Abstract
Context
Critical Access Hospitals (CAHs) play a crucial role in the nation’s rural safety net. Current policy efforts have focused primarily on helping these small, isolated hospitals remain financially viable to ensure access for Americans living in rural areas. However, we know little about the quality of care they provide, or the outcomes their patients achieve.
Objective
To examine the quality of care and patient outcomes at CAHs, and to understand why patterns of care might differ for CAHs versus non-CAHs.
Design
Retrospective analysis of national data from Medicare and other sources.
Setting
U.S. hospitals.
Patients
Medicare fee-for-service beneficiaries with acute myocardial infarction (AMI), congestive heart failure (CHF), and pneumonia, discharged in 2008–2009.
Main Outcome Measures
Clinical capabilities, performance on processes of care, and 30-day mortality rates.
Results
Compared to other hospitals, CAHs were less likely to have intensive care units (30.0% versus 74.4%, p<0.001), cardiac catheterization capabilities (0.5% versus 47.7%, p<0.001), and at least basic electronic health records (4.6% versus 9.9%, p<0.001). CAHs had lower performance on process measures than non-CAHs for all three conditions examined (Hospital Quality Alliance summary score for AMI 91.0% versus 97.8%, for CHF, 80.6% versus 93.5%, and for pneumonia 89.3% versus 93.7%, p<0.001 for each). Patients admitted to a CAH had higher 30-day mortality rates for each condition than those admitted to non-CAHs (for AMI, 23.5% versus 16.2%, Odds Ratio (OR) 1.70 (95% confidence interval 1.61, 1.80), p<0.001; for CHF, 13.4% versus 10.9%, OR 1.28 (1.23, 1.32), p<0.001; and for pneumonia 14.1% versus 12.1%, OR 1.20 (1.16, 1.24) p<0.001).
Conclusions
Care in CAHs, compared with non-CAHs, is associated with worse processes of care and higher mortality rates.
Introduction
Critical Access Hospitals (CAHs) play an important and unique role in the nation’s healthcare system, caring for Americans who live in rural areas and might otherwise have no accessible inpatient provider. This hospital designation, created by the Medicare Rural Hospital Flexibility Program of the 1997 Balanced Budget Act, resulted from a federal effort to increase resources for small, geographically isolated hospitals, many of which were struggling financially. The bill defined CAHs as hospitals with no more than 25 acute care beds, located more than 35 miles from the nearest hospital; hospitals that converted to CAH status became eligible for cost-based reimbursement rather than diagnosis-related group (DRG)-based reimbursement.1 As a result, margins improved and closures among these small rural hospitals fell dramatically;2, 3 over a quarter of the acute care hospitals in this country now have the CAH designation.
The CAH designation was created with the goal of ensuring “proximate access” to basic inpatient and emergency care close to home for the approximately 20% of the U.S. population that still lives in rural communities.4 The program has been highly successful in protecting access to inpatient care for rural communities, while providing care that receives high scores on patient satisfaction.5 However, despite broad policy interest in helping CAHs provide access to inpatient care, we have little information about the quality of care they provide: these hospitals are exempt from reporting to both the Joint Commission performance measure program6 and the Hospital Quality Alliance (HQA) national public reporting program.7 We are unaware of recent national data comparing outcomes at these hospitals to a national sample. CAHs have less access to capital and fewer health care providers in their communities, including fewer specialists.8 Therefore, these hospitals may face equal or greater challenges in delivering high quality care9 compared with other vulnerable hospitals, such as Safety Net providers, that have been more extensively studied.10 Understanding whether the Critical Access designation has been helpful in not just improving access, but also in ensuring high quality care, is a key element in evaluating federal efforts to ensure an effective rural health system.
Therefore, we sought to examine CAHs’ clinical and personnel resources, the quality of care they deliver, and their patients’ outcomes. We focused on three common conditions: congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia. We also sought to identify what factors, such as clinical capabilities, size, patient volume, or other related issues, might explain any differences in outcomes of care.
Methods
Data
Hospitals
We used the Medicare Provider Analysis and Review file (MedPAR) to identify non-federal hospitals providing acute care services to Medicare beneficiaries in the 50 U.S. states or District of Columbia. We used the 2009 American Hospital Association (AHA) survey to obtain data on hospital characteristics including critical access designation, size, ownership, teaching status, and region. We linked these data with the 2009 Area Resource File (ARF), which contains county-level data on median household income and poverty rate. While the original legislation specified that only isolated rural hospitals qualified for CAH status, states subsequently granted exemptions for this rule, allowing some hospitals in suburban or even urban settings to be eligible. Therefore, we linked the Rural Urban Commuting Area (RUCA) codes, which detail population density and urbanization at a granular level to examine the degree to which rurality affected our findings.11
Patients
We defined our study population as Medicare Fee-for-Service beneficiaries admitted to the hospitals in our sample in 2008 or 2009 with a primary discharge diagnosis of AMI, CHF, or pneumonia (International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9) codes for CHF 398.91, 404.x1, 404.x3, 428.0 to 428.9, for AMI 410.xx, excluding 410.x2, and for pneumonia 480 to 486). Patient race was categorized based on self-report, as reported to Medicare. We followed the Center for Medicare and Medicaid Services (CMS) approach for classifying “index admissions”,12 allowing patients to be included in the sample more than once. All patients were assigned to the admitting hospital regardless of whether they were transferred. Our final patient population included 2,351,701 admissions across these three conditions.
