Abstract
Background
There is controversy about how to treat vertebral fractures. Conservative care is the default approach. Radiofrequency kyphoplasty uses ultrahigh viscosity cement to restore spinal posture and stabilize the fracture. The aims of this study were to compare radiofrequency kyphoplasty to conservative care and assess the usual algorithm of starting all patients on conservative care for 6 weeks before offering surgery.
Methods
Elderly patients with painful osteoporotic vertebral compression fractures were all treated with 6 weeks of conservative care (analgesics, bracing, and physiotherapy). They were then offered the choice of continuing conservative care or crossing over to radiofrequency kyphoplasty, at 6 and 12 weeks. Clinical success was defined as: (1) VAS pain improvement ≥2, (2) final VAS pain ≤5, (3) no functional worsening on ODI.
Results
After the initial 6 weeks of conservative care, only 1 of 65 patients met the criteria for clinical success, and median VAS improvement was 0. After 12 weeks of conservative care, only 5 of 38 patients met the criteria for clinical success, and median VAS improvement was 1. At the 6-week follow-up after radiofrequency kyphoplasty, 31 of 33 surgery patients met the criteria for clinical success, and median VAS improvement was 5.
Conclusion
For the vast majority of patients with a VAS ≥5, conservative care did not provide meaningful clinical improvement. In contrast, nearly all patients who underwent radiofrequency kyphoplasty had rapid substantial improvement. Surgery was clearly much more effective than conservative care and should be offered to patients much sooner.
Keywords: Osteoporosis, Vertebral compression fractures, Kyphoplasty, Conservative treatment
Introduction
Controversy erupted in the medical literature and beyond after two randomized controlled trials concluded that vertebroplasty was no more effective than a sham procedure for treating vertebral compression fractures [1–10]. Meanwhile, patients in pain from vertebral fractures continue arriving to hospitals every day looking for relief. If vertebroplasty may not be as efficacious as previously believed, how effective are our other treatment options, and what should we be advising our patients? How much can conservative care help them? How promising are new forms of kyphoplasty? Do certain subgroups of patients benefit more or less than average from one or the other of these forms of treatments? Comparative effectiveness research [11–13] is the new paradigm for generating high-quality medical evidence. This study presents a comparative assessment of conservative care and radiofrequency kyphoplasty for osteoporotic vertebral compression fractures.
Radiofrequency kyphoplasty is a new form of surgical treatment. It injects an ultrahigh viscosity cement into the fractured vertebral body, using radiofrequency to achieve the proper consistency of the cement. This ultrahigh viscosity cement is designed to first restore proper height and alignment to the fractured vertebra and then to stabilize the fracture, thereby preventing further intravertebral motion and reducing pain. This is the first published clinical study on radiofrequency kyphoplasty.
The aim of this study is to provide scientific knowledge about the relative merits of conservative care and radiofrequency kyphoplasty for the treatment of vertebral compression fractures in a routine practice population. The study had several specific questions. (1) How beneficial is the initial 6 weeks of conservative treatment? (2) How beneficial is it to continue conservative care for an additional 6 weeks? (3) Which patients choose to cross over to surgical treatment? (4) How beneficial is radiofrequency kyphoplasty for vertebral compression fractures? (5) Do particular subgroups of patients benefit more or less from either conservative care or radiofrequency kyphoplasty? (6) How much does posture improve from conservative care or from radiofrequency kyphoplasty? The hope of this study was to provide new empirical evidence that could improve treatment decision-making for the medical condition of painful vertebral compression fractures.
Methods
Study design and patients
This is a prospective comparative effectiveness study. All patients of age 50 years and above who presented for osteoporotic vertebral compression fractures from mid-2009 to late 2010 were considered eligible for inclusion in this study. A VAS pain score ≥5 on a 10-point scale was required to be included. A total of 187 patients were screened, but only 67 could be included. Patients were excluded if they had tumor, infection, previous surgery at the fractured level, or current cortisone treatment. Two patients had a vertebra plana. All patients received a radiograph of the thoracic and lumbar spine as well as an MRI.
