Abstract
Purpose
U-shaped sacral fractures usually result from axial loading of the spine with simultaneous sacral pivoting due to a horizontal fracture which leads to a highly unstable spino-pelvic dissociation. Due to the rarity of these fractures, there is lack of an agreed treatment strategy.
Methods
A thorough literature search was carried out to identify current treatment concepts. The studies were analysed for mechanism of injury, diagnostic imaging, associated injuries, type of surgery, follow-up times, complications, neurological, clinical and radiological outcome.
Results
Sixty-three cases were found in 12 articles. No Class I, II or III evidence was found in the literature. The most common mechanism of injury was a fall or jump from height. Pre-operative neurological deficit was noted in 50 (94.3%) out of 53 cases (not available in 10 patients). The most used surgical options were spino-pelvic fixation with or without decompression and ilio-sacral screws. Post-operative complications occurred in 24 (38.1%) patients. Average follow-up time was 18.6 months (range 2–34 months). Full neurological recovery was noted in 20 cases, partial recovery in 14 and 9 patients had no neurological recovery (5 patients were lost in follow-up). Fracture healing was mentioned in 7 articles with only 1 case of fracture reduction loss.
Conclusion
From the current available data, an evidence based treatment strategy regarding outcome, neurological recovery or fracture healing could not be identified. Limited access and minimal-invasive surgery focussing on sacral reduction and restoration seems to offer comparable results to large spino-pelvic constructs with fewer complications and should be considered as the method of choice. If the fracture is highly unstable and displaced, spino-pelvic fixation might offer better stability.
Keywords: U-shaped fracture, Sacrum, Roy-Camille, Treatment strategy, Systematic review
Introduction
U-shaped sacral fractures usually occur in multiply injured patients after a jump or fall from height [9]. However, these fractures are rare and often missed or under-diagnosed primarily because of the nature and severity of other injuries. Secondly, obtaining adequate imaging is difficult [14]. Nonetheless, the rate of associated neurological deficit or other major injuries with U-shaped sacral fractures is very high.
U-shaped fractures normally have two major biomechanical components. First of all, severe spinal axial loading results in a vertical, bilateral and transforaminal fracture (between the alae and sacral segments). Due to vertical instability and high-energy transfer, the sacrum is forced into a rotational movement. An additional horizontal fracture, normally between S1 and S2, is the result, causing complete instability and disruption of the posterior integrity due to sacral pivoting while the posterior pelvic ring itself stays intact with no contact to the spine. The rostral part of the sacrum stays attached to the lumbar spine while the caudal part stays in the posterior pelvic ring (Fig. 1). This so called spino-pelvic dissociation is the reason for the high rate of associated neurological injuries in U-shaped sacral fractures ranging from incomplete radiculopathy to complete cauda equina syndrome and ruptured nerve roots [3, 5, 6, 9, 11, 12].
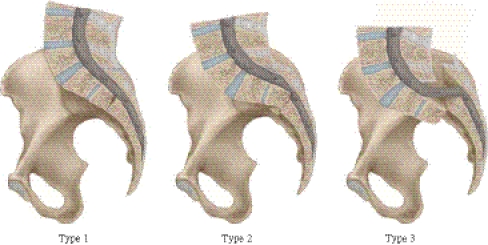
Fig. 1.
Illustration of fracture mechanism in Roy-Camille Type 1–3
Roy-Camille [22] first described the injury pattern of U-shaped sacral fractures in 1984. Based on the relative position of the cephalad component to the rostral fragment, U shaped sacral fractures are classified into three types. Type 1 is a flexion fracture where the upper fragment dislocates anteriorly. Type 2 is also a flexion fracture, but the upper fragment displaces posteriorly and becomes almost horizontal on the lower fragment. Type 3 is an extension fracture where the upper fragment is vertical and displaced antero-inferiorly in front of the lower fragment. Strange-Vognsen and Lebech [29] described a special type, where the upper fracture part is not displaced (despite the U-shaped fracture pattern) but is still massively impacted.
Due to relatively low incidence of U-shaped sacral fractures, the majority of spinal and orthopaedic surgeons have limited experience of diagnosing and treating these fractures [11, 27].
The purpose of this study was primarily to explore literature about the current management strategies of U-shaped sacral fractures. Where mentioned, we also looked for associated neurological injuries, complications of surgery and long-term outcomes.