Outcomes
We used the AHA survey to quantify resources that have been associated with better care,14, 15 including the presence of an intensive care unit, the ability to perform cardiac catheterization or surgery, and nurse staffing levels. Nurse staffing was estimated by calculating the number of full-time equivalent nurses on staff per 1000 patient-days.16, 17 We used the ARF to estimate the total physician and subspecialist supply for the county in which each hospital was located. Each hospital’s HIT resources were determined from the AHA HIT survey, which was distributed to every acute-care hospital in the U.S. in 2009. The survey asked responding hospitals to report the degree of adoption of specific electronic health record (EHR) functions and achieved a response rate of 63%.18
We used Hospital Quality Alliance (HQA) data to obtain hospitals’ performance on process measures for AMI, CHF, and pneumonia during 2009; because of sample size cutoffs and reporting exemptions, these measures were available for only a subset of the hospitals in our sample. We calculated an overall performance score for each hospital for each condition19 (see eTable 1 for list of measures). We used Medicare data to calculate mortality within 30 days of admission. Each patient’s likelihood of death was adjusted for age, sex, race, and medical comorbidities using the CMS Hierarchical Condition Category (HCC) mortality models,20 which were developed by CMS and have been demonstrated in recent studies to have a superior c-statistic and predictive accuracy than the Charlson and Elixhauser methods.21
Analysis
We compared summary statistics for hospital characteristics, demographics, and patient comorbidities between CAHs and non-CAHs using chi-square tests and t-tests or Wilcoxon tests as appropriate. We used chi-square tests to compare the presence of each clinical resource and functionality between CAHs and non-CAHs. We analyzed performance on the HQA metrics, weighting each hospital’s performance by its number of patients with that diagnosis. We then created weighted hospital-level linear regression models for risk-adjusted 30-day mortality rates.
We subsequently built multivariable regression models. We first adjusted for factors that are outside the control of the hospitals and policy makers, including region, hospital ownership, and median county income. We next added variables to the model that we postulated might be in the explanatory pathway between CAH status and outcomes, and might be amenable to change by either hospitals or policy makers. We did this in a stepwise fashion, first adding measures of clinical personnel, followed by clinical resources and system membership, the presence of an EHR, and annual condition-specific case volume. Finally, we examined models adjusting for rurality using the RUCA codes (divided into urban, large town, small town, and rural categories). While rurality is highly collinear with being a CAH, it may also be correlated with other, unmeasured (or inadequately measured) factors including travel time and quality of clinical personnel and resources.
Because CAHs transfer more patients than non-CAHs, we examined, in sensitivity analyses, differences in mortality rates after excluding all transfers. To better understand whether differences in outcomes between CAHs and other hospitals were driven primarily by size and rural status, or whether these differences might be driven by other factors such as CAHs’ exemption from reporting or payment mechanisms, we conducted additional sensitivity analyses, restricting our sample to small, rural hospitals. Finally, we used established methods3, 4 to model the degree of association between an unmeasured confounder and both our primary predictor (CAH status) and our outcome (mortality) that would have had to be present in order to eliminate our findings.
To account for multiple comparisons, we considered a two-sided p-value of less than 0.008 to be significant. Analyses were performed using SAS version 9.2 (Cary, NC).
Results
Hospital characteristics and resources
Of the 4,738 hospitals providing acute care to Medicare beneficiaries in 2008–2009, 1,268 (27%) were designated as CAHs. The median number of operational beds in a CAH was 18 (interquartile range (IQR) 14, 23), compared with 82 (IQR 41, 154) for non-CAHs (Table 1). CAHs were more likely to be publicly owned, and less likely to be a teaching hospital, located in an urban area or large town, or part of a hospital system. Nearly half of the CAHs were located in the Midwest. In general, CAHs were located in counties with a lower median income than non-CAHs and served a higher proportion of Medicare patients but a lower proportion of Medicaid patients.
Table 1.
Comparison of hospital characteristics between CAHs and non-CAHs
| Hospital Characteristics | Critical Access Hospitals N=1268 |
Non-Critical Access Hospitals N=3470 |
|
|---|---|---|---|
| Medical/surgical hospital bed capacity, median (IQR) | 18 (14, 23) | 82 (41, 154) | |
| Ownership | Public | 559 (44.1%) | 571 (16.5%) |
| For-profit | 50 (3.9%) | 781 (22.5%) | |
| Non-profit | 659 (52.0%) | 2118 (61.0%) | |
| Major teaching hospital | 0 (0%) | 285 (8.2%) | |
| Rural/urban category (RUCA) | Urban | 59 (4.7%) | 2287 (66.0%) |
| Large town | 120 (9.5%) | 698 (20.2%) | |
| Small town | 628 (49.5%) | 379 (10.8%) | |
| Rural | 461 (36.4%) | 106 (3.1%) | |
| Region | Northeast | 65 (5.1%) | 548 (15.8%) |
| Midwest | 621 (49.0%) | 778 (22.4%) | |
| South | 332 (26.2%) | 1495 (43.1%) | |
| West | 250 (19.7%) | 649 (18.7%) | |
| County income, median (IQR) | $29,041 (25,795, 32,723) | $34,619 (28,841, 41,626) | |
| Percent county poverty, median, (IQR)† | 13.5% (10.8, 17.2) | 14.3% (10.6, 17.1) | |
| Proportion Medicare patients, median (IQR) | 56.8% (50.6, 67.3) | 45.3% (40.0, 52.2) | |
| Proportion Medicaid patients, median (IQR) | 11.2% (6.3, 16.1) | 16.6% (11.2, 21.3) | |
| Volume of Medicare patients, median (IQR)* | AMI | 7 (3, 12) | 84 (29, 203) |
| CHF | 35 (19, 58) | 206 (102, 391) | |
| Pneumonia | 60 (34, 94) | 193 (111, 312) | |
AMI = acute myocardial infarction; CHF = congestive heart failure; IQR = Interquartile Range; RUCA=Rural Urban Commuting Area (Urban = 50,000 or more, Large town = 10,000–49,999, Small town = 2,500–9,999, Rural = <2,500)
Over the 23 month study period.
p-value >0.05. Otherwise p-value for all comparisons <0.001.