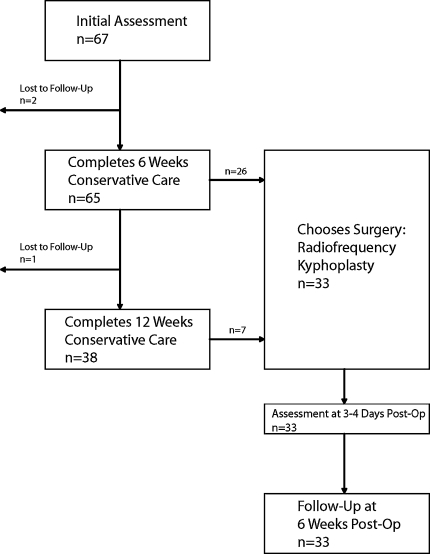
At initial presentation, all study patients were assessed clinically and radiographically and were started on conservative care. After 6 weeks of conservative care, patients were assessed again and offered the choice of either continuing conservative care or crossing over to surgical treatment. The choice was left up to the patient. Other treatment options were not offered. Patients who continued conservative care were assessed again in another 6 weeks and again offered the choice to cross over to surgery. Surgery was not offered later if not elected after 12 weeks of conservative care. Patients who opted for surgery were assessed clinically and radiographically at 3–4 days post-op and again at a follow-up visit 6 weeks post-operatively. The study design and patient flow are presented in Fig. 1.
Fig. 1.
Study design flowchart
Conservative care
Conservative care was tailored to the needs, wishes, and capabilities of each individual patient. It generally consisted of analgesic medication, bracing, and physiotherapy. For analgesic medication, patients were initially prescribed ibuprofen 400 mg 3×/d. If patients later requested further analgesia, they were either prescribed metamizole 500 mg 3×/d or sustained-release tramadol hydrochloride 100 mg 2×/d or referred to the hospital’s pain clinic, where they could receive percutaneous fentanyl. For bracing, the patients received the Spinomed III brace [Medi; Whitsett, NC, USA], which provides support yet can be worn comfortably under clothing. Physiotherapy was generally prescribed twice per week and consisted of massage and heat packs. Patients were advised to do normal walking as exercise, but to avoid weight lifting. Bed rest was not recommended.
Surgical treatment
Patients electing for surgery received radiofrequency kyphoplasty under general anesthesia on an inpatient basis at a university hospital. Radiofrequency kyphoplasty (StabiliT Vertebral Augmentation System; Dfine; San Jose, CA, USA) uses a minimally invasive unipedicular approach for unilateral access to the vertebral body and intermittent fluoroscopy for visualization. The system injects ultrahigh viscosity PMMA cement (ER2 Bone Cement; Dfine) into the vertebral cavity. The use of this ultrahigh viscosity bone cement is designed to first restore the height and alignment of the vertebral body and then stabilize the fracture, thereby reducing pain. Radiofrequency kyphoplasty has been described in further detail previously [15]. Post-operatively, patients also continued physiotherapy. Bracing was discontinued at surgery. Analgesics were reduced to an “as-needed” schedule, whereby most patients tapered off and discontinued.
Outcome measures
Pain was measured, with specific reference to the patient’s back, with a visual analog scale, consisting of a ruled 10-cm line, numbered 0–10, above a series of six round faces transitioning from a large smile to bawling tears. Functioning was measured with a German version of the ODI questionnaire, which provides an even-numbered score from 0 to 100.
Radiographic outcomes
Plain X-rays in the lateral position were taken at all study visits by the department of radiology. Central and anterior vertebral heights were measured. Kyphosis was measured as the angle of the endplates of the fractured vertebra. All patients were followed for 1 year to assess whether or not new fractures occurred.
Clinical success
Clinical success was a composite measure defined as meeting all three of the following criteria: (1) improvement of VAS ≥2 points, (2) final VAS ≤5, and (3) maintenance or improvement of ODI. This composite definition is the one used recently by the United States Food and Drug Administration for a trial on vertebroplasty [16]. It is somewhat more stringent than the use of the minimum clinically important difference for a single variable that has been used in other “level one” studies published in major journals [1, 2, 17, 18].
