Introduction
Multiple myeloma (MM) is a B-cell malignancy occurring due to monoclonal expansion of plasma cells. It accounts for 10% of all hematopoietic malignancies. The classic triad in the diagnosis of MM is detection of serum or urine monoclonal or M protein, greater than 10% plasmacytosis on bone marrow examination and the presence of lytic bone lesions on radiological evaluation [1]. In rare instances, the plasma cell neoplasm may arise within the soft tissues, termed as extramedullary plasmacytomas (EMP) [2]. The EMP can occur as a de novo disease (primary or true EMP) or as a manifestation of MM (secondary EMP). .Although, over 80% of these EMP occurs in the head and neck region, but the involvement of the thyroid cartilage is a rare phenomenon. Only few cases have been reported in the English literature so far [3–6].
We report a 63- year- old patient with multiple myeloma, who developed plasmacytoma involving the thyroid cartilage 4 years after treatment with chemotherapy and autologous stem cell transplantation (ASCT).
Case Report
A 63-year-old man presented with complaints of increasing hoarseness of voice of 18 days duration, pain in the neck and difficulty in deglutition & breathing of 8 days duration. He had been diagnosed to be a case of multiple myeloma with plasmacytoma of the manubrium sterni and had been treated with VAD (vincristine, Adriamycin and dexamethasone) chemotherapy followed by ASCT with partial response.
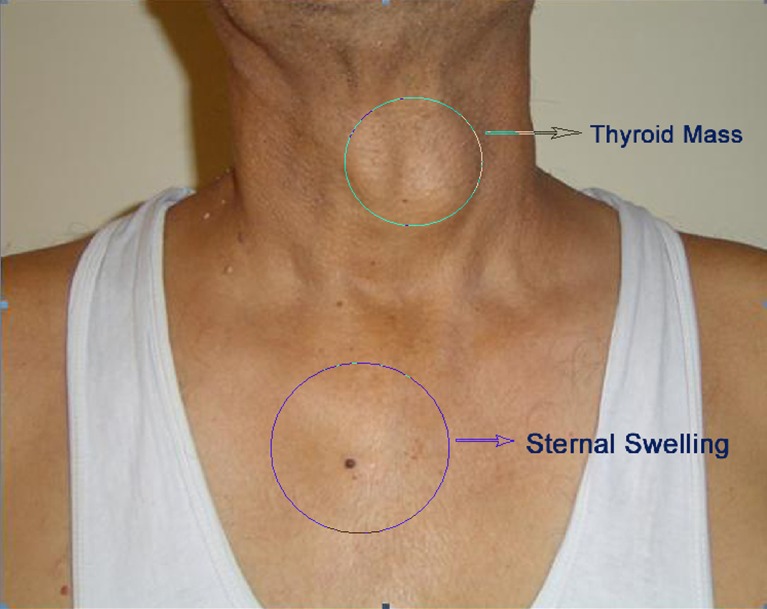
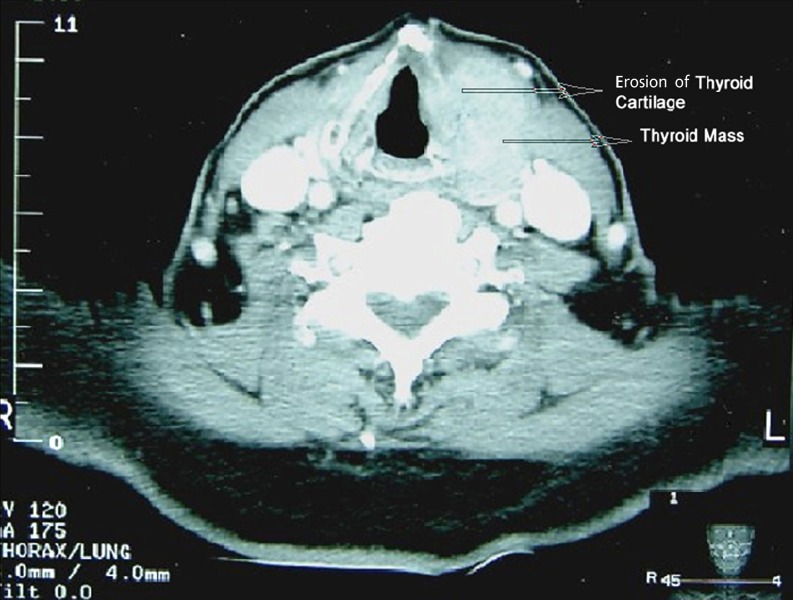
Physical examination revealed a nodule in left thyroid lobe and swelling of the manubrium sterni (Fig. 1). Indirect laryngoscopy revealed left vocal cord palsy. Investigations showed Hemoglobin 10.3 g/dl, total leukocyte count 4.9 × 109/l and platelet count 136 × 109/l. Serum protein electrophoresis showed no M-band in slow gamma region with IgG protein level 2,386 mg (normal 800–1,800 mg/dl). Bone marrow biopsy revealed hypocellular marrow with reduced normal hematopoietic elements with absence of plasma cells. Plain X-ray of the neck showed soft tissue mass containing discrete calcification in the anterior part of the neck abutting the thyroid cartilage. CT scan of the neck showed left thyroid mass with invasion of the left thyroid cartilage and vocal cord (Fig. 2). CT scan of the thorax revealed residual expansile lesion in the upper part of the sternum. Fine needle aspiration cytology (FNAC) from left thyroid nodule showed sheets of discretely lying mature and atypical plasma cells in a hemorrhagic background. The atypical plasma cells displayed variation in size and degree of plasmacytic differentiation, central to eccentric enlarged round, oval or irregular nucleus with nucleolar prominence. A diagnosis of extramedullary relapse was made.
