.
METHODS: A total of 186 patients with adhesive small bowel obstruction treated from September 2007 to February 2011 were enrolled into this prospective randomized controlled study. The endoscopically advanced new ileus tube was used for gastrointestinal decompression in 96 patients and ordinary nasogastric tube (NGT) was used in 90 patients. The therapeutic efficacy was compared between the two groups.
RESULTS: Compared with the NGT group, the ileus tube group experienced significantly shorter time for relief of clinical symptoms and improvement in the findings of abdominal radiograph (4.1 ± 2.3 d vs 8.5 ± 5.0 d) and laboratory tests (P < 0.01). The overall effectiveness rate was up to 89.6% in the ileus tube group and 46.7% in the NGT group (P < 0.01). And 10.4% of the patients in the ileus tube group and 53.3% of the NGT group underwent surgery. For recurrent adhesive bowel obstruction, ileus tube was also significantly more effective than NGT (95.8% vs 31.6%). In the ileus tube group, the drainage output on the first day and the length of hospital stay were significantly different depending on the treatment success or failure (P < 0.05). The abdominal radiographic improvement was correlated with whether or not the patient underwent surgery.
CONCLUSION: Ileus tube can be used for adhesive small bowel obstruction. Endoscopic placement of the ileus tube is convenient and worthy to be promoted despite the potential risks.
Keywords: Adhesive, Small bowel obstruction, Ileus tube, Nasogastric intubation, Gastrointestinal decompression
INTRODUCTION
Gastrointestinal decompression is the most effective approach to treat the patients with acute bowel obstruction without any indications of strangulation[1,2]. The traditional nasogastric tube (NGT) is not long enough for suctioning the distal intestine and its decompression efficacy is relatively low. Since the 1930s, the concept of nasointestinal decompression and use of nasointestinal tubes have been developed and applied in clinical practice. Some studies have verified the efficacy of long nasointestinal tubes in treating adhesive small bowel obstructions (SBO)[3-7]. However, a prospective randomized trial demonstrated no significant differences with regard to the decompression achieved, the success of non-surgical treatment, or the morbidity rate after surgical intervention as compared with the use of short NGT[8]. In 2003, a new hydrophilic silicon triple-lumen ileus tube was first introduced and used in Japan for nasointestinal decompression. It could be advanced through the gastroscope in shorter time with a higher tolerance[9]. Up till now, there has been no randomized controlled study about the efficacy of the ileus tube. This randomized controlled trial attempted to investigate and compare the decompression efficacy between the new ileus tube and the traditional NGT for patients with adhesive SBO.
MATERIALS AND METHODS
Patients
Approved by the hospital’s ethics committee, a total of 186 patients with acute adhesive SBO who were admitted to the Gastroenterology and Colorectal Surgery wards of the First Affiliated Hospital, College of Medicine, Zhejiang University and its Ningbo Branch Hospital from September 2007 to February 2011 were enrolled into this study. The entry criteria were as follows: (1) clinical symptoms and physical signs arising from acute bowel obstruction; (2) a diagnosis of adhesive SBO based on abdominal plain films and computed tomography (CT) scans confirmed by at least two attending radiologists; and (3) admission to the hospital within 12 h after bowel obstruction onset. All patients who presented with symptoms of fever, vomiting or hematemesis, hematochezia, severe or sudden abdominal pain, and the signs of tachycardia, leukocytosis, abdominal tenderness, peritoneal irritation, asymmetric abdominal distension or isolated swelling bowel loops and even shock, should be suspected of strangulation obstruction, which needed immediate operation. Besides, patients who had contraindications for endoscopy, or with postoperative adynamic obstruction or malignancy, or who had been treated in other hospitals before admission were excluded. Patients were randomized into two groups by the sealed envelope method: the ileus tube group and the NGT group; an opaque box containing an equal number of envelopes that indicated either ileus tube or NGT, was used for randomization. Written informed consents were obtained from all the patients before enrollment. This trial conformed to the provisions of the World Medical Association Declaration of Helsinki. Ileus tube was used in 96 patients (56 men and 40 women) for gastrointestinal decompression; their ages ranged from 21 to 86 years (mean, 58 years). Among the 96 patients, 25 had a history of prior adhesion, and 89 patients received prior abdominal surgery. Ninety patients (56 men and 34 women) treated with NGT served as the control group; their ages ranged from 19 to 86 years (mean, 54 years). Among the 90 patients, 38 had a history of prior adhesion, and 86 had a history of abdominal surgery.
Patient preparation
On admission, all patients underwent abdominal plain film radiography and CT scanning to confirm acute bowel obstruction. Patients requiring emergency surgery were excluded. Performed by the same technicians, the ileus tube was advanced endoscopically and the traditional NGT was inserted for gastrointestinal decompression at a similar negative pressure level for constant suction. For all patients, routine laboratory blood tests were performed, and C-reactive protein (CRP) level and erythrocyte sedimentation rate (ESR) were determined.