Statistical analysis
Quality control was performed on the database to check for missing, improbable, or inconsistent entries. Descriptive statistics were used to characterize the patient sample and outcomes. Wilcoxon matched-pairs signed-ranks tests were used to test the statistical significance of differences in VAS or ODI scores from baseline (or pre-op) to follow-up. Forward stepwise linear regression analysis was used to determine which types of patients benefited more or less from conservative care or surgery, in terms of the change in VAS or ODI. Logistic regression analysis was used to determine if certain types of patients were more or less likely to elect for surgery, or more or less likely to meet the criteria for clinical success. The regression analyses explored the following variables as possible predictors: patient number (in chronological order), sex, age, number of spinal levels treated, use of osteoporotic medication (Y/N), symptom duration until initial presentation (weeks), and symptom duration until surgery (weeks).
Results
Patient sample
There were 67 patients, of whom 35 (52%) were female. The median (range) age was 65 years (52–92). There were 44 single-level, 14 two-level, 8 three-level, and 1 four-level patients, and thus a total of 100 fractured vertebrae (Table 1). The median (range) duration of symptoms at the time of initial presentation was 5 (1–8) weeks.
Table 1.
Distributions of the 100 fractures across the spinal levels
| Level | n |
|---|---|
| T5 | 1 |
| T6 | 0 |
| T7 | 0 |
| T8 | 5 |
| T9 | 11 |
| T10 | 5 |
| T11 | 7 |
| T12 | 13 |
| L1 | 13 |
| L2 | 12 |
| L3 | 13 |
| L4 | 12 |
| L5 | 8 |
Clinical outcomes of the initial 6 weeks of conservative care
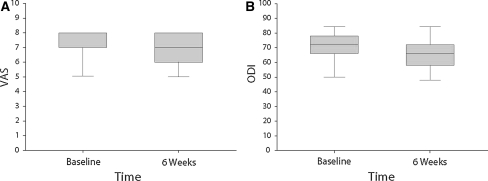
The patients had a high level of pain at baseline, showing little improvement by 6 weeks (Fig. 2a). The difference in scores from baseline to 6 weeks was statistically significant, but the actual magnitude of difference was generally not clinically relevant. The median (range) improvement in VAS score was 0 (−1 to 2) points. There were 40 patients who had no change in VAS score, 24 who showed improvement, and 1 patient who worsened.
Fig. 2.
Clinical outcomes for the initial 6 weeks of conservative care. The box and whisker plots show the distribution of data for VAS pain and ODI functioning scores. a VAS pain. At baseline, the median, 75th quartile, and maximum score were all 8. At 6 weeks, the 75th quartile and maximum were both 8. The difference in scores between baseline and 6 weeks was statistically significant (p < 0.001). b ODI functioning. The difference in scores between baseline and 6 weeks was statistically significant (p < 0.001)
The patients experienced a high level of disability, which showed little improvement by 6 weeks (Fig. 2b). Again, the difference in scores from baseline to 6 weeks was statistically significant, but generally not clinically relevant. The median (range) improvement of ODI score was 6 (−10 to 24) points.
After 6 weeks of conservative care, there was only 1 of 65 patients who met the criteria for clinical success. In the regression analyses, none of the explored variables was a significant predictor of change in VAS or ODI, or meeting the criteria of success.
Clinical outcomes of continuing conservative care for another 6 weeks
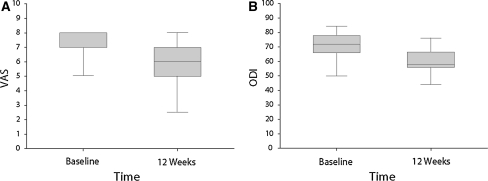
There were 38 patients who continued conservative care for a total of 12 weeks from the initial presentation (Fig. 1). The patients had a high level of pain at baseline, with only a small proportion of patients showing substantial improvement by 12 weeks (Fig. 3a). The difference in scores from baseline to 12 weeks was statistically significant, but the actual magnitude of difference was clinically marginal. The median (range) improvement of VAS score was 1 (−1 to 5.5) points. There were 29 patients who showed improvement of VAS score, 8 who showed no change, and 1 who worsened.