Methods
A thorough literature search was performed using Medline via Pub Med and Ovid Online for articles published on U-shaped sacral fractures. The search was limited to the English, German and French language articles only. The keywords used included isolated, sacral fractures, U-shaped, spino-pelvic dissociation, management and outcome. Papers in which U-shaped sacral fractures were mentioned only to describe a specific type of sacral fractures as well as sacral insufficiency fractures and tumour cases were excluded. Only those papers where the management of at least one case was mentioned were included. Additional papers were extracted from the references of the papers found in the literature search.
The studies were analysed for number of patients, mechanism of injury, associated injuries, neurological deficits, treatment modalities, complications of surgery (where applicable), follow-up time and outcomes.
Results
Twelve papers were identified and included in this review. Published papers with combined injuries of the pelvic ring were included. No studies fulfilling level I, II or III criteria for evidence were found in English, German and French literature. A summary of the included studies is given in Table 1.
Table 1.
Study types, mechanism of injury and imaging
| Study number | Study type/(number of cases) | Authors | Male: female | Mean age (range) | Mechanism of Injury | Associated injuries | Diagnostic imaging | Further imaging |
|---|---|---|---|---|---|---|---|---|
| 1 | Case report (1) | Rhee WT et al. [21] | 1:0 | 26 | CI = 1 | Yes | CT | MRI |
| 2 | Case report (2) | Hussin P et al. [13] | 1:1 | 18 (8–28) | AF = 1, CI = 1 | Yes | X-ray | CT |
| 3 | Case report (1) | Vilela MD [32] | 1:0 | 23 | RTA = 1 | Yes | X-ray | CT |
| 4 | Case report (1) | Vilela MD [33] | 1:0 | 37 | GS = 1 | Yes | CT | X-ray |
| 5 | Clinical series (4) | Hunt N et al. [14]. | 2:2 | 30 (23–36) | SA = 3, RTA = 1 | Yes | X-ray | CT |
| 6 | Clinical series (3) | Mouhsine E et al. [19] | 3:0 | 31 (22–41) | SA = 2, CI = 1 | Yes | CT | X-ray |
| 7 | Retrospective clinical study (13) | Nork SE et al. [20] | 11:2 | 31 (21–60) | AF = 4, SA = 3, IA = 2, RTA = 4 | Yes | X-ray | CT |
| 8 | Retrospective QoL study (8) | Gribnau AJ et al. [11] | 3:5 | 29 (19–55) | SA = 7, AF = 1 | Yes | X-ray | CT |
| 9 | Retrospective clinical study (19) | Schildhauer TA et al. [28] | 11:8 | 33 (15–35) | AF = 10, RTA = 7, CI = 2 | Yes | X-ray | CT |
| 10 | Retrospective clinical study (5) | Taguchi T et al. [30] | 1:5 | 34 (17–51) | SA = 5 | N/M | X-ray | CT |
| 11 | Clinical series (3) | Sabourin M et al. [14] | 2:1 | 39 (24–61) | SA = 2, AF = 1 | Yes | X-ray | CT |
| 12 | Clinical series (3) | König MA et al. [17] | 0:3 | 22 (18–30) | AF = 1, RTA = 1, SA = 1 | Yes | CT | X-ray |
SA suicidal attempt, AF accidental fall, RTA road traffic accident, CI crush injuries GS gunshot injury, QoL quality of life, N/M not mentioned
Four case reports were found describing U-shaped fractures and their surgical treatment [13, 21, 32, 33] as well as four case series [14, 17, 19, 24]. All in all, four retrospective studies were found in the literature and included into this review [11, 20, 28, 30].
In total, 63 cases of U-shaped sacral fractures were identified (average = 5.25 per study; range 1–19 per study). The age range in the studies was 8–60 years (average = 29.4) with 37 male and 26 female patients (Table 1).
Mechanism of Injury
The most common mechanism of injury was suicidal jump (23), followed by fall from height (18). These two injury patterns are responsible for the majority (67.2%) of all published cases. Road traffic accidents (14) are the third most common cause followed by crush injuries (5), industrial injuries (2) and one gunshot injury.
Pre-operative imaging
X-ray imaging was the first radiological tool in nine papers whereas four authors used CT scan as primary imaging. Additional imaging was reciprocal in all studies except one where an MRI scan was performed after a CT scan [21].