Instrument and procedures
The CLINY Ileus Tube suite (Create Medic, Tokyo, Japan) and the ordinary NGT (Terumo Medic, Hangzhou, China) were used. The ileus tube is 300 cm in length and 16 Fr with three channels (suction channel, injection channel and balloon channel) and two balloons (anterior balloon and posterior balloon). Beside the tip hole, there are side holes in the distal end of the tube. Compared with other long tubes, this tube has weighted tip which consists of several metal balls for easier advancing. The posterior balloon is intended for contrast radiography. Water and contrast medium can be injected into the tube for lavage and imaging. Under some instances, the tube can directly remove the obstruction by its weighted tip. The guidewire is 350 cm long and 1.24 mm in diameter. The NGT is 110 cm in length and 16 Fr. All patients received gastrointestinal decompression within 12 h after admission. In the ileus tube group, the tube was pre-set through the nasal cavity to the stomach. The guidewire was inserted into the main channel to the tips. After endoscopic suction of stomach contents, the wire was moved into the descending duodenum by forceps, and the tube was inserted into the duodenum while the wire was kept fixed (Figure 1). Then the anterior balloon was inflated with 20 mL distilled water. The gastroscope was withdrawn after the long tube was fixed to the cheek. The tube was propelled by bowel peristalsis and its weighted tip, and the outside terminal of the tube was connected to a spontaneous negative pressure bag. Intermittent lavage (twice a day) through the long tube was performed from the second day after intubation, and the length of the advanced tube was carefully measured. In the control group, the NGT was inserted from nose to stomach to a depth of 45-55 cm. All patients were supported with total parenteral nutrition and received nothing by mouth. Emergency surgery was performed when the patient was suspected to have developed bowel ischemia. The potential risks for endoscopic placement of the ileus tube were throat injury, upper gastrointestinal perforation and bleeding, aspiration pneumonia and cardiovascular events.
Figure 1.
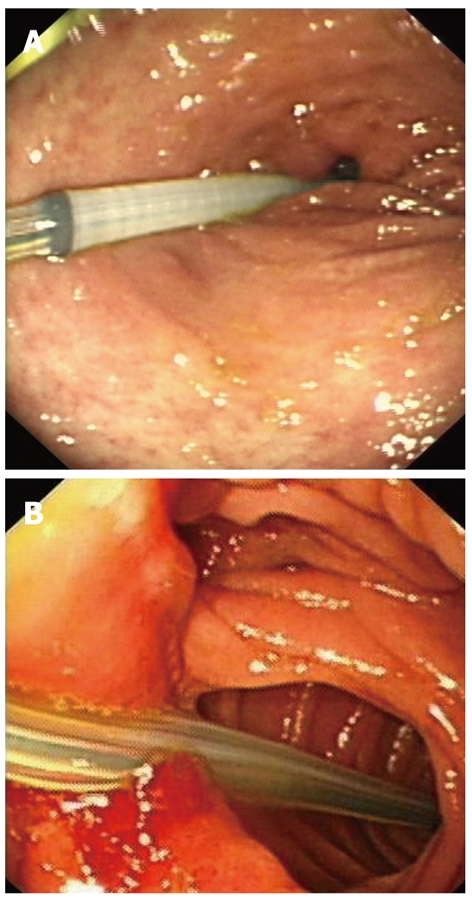
Endoscopic placement of ileus tube. A: An ileus tube is passed through the pylorus under gastroscopy in a patient with postoperative adhesive small bowel obstruction; B: An ileus tube led by a guidewire is endoscopically advanced into the efferent loop in a patient who had distal partial gastrectomy.
Outcome measurement
We compared the clinical and laboratory variables before intubation, including age, sex, type of prior surgery, symptoms and physical signs, and laboratory indexes on admission between the two groups. Physical examination (every 2 h), laboratory test (once a day) and abdominal imaging (days 2-7) were conducted frequently after intubation. The clinical and laboratory findings included: the time for relief of abdominal symptoms; time for abdominal radiographic improvement and recovery of white blood cell (WBC) counts, CRP level and ESR; drainage volume on the first day; surgery rate, the overall efficacy and the different therapeutic responses to the two kinds of tubes. The therapeutic effectiveness in the ileus tube group was defined as clinical or radiological improvement, relief of abdominal symptoms, decreased drainage volume, disappearance of air-fluid levels or reduced gas and fluid in bowel loops. Oral feeding was then administered gradually and the tube was removed. If the patient presented no improvement 72 h after decompression, or even progressed into strangulation, surgery is recommended[4]. In the NGT group, if a fairly prompt response occurs within 48 h, especially within the first 8-12 h after nasogastric decompression and resuscitation, the obstruction will probably be resolved without surgery[10,11]. Surgery was recommended if patients showed no response 72 h after non-surgical treatment, which was defined as treatment failure[12], otherwise, conservative treatment was continued.