Fig. 3.
Clinical outcomes for 12 weeks of conservative care. The box and whisker plots show the distribution of data for VAS pain and ODI functioning scores. a VAS pain. At baseline, the median, 75th quartile, and maximum score were all 8. The difference in scores between baseline and 12 weeks was statistically significant (p < 0.001). b ODI functioning. The difference in scores between baseline and 12 weeks was statistically significant (p < 0.001)
The patients experienced a high level of disability at the initial presentation, which showed a very minor improvement for most of the sample by 12 weeks (Fig. 3b). Again, the difference in scores from baseline to 12 weeks was statistically significant, but clinically marginal. The median (range) improvement of ODI score was 8 (−8 to 22) points.
Among the 38 patients who continued conservative care for 12 weeks, only 5 met the criteria for clinical success. In the regression analyses, none of the explored variables were a significant predictor of change in VAS or ODI or being clinically successful.
Patient choice to crossover to surgery
There were 33 patients (49%) who crossed over to surgery (26 at 6 weeks and 7 at 12 weeks; Fig. 1). Logistic regression analysis showed that the more fractured levels the patients had, the more likely they were to cross over to surgery (OR = 3.27, 95% CI of OR = 1.40–7.64, p = 0.006). Compared to patients under the age of 65 years, patients of age 65–74 years were more likely to undergo surgery (OR = 3.82, 95% CI of OR = 1.02–14.32, p = 0.047), while patients 75 years and older did not differ significantly from patients under age 65 years. No other variable tested (sex, VAS, ODI, osteoporosis medication, symptom duration) was a significant predictor of the crossover to surgery. Nonetheless, number of levels and age accounted for only a small amount of the decision to cross over to surgery (pseudo-R2 = 0.19).
Clinical outcomes of radiofrequency kyphoplasty
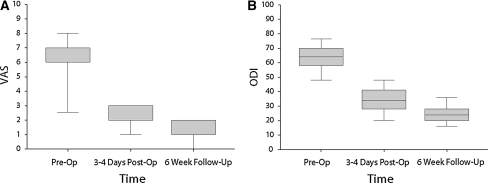
The patients had a high level of pain at pre-op, which showed a dramatic improvement for virtually the entire sample by 3–4 days post-op and further minor improvement by the 6-week follow-up (Fig. 4a). The difference in scores from pre-op to 6 weeks was statistically significant and clinically relevant. The median (range) improvement in VAS pain at 6 weeks post-op was 5 (1–7) points. All 33 surgery patients had an improvement of VAS scores; none remained the same or worsened.
Fig. 4.
Clinical outcomes for surgical treatment with radiofrequency kyphoplasty. The box and whisker plots show the distribution of data for VAS pain and ODI functioning scores. a VAS pain. At pre-op, the median and 75th quartile were both 7. At 3–4 days post-op, the 25th quartile and the median were both 2; the 75th quartile and maximum were both 3. At the 6-week follow-up, the minimum was 0; the 25th quartile and the median were both 1; the 75th quartile and maximum were both 2. The difference in scores between pre-op and 6 weeks was statistically significant (p < 0.001). b ODI functioning. The difference in scores between pre-op and 6 weeks was statistically significant (p < 0.001)
The patients experienced a high level of disability at pre-op, which showed substantial improvement for the entire sample by 3–4 days post-op and further minor gains by the 6-week follow-up (Fig. 4b). Again, the difference in scores from pre-op to 6 weeks was statistically significant and clinically relevant. The median (range) improvement in ODI functioning at 6 weeks post-op was 38 (22–56) points.