Patient characteristics
We identified 2,351,701 index admissions for CHF, AMI, or pneumonia during our study period, of which 149,989 were to CAHs. Patients admitted to CAHs tended to be older, and had a higher incidence of diabetes and depression, but a lower incidence of hypertension, renal failure, and chronic lung disease (Table 2). Patients admitted to CAHs were more likely to be transferred to another acute care hospital than those admitted to non-CAHs (AMI 29.7% versus 9.5%, CHF 7.4% versus 2.5%, pneumonia 5.6% versus 1.5%, p<0.001 for each), and had significantly shorter lengths of stay for all three conditions. Patients admitted to CAHs were less likely to be transferred to a hospice at the time of discharge than patients admitted to non-CAHs.
Table 2.
Comparison of patient characteristics between CAHs and non-CAHs
| Patient characteristics | Acute myocardial infarction | Congestive heart failure | Pneumonia | ||||
|---|---|---|---|---|---|---|---|
| CAH N=10,703 |
Non-CAH N=469,695 |
CAH N=52,927 |
Non-CAH N=958,790 |
CAH N=86,359 |
Non-CAH N=773,227 |
||
| Age (median, IQR) | 84 (77, 89) | 78 (72, 85) | 83 (76, 88) | 81 (74, 87) | 81 (74, 87) | 80 (73, 86) | |
| Female sex | 58.1% | 49.2% | 58.7% | 54.9% | 54.6% | 54.6%** | |
| Race | White | 95.7% | 87.8% | 93.6% | 83.8% | 95.0% | 87.6% |
| Black | 2.5% | 7.6% | 4.2% | 11.7% | 2.5% | 7.5% | |
| Hispanic | 0.4% | 1.6% | 0.5% | 1.9% | 0.5% | 1.9% | |
| Other/Unknown | 1.4% | 3.0% | 1.7% | 2.6% | 2.0% | 3.0% | |
| Hypertension | 52.9% | 57.7% | 51.3% | 57.4% | 48.6% | 55.0% | |
| Diabetes | 30.1% | 23.7% | 34.8% | 31.3% | 24.6% | 23.7% | |
| Chronic pulmonary disease | 21.6% | 18.6% | 31.9% | 30.9% | 43.5% | 44.8% | |
| Chronic kidney disease | 16.0% | 16.9%* | 20.6% | 28.8% | 9.5% | 14.1% | |
| Peripheral vascular disease | 6.6% | 8.9% | 5.9% | 7.1% | 4.5% | 5.1% | |
| Depression | 4.9% | 3.1% | 5.8% | 3.9% | 7.6% | 6.7% | |
| Length of stay (mean, SD) | 3.0 (1.2) | 4.9 (2.6) | 3.6 (0.7) | 5.2 (3.8) | 4.1 (0.8) | 5.9 (2.4) | |
| Discharged to hospice | 2.8% | 3.7% | 1.2% | 3.2% | 1.0% | 3.0% | |
p=0.01,
p>0.05.
Groups may not sum to 100% due to rounding. P value <0.001 for each comparison except where indicated. Patients assigned to the admitting hospital for purposes of categorization.
Clinical Resources
CAHs had fewer clinical resources than other hospitals: they were less likely to have intensive care units, cardiac catheterization capability, or the ability to perform surgeries (Table 3). CAHs had comparable nurse-staffing levels to non-CAHs, but were located in counties with fewer specialists, with a seven-fold difference in the supply of cardiologists and pulmonologists per 100,000 population.
Table 3.
Comparison of clinical resources between CAHs and non-CAHs
| Clinical Resources | Critical Access Hospitals (N=1268) |
Non-Critical-Access Hospitals (N=3470) |
P value |
|---|---|---|---|
| Member of hospital system | 374 (29.5%) | 1653 (47.6%) | <0.001 |
| Medical intensive care unit | 380 (30.0%) | 2581 (74.4%) | <0.001 |
| Cardiac intensive care unit* | 120 (11.1%) | 1301 (44.0%) | <0.001 |
| Cardiac catheterization | 6 (0.5%) | 1654 (47.7%) | <0.001 |
| PET scanner* | 26 (2.4%) | 632 (21.4%) | <0.001 |
| Surgical capability | 1104 (87.1%) | 3386 (97.6%) | <0.001 |
| Nurse-to-census ratio, median (IQR) | 6.9 (2.6, 11.2) | 6.4 (4.9, 8.2) | 0.35 |
| Total physicians per 100,000 (mean, SD)† | 92.6 (94.6) | 256.0 (210.3) | <0.001 |
| Generalists per 100,000 (mean, SD)† | 50.0 (36.1) | 52.2 (29.0) | <0.001 |
| Cardiologists per 100,000 (mean, SD)† | 1.0 (3.3) | 7.0 (7.2) | <0.001 |
| Pulmonologists per 100,000 (mean, SD)† | 0.4 (1.4) | 3.3 (3.3) | <0.001 |
=of 4033 hospitals reporting these measures.
=reported at the county level; means reported because medians were zero for CAHs and therefore less interpretable.
PET = positron emission tomography.
CAHs were less likely to have the key functions that comprise an EHR. Overall, just 4.6% of CAHs had at least a basic EHR18 compared with 9.9% of non-CAHs. Each EHR component, including clinical documentation, results viewing, computerized physician order entry, and decision support was present less often at CAHs; we found no difference in adoption of telemedicine (Table 4). CAHs were also less likely to be exchanging clinical data electronically with other hospitals or with outpatient practices.
Table 4.