Sample size calculation
Determination of the sample size was based on the previous studies[4,9]. The effectiveness rate was 51% in the short tube decompression while 85.7% in the long nasointestinal tube. If the effectiveness rate of the NGT and the ileus tube was defined as 50% and 80%, respectively, a study with 48 patients per group would have a 90% power to detect a difference at a two-sided significance level of 0.05. We extended our sample size to account for potential dropouts
Statistical analysis
Statistical analysis was performed using SPSS software version 16.0 (SPSS Inc, Chicago). Results were expressed as mean ± SD. The χ2 test was used to identify differences in the effectiveness rate between the two groups. The Student’s t test was used for unpaired data to determine differences in means between the two groups. Odds ratios (ORs) were determined by logistic regression analysis. Two-tailed P value of < 0.05 was considered statistically significant.
Study limitations
This study was designed as a randomized controlled trial (RCT), but it was not double-blinded. No standard criteria are available for the treatment success by this long tube in the literature. The two kinds of tubes were placed by different methods, while the patients in ileus tube group suffered more during intubation.
RESULTS
Patient clinical characteristics
Of the 186 patients, 96 were treated with ileus tube, and 90 were randomized into NGT group. There was no significant difference between the two groups with regard to clinical characteristics and laboratory variables documented on admission, including age, sex, abdominal symptoms, and laboratory indexes such as WBC counts, CRP, and ESR (P > 0.05). The type of prior surgery and obstruction also did not differ significantly (P > 0.05). In this study, the ileus tube or NGT was successfully placed in all the patients, without any obvious complications. Patient characteristics of the two groups are shown in Table 1.
Table 1.
Clinical characteristics, difference decompression responses and therapeutic efficacies of ileus tube group and nasogastric tube group
| Clinical characteristics | Ileus tube group(n = 96) | NGT group(n = 90) | P value | OR (95% CI) |
| Mean age (yr) | 58 | 54 | 0.07 | - |
| Male/female | 56/40 | 56/34 | 0.59 | - |
| Past laparotomies (n) | 89 | 86 | 0.41 | 0.59 (0.17–2.09) |
| Surgery type | ||||
| Colorectal surgery | 35 | 28 | 0.35 | 1.34 (0.72–2.50) |
| Small-bowel resection | 15 | 14 | 0.92 | 1.04 (0.47–2.31) |
| Gastroduodenal surgery | 8 | 12 | 0.3 | 0.61 (0.24–1.57) |
| Appendectomy | 8 | 6 | 0.62 | 1.32 (0.44–3.97) |
| Gallbladder and pancreas surgery | 4 | 4 | 1 | 0.97 (0.23–3.99) |
| Splenectomy | 3 | 4 | 0.96 | 0.72 (0.16–3.29) |
| Bladder or kidney surgery | 2 | 2 | 1 | 0.97 (0.13–7.01) |
| Gynecologic surgery | 14 | 16 | 0.61 | 0.82 (0.37–1.80) |
| Symptoms on admission (n) | - | |||
| Abdominal pain | 85 | 82 | 0.56 | 0.75 (0.29–1.97) |
| Distention | 93 | 85 | 0.65 | 1.82 (0.42–7.86) |
| Nausea or vomiting | 58 | 65 | 0.09 | 0.59 (0.32–1.09) |
| Disappearance of flatus and defecation | 84 | 72 | 0.17 | 1.75 (0.29–3.88) |
| Laboratory data before intubation (n) | ||||
| Elevated WBC count | 70 | 67 | 0.81 | 0.92 (0.48–1.78) |
| Elevated CRP level | 37 | 42 | 0.26 | 0.72 (0.40–1.29) |
| Elevated ESR level | 31 | 27 | 0.74 | 1.11 (0.60–2.07) |
| Therapeutic efficacies (%) | ||||
| Rate of abdominal pain or distention relieved within 48 h | 95.8 (92/96) | 46.7 (42/90) | < 0.01 (χ2 = 55.75) | 26.29 (8.90–77.66) |
| Surgery rate | 10.4 (10/96) | 53.3 (48/90) | < 0.01 (χ2 = 39.87) | 0.10 (0.05–0.22) |
| Effectiveness rate for recurrent adhesive small bowel obstruction | 95.8 (24/25) | 31.6 (12/38) | < 0.01 (χ2 = 25.55) | 52.00 (6.28–430.67) |
| Total effectiveness rate | 89.6 (86/96) | 46.7 (42/90) | < 0.01 (χ2 = 39.87) | 9.83 (4.53–21.33) |
| Differences in decompression responses by ileus tube and NGT (mean ± SD) | t | |||
| Time for relief of abdominal pain or distention (h) | 23.8 ± 10.9 | 59.1 ± 30.1 | < 0.01 | -10.4 |
| Appearance of flatus and defecation (d) | 2.4 ± 1.7 | 6.5 ± 3.2 | < 0.01 | -10.4 |
| Time to abdominal radiographic improvement (d) | 4.1 ± 2.3 | 8.5 ± 5.0 | < 0.01 | -6.9 |
| WBC recovery (d) | 4.0 ± 2.4 | 7.0 ± 4.8 | < 0.01 | -4.6 |
| CRP recovery (d) | 5.5 ± 2.5 | 8.8 ± 3.9 | < 0.01 | -4.4 |
| ESR recovery (d) | 5.8 ± 2.4 | 8.7 ± 3.9 | < 0.01 | -4.1 |
| Drainage volume on the first day (mL) | 698 ± 428 | 280 ± 167 | < 0.01 | 8.9 |
CI: Confidence interval; CRP: C-reaction protein; ESR: Erythrocyte sedimentation rate; NGT: Nasogastric tube; OR: Odds ratio; SD: Standard deviation; WBC: White blood cells.