Associated injuries
Associated injuries were noted in 61 patients (96.8%). Due to the occurrence of U-shaped fractures in patients with multiple injuries, one or more than one type of injury might have been noted in each case. These injuries included additional pelvic ring fractures 28 (44.4%), or isolated acetabular fractures 4 (6.6%). Half of all patients, therefore, had pelvic involvement. Additional spinal injuries were reported in 20 (31.7%) patients; 3 (4.8%) spinal cord injuries occurred. Skull or brain injuries appeared in 7 (11.5%) of the cases. The chest cavity was injured 12 times (19.7%), whereas abdominal injuries were mentioned 10 times (16.4%). Life-threatening injuries for both cavities like bilateral pneumothorax, liver or bladder rupture were reported. The lower extremity was affected in 20 cases (31.7%) in which bilateral or single-sided calcaneal fractures were most commonly reported (13 cases). Rare associated injuries included femoral or pilon tibiale fractures (5), Lisfranc fracture luxation (1) or sub-total leg amputation (1). Four (6.3%) patients had upper limb fracture involvement with mainly radial fractures.
Neurological assessment
Pre-operative neurological examination was reported in 53 (84.1%) patients. In the remaining 10 patients, initial neurological examination was not possible or not mentioned because of sedation and mechanical ventilation at the time of assessment in 2 cases, or due to severity of injuries in 8 cases (Table 2).
Table 2.
Neurological findings, surgical procedures and outcome
| Study number | Mean time from admission to surgery (d) | Pre-op neurology | Type of surgery | Mean follow-up time (month) | Neurological recovery | Radiological healing/loss of reduction | Complications |
|---|---|---|---|---|---|---|---|
| 1 | 21 | AB = 1 | SP = 1 | N/M | N/M | N/M | N/M |
| 2 | 3 | AB = 2 | Open reduction, laminectomy, immobilisation | 2 | CR = 2 | N/M | None |
| 3 | N/M | AB = 1 | SP + decomp = 1 | 12 | PR = 1 | No loss of reduction | N/M |
| 4 | 19 | AB = 1 | SP + decomp = 1 | 24 | NR = 1 | Healing confirmed | N/M |
| 5 | N/M | N = 2, AB = 2 |
SP = 1, TAO = 1, IS = 2 | 5 | N = 2, PR = 1, NR = 1 |
N/M | N/M |
| 6 | 9 | AB = 3 | Modified TAO = 3 | 11 | N/M | Healing confirmed | Screw insertion pain |
| 7 | 4 | N/A = 2, N = 2, AB = 9 |
IS = 13 | 14 | N = 2, aCR = 9, PR = 1, NR = 1 |
Healing confirmed | Disengagement of IS = 1 |
| 8 | 7 | N/A = 7, AB = 1 |
TAO ± Plate = 5, IS = 2, TSP = 1 |
29 | NR = 1, bPR = 7 |
No loss of reduction in all patients | Wound infection = 3 Persistent pain with metal work removal = 3 |
| 9 | N/M | AB = 19 | SP + decomp = 19 | 31 | CR = 10, PR = 5, NR = 3, 1 lost FU |
Healing confirmed | Wound infection = 5, decubitus ulcer = 1, IS loosening = 3, Metal work removal = 2 |
| 10 | N/M | N = 1, AB = 4 |
IS + Plate = 4, IS = 1 | N/M | N = 1, PR = 4 |
Healing confirmed | N/M |
| 11 | N/M | AB = 3 | SSP = 3 | 34 | CR = 1, PR = 1, NR = 1 |
N/M | Superficial wound infection = 1 |
| 12 | 6 | N/A = 1, AB = 2 |
IS = 3 | 24 |
cCR = 1, PR = 1, NR = 1 |
Healing confirmed = 2 Loss of reduction = 1 |
Loss of reduction |
AB abnormal, N normal, N/M not mentioned, N/A not available, SP spino-pelvic fixation, decomp decompression, IS ilio-sacral screws, TAO triangular osteosynthesis, TSP transsacral plate, SSP sacro-sacral plate, CR complete recovery, NR no recovery, PR partial recovery, mo months
aTwo patients had no pre-op assessment but no neurological deficit was seen at follow-up
bThe pre-op neurological assessment was not possible in 7 cases in this study. Immediate post-op neurology was abnormal in all eight patients
cPre-op neurological assessment was not possible but no neurological deficit was seen at follow-up
Where the neurological examination was performed, 3 (5.7%) patients had normal neurology and 50 (94.3%) had abnormal pre-operative neurology. The neurological deficits included bowel or bladder dysfunction in 22, motor weakness in 15 and paraesthesia in 5 cases. In five studies, Gibbons [9] classification of cauda equina impingement was used for neurological assessment. Interestingly, no case report used this classification. Two studies (27 cases) reported immediate post-op Gibbons scores.