Comparison of Health Information Technology resources between CAHs and non-CAHs*
| Health Information Technology component | Critical Access Hospitals N=1241 |
Non-Critical-Access Hospitals N=3208 |
P value | |
|---|---|---|---|---|
| Overall EHR adoption | Comprehensive | 17 (1.4%) | 100 (3.1%) | <0.001 |
| Basic | 63 (5.1%) | 345 (10.8%) | ||
| None | 1160 (93.5%) | 2763 (86.1%) | ||
| Clinical Documentation | ||||
| Medication lists | 575 (46.3%) | 2373 (74.0%) | <0.001 | |
| Physician notes | 299 (24.1%) | 1162 (36.2%) | <0.001 | |
| Problem lists | 399 (32.2%) | 1642 (51.2%) | <0.001 | |
| Results Viewing | ||||
| Laboratory results | 816 (65.8%) | 2928 (91.3%) | <0.001 | |
| Radiologic reports | 857 (69.1%) | 2941 (91.7%) | <0.001 | |
| Computerized Physician Order Entry | ||||
| Medications | 240 (19.3%) | 1077 (33.6%) | <0.001 | |
| Decision Support Tools | ||||
| Clinical guidelines | 236 (19.0%) | 1185 (36.9%) | <0.001 | |
| Clinical reminders | 277 (22.3%) | 1397 (43.6%) | <0.001 | |
| Drug-drug interaction alerts | 538 (43.4%) | 2245 (70.0%) | <0.001 | |
| Telemedicine | ||||
| Any telemedicine | 441 (35.5%) | 1143 (35.6%) | 0.95 | |
| Health Information Exchange | ||||
| Any exchange with another hospital | 618 (49.8%) | 1935 (60.3%) | <0.001 | |
| Any exchange with a physician practice | 326 (26.3%) | 1522 (47.4%) | <0.001 | |
Based on responses from the hospitals that returned the HIT survey; all results are weighted for nonresponse bias to produce a representative sample.
Percentages indicate the proportion of hospitals responding that the function is active in at least one unit of the hospital.
CAH=Critical Access Hospital; EHR=Electronic Health Record.
Processes of Care
For all three conditions, CAHs had lower performance on HQA measures than non-CAHs among reporting hospitals (Figure 1). For patients admitted with AMI, CAHs provided care that was concordant with HQA process measures 91.0% of the time compared to 97.8% for non-CAHs (difference of 6.8%, p<0.001). The difference was larger for CHF (12.9%) and smaller but still significant for pneumonia (4.4%). For 14 of the 17 individual measures, CAHs performed worse than non-CAHs (eTable 2). These differences persisted after adjusting for case mix and hospital characteristics (eTable 3)
Figure 1.
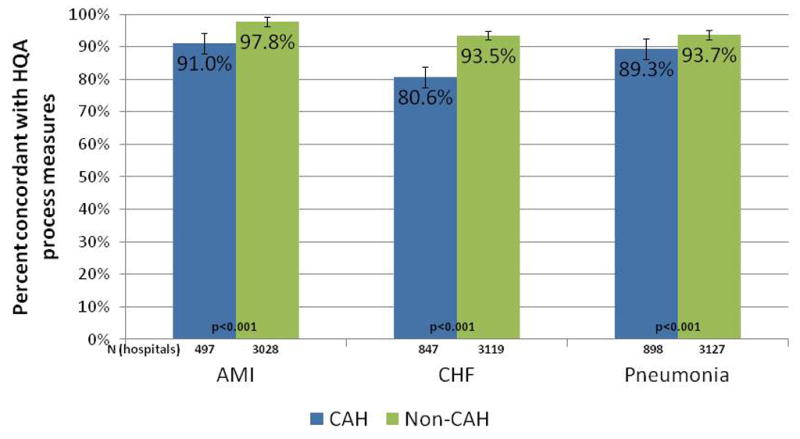
Hospital Quality Alliance summary scores, mean percent concordant
AMI=acute myocardial infarction; CHF=congestive heart failure; CAH=Critical Access Hospital; HQA=Hospital Quality Alliance.
Clinical Outcomes
Patients admitted to CAHs had higher 30-day risk-adjusted mortality rates for all three conditions than patients admitted to non-CAHs (Table 5). Patients admitted to a CAH had 7.3% higher absolute 30-day mortality rates for AMI (23.5% versus 16.2%, Odds Ratio (OR) 1.70, 95% confidence interval (CI) 1.61, 1.80, p<0.001); 2.5% higher mortality rates for CHF (13.4% versus 10.9%, OR 1.28, 95% CI 1.23 to 1.32, p<0.001); and 2% higher mortality rates for pneumonia (14.1% versus 12.1%, OR 1.20, 95% CI1.16 to 1.24, p<0.001) than those admitted elsewhere. When we limited our analyses to non-transferred patients, our results were similar (eTable 4).
Table 5.
Risk-adjusted 30-day mortality rates among Critical Access and non-Critical Access hospitals for common medical conditions.
