Abstract
Group A streptococcus (GAS) is a β-hemolytic bacterium often found in the throat and skin. The two most severe clinical manifestations of GAS are streptococcal toxic shock syndrome and necrotizing fasciitis. Intravenous immunoglobulin (IVIg) is a gamma globulin made from purified pooled plasma of thousands of donors, consisting mainly of IgG. We report the case of a 40-year-old man admitted after 2 days of vomiting and severe right-sided chest pain. He was hypotensive with a sinus tachycardia, pyrexial, and vasodilated. The only other positive finding was a swollen and erythematous chest wall. Muscle layer biopsies and blood cultures soon grew extensive GAS, and an initial diagnosis of necrotizing fasciitis was made. The clinical syndrome was of severe septic shock secondary to invasive GAS. The patient quickly deteriorated with a worsening metabolic acidosis. Despite maximal intensive care therapy including fluids, vasoactive agents, and also activated protein C, the patient continued to remain profoundly hypotensive. A decision was made to commence IVIg, with the aim of immunomodulation of the inflammatory cascade seen in sepsis. Over the next 24 hours the patient improved, was extubated 3 days later, and subsequently discharged from hospital after 2 weeks. Although the evidence for the use of IVIg in severe invasive GAS disease is limited, we feel that on reviewing the available literature its use in this case was justified. The limited worldwide supply and high costs, together with a limited evidence base, warrant restricting its use to cases in which conventional therapy has failed. The literature for use of intravenous immunoglobulin in invasive GAS infection will be reviewed in this article.
Keywords: Group A streptococcal disease, immunomodulation, intravenous immunoglobulin, septic shock
Introduction
Group A streptococcus (Strep. Pyogenes or GAS) is a β-hemolytic bacterium often found in the throat and the skin. It can be asymptomatic or cause simple infections like impetigo. The two most severe manifestations of GAS are streptococcal toxic shock syndrome (STSS) and necrotizing fasciitis (NF).[1] Annually in the United States there are between 9,000-11,500 cases of invasive disease (3.2 to 3.9/100,000 population); STSS and NF each account for approximately 6-7% of invasive cases. Each year there are greater than 10 million noninvasive GAS infections.[2]
The isolation of GAS, in a patient with severe sepsis, from a normally sterile site defines severe invasive GAS disease. GAS produces exotoxins and these superantigens are thought to circumvent traditional immune mechanisms, producing vast discharge of inflammatory cytokines.[3] There is an identifiable need for adjunctive therapy in these cases, as attributable mortality may be as high as 80%, despite prompt antimicrobial therapy.[1]
Case Report
A 40-year-old ex-smoker presented after 2 days of vomiting and severe right-sided chest pain. He was hypotensive with a sinus tachycardia, pyrexial, and vasodilated. The only other positive examination finding was a swollen and erythematous chest wall. Electrocardiogram, echocardiogram, and CXR were normal. Relevant blood tests were a reduced WCC at 2 × 109/L, raised CRP 361 mg/L, and acute renal failure with urea 14.8 mmol/L and creatinine 358 mmol/L. There were no factors predisposing to the patient being immunocompromised, and a human immunodeficiency virus (HIV) test was negative. Blood gases showed pH 7.12, base excess 10, lactate 4.2, pO2 17.5 kPa, and pCO2 3.1 on 80% inspired oxygen. The patient initially received 4 L of fluid resuscitation and intravenous tazocin and clarithromycin. He remained in severe septic shock despite further fluid boluses and a noradrenaline infusion. Following intubation he was commenced on renal replacement therapy, at 80 ml/kg for severe sepsis. Vasopressin and dobutamine were added, and cardiac output monitoring with pulse contour analysis (Lidco)© commenced: ScvO2 was 80%. Hydrocortisone and drotrecogin alfa (activated protein C) (APC) (see footnote) were also instituted. In relation to indications for the use of APC, all four systemic inflammatory response syndrome (SIRS) criteria were met; the patient had more than one sepsis-induced organ failure and there were no specific contraindications. In particular the platelet count was > 30 × 109/L (at 90 ×109/L) and the INR < 3.0 (1.5). The patient remained in a refractory septic shock and in multiorgan failure, and an adrenaline infusion was commenced.