Surgical technique
Surgical techniques can be divided into two main criteria regarding the fixation of U-shaped fractures. One is fixation of the fracture elements in open procedures. The other one is limited access or minimally-invasive surgery for restoration of the sacrum only. The overview of the different surgical strategies in different papers is given in Table 2.
Open Techniques
Open techniques normally involve multi-segmental fusion of the lumbar spine to the pelvis, sacrificing lumbar flexibility for fracture reduction and fixation.
The so-called spino-pelvic fixation, where the lumbar spine is fixed to the pelvis (vertebropelvic fixation) with pedicle screws and ilio-sacral screws, was the method of choice in 23 (36.5%) patients combined with decompression of the nerve roots in 20 cases [14, 21, 28, 32, 33]. Ilio-sacral screws combined with plate fixation were used in four patients (6.3%) [30]. Triangular osteosynthesis (another vertebropelvic fixation method, using screws or a plate as surgical treatment) was reported in two patients with modifications like plate fixation and decompression in seven patients (14.3% of all cases) [11, 14, 19]. In two (3.2%) patients open reduction and laminectomy were performed followed by immobilisation, and only one (1.6%) patient had trans-sacral plate alone [11, 13].
Limited access and minimal-invasive techniques
Restoration of the sacrum alone offers fracture reduction and fixation without fusion of motion segments in the lumbar spine. Ilio-sacral screw fixation as percutaneous osteosynthesis was performed in 20 (31.7%) of the U-shaped fractures in which the screws were either inserted unilaterally, bilaterally or trans-sacrally [17, 20]. Another recently published treatment option is a shortening osteotomy and sacro-sacral plating in limited access surgery in 3 cases of U-shaped fractures (4.8%) [24].
Post-operative complications
Interestingly, only one case report reported no post-operative complications [13]. Five studies with a total of 12 cases are not mentioning post-operative complications at all. Out of the remaining cases, 24 (38.1%) patients had post-operative complications.
Hardware associated complications
Hardware problems were reported in 2 cases of minimal-invasive treatment. One patient, initially treated with a percutaneous single unilateral ilio-sacral screw, had disengagement of the ilio-sacral screw without fixation failure [20]. The screw was removed 12 weeks after surgery due to persistent buttock pain. In the second study with percutaneous ilio-sacral screw insertion, one patient had a loss of reduction after 6 months without any further surgical intervention [17].
However, hardware associated problems occurred in open surgery as well. Screw loosening was reported in 3 cases with no additional surgery [28]. Three patients with triangular screw and trans-sacral plate fixation and two with spino-pelvic fixation complained of persistent pain from posterior prominent metal work and underwent removal of metal work after fracture healing [11, 28]. In another study, three patients complained of persistent pain at the screw insertion site, but no metalwork removal was needed [19].
Wound complications
Wound healing problems were noted in ten patients [11, 24, 28] of which eight required surgical washout, wound debridement and intravenous antibiotics, and one decubital ulcer due to metal work prominence needed surgical wound cleaning. All of these cases occurred in the open surgery group. Only one case of superficial wound infection was reported in the limited access study with shortening osteotomy and sacro-sacral plate fixation [24].
Follow-up and outcome
The follow-up time was mentioned in 10 studies (58 patients) with an average of 18.6 months (range 2–29 months). Where mentioned, only one patient was lost due to insufficient follow-up time [28].
The most common outcome measures used were neurological recovery and radiological healing. Ten studies with a total of 59 patients commented on post-operative neurological assessment, but as mentioned earlier the pre-operative neurology was only recorded in 53 patients. The 11 patients with pre-operative normal neurology had no neurological deficit after surgery. Out of 48 patients with pre-operative abnormal neurology, 5 patients did not have follow-up neurological assessment. Imaging to confirm fracture healing and alignment was reported in 8 articles with a total of 53 cases [11, 17, 19, 20, 28, 30, 32, 33].