Therapeutic efficacies
The time for improvement in abdominal symptoms, radiographic findings, and laboratory variables was significantly shorter (P < 0.01) in the ileus tube group as compared with the NGT group. In addition, more patients had relief from abdominal pain or distention within 48 h in the ileus tube group (P < 0.01). The drainage volume on the first day after intubation was 698 ± 428 mL in the ileus tube group and 280 ± 167 mL in the NGT group, with a significant difference (P < 0.01, t = 8.9). After ileus tube decompression, 86 patients presented clinical or radiographic relief (Figure 2), the tube was removed one week after oral feeding was started, with an effectiveness rate up to 89.6% (86/96). The other 10 patients defined as treatment failure by gastroenterography underwent operation to determine the site of the obstruction (Figure 3). In follow-up study, 6 patients still had recurrent adhesive SBO confirmed by surgery, the intervals varied from one month to seven months. In the control group, the total effectiveness rate was 46.7% (42/90); the other 48 patients defined as treatment failure were managed with surgery. However, 16 patients had recurrent adhesive SBO after successful treatment, the recurrence peak occurred between 3 mo and 5 mo (Table 1).
Figure 2.
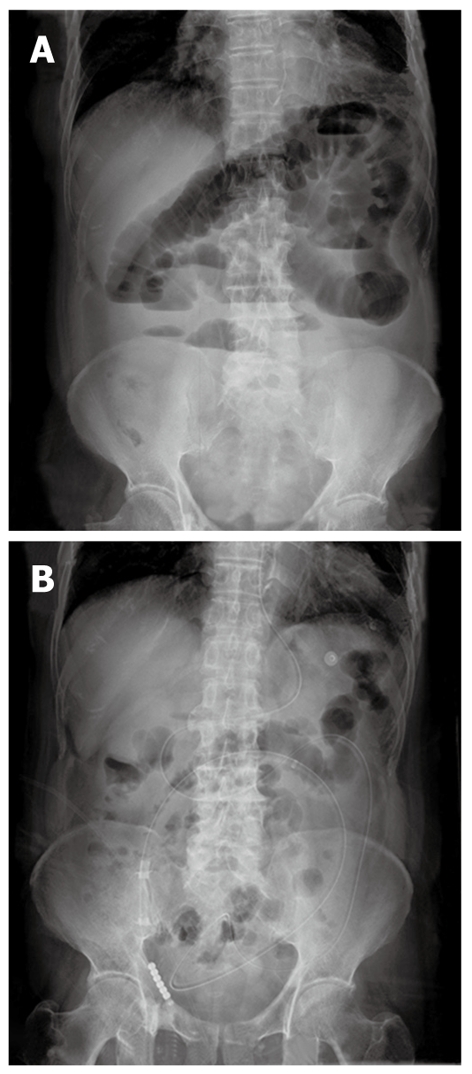
Radiographs of ileus tube decompression. Plain abdominal radiographs (A) and (B) reviewed 3 d after ileus tube decompression compared with scans on admission in a patient with postoperative adhesive small bowel obstruction. A: The diffuse distended loops of small bowel that was filled with gas and fluid before intubation; air-fluid levels were seen in the enteric cavity; B: Reviewed 3 d after intubation; the previous gas-filled or fluid-filled small bowel loops showed no evidence of distention, the air-fluid levels disappeared, and the long tube had moved downward while the tip reached the distal jejunum.
Figure 3.