| AMI | CHF | Pneumonia | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Model specifications | CAH | Non-CAH | Odds Ratio | CAH | Non-CAH | Odds Ratio | CAH | Non-CAH | Odds Ratio |
| Raw mortality rates | 25.2% | 15.2% | 13.8% | 10.6% | 13.0% | 11.9% | |||
| Adjusted for age, sex, race, and medical comorbidities | 23.5% | 16.2% | 1.70 (1.61, 1.80) | 13.4% | 10.9% | 1.28 (1.23, 1.32) | 14.1% | 12.1% | 1.20 (1.16, 1.24) |
| Add use of hospice services | 24.6% | 16.3% | 1.86 (1.75, 1.98) | 14.6% | 11.0% | 1.44 (1.39, 1.49) | 15.0% | 12.2% | 1.32 (1.28, 1.36) |
| Add ownership, region, income | 22.1% | 16.1% | 1.61 (1.51, 1.71) | 13.1% | 11.0% | 1.25 (1.21, 1.30) | 13.6% | 12.3% | 1.14 (1.07, 1.22) |
| Add clinical personnel | 23.2% | 16.0% | 1.75 (1.64, 1.86) | 15.5% | 10.6% | 1.65 (1.46, 1.86) | 13.7% | 12.1% | 1.17 (1.09, 1.26) |
| Add clinical resources, system | 20.0% | 16.1% | 1.39 (1.30, 1.49) | 14.1% | 10.6% | 1.44 (1.27, 1.63) | 13.4% | 12.2% | 1.14 (1.09, 1.19) |
| Add EHR | 20.0% | 16.1% | 1.39 (1.29, 1.49) | 14.1% | 10.6% | 1.44 (1.27, 1.63) | 13.4% | 12.2% | 1.13 (1.05, 1.22) |
| Add condition-specific volume | 19.5% | 15.7% | 1.38 (1.28, 1.48) | 12.6% | 10.6% | 1.25 (1.11, 1.41) | 11.5% | 12.3% | 0.91* (0.85, 0.99) |
| Add rural-urban code (RUCA) | 17.7% | 15.8% | 1.18 (1.09, 1.28) | 11.9% | 10.6% | 1.15* (1.00, 1.31) | 11.5% | 12.3% | 0.92* (0.87, 0.97) |
: p<0.05;
p<0.001 for all other comparisons.
AMI=acute myocardial infarction; CHF=congestive heart failure; CAH=Critical Access Hospital; EHR=electronic health record; RUCA=rural-urban commuting area.
We next built models that serially adjusted for variables that might be in the explanatory pathway to identify potentially actionable differences between CAHs and non-CAHs that contribute to outcomes. We found that differences in clinical personnel and resources into the model slightly attenuated the findings (Table 5); even after fully adjusting for all variables, including rurality, differences in mortality between CAHs and non-CAHs persisted for AMI (OR 1.18, 95% CI 1.09 to1.28, p<0.001) and for CHF (OR 1.15, 95% CI 1.00 to 1.31, p=0.04), but not pneumonia (OR 0.92, 95% CI 0.87 to 0.97, p=0.003).
When we limited our analyses to small, rural hospitals (81% of the CAHs and 11% of the non-CAHs), we found differences in resources (eTable 5a/b), quality of care, and outcomes between those with versus without the CAH designation. Although there were no significant differences in measured quality for AMI (HQA summary score 89.7 versus 90.3, p=0.59), CAHs had higher mortality than non-CAHs for this condition (OR 1.14 (1.05, 1.24), p=0.003). CAHs had lower performance on quality measures and higher mortality for CHF (HQA summary score 78.7 versus 84.8, p<0.001; OR for mortality 1.09 (1.03, 1.16), p=0.003), and lower performance on quality measures but identical mortality for pneumonia (HQA summary score 88.7 versus 91.1, p<0.001; OR for mortality 1.05 (0.99, 1.11), p=0.11, Table 6).
Table 6.
Quality of care and 30-day mortality, including only small, rural hospitals
| AMI | CHF | Pneumonia | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CAH | Non-CAH | Odds Ratio | CAH | Non-CAH | Odds Ratio | CAH | Non-CAH | Odds Ratio | |
| Number of patients | 7,809 | 8,200 | n/a | 40,044 | 35,594 | n/a | 66,605 | 46,270 | n/a |
| Number of hospitals | 908 | 357 | n/a | 1007 | 369 | n/a | 1018 | 369 | n/a |
| Quality of care: | |||||||||
| Number of hospitals reporting | 359 | 300 | n/a | 643 | 345 | n/a | 684 | 347 | n/a |
| Condition-specific HQA summary score (mean) | 89.7 | 90.3* | n/a | 78.7 | 84.8† | n/a | 88.7 | 91.1† | n/a |
| 30-day mortality: | |||||||||
| Raw mortality rates | 26.5% | 22.9% | 13.8% | 11.9% | 13.0% | 12.3% | |||
| Adjusted for age, sex, race, and medical comorbidities | 26.1% | 23.9% | 1.14† (1.05, 1.24) | 13.4% | 12.5% | 1.09† (1.03, 1.16) | 13.0% | 12.5% | 1.05* (0.99, 1.11) |
Small rural hospitals were classified as those with fewer than 100 beds, located in RUCA rural or RUCA small town areas.
: p>0.05;
p ≤0.003.
AMI=acute myocardial infarction; CHF=congestive heart failure; CAH=Critical Access Hospital; HQA=Hospital Quality Alliance.
In our sensitivity analysis, we found that unmeasured confounding was unlikely to explain our findings. For AMI, for example, if an unmeasured confounder tripled mortality risk (a much stronger predictor of mortality than any of our current comorbidities) and was three times more common in CAH patients than non-CAH patients, the odds ratio for mortality associated with receiving care at a CAH would decrease to 1.44, still statistically significant and clinically meaningful.
Discussion
Despite more than a decade of concerted policy efforts to improve rural healthcare, our findings suggest that substantial challenges remain. While CAHs provide much needed access to care for many of the nation’s rural citizens, we found that these hospitals, with their fewer clinical and technological resources, less often provided care consistent with standard quality metrics and generally had worse outcomes than non-CAHs. The absolute differences in outcomes were even larger than those reported in the initial work on this topic by Keeler et al., who demonstrated an excess all-cause mortality of 1.4% in rural hospitals using data from the 1980s,22 and comparable to differences noted by the Medicare Payment Advisory Committee (MedPAC) using data from 2003.2 These findings suggest that efforts to date have been insufficient in improving the quality of inpatient care in rural communities – and indicate a need for greater policy attention to the challenges these providers face.