Neurological outcome
For the sake of comparison between pre-operative and post-operative neurology in relation to surgical procedure, we focused only on those cases where complete pre-operative neurological assessment was recorded.
Among the remaining 43 patients, 20 (46.5%) had complete recovery. Two of these patients had open reduction, laminectomy and immobilisation, 7 had percutaneous sacro-iliac screws, 10 were treated with spino-pelvic fixation and decompression, and one patient had a sacro-sacral plate fixation. Fourteen patients (32.6%) had an incomplete recovery of their neurological deficits with mainly bowel and bladder function improvement at follow-up. Six of these patients had a spino-pelvic fixation, three sacro-iliac screws, three sacro-iliac screws with plate fixation and one sacro-sacral plate fixation.
Unfortunately, no long-term neurological improvement was seen in nine (21.9%) patients who had documented pre-operative abnormal neurology. Out of the open procedure group, five had spino-pelvic fixation and one triangular osteosynthesis. Three patients were treated with ilio-sacral screws and one sacro-sacral plate out of the minimally-invasive patients.
Radiological outcome
Fracture healing or fracture alignment was mentioned in 52 patients. Thirty-six underwent one of the open techniques for U-shaped fractures. Fifteen patients with minimally-invasive treatment had confirmed fracture healing or no loss of fracture reduction. Only one patient had a loss of reduction after anatomical alignment of the fracture at the 6-month follow-up (Table 2) [17].
Discussion
U-shaped sacral fractures usually result from axial loading of the spine with a significant amount of force and pivoting of the sacrum, leaving the spine and the pelvic ring as two complete dissociated bony structures [20]. The most common mechanism is a jump or fall from height. In this review, 67.3% of the fractures resulted from a jump or fall from height. Other mechanisms include motor vehicle accident, crush injuries and industrial accidents [11, 14, 20, 24]. Roy-Camille et al. first described the mechanism of U shaped sacral fractures in 1985. This classification depends on the displacement of the cephalad structure, the lumbar spine, against the intact posterior pelvic ring. If the lumbar spine is in lordosis at the time of injury then the upper fragment slips down vertically in front of the lower fragment (Type 3). On the other hand, if the lumbar spine is in kyphosis at the time of injury (a spontaneous protection position during fall) then initially the upper fragment bends forward (Type 1). With continued forward flexion, the upper fragment may then displace posteriorly and may become more or less horizontal lying on the superior surface of the lower fragment [22]. Irrespective of the type of fracture, the U-shaped sacral fractures are highly unstable fractures due to spino-pelvic dissociation [3, 11, 14, 15].
Due to the high-energy mechanism of U-shaped sacral fractures, they are often accompanied by other significant injuries. These injuries can range from calcaneal fractures (a common injury as result of fall) to severe chest injuries and even upper limb fractures [11, 17]. In this systematic review, 96.8% of patients were found to have associated injuries with U-shaped sacral fractures which result in prolonged immobilisation and its adverse consequences. If the U-shaped fractures are not diagnosed and treated properly and in a timely manner, they can result in progressive deformity and chronic pain [11]. Furthermore, due to unstable nature of the fracture and proximity to sacral and lumbar nerve roots, there is high association with neurological impairment [11]. Every effort should be made to evaluate and document the pre-operative neurological status although in patients with multiple injuries this might not be possible due to mechanical ventilation or life-threatening injuries needing immediate surgery. After the surgery it is very difficult to say whether the neurological injury resulted from initial injury or as a consequence of the surgical procedure. In this review, pre-operative neurology was not assessed in ten patients, post-operative neurology was abnormal in seven of these patients.
In polytrauma patients with other significant injuries, sacral fractures can be easily masked and missed. It is of paramount importance to actively look for these fractures in patients with a history of a fall from height, especially if the patients have clinical clues for sacral fracture like bruising over the lumbosacral area, tenderness or neurological deficit, then imaging should be arranged to rule out sacral fracture. On the standard AP X-rays, the transverse component of the fracture can be missed due to angulation of the fracture and bowel shadow. The apparent paradoxic pelvic inlet view of central bodies of upper sacral segments on standard AP X-rays should alert the treating physician [20]. Other features of U-shaped sacral fractures on a plain AP radiograph include bilateral transforaminal fractures, irregularities of superior sacral foraminal lines and transverse process fractures of the L5 vertebra [20, 22]. A lateral sacral radiograph is required for diagnosis but this is not part of trauma series [4, 13]. Once there is suspicion of U-shaped sacral fracture, a computed tomogram (CT) is almost always needed for fracture diagnosis and displacement assessment as well as devising the treatment plan [20, 25,31]. In this study, all the 30 patients had a CT scan either at presentation or after the initial radiographs.