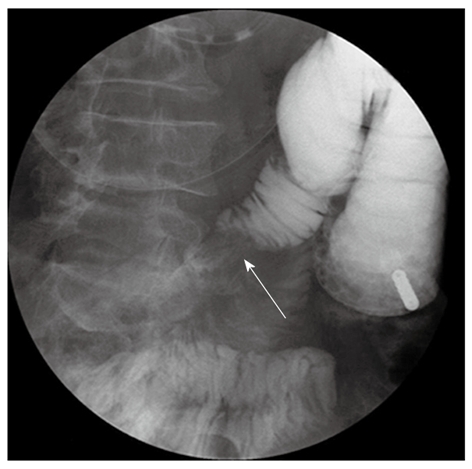
Diagnostic radiographic enteroclysis. Gastroenterography displayed on the 5th day of ileus tube decompression in a patient with postoperative adhesive small bowel obstruction. The tip of the tube had reached to the distal jejunum. After the anterior balloon was inflated with gas, angiografin was injected into the tube for gastrointestinal imaging to locate the lesion or stenosis in the bowel. Stenosis was found (arrow) in the small intestine with a filling defect, but none was developed in the distal bowel.
Therapeutic outcome in ileus tube group treated with or without surgery
In the ileus tube group, 10 patients without initial relief underwent surgery to remove the obstruction. Significant differences were found in the drainage output on the first day and the length of hospital stay (P < 0.05). Besides, no patient showed abdominal radiographic improvement within 72 h in decompression in the surgical group as compared to 51.2% (44/86) in the non-surgical group. These results are summarized in Table 2.
Table 2.
Therapeutic outcomes in ileus tube group treated with or without surgery (mean ± SD)
| Variables | Surgical treatment | Non-surgical treatment | P value | t |
| Cases (n) | 10 | 86 | - | - |
| Time for relief of distention (h) | 27.6 ± 16.9 | 23.4 ± 10.2 | 0.51 | 0.69 |
| Appearance of flatus and defecation (d) | 3.2 ± 2.4 | 2.4 ± 1.7 | 0.27 | 1.12 |
| Radiographic improvement within 72 h (n) | 0 | 44 | - | - |
| WBC recovery (d) | 5.2 ± 1.9 | 4.0 ± 2.4 | 0.26 | 1.14 |
| CRP recovery (d) | 8.3 ± 5.0 | 5.3 ± 2.1 | 0.40 | 1.04 |
| ESR recovery (d) | 5.0 ± 2.8 | 5.9 ± 2.3 | 0.61 | -0.51 |
| Drainage volume on the first day (mL) | 390 ± 287 | 734 ± 428 | 0.02a | -2.47 |
| Length of hospital stay (d) | 33.0 ± 13.7 | 21.5 ± 10.4 | < 0.01a | 3.19 |
P < 0.05 vs therapeutic outcomes in ileus tube group treated with or without surgery. CRP: C-reaction protein; ESR: Erythrocyte sedimentation rate; SD: Standard deviation; WBC: White blood cells.
DISCUSSION
Conservative treatment is usually administered to the patients with acute bowel obstruction when ischemic bowel is excluded. Surgeons are inclined to choose conservative treatment for adhesive bowel obstruction because of the risk of recurrence along with surgery[13]. Since the 1930s, various types of tubes have been devised and used for nasointestinal decompression[14,15]. A tube was designed specifically for endoscopic placement and the ileus tube has been developed with three channels and two balloons. A study confirmed an efficacy rate of ileus tube of up to 85.7% for intraluminal decompression in the bowel[9]. Intubation methods then changed from fluoroscopy to direct placement under endoscopy and afforded safety and high success rates[16-21]. However, if there is any side effect along with the endoscopic placement procedure, the tube should be pulled out and endoscopic treatment for gastrointestinal bleeding or perforation should be given if possible. If patients have aspiration pneumonia, antibiotics and mechanical ventilation should be considered. Intensive care and emergent therapy are needed for any cardiovascular event. Our clinical practice testified the safety and flexibility of the endoscopic placement of the ileus tube, and the procedure and the instruments we used are available in most hospitals. However, the long tube and endoscopy cost more than ¥4000 RMB, that is 20 times more than an ordinary NGT, even though it is much lower than surgery. The cost as well as the discomfort caused by endoscopy may limit the promotion of the use of ileus tube.
From the data of this study, we found a great comparability between our two groups with regard to sex, age, past laparotomies, symptoms, and radiographic signs as well as laboratory findings on admission. It is known that delayed visit to hospital leads to a higher failure in conservative measures, so we selected the patients admitted within 12 h after obstruction onset to enforce the rigidity of the study. With bowel peristalsis and the weighted tip, the ileus tube passes downward to the small bowel and decompression can be achieved. As the tip can reach to the site of obstruction, thorough suctioning can be performed, leading to a rapid relief of the symptoms, as shown in our results. In addition, the recovery time for laboratory variables of inflammatory markers was shorter in ileus tube group, probably because of the improvement in the blood supply to the bowel wall, which can reduce the local inflammatory response and bacterial multiplication. A previous study demonstrated no significant differences in therapeutic efficacy between the long and short tube decompression[8]. However, we found that in the ileus tube group the effectiveness rate was significantly higher and the surgery rate was lower than that in the control group. We attribute it to the advanced technique of the tube and the endoscopic placement method that can avoid the delay by passing beyond the pylorus. Another study confirmed that a previous episode of adhesive bowel obstruction and the duration of the tips not advancing (> 72 h) were highly correlated with a recurrence of obstruction. If patients fail to respond 3 d after decompression or have indications of ischemic bowel or the drainage volume is > 500 mL on the third day, surgery is recommended[22,23]. For NGT decompression, after 48 h of non-operative management, the risk of complications increases substantially, and the probability for resolving the obstruction diminishes. Surgery is required if a patient’s condition has deteriorated or has not significantly improved within 72 h. In the ileus tube group, intermittent lavage was performed from the second day after intubation so that we could record the drainage volume on the first 24 h to compare the decompression responses with the NGT group.