By the 6-week follow-up, 31 of 33 surgery patients met the criteria for clinical success. In the regression analysis, the only variable that significantly predicted the change in VAS pain score from pre-op to 6-week follow-up was whether the patient had surgery after 6 or 12 weeks of conservative care (coeff. = 1.83, F = 15.4, p < 0.001, R2 = 0.332). Patients who had surgery after only 6 weeks of conservative care had significantly more improvement in VAS pain than patients who had surgery after 12 weeks (median VAS improvement: 5.5 vs. 4, p = 0.007, according to Mann–Whitney rank sum test). None of the explored variables was a significant predictor of ODI or clinical success.
Radiographic outcomes
During the initial 6 weeks of conservative care, most vertebrae lost anterior and central height and had an increase of kyphosis (Table 2). Among the patients who completed 12 weeks of conservative care, all vertebrae lost anterior and central height and had increased kyphosis (Table 3). Among the vertebrae treated with RFK, none lost anterior height, central height remained the same on average, and kyphosis was reduced in the majority of patients (Table 4). Cement leakage was seen on post-operative plain X-rays in 3 of 56 levels operated. New fractures occurred in seven patients in the total sample, of whom five had received only conservative care and two had also received surgery.
Table 2.
Radiographic outcomes from the initial 6 weeks of conservative care for the entire sample
| Anterior vertebral height | Central vertebral height | Kyphosis | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 weeks | Change | Baseline | 6 weeks | Change | Baseline | 6 weeks | Change | |
| Max | 28 | 26 | 0 | 26 | 25 | 0 | 16 | 18 | 6 |
| Median | 24 | 22 | −2 | 24 | 22 | −2 | 12 | 15 | 3 |
| Min | 18 | 16 | −6 | 19 | 18 | −4 | 8 | 1 | −11 |
The table shows the results for anterior vertebral height (in mm), central vertebral height (in mm), and kyphosis (in °) for all 100 vertebrae in this study. The rows present the maximum, median, and minimum scores to show the distribution of the data. Each individual vertebra’s change from baseline to 6 weeks was calculated; the “change” columns are the maximum, median, and minimum of these changes (not the change of the maximum, median, and minimum)
Table 3.
Radiographic outcomes from 12 weeks of conservative care
| Anterior vertebral height | Central vertebral height | Kyphosis | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 12 weeks | Change | Baseline | 12 weeks | Change | Baseline | 12 weeks | Change | |
| Max | 27 | 25 | −1 | 26 | 23 | −1 | 16 | 20 | 7 |
| Median | 23 | 19 | −3 | 24 | 20 | −3 | 12 | 16 | 4 |
| Min | 19 | 16 | −7 | 19 | 17 | −5 | 8 | 13 | 1 |
The table shows the results for anterior vertebral height (in mm), central vertebral height (in mm), and kyphosis (in °) for the 54 vertebrae in the 38 patients who completed 12 weeks of conservative care. The rows present the maximum, median, and minimum scores to show the distribution of the data. Each individual vertebrae’s change from baseline to 12 weeks was calculated
Table 4.
Radiographic outcomes from surgery
| Anterior vertebral height | Central vertebral height | Kyphosis | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op 6 weeks | Change | Pre-op | Post-op 6 weeks | Change | Pre-op | Post-op 6 weeks | Change | |
| Max | 25 | 26 | 2 | 25 | 26 | 3 | 19 | 18 | 0 |
| Median | 22 | 22 | 0 | 21 | 22 | 0 | 15 | 14 | −1 |
| Min | 16 | 16 | 0 | 18 | 18 | −2 | 10 | 9 | −3 |
The table shows the results for anterior vertebral height (in mm), central vertebral height (in mm), and kyphosis (in °) for the 56 vertebrae in the 33 patients who underwent surgery. The rows present the maximum, median, and minimum scores to show the distribution of the data. Each individual vertebra’s change from pre-op to post-op 6 weeks was calculated
Discussion
Vertebral compression fractures are a very painful and debilitating condition, occurring mainly among the elderly. There has been widespread controversy about the effectiveness of vertebroplasty in the wake of two randomized controlled trials concluding that it was no better than placebo [1–10]. While scientific discussion is interesting, the vertebroplasty debate has not yet led to much constructive guidance on how to better treat these patients. Meanwhile, elderly patients continue to arrive at the hospital in pain, seeking relief. The two main alternatives to vertebroplasty are either traditional conservative care or some new form of kyphoplasty. The recent AAOS treatment guidelines are inconclusive on conservative care and provide a recommendation for balloon kyphoplasty [14]. In contrast to the existing evidence, real-world practice generally insists that all vertebral fracture patients first receive at least 6 weeks of conservative care, and many patients only receive conservative care or no treatment at all.