The CAH designation, created with the goal of preserving access to care for Americans living in rural areas, directed financial resources to vulnerable rural hospitals at a time when many were closing due to financial insolvency. A number of regulations intended to promote quality were included in the legislation, including a formal requirement for credentialing and a state-run evaluations of quality. In return, designation as a CAH provided hospitals with financial security through cost-based reimbursement, which led to a significant improvement in these hospitals’ financial stability and allowed them to remain open, preserving access9, 24, 25 while maintaining patient satisfaction scores equal to or greater than non-CAHs.5 However, our findings suggest that these efforts have been inadequate in ensuring high quality care.
CAHs had significantly poorer performance on process measures, which may be due to fewer resources to devote to quality improvement. Because CAHs are not required to report HQA data,7 the CAHs that reported (which ranged from 39% of CAHs for AMI to 71% of CAHs for pneumonia) probably represent a higher-performing subset of CAHs than those choosing not to, likely understating the true differences in care. Further, CAHs have typically been exempt from pay-for-performance programs in the past, and will likely be excluded from national value-based purchasing efforts at least in the near-term.26–28 Engaging in the process of collecting and reporting data is an important step towards developing an internal quality improvement strategy;29 indeed, the Institute of Medicine has recommended that all CAHs participate in the HQA program for this reason.30
We found that personnel and clinical resources explained some of the mortality differences between CAHs and other hospitals. Assuring adequate personnel and resources is challenging for CAHs9, 25 given their difficulties in recruiting health care providers.25 Shorter lengths of stay, poor care transitions, or inadequate outpatient and home-based care31–33 may also contribute to poorer outcomes. Policy efforts to bring needed providers to underserved areas to ensure that CAHs have key clinical resources may be helpful. Given prior evidence that being a member of a hospital system may be related to improved clinical outcomes,34, 35 promoting partnerships with healthcare systems might be a useful strategy to help CAHs. Such partnerships could include onsite rotations by clinicians with specialty training, increased use of telemedicine, or formal referral and transfer agreements; arrangements that allow patients to remain close to home while still facilitating access to specialty care are likely to be particularly well-received by patients. One approach might be to provide financial incentives for tertiary care hospitals to partner with CAHs, potentially tying incentives to the CAH’s performance on quality metrics.
Although we did not find that the presence of an EHR explained a significant amount of the difference in clinical outcomes between CAHs and non-CAHs, this area warrants extra attention. The use of technology, particularly telemedicine and clinical data exchange, has important applications in underserved areas.36–39 CAHs lack financial capital and access to the personnel needed to install and effectively maintain these systems.40, 41 The federal effort to promote EHR adoption among CAHs has focused on technical assistance by the Regional Extension Centers (RECs).42 However, some RECs have elected not to work with CAHs and others are charging fees that may be unaffordable for CAHs. Policy makers may need to consider additional strategies to avoid exacerbating an already emerging digital divide.18
Adding rurality to our models seemed to explain some of the mortality differences we saw, and when we compared small, rural CAHs to small, rural non-CAHs, the excess mortality at CAHs was smaller. Our findings suggest that a substantial proportion of the barriers faced by CAHs are due to their size and their rural location, even after accounting for other factors such as clinical resources and personnel. Rurality is likely associated with other unmeasured factors such as travel distances to primary care or hospital, that impact outcomes; better understanding what factors are closely correlated with rurality that help explain these gaps in outcomes would be helpful in formulating effective interventions to help CAHs.
Despite the significant policy attention directed towards these vulnerable hospitals, there has been little empirical work on quality of care in a national sample of CAHs. Lutfiyya and colleagues examined performance on HQA process measures in 2004, the first year for which these data were available, and found that that CAHs had lower performance than non-CAHs.43 More recent comparisons have shown mixed results; some have found that rural hospitals provide lower quality care,44, 45 while others have failed to find a difference,46 although the study that found no difference examined self-selected hospitals engaged in national quality improvement programs.46 Using 2003 data, MedPAC found that, compared to other rural hospitals, CAHs had higher risk-adjusted mortality rates for CHF, AMI, pneumonia, stroke, and gastrointestinal hemorrhage; our findings extend the MedPAC work by focusing on a contemporary sample and a comparison group of non-rural hospitals, and by assessing care across a wide range of metrics while accounting for hospital characteristics and resources.2
Our study has limitations. We used administrative data, which fail to capture important clinical and patient characteristics (such as educational attainment) that likely affect outcomes. Based on our sensitivity analysis, however, we believe it is unlikely that any unmeasured confounder could be strong enough to fully account for the difference between CAH and non-CAH outcomes. We lacked data on the experience or qualifications of the clinicians caring for patients at CAHs, which could have potentially explained some of our findings. We were also unable to assess the role of patient choice in patterns of care; patients may have declined transfer for more advanced care due to personal preference even if clinicians recommended that a transfer occur. We could not examine outpatient care, and thus were unable to assess to what extent these differences might affect our findings. Because we relied on Medicare fee-for-service data for outcomes, we could not assess whether the patterns observed are also true for Medicare Advantage patients or for younger patients. Finally, mortality may be a crude measure of hospital quality, and therefore, we attempted to incorporate both structural and process measures to paint a more comprehensive view of care at CAHs.
Conclusions
Critical Access Hospitals play an essential role in ensuring access to health care for Americans living in rural areas. However, these institutions face many challenges, remain under-resourced both in terms of clinical and technological capabilities, perform worse on process measures, and have higher mortality rates than non-CAHs. More than a decade after major federal and state efforts to save America’s rural hospitals, these findings should be seen as a call to focus on helping these providers improve their care so that all Americans have access to high quality inpatient care regardless of where they live.