Fig. 1.
Clinical photograph showing sternal swelling and left thyroid mass
Fig. 2.
CT scan of the neck showing soft tissue mass with erosion of left thyroid cartilage
The patient developed further worsening of hoarseness, breathing and dysphasia over the next few days, prompting the decision for surgical intervention. Intra-operatively, the nodule was very hard and friable and was densely adherent in the region of thyroid cartilage. An en-bloc resection of the mass including the thyroid cartilage was performed. The laryngeal mucosa was free of tumor mass and so spared. The right thyroid lobe did not show any pathology. Histopathology examination of the resected specimen showed diffuse population of immature plasma cell. The thyroid cartilage and bony trabeculae was infiltrated by tumor cells. The section from right thyroid lobe biopsy showed normal thyroid gland histology.
The post-operative course was uneventful and the patient was discharged on the third post-operative day. In the second post-operative week, during follow-up, the operative wound had healed well and the patient was symptom free. He reported to hospital again after 1 month with complaints of low backache, fever and altered sensorium. The patient was hospitalized and revaluated. The serum IgG immunoglobulin level was 6,600 mg/dl (normal range 800–1,800 mg/dl) bone marrow showed presence of plasma cells suggestive of bone marrow relapse. The patient refused further treatment and died after 1 week due to septicemia.
Discussion
Extramedullary plasmacytoma (EMP) are localized plasma cell neoplasm, which arise within soft tissue and account for 4% of all plasma cell disorders. Eighty percent of primary EMP occur in head and neck region and account for less than 1% of all head and neck tumors. The most common sites of involvement are sinonasal/nasopharyngeal area, oropharynx, and larynx in decreasing order of frequency. The diagnosis of primary EMP is made only after exclusion of MM, because one-third of the patients with EMP have underlying MM [7]. In majority of MM patients, EMP is clinically silent. On autopsy studies the usual site of involvement are liver, spleen and lymph nodes. The symptoms due to EMP are typically related to the site of lesions and in decreasing order of frequency are soft tissue mass [80%], airway obstruction [35%], epistaxis [35%] tumor associated local pain [20%], proptosis [15%], nasal discharge [10%] and cranial nerve palsy [10%] [8].
Involvement of thyroid cartilage is rare presentation and only few cases have been reported in the literature [3–6]. All had underlying multiple myeloma. In three patients, thyroid cartilage involvement was the initial presenting manifestation of multiple myeloma [4–6]. In the other patients, it was the site of relapse [3]. All these patients presented with anterior neck swelling, hoarseness and progressively increasing stridor. The symptoms are due to direct compression of larynx, infiltration or edema of the vocal cords [3–6]. Two factors forms the plausible basis of thyroid cartilage involvement in multiple myeloma, that are
Direct extension from adjacent plasmacytoma or
Metaplasia of cartilage to bone with formation of a marrow cavity in which plasma cell infiltration can take place.
The treatment of primary EMP of the head neck is controversial. Some authors recommend radiation therapy alone as EMP is highly radiosensitive [9, 10]. However, the dosage of radiation is not been well defined. Regimens with dosage between 3,000 and 8,000 rads over period of 3 to 6 weeks have been used [9]. Alexiou et al. [11] have recommended surgery, if the EMP is well localized and completely resectable. If complete removal is not possible, because of adjacent vital organs, the surgery followed by radiotherapy is preferred.