We admitted relatively a large number of patients with adhesive SBO for this study. Our results showed that for adhesive SBO, the ileus tube had the decompression efficacy that was significantly superior to the NGT, especially for patients with recurrent adhesive SBO. Although a tendency toward recurrence can not be avoided after successful treatment using the ileus tube in patients with past episodes, it is still superior to the traditional NGT treatment and should be therefore recommended in clinical practice. The ileus tube has many advantages in addition to thorough decompression. It can remove the kinks in the obstructed bowel loops when the tip progresses downward, and the long tube itself can perform through a straddle mechanism to arrange the bowel and reduce the adhesion recurrence rate. Diagnostic radiographic enteroclysis studies are facilitated, which are helpful to surgeons for preoperative preparation[24,25].
Previous studies have confirmed the efficacy of nasointestinal decompression through a long tube for SBO, especially for adhesive SBO[3-7]. The approach of endoscopic placement of the long tube was also advised[15,26]. According to our clinical application, the ileus tube has a prospective therapeutic efficacy for adhesive SBO. However, surgical intervention can easily be undertaken when NGT decompression failed, because it is thought to be the most immediate modality for remission. Another focus is that water-soluble contrast agent (WSCA) is helpful in the diagnosis and treatment of adhesive SBO according to a recent meta-analysis[27], appearance of contrast in the colon within 4-24 h after administration had a sensitivity of 96% and a specificity of 98% in predicting resolution of SBO. The WSCA can draw fluid from intravascular and extracellular spaces into bowel lumen because of its high osmolarity, thus promoting proximal bowel distension and peristalsis, and avoiding the operative interference. However, as there are potential risks of renal failure and anaphylaxis, these agents still can not take the place of gastrointestinal decompression, which is thought to be the key to the treatment of bowel obstruction. Based on our results, we highly recommend this triple-lumen tube for patients with adhesive SBO. The endoscopic placement of the tube is convenient, and with close monitoring and intermittent lavage, surgeries can be avoided.
We also tried to find certain indications for surgical interventions in the patients treated with ileus tube. Compared with patients who underwent surgery in the ileus tube group, those who were successfully managed without surgery had a significantly shorter hospital stay and a larger drainage output on the first day after intubation. Up to 51.2% of the patients showed abdominal radiographic improvement within the first 3 d in the non-surgical group while no patient achieved relief in the surgical group. This indicates that the drainage output on the first day and radiographic improvement could be two independent factors for evaluating the therapeutic efficacy of nasointestinal decompression. They may also be indications for surgery. Further studies should be performed to identify the clinical value of the ileus tube within the parameters of indications for surgery.
In summary, we believe that endoscopic placement of transnasal ileus tube is safe, effective, and convenient and is worth being promoted in clinical practice. The ileus tube can quickly relieve the clinical symptoms and reduce the rate of surgical indications. It is greatly superior to the NGT in treating patients with adhesive SBO. However, the potential risks and extra costs should be taken into consideration when selecting patients. For patients with recurrent adhesive SBO, the use of triple-lumen ileus tube is the optimal choice. Close observation of drainage output and abdominal radiographic changes during decompression can help provide some clues for indications of surgery.
COMMENTS
Background
Adhesive small bowel obstruction is a worldwide problem characterized by a high incidence rate and repeated episodes. Gastrointestinal decompression is one of the important approaches in conservative therapy. However, surgical intervention can easily be undertaken when nasogastric tube decompression failed. Long intestinal tube for nasointestinal decompression is a new method for adhesive small bowel obstruction and has been successfully applied in clinical practice and the therapeutic efficacies were satisfactory.
Research frontiers
A new long tube named ileus tube was first introduced in Japan in 2003, and later studies have confirmed its therapeutic value in adhesive small bowel obstruction. However, there had been no randomized controlled study about the efficacy of the ileus tube. This randomized controlled trial attempted to investigate and compare the decompression efficacy between the new ileus tube and the traditional nasogastric tube (NGT) for patients with adhesive small bowel obstruction.