Supplementary Material
Acknowledgments
Dr. Joynt had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
We thank Jie Zheng, PhD, from the Department of Health Policy and Management, Harvard School of Public Health, for assistance with statistical programming. Dr. Zheng received compensation as part of regular employment.
Funding:
None.
Footnotes
The views expressed in this paper are those of the author and do not reflect the views of the Departments of Health and Human Services, Veterans Affairs, or other institutions with which the authors are affiliated.
Disclosures:
Dr. Joynt has no conflicts to declare. Dr. Harris has no conflicts to declare. Dr. Orav has no conflicts to declare. Dr. Jha has no relevant conflicts; he has provided consulting support to UpToDate and is on the Scientific Advisory Board for Humedica.
References
- 1.The Balanced Budget Act of 1997. HR 2015; 1997.
- 2.Medicare Payment Advisory Committee. Report to the Congress: Issues in a Modernized Medicare Program. Washington, D.C: MedPAC; 2005. [Google Scholar]
- 3.Stensland J, Davidson G, Moscovice I. The Financial Benefits of Critical Access Conversion: Working Paper 44. Minneapolis, MN: University of Minnesota Rural Health Research Center; 2004. [Google Scholar]
- 4.U.S. Census Bureau. Census 2000 Summary File Data. U.S. Census Bureau; 2000. [Google Scholar]
- 5.Casey MM, Davidson G. Upper Midwest Rural Health Research Center Final Report #10: Patient Assessments and Quality of Care in Rural Hospitals. Minneapolis, MN: Upper Midwest Rural Health Research Center, University of Minnesota; 2010. [Google Scholar]
- 6.The Joint Commission. 2010 ORYX Performance Measure Reporting Requirements for Hospitals and Guidelines for Measure Selections. Washington, D.C: The Joint Commission; 2009. [Google Scholar]
- 7.Casey M, Moscovice I Flex Monitoring Team. CAH Participation in Hospital Compare and Initial Results: Rural Health Research Centers at the Universities of Minnesota. North Carolina, and Southern Maine: Feb, 2006. [Google Scholar]
- 8.Gamm LD, Hutchison Linnae L, Dabney Betty J, Dorsey Alicia M, editors. Rural Healthy People 2010: A Companion Document to Healthy People 2010. Vol. 1. College Station, Texas: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. [Google Scholar]
- 9.Moscovice I, Rosenblatt R. Quality-of-care challenges for rural health. J Rural Health. 2000 Spring;16(2):168–176. doi: 10.1111/j.1748-0361.2000.tb00451.x. [DOI] [PubMed] [Google Scholar]
- 10.Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. Jama. 2008 May 14;299(18):2180–2187. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- 11.United States Department of Agriculture Economic Research Service. [Accessed November 1, 2010];Measuring Rurality: Rural-Urban Commuting Area Codes. http://www.ers.usda.gov/briefing/Rurality/RuralUrbanCommutingAreas/
- 12.Desai MM, Lin Z, Schreiner GC, et al. 2009 Measures Maintenance Technical Report: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk Standardized Readmission Measures. New Haven, CT: Yale-New Haven Health Services Corporation/Center for Outcomes Research and Evaluation (YNHHSC/CORE); 2009. [Google Scholar]
- 13.Krumholz HM, Normand SL, Galusha DH, et al. Risk-Adjustment Models for AMI and HF 30-Day Mortality. New Haven, CT: Yale University; 2005. [Google Scholar]
- 14.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why?: implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011 Jan 1;4(1):53–59. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Funk LM, Gawande AA, Semel ME, et al. Esophagectomy outcomes at low-volume hospitals: the association between systems characteristics and mortality. Ann Surg. 2011 May;253(5):912–917. doi: 10.1097/SLA.0b013e318213862f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009 Dec 31;361(27):2637–2645. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]
- 17.Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med. 2008 Oct 30;359(18):1921–1931. doi: 10.1056/NEJMsa0804116. [DOI] [PubMed] [Google Scholar]
- 18.Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009 Apr 16;360(16):1628–1638. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 19.Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals--the Hospital Quality Alliance program. N Engl J Med. 2005 Jul 21;353(3):265–274. doi: 10.1056/NEJMsa051249. [DOI] [PubMed] [Google Scholar]
- 20.Pope G, Kautter J, Ingber M, Freeman S, Sekar R, Newhart C. Evaluation of the CMS-HCC Risk Adjustment Model. Research Triangle Park, NC: RTI International, under contract from the Centers for Medicare and Medicaid Services; 2011. [Google Scholar]
- 21.Li P, Kim MM, Doshi JA. Comparison of the performance of the CMS Hierarchical Condition Category (CMS-HCC) risk adjuster with the Charlson and Elixhauser comorbidity measures in predicting mortality. BMC Health Serv Res. 2010;10:245. doi: 10.1186/1472-6963-10-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keeler EB, Rubenstein LV, Kahn KL, et al. Hospital characteristics and quality of care. Jama. 1992 Oct 7;268(13):1709–1714. [PubMed] [Google Scholar]
- 23.Pathman DE, Ricketts TC, 3rd, Konrad TR. How adults’ access to outpatient physician services relates to the local supply of primary care physicians in the rural southeast. Health Serv Res. 2006 Feb;41(1):79–102. doi: 10.1111/j.1475-6773.2005.00454.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Medicare Payment Advisory Committee. Report to the Congress: Medicare in Rural America. Washington, D.C: MedPAC; 2001. [Google Scholar]