Surgical stabilisation is thought to be more beneficial compared to non-operative management [3, 18, 27]. This review is focussing on all the patients who were treated by surgical stabilisation. In polytrauma patients, surgical stabilisation enables early mobilisation and avoids recumbence and its systemic adverse effects [1, 2, 10, 14, 18–20, 27, 30]. In addition to delayed mobilisation, without surgical treatment these highly unstable fractures may lead to deterioration in deformity and result in chronic pain. However, because of the low incidence and the heterogeneous nature of these fractures the evidence in literature is not convincing enough to support any specific treatment modality [1, 11].
In this review, the two most commonly used surgical techniques were spino-pelvic fixation and ilio-sacral screw fixation which were inserted unilaterally, bilaterally or trans-sacrally. The advocates of ilio-sacral screws argue that this technique causes less blood loss, less operative time and reduced post-op wound problems [7, 17, 20]. Due to high rate of associated neurological deficits with U shaped sacral fractures, it is generally thought that sacral decompression might help with the neurological recovery. In this review, among the patients who had recorded complete neurological recovery, 7 were treated with percutaneous ilio-sacral screws and 13 had decompression with either a spino-pelvic fixation, sacro-sacral plate or immobilisation [13, 20, 28]. However, the difficulty of inserting these percutaneous screws should not be underestimated [8, 33, 34]. Routt et al. [23] reported that there is a 10% chance of erroneous insertion of percutaneous ilio-sacral screws. For safe insertion, intra-operative orthogonal pelvic inlet and outlet and lateral sacral images are correlated with pre-operative CT scan images [20, 23, 34]. In experienced hands, the ilio-sacral screws can be inserted safely without electro-diagnostic monitoring [8].
Triangular osteosynthesis technique combines the vertical component (lumbopelvic distraction osteosynthesis) with transverse fixation (iliosacral screw or transiliac/transsacral plate). This construct provides multiplanar stability [16, 26, 27], which can allow early post-operative mobilisation with full weight bearing [26]. For U-shaped sacral fractures there is no comparative study between ilio-sacral screws and triangular osteosynthesis. Schildhauer et al. [26] in a cadaveric study compared the biomechanical stability of triangular osteosynthesis and ilio-sacral screws for vertical transforaminal fractures under cyclical loads. They concluded that triangular osteosynthesis provides significantly greater stability than ilio-sacral screws in vitro cyclical loading conditions, but there is no clinical study which has compared the long-term results of ilio-sacral screws to triangular osteosynthesis in U-shaped sacral fractures. However, because of greater biomechanical stability spino-pelvic reconstruction could be of advantage if the U-shaped fracture is highly displaced. In terms of complications, wound infections and pain due to prominent metalwork are comparatively common in patients with triangular osteosynthesis and spino-pelvic fixation [11, 28]. In this systematic review we found that 3 out of 6 patients (50%) with triangular osteosynthesis needed removal of metalwork and 2 out of 19 (10.5%) in the largest series of spino-pelvic fixation [1, 28].
Decompression alone will not provide any stability and long immobilisation will be required [13]. Decompression with spino-pelvic stabilisation can provide stability and early mobilisation is possible. However, from the current available evidence it can not be stated with confidence whether decompression has significant superiority in terms of long term neurological recovery.
Conclusion
U-shaped sacral fractures are rare injuries resulting from high-energy trauma. These fractures have a high rate of associated injuries and neurological deficit. The most common mechanism of injury is a jump or fall from height. Therefore, in the presence of other injuries resulting from this mechanism (e.g. bilateral calcaneal fractures), the U-shaped sacral fractures should be actively looked for and ruled out with proper imaging. Although lateral sacral radiographs can help in detecting these fractures, computed tomography is required most of the time to define the injury and plan treatment.
According to the current literature, the most common surgical method for treatments of U-shaped sacral fractures is percutaneous ilio-sacral screws and spino-pelvic fixation. Due to the limited amount of published cases, an evidence-based treatment strategy cannot be identified but a trend is seen towards minimal-invasive or limited access surgery. Open reconstruction could be a salvage option for fractures with massive displacement of the bony elements.