The aim of this study was not simply to compare conservative care to kyphoplasty. Rather, the aim was to assess whether the current treatment algorithm (6 weeks of conservative care for all patients, followed by the choice of continuing conservative care or have surgery, left entirely to the patient’s preferences) can somehow be better optimized. According to this study, the initial 6 weeks of conservative treatment is virtually useless. Only 1 in 65 patients met the criteria for clinical success after 6 weeks of conservative care. Incidentally, the one “successful” patient nonetheless opted for surgery right after those 6 weeks. On average, the other patients experienced no benefit, with the median change of VAS pain score being zero and the median improvement of ODI score (6 points) being below the minimum important difference. Thus, any patient who pursues conservative care can expect to experience about the same level of pain and disability unchanged for at least 6 weeks.
Continuing conservative care for a total of 3 months may help some patients, but remains an unlikely gamble. In this study, there were only 5 of 38 (13%) patients who met the criteria for clinical success after 12 weeks of conservative care. Despite very substantial improvement, two of these five patients nonetheless opted for surgery after 12 weeks of conservative care and both obtained some further minor alleviation. Given the low success rate for conservative care, it really should only be administered to patients with a strong preference.
Of 33 patients, 31 receiving radiofrequency kyphoplasty met the criteria for clinical success, and the other 2 showed clinical improvement. The median improvement of VAS pain was 5 points, and the median improvement of ODI functioning was 38 points.
Conservative care almost always led to a further loss of vertebral height and increasing kyphosis (Tables 2, 3). Radiofrequency kyphoplasty generally prevented further loss of vertebral height and made minor improvements in kyphosis (Table 4).
This study could not shed much light on the question which patients chose to cross over to surgical treatment. Multilevel patients and patients of age 65–75 years were more likely to undergo surgery, but these factors did not account for much of the data variance. So crossover to surgery seems based mainly on patient preferences or unknown factors.
Furthermore, this study was unable to find any patient or baseline medical characteristics that have prognostic value if particular subgroups of patients benefit more or less from either conservative care or radiofrequency kyphoplasty. Statistically, it became unlikely to find any such prognostic factors, because there were almost no surgery patients who were not clinically successful and so few patients who benefited from conservative care. In sum, there is almost a night-and-day difference between conservative care and radiofrequency kyphoplasty in the treatment of vertebral compression fractures in our patient population. Given these results, as well as past literature [14, 17, 18], it is difficult to grasp why patients endure 6 weeks of pain and ineffective conservative care before being offered the option of quick and effective surgical treatment. With such a stark difference in outcomes, it is also unclear why about half the vertebral compression fracture patients never opt for surgery. They may be poorly informed about the likely difference in clinical outcomes or may harbor excessive worries about having an operation. Further research is needed on these patient factors, to improve patient counseling.
Acknowledgments
We would like to thank Ayçe Atalay, MD, and Adela Castelló MPH, MSc, (both from Mercury Medical Research & Writing) for contributing to database quality control (AA) and statistical analysis (AA and AC).
Conflict of interest
None.