Innovations and breakthroughs
The previous studies of long intestinal tube for gastrointestinal decompression were mainly described retrospectively. This research compared the therapeutic efficacies between the new long tube and the ordinary NGT in a large number of patients. The authors confirmed the superiority of the new ileus tube to the ordinary NGT through a series of statistical analysis. The authors also introduced the detailed procedure of the endoscopic placement of this long tube.
Applications
The study indicated the therapeutic value of the new ileus tube. The application of the ileus tube can significantly reduce the surgery rate and the hospital-stay cost, and the endoscopic placement method introduced by the authors can be applied in almost all the hospitals. Thus, the use of ileus tube is worthy to be promoted.
Peer review
This is an important area and the work represents a significant advance in clinical therapy. As it is possible not only to increase efficacy on a single intervention but also reduce the need for subsequent intervention, the technology provides the possibility to lower costs and reduce intervention to the patient.
Footnotes
Peer reviewers: Dr. Giuseppe Chiarioni, Azienda Ospedaliera di Verona, Division of Gastrointestinal Rehabilitation, Ospedale di Valeggio s/M, 37067 Valeggio, Italy; Mauro Bortolotti, Professor, University of Bologna, Internal Medicine and Gastroenterology, Via Massarenti 48, 40138 Bologna, Italy
S- Editor Gou SX L- Editor Ma JY E- Editor Zhang DN
References
- 1.Plusczyk T, Bolli M, Schilling M. [Ileus disease] Chirurg. 2006;77:898–903. doi: 10.1007/s00104-006-1237-9. [DOI] [PubMed] [Google Scholar]
- 2.Shittu OB, Gana JY, Alawale EO, Ogundiran TO. Pattern of mechanical intestinal obstruction in Ibadan: a ten year review. Afr J Med Med Sci. 2001;30:17–21. [PubMed] [Google Scholar]
- 3.Wolfson PJ, Bauer JJ, Gelernt IM, Kreel I, Aufses AH. Use of the long tube in the management of patients with small-intestinal obstruction due to adhesions. Arch Surg. 1985;120:1001–1006. doi: 10.1001/archsurg.1985.01390330013002. [DOI] [PubMed] [Google Scholar]
- 4.Gowen GF. Long tube decompression is successful in 90% of patients with adhesive small bowel obstruction. Am J Surg. 2003;185:512–515. doi: 10.1016/s0002-9610(03)00074-6. [DOI] [PubMed] [Google Scholar]
- 5.Snyder CL, Ferrell KL, Goodale RL, Leonard AS. Nonoperative management of small-bowel obstruction with endoscopic long intestinal tube placement. Am Surg. 1990;56:587–592. [PubMed] [Google Scholar]
- 6.Sprouse LR, Arnold CI, Thow GB, Burns RP. Twelve-year experience with the Thow long intestinal tube: a means of preventing postoperative bowel obstruction. Am Surg. 2001;67:357–360. [PubMed] [Google Scholar]
- 7.Fazel MZ, Jamieson RW, Watson CJ. Long-term follow-up of the use of the Jones’ intestinal tube in adhesive small bowel obstruction. Ann R Coll Surg Engl. 2009;91:50–54. doi: 10.1308/003588409X358999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleshner PR, Siegman MG, Slater GI, Brolin RE, Chandler JC, Aufses AH. A prospective, randomized trial of short versus long tubes in adhesive small-bowel obstruction. Am J Surg. 1995;170:366–370. doi: 10.1016/s0002-9610(99)80305-5. [DOI] [PubMed] [Google Scholar]
- 9.Tanaka S, Yamamoto T, Kubota D, Matsuyama M, Uenishi T, Kubo S, Ono K. Predictive factors for surgical indication in adhesive small bowel obstruction. Am J Surg. 2008;196:23–27. doi: 10.1016/j.amjsurg.2007.05.048. [DOI] [PubMed] [Google Scholar]
- 10.Cox MR, Gunn IF, Eastman MC, Hunt RF, Heinz AW. The safety and duration of non-operative treatment for adhesive small bowel obstruction. Aust N Z J Surg. 1993;63:367–371. doi: 10.1111/j.1445-2197.1993.tb00404.x. [DOI] [PubMed] [Google Scholar]
- 11.Sosa J, Gardner B. Management of patients diagnosed as acute intestinal obstruction secondary to adhesions. Am Surg. 1993;59:125–128. [PubMed] [Google Scholar]