The radiological outcome showed good fracture alignment and healing in both groups indicating open, and minimally-invasive treatment strategies offer good fracture management.
However, sacral reduction and restoration techniques offer less surgical time and blood loss whilst preserving lumbar flexibility and should be the method of choice if the fracture is not highly unstable. There are fewer wound and metalwork related complications, and there is no evidence that neurological recovery is worse in minimally-invasive fixation compared to open procedures.
Acknowledgments
All figures and drawings used in this publications have been provided by Spinegraphics Nottingham (spinegraphics@gmx.net).
Conflict of interest
No benefits or funds in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Bellabarba C, Schildhauer TA, Vaccaro AR, Chapman JR. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine. 2006;31(11 Suppl):S80–S88. doi: 10.1097/01.brs.0000217949.31762.be. [DOI] [PubMed] [Google Scholar]
- 2.Browner BD, Cole JD, Graham JM, Bondurant FJ, Nunchuck-Burns SK, Colter HB. Delayed posterior internal fixation of unstable pelvic fractures. J Trauma. 1987;27(9):998–1006. doi: 10.1097/00005373-198709000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81. [PubMed] [Google Scholar]
- 4.Dussa CU, Soni BM. Influence of type of management of transverse sacral fractures on neurological outcome. A case series and review of literature. Spinal Cord. 2008;46:590–594. doi: 10.1038/sc.2008.59. [DOI] [PubMed] [Google Scholar]
- 5.Fisher RG. Sacral fracture with compression of cauda equina: surgical treatment. J Trauma. 1988;28:1678–1680. doi: 10.1097/00005373-198812000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Fountain SS, Hamilton RD, Jameson RM. Transverse fractures of the sacrum. A report of six cases. J Bone Joint Surg Am. 1977;59:486–489. [PubMed] [Google Scholar]
- 7.Gänsslen A, Hüfner T, Krettek C. Percutaneous iliosacral screw fixation of unstable pelvic injuries by conventional fluoroscopy. Oper Orthop Traumatol. 2006;18:225–244. doi: 10.1007/s00064-006-1173-3. [DOI] [PubMed] [Google Scholar]
- 8.Gardner MJ, Farrell ED, Nork SE, Segina DN, Routt ML., Jr Percutaneous placement of iliosacral screws without electrodiagnostic monitoring. J Trauma. 2009;66:1411–1415. doi: 10.1097/TA.0b013e31818080e9. [DOI] [PubMed] [Google Scholar]
- 9.Gibbons KJ, Soloniuk DS, Razack N. Neurological injury and patterns of sacral fractures. J Neurosurg. 1990;72:889–893. doi: 10.3171/jns.1990.72.6.0889. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein A, Phillips T, Sclafani SJ, Scalea T, Duncan A, Goldstein J, Panetta T, Shaftan G. Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma. 1986;26:325–333. doi: 10.1097/00005373-198604000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Gribnau AJ, Hensbroek PB, Haverlag R, Ponsen KJ, Been HD, Goslings JC. U-shaped sacral fractures: surgical treatment and quality of life. Injury. 2009;40:1040–1048. doi: 10.1016/j.injury.2008.11.027. [DOI] [PubMed] [Google Scholar]
- 12.Hessmann MH, Rommens PM. Transverse fracture-dislocation of the sacrum: a diagnostic pitfall and a surgical challenge. Acta Chir Belg. 2002;102:46–51. doi: 10.1080/00015458.2002.11679263. [DOI] [PubMed] [Google Scholar]
- 13.Hussin P, Chan CY, Saw LB, Kwan MK. U-shaped sacral fracture: an easily missed fracture with high morbidity A report of two cases. Emerg Med J. 2009;26:677–678. doi: 10.1136/emj.2008.064972. [DOI] [PubMed] [Google Scholar]
- 14.Hunt N, Jennings A, Smith M. Current management of U-shaped sacral fractures or spino-pelvic dissociation. Injury. 2002;33:123–126. doi: 10.1016/S0020-1383(00)00179-0. [DOI] [PubMed] [Google Scholar]
- 15.Isler B. Lumbosacral lesions associated with pelvic ring injuries. J Orthop Trauma. 1990;4:1–6. doi: 10.1097/00005131-199003000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Josten C, Schildhauer TA, Muhr G. Therapy of unstable sacrum fractures in pelvic ring. Results of osteosynthesis with early mobilization. Chirurg. 1994;65:970–975. [PubMed] [Google Scholar]