- 25.Casey MM, Moscovice I. Quality improvement strategies and best practices in critical access hospitals. J Rural Health. 2004 Fall;20(4):327–334. doi: 10.1111/j.1748-0361.2004.tb00046.x. [DOI] [PubMed] [Google Scholar]
- 26.United States Senate. HR 3590: The Patient Protection and Affordable Care Act. 2009. [Google Scholar]
- 27.CMS Hospital Pay-for-Performance Workgroup. US Department of Health and Human Services, Medicare Hospital Value-Based Purchasing Plan Development, Issues Paper. Baltimore, MD: Centers for Medicare and Medicaid Services; 2007. [Google Scholar]
- 28.Federal Register; Department of Health and Human Services Centers for Medicare & Medicaid Services. 42 CFR Parts 422 and 480; Medicare Programs; Hospital Inpatient Value-Based Purchasing Program; Proposed Rule. 2010. [Google Scholar]
- 29.Jha AK, Orav EJ, Li Z, Epstein AM. The inverse relationship between mortality rates and performance in the Hospital Quality Alliance measures. Health Aff (Millwood) 2007 Jul-Aug;26(4):1104–1110. doi: 10.1377/hlthaff.26.4.1104. [DOI] [PubMed] [Google Scholar]
- 30.Institute of Medicine Committee on the Future of Rural Health Care, Quality Board on Health Care Services. Quality through collaboration: The future of rural health care. Washington DC: National Academies Press; 2005. [Google Scholar]
- 31.Sutton J. Patterns Of Post-Acute Utilization In Rural And Urban Communities: Home Health, Skilled Nursing, and Inpatient Medical Rehabilitation. Bethesda, MD: NORC Walsh Center for Rural Health Analysis; 2005. [Google Scholar]
- 32.Hartman L, Jarosek SL, Virnig BA, Durham S. Medicare-certified home health care: urban-rural differences in utilization. J Rural Health. 2007 Summer;23(3):254–257. doi: 10.1111/j.1748-0361.2007.00098.x. [DOI] [PubMed] [Google Scholar]
- 33.Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. 2006 Spring;22(2):140–146. doi: 10.1111/j.1748-0361.2006.00022.x. [DOI] [PubMed] [Google Scholar]
- 34.Hines S, Joshi MS. Variation in quality of care within health systems. Jt Comm J Qual Patient Saf. 2008 Jun;34(6):326–332. doi: 10.1016/s1553-7250(08)34041-0. [DOI] [PubMed] [Google Scholar]
- 35.Chukmaitov AS, Bazzoli GJ, Harless DW, Hurley RE, Devers KJ, Zhao M. Variations in inpatient mortality among hospitals in different system types, 1995 to 2000. Med Care. 2009 Apr;47(4):466–473. doi: 10.1097/MLR.0b013e31818dcdf0. [DOI] [PubMed] [Google Scholar]
- 36.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006 May 16;144(10):742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 37.McCambridge M, Jones K, Paxton H, Baker K, Sussman EJ, Etchason J. Association of health information technology and teleintensivist coverage with decreased mortality and ventilator use in critically ill patients. Arch Intern Med. 2010 Apr 12;170(7):648–653. doi: 10.1001/archinternmed.2010.74. [DOI] [PubMed] [Google Scholar]
- 38.Audebert HJ, Schultes K, Tietz V, et al. Long-term effects of specialized stroke care with telemedicine support in community hospitals on behalf of the Telemedical Project for Integrative Stroke Care (TEMPiS) Stroke. 2009 Mar;40(3):902–908. doi: 10.1161/STROKEAHA.108.529255. [DOI] [PubMed] [Google Scholar]
- 39.Shea S, Weinstock RS, Teresi JA, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009 Jul-Aug;16(4):446–456. doi: 10.1197/jamia.M3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bahensky JA, Ward MM, Nyarko K, Li P. HIT Implementation in Critical Access Hospitals: Extent of Implementation and Business Strategies Supporting IT Use. J Med Syst. 2009 Dec 2; doi: 10.1007/s10916-009-9397-z. [DOI] [PubMed] [Google Scholar]
- 41.Wakefield DS, Ward MM, Loes JL, O’Brien J. A network collaboration implementing technology to improve medication dispensing and administration in critical access hospitals. J Am Med Inform Assoc. 2010 Sep-Oct;17(5):584–587. doi: 10.1136/jamia.2010.004267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.The Office of the National Coordinator for Health Information Technology. [Accessed November 18, 2010];RECs Support Critical Access and Rural Hospitals. http://healthit.hhs.gov/portal/server.pt?open=512&mode=2&objID=3152.
- 43.Lutfiyya MN, Bhat DK, Gandhi SR, Nguyen C, Weidenbacher-Hoper VL, Lipsky MS. A comparison of quality of care indicators in urban acute care hospitals and rural critical access hospitals in the United States. Int J Qual Health Care. 2007 Jun;19(3):141–149. doi: 10.1093/intqhc/mzm010. [DOI] [PubMed] [Google Scholar]
- 44.Sheikh K, Bullock C. Urban-rural differences in the quality of care for medicare patients with acute myocardial infarction. Arch Intern Med. 2001 Mar 12;161(5):737–743. doi: 10.1001/archinte.161.5.737. [DOI] [PubMed] [Google Scholar]
- 45.Baldwin LM, MacLehose RF, Hart LG, Beaver SK, Every N, Chan L. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health. 2004 Spring;20(2):99–108. doi: 10.1111/j.1748-0361.2004.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 46.Ambardekar AV, Fonarow GC, Dai D, et al. Quality of care and in-hospital outcomes in patients with coronary heart disease in rural and urban hospitals (from Get With the Guidelines-Coronary Artery Disease Program) Am J Cardiol. 2010 Jan 15;105(2):139–143. doi: 10.1016/j.amjcard.2009.09.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