References
- 1.Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. NEJM. 2009;361:557–568. doi: 10.1056/NEJMoa0900429. [DOI] [PubMed] [Google Scholar]
- 2.Kalmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. NEJM. 2009;361:569–579. doi: 10.1056/NEJMoa0900563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinstein JN. Balancing science and informed choice in decisions about vertebroplasty. NEJM. 2009;361:619–621. doi: 10.1056/NEJMe0905889. [DOI] [PubMed] [Google Scholar]
- 4.Aebi M. Vertebroplasty: about sense and nonsense of uncontrolled “controlled randomized prospective trials”. Eur Spine J. 2009;18:1247–1248. doi: 10.1007/s00586-009-1164-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noonan P. Randomized vertebroplasty trials: bad news or sham news? Am J Neuroradiol. 2009;30:1808–1809. doi: 10.3174/ajnr.A1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalmes D, Buchbinder R, Jarvik J, Heagerty P, Comstock B, Turner J, Osborne R. Response to “randomized vertebroplasty trials: bad news or sham news?”. Am J Neuroradiol. 2009;30:1809–1810. doi: 10.3174/ajnr.A1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buchbinder R, Osborne RH, Kallmes D. Vertebroplasty appears no better than placebo for painful osteoporotic spinal fractures, and has potential to cause harm. MJA. 2009;191:476–477. doi: 10.5694/j.1326-5377.2010.tb03467.x. [DOI] [PubMed] [Google Scholar]
- 8.Clark WA, Diamond TH, McNeil HP, Gonski PN, Schlaphoff GP, Rouse JC. Vertebroplasty for painful acute osteoporotic vertebral fractures: recent Medical Journal of Australia editorial is not relevant to the patient group that we treat with vertebroplasty. MJA. 2010;192:334–337. doi: 10.5694/j.1326-5377.2010.tb03533.x. [DOI] [PubMed] [Google Scholar]
- 9.Buchbinder R, Osborne RH, Kallmes D. Invited editorial presents an accurate summary of the results of two randomized placebo-controlled trials of vertebroplasty. MJA. 2010;192:338–341. doi: 10.5694/j.1326-5377.2010.tb03534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weyden MB. Vertebroplasty, evidence and professional protest. MJA. 2010;192:301–302. doi: 10.5694/j.1326-5377.2010.tb03526.x. [DOI] [PubMed] [Google Scholar]
- 11.Sox HC, Greenfield S. Comparative effectiveness research: a report from the Institute of Medicine. Ann Intern Med. 2009;151:203–205. doi: 10.7326/0003-4819-151-3-200908040-00125. [DOI] [PubMed] [Google Scholar]
- 12.Luce BR, Kramer JM, Goodman SN, Connor JT, Tunis S, Whicher D, Schwartz JS. Rethinking randomized clinical trials for comparative effectiveness research: the need for transformational change. Ann Intern Med. 2009;151:206–209. doi: 10.7326/0003-4819-151-3-200908040-00126. [DOI] [PubMed] [Google Scholar]
- 13.Schneeweiss S. On guidelines for comparative effectiveness research using nonrandomized studies in secondary data sources. Value Health. 2009;12:1041. doi: 10.1111/j.1524-4733.2009.00607.x. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Orthopedic Surgeons. The Treatment of Symptomatic Osteoporotic Spinal Compression Fractures: Guideline and Evidence Report. Accessed on 16 December 2010 at: http://www.aaos.org/Research/guidelines/SCFguideline.pdf
- 15.Elgeti FA, Marnitz T, Kröncke TJ, Gebauer B. DFine Radiofrequenzkyphoplastie (RFK)—Kyphoplastie mit ultrahochviskösem Zement. RöFo. 2010;182:803–805. doi: 10.1055/s-0029-1245385. [DOI] [PubMed] [Google Scholar]
- 16.Bae HW, Linovitz R, Maurer P, et al. Correlation of early pain and long-term functional results from a multi-center, prospective, randomized, controlled FDA-IDE vertebroplasty trial. Spine J. 2010;10:64S–65S. doi: 10.1016/j.spinee.2010.07.175. [DOI] [Google Scholar]
- 17.Klazen CAH, Lohle PNM, Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376:1031–1033. doi: 10.1016/S0140-6736(10)61162-2. [DOI] [PubMed] [Google Scholar]
- 18.Wardlaw D, Cummings SR, Meirhaeghe J, Bastian L, Tillman JB, Ranstam J, Eastell R, Shabe P, Talmadge K, Boonen S. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373:1016–1024. doi: 10.1016/S0140-6736(09)60010-6. [DOI] [PubMed] [Google Scholar]