- 12.Catena F, Di Saverio S, Kelly MD, Biffl WL, Ansaloni L, Mandalà V, Velmahos GC, Sartelli M, Tugnoli G, Lupo M, et al. Bologna Guidelines for Diagnosis and Management of Adhesive Small Bowel Obstruction (ASBO): 2010 Evidence-Based Guidelines of the World Society of Emergency Surgery. World J Emerg Surg. 2011;6:5. doi: 10.1186/1749-7922-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duron JJ, Silva NJ, du Montcel ST, Berger A, Muscari F, Hennet H, Veyrieres M, Hay JM. Adhesive postoperative small bowel obstruction: incidence and risk factors of recurrence after surgical treatment: a multicenter prospective study. Ann Surg. 2006;244:750–757. doi: 10.1097/01.sla.0000225097.60142.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maglinte DD, Stevens LH, Hall RC, Kelvin FM, Micon LT. Dual-purpose tube for enteroclysis and nasogastric-nasoenteric decompression. Radiology. 1992;185:281–282. doi: 10.1148/radiology.185.1.1523326. [DOI] [PubMed] [Google Scholar]
- 15.Gowen GF. Rapid resolution of small-bowel obstruction with the long tube, endoscopically advanced into the jejunum. Am J Surg. 2007;193:184–189. doi: 10.1016/j.amjsurg.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 16.Kim IG. Endoscopic guided intubation of long nasointestinal decompression tube. Surg Gynecol Obstet. 1985;161:282–284. [PubMed] [Google Scholar]
- 17.Gowen GF, DeLaurentis DA, Stefan MM. Immediate endoscopic placement of long intestinal tube in partial obstruction of the small intestine. Surg Gynecol Obstet. 1987;165:456–458. [PubMed] [Google Scholar]
- 18.Ishizuka M, Nagata H, Takagi K, Kubota K. Transnasal fine gastrointestinal fiberscope-guided long tube insertion for patients with small bowel obstruction. J Gastrointest Surg. 2009;13:550–554. doi: 10.1007/s11605-008-0587-7. [DOI] [PubMed] [Google Scholar]
- 19.Frech EJ, Adler DG. Endoscopic therapy for malignant bowel obstruction. J Support Oncol. 2007;5:303–310, 319. [PubMed] [Google Scholar]
- 20.Kanno Y, Hirasawa D, Fujita N, Noda Y, Kobayashi G, Ishida K, Ito K, Obana T, Suzuki T, Sugawara T, et al. Long intestinal tube insertion with the ropeway method facilitated by a guidewire placed by transnasal ultrathin endoscopy for bowel obstruction. Dig Endosc. 2009;21:196–200. doi: 10.1111/j.1443-1661.2009.00886.x. [DOI] [PubMed] [Google Scholar]
- 21.Sato R, Watari J, Tanabe H, Fujiya M, Ueno N, Konno Y, Ishikawa C, Ito T, Moriichi K, Okamoto K, et al. Transnasal ultrathin endoscopy for placement of a long intestinal tube in patients with intestinal obstruction. Gastrointest Endosc. 2008;67:953–957. doi: 10.1016/j.gie.2008.01.043. [DOI] [PubMed] [Google Scholar]
- 22.Sakakibara T, Harada A, Ishikawa T, Komatsu Y, Yaguchi T, Kodera Y, Nakao A. Parameter predicting the recurrence of adhesive small bowel obstruction in patients managed with a long tube. World J Surg. 2007;31:80–85. doi: 10.1007/s00268-006-0158-6. [DOI] [PubMed] [Google Scholar]
- 23.Sakakibara T, Harada A, Yaguchi T, Koike M, Fujiwara M, Kodera Y, Nakao A. The indicator for surgery in adhesive small bowel obstruction patient managed with long tube. Hepatogastroenterology. 2007;54:787–790. [PubMed] [Google Scholar]
- 24.Maglinte DD, Kelvin FM, Micon LT, Dorenbusch MJ, Chernish SM, Graffis RF, Stevens LH, Lappas JC. Nasointestinal tube for decompression or enteroclysis: experience with 150 patients. Abdom Imaging. 1994;19:108–112. doi: 10.1007/BF00203482. [DOI] [PubMed] [Google Scholar]
- 25.Maglinte DD, Kelvin FM, Sandrasegaran K, Nakeeb A, Romano S, Lappas JC, Howard TJ. Radiology of small bowel obstruction: contemporary approach and controversies. Abdom Imaging. 2005;30:160–178. doi: 10.1007/s00261-004-0211-6. [DOI] [PubMed] [Google Scholar]
- 26.Endo H, Inamori M, Murakami T, Yoshida K, Higurashi T, Iida H, Takahashi H, Akiyama T, Akimoto K, Sakamoto Y, et al. Usefulness of transnasal ultrathin endoscopy for the placement of a postpyloric decompression tube. Digestion. 2007;75:181. doi: 10.1159/000107937. [DOI] [PubMed] [Google Scholar]
- 27.Branco BC, Barmparas G, Schnüriger B, Inaba K, Chan LS, Demetriades D. Systematic review and meta-analysis of the diagnostic and therapeutic role of water-soluble contrast agent in adhesive small bowel obstruction. Br J Surg. 2010;97:470–478. doi: 10.1002/bjs.7019. [DOI] [PubMed] [Google Scholar]