In patients with MM who have secondary EMP, chemotherapy and bone marrow transplantation remains the treatment of choice. Low dose radiotherapy (1,500–2,000 cGy) and surgery becomes an option, if there is airway compression or vital organs are involved.
All the four cases with secondary EMP involving the thyroid cartilage received local radiotherapy to relieve airway compression. Two patients who received radiotherapy in lower dose (1,500 cG) along with three cycles of VAD chemotherapy showed no significant decrease in tumor size and had to receive additional radiotherapy in higher doses (3,600 cG and 3,000 cG respectively) [4, 5]. The other two patients who received higher doses of radiotherapy (4,000 cG and 5,000 cG respectively) showed response with decrease in tumor mass and relief of airway obstruction. [3, 6]. In our patient the thyroid cartilage involvement was the manifestation of multiple myeloma relapse. We considered surgery rather than radiotherapy because the tumor mass was rapidly increasing in size and the patient had developed life threatening airway compression.
In summary, thyroid cartilage is a rare site of EMP and evaluation for underlying MM must be made in all patients. In patients with primary EMP, radiotherapy is therapy of choice. In patients with secondary EMP, treatment is directed towards the underlying MM and therapy of the EMP is palliative. Although, surgery stands as a ‘fallback’ option in secondary EMP but in life threatening situations, our clinical sense of judgment takes precedence. If the lesion is localized and amenable to surgery, it could be the first choice since it definitely carries less morbidity to the patient in terms of duration of treatment and the side effects.
References
- 1.Kyle RA. Diagnostic criteria of multiple myeloma. Hematol Oncol Clin North Am. 1992;6:347–58. [PubMed] [Google Scholar]
- 2.Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders. Report of the international myeloma working group. Brit J Hematol 2003:121:749–759 [PubMed]
- 3.Van Dyke CW, Masaryk TJ, Lavertu P. Multiple myeloma involving the thyroid cartilage. AJNR Am J Neuroradiol. 1996;17:570–572. [PMC free article] [PubMed] [Google Scholar]
- 4.Sosna J, Slasky BS, Paltiel O, Pizov G, Libson E. Multiple myeloma involving the thyroid cartilage: case report. AJNR Am J Neuroradiol. 2002;23:316–318. [PMC free article] [PubMed] [Google Scholar]
- 5.Gross M, Eliashar R, Petrova P, Goldfarb A, Sichel JY. Neck mass as primary manifestation of multiple myeloma originating in the thyroid cartilage. Otolaryngol Head Neck Surg. 2002;126:326–8. doi: 10.1067/mhn.2002.123045. [DOI] [PubMed] [Google Scholar]
- 6.Aslan I, Yenice H, Baserer N. An indolent course of multiple myeloma mimicking a solitary thyroid cartilage plasmacytoma. Eur Arch otorhinolaryngol. 2002;259:84–6. doi: 10.1007/s004050100399. [DOI] [PubMed] [Google Scholar]
- 7.Ewing MR, Foote FW., Jr Plasma cell tumors of the mouth and upper air passages. Cancer. 1952;5:499–513. doi: 10.1002/1097-0142(195205)5:3<499::AID-CNCR2820050310>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 8.Kapadia SB, Desai U, Cheng VS. Extramedullary plasmacytoma of the head and neck. Medicine (Baltimore) 1982;61:317–329. doi: 10.1097/00005792-198209000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Abemayor E, Canalis RF, Greenberg P, Wortham DG, Rowland JP, Sun NC. Plasma cell tumors of the head and neck. J Otolaryngol. 1988;17:376–381. [PubMed] [Google Scholar]
- 10.Susnerwala SS, Shanks JH, Banerjee SS, Scarffe JH, Farrington WT, Slevin NJ. Extramedullary plasmacytoma of the head and neck region: clinicopathological correlation in 25 cases. Br J cancer. 1997;75:921–927. doi: 10.1038/bjc.1997.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alexiou C, Kau RJ, Dietzfelbinger H, Kremer M, Spiess JC, Scharatzenstaller B, Arnold W. Extramedullary plasmacytoma. Tumor occurrence and therapeutic concepts. Cancer. 1999;85:2305–2314. doi: 10.1002/(SICI)1097-0142(19990601)85:11<2305::AID-CNCR2>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]