- 17.König MA, Seidel U, Heini P, Orler R, Quraishi NA, Boszczyk BM (2011) Minimal-invasive percutaneous reduction and trans-sacral screw fixation for U-shaped fractures. J Spinal Disord (Epub ahead of print) [DOI] [PubMed]
- 18.Matta JM, Tornetta P 3rd (1996) Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res (329):129–40 [DOI] [PubMed]
- 19.Mouhsine E, Wettstein M, Schizas C, Borens O, Blanc CH, Leyvraz PF, Theumann N, Garofalo R. Modified triangular posterior osteosynthesis of unstable sacrum fracture. Eur Spine J. 2006;15:857–863. doi: 10.1007/s00586-004-0858-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nork SE, Jones CB, Harding SP, Mirza SK, Routt ML., Jr Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma. 2001;15:238–246. doi: 10.1097/00005131-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Rhee WT, You SH, Jang YG, Lee SY. Lumbo-sacro-pelvic fixation using iliac screws for the complex lumbo-sacral fractures. J Korean Neurosurg Soc. 2007;42:495–498. doi: 10.3340/jkns.2007.42.6.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum. Suicidal jumper’s fracture. Spine. 1985;10:838–845. doi: 10.1097/00007632-198511000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Routt ML, Jr, Simonian PT, Agnew SG, Mann FA. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma. 1996;10:171–177. doi: 10.1097/00005131-199610000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Sabourin M, Lazennec JY, Catonne Y, Pascal-Moussellard H, Rousseau MA. Shortening osteotomy and sacro-sacral fixation for U-shaped fractures. J Spinal Disord Tech. 2010;23(7):457–460. doi: 10.1097/BSD.0b013e3181bee88f. [DOI] [PubMed] [Google Scholar]
- 25.Savolaine ER, Ebraheim NA, Rusin JJ, Jackson WT. Limitations of radiography and computed tomography in the diagnosis of transverse sacral fracture from a high fall. A case report. Clin Orthop Relat Res. 1991;272:122–126. [PubMed] [Google Scholar]
- 26.Schildhauer TA, Ledoux WR, Chapman JR, Henley MB, Tencer AF, Routt ML., Jr Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22–31. doi: 10.1097/00005131-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma. 1998;12:307–314. doi: 10.1097/00005131-199806000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Schildhauer TA, Bellabarba C, Nork SE, Barei DP, Routt ML, Jr, Chapman JR. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20:447–457. doi: 10.1097/00005131-200608000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Strange-Vognsen HH, Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma. 1991;5(2):200–203. doi: 10.1097/00005131-199105020-00014. [DOI] [PubMed] [Google Scholar]
- 30.Taguchi T, Kawai S, Kanuko K, Yugue D. Operative management of displaced fractures of the sacrum. J Orthop Sci. 1999;4:347–352. doi: 10.1007/s007760050115. [DOI] [PubMed] [Google Scholar]
- 31.Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman JR, Schildhauer T, Routt ML, Sasso RC. Diagnosis and management of sacral spine fractures. Instr Course Lect. 2004;53:375–385. [PubMed] [Google Scholar]
- 32.Vilela MD, Jermani C, Braga BP. Lumbopelvic fixation and sacral decompression for a U-shaped sacral fracture: case report. Arq Neuropsiquiatr. 2007;65:865–868. doi: 10.1590/S0004-282X2007000500028. [DOI] [PubMed] [Google Scholar]
- 33.Vilela MD, Gelfenbeyn M, Bellabarba C. U-shaped sacral fracture and lumbosacral dislocation as a result of a shotgun injury: case report. Neurosurgery. 2009;64:E193–E194. doi: 10.1227/01.NEU.0000336313.88450.5E. [DOI] [PubMed] [Google Scholar]
- 34.Ziran BH, Wasan AD, Marks DM, Olson SA, Chapman MW. Fluoroscopic imaging guides of the posterior pelvis pertaining to iliosacral screw placement. J Trauma. 2007;62:347–356. doi: 10.1097/01.ta.0000229789.18211.85. [DOI] [PubMed] [Google Scholar]