An ultrasound scan of the chest wall showed no collections or abscess formation. Biopsies of the chest wall showed healthy tissue. However muscle layer biopsies and blood cultures soon grew extensive GAS and an initial diagnosis of NF was made. Further serotyping identified the highly virulent M1 subtype, which is disseminated worldwide. Microbiological advice was to change antibiotic therapy to benzlpenicillin and clindamycin. The patient was felt to be too unstable to take to theatre for debridement, and a plan was made to observe the chest wall and attempt operative intervention only if there was spreading fasciitis. The patient met the criteria[4] for the streptococcal toxic shock syndrome (STSS). Utilizing the recent centers for disease control (CDC)[5] position statement for the clinical case definition of STSS, classifies this patient as a confirmed case of STSS. In addition to identifying GAS from a normally sterile site (blood), the patient also satisfied the clinical manifestations within the definition. Namely these were hypotension (systolic blood pressure ≤ 90 mmHg) and multiorgan involvement characterized by the presence of two or more of renal impairment, coagulopathy, liver involvement, acute respiratory distress syndrome, a generalized erythematous macular rash, and soft tissue necrosis, including NF. A decision was made to commence intravenous immunoglobulin (IVIg) at 1 g/kg on day 1, followed by 0.5 g/kg on days 2 and 3, as the patient was continuing to deteriorate despite the above maximal medical therapy. The relevant public health authorities were informed, noting that scarlet fever (also caused by GAS) remains a notifiable disease in the United Kingdom. Over the next 24 hours the patient improved, was extubated 3 days later and was subsequently discharged from hospital after 2 weeks. The exact role played by IVIg within the improvement of this patient is difficult to quantify within the context of a case report; however we will discuss the mechanisms and evidence base, which we feel justified its use in this case.
Discussion
IVIg is a gamma globulin made from purified pooled plasma of thousands of donors, consisting mainly of IgG, and sourced from outside the United Kingdom due to the risk of Creutzfeldt-Jakob disease.[6] IVIg is thought to work by a variety of mechanisms including antibody protection against lipopolysaccharides, neutralizing superantigens, modulation of Fc-receptor blockade and expression, inhibition of membrane attack complexes (C5b-9), and complement activation and also by facilitating the opsonization of GAS bacteria. This concept of immunomodulation of the inflammatory cascade may apply during sepsis, with use of IVIg in GAS.[6,7]
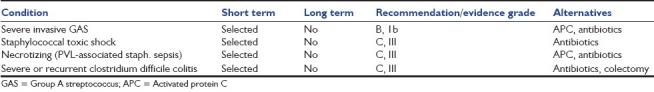
A multicenter, double-blind RCT examining the use of high dose IVIG as adjunctive therapy in STSS, in addition to clindamycin and penicillin, was published in 2003.[7] Placebo control was with 1% albumin, with the primary end point being effect on 28-day mortality with use of IVIg (1 g/kg on day 1, then 0.5 g/kg on days 2 and 3). This is the protocol currently used in our unit. Power calculation was for 120 patients, and only 21 were randomized due to recruitment difficulties. An insignificant trend toward lower mortality (10% vs. 36%), as well as a significant decrease in sepsis-related SOFA scores at days 2 (P=0.02) and 3 (P=0.04), was observed in the IVIg group. Further evidence is provided from a Canadian observational study comparing 21 consecutive patients who were given IVIg for STSS.[8] Although there was no difference in duration of ventilation or hospital stay (LOS), survival to 30 days was improved in the IVIg group (67% vs. 34%, P=0.02). In contrast a recent paper examining the use of IVIg in 84/192 pediatric STSS patients found no significant mortality reduction and longer LOS and higher hospital costs.[9] Current UK Department of Health guidelines for use of IVIg in infectious diseases [Table 1] recommends that “IVIg may be added to adequate toxin-neutralising antimicrobials, source control and sepsis management when these approaches have failed to elicit a response.”[10]
Table 1.
United Kingdom department of health guidelines for immunoglobulin use in infectious diseases[5]
This patient had severe septic shock where use of IVIg has also been reported. Turgeon et al.[11] looked at RCTs comparing IVIg with placebo (or no intervention) in critically ill adult patients with sepsis, and found a 26% survival benefit associated with use of polyclonal IVIg (RR 0.74 [95% CI, 0.62--0.89]: P=0.001 with a number of patients needed to treat to save one life (NNT) of 9. A meta-analysis by Laupland et al.[12] found overall significant reduction in mortality with IVIG treatment (OR 0.66 (95% CI, 0.53--0.83; P<0.0005), although this result was not confirmed when only high-quality studies were analyzed. Kreyman et al.[13] looked at 27 RCTs, 15 of which involved 1492 adults and children with trials of polyclonal IVIG in septic patients. Again reduced mortality was demonstrated, with adult data showing RR 0.79 (95% CI, 0.69--0.90). Among the authors’ conclusions in these trials was that, “an adequately powered RCT was needed to confirm the effects of IVIG in septic shock,” on the background of previous trials having methodological flaws and heterogeneous data. In 2007 the placebo-controlled RCT SBITS was published, which examined the use of IVIg in patients with sepsis.[14] Twenty-eight-day mortality was not reduced significantly, 37.3% versus 39.3% in the IVIg group (P=0.6695), and there was also no improvement in 7-day mortality or pulmonary function. One point of note was that this trial used a smaller total dose of IVIg (0.9 mg/kg), than the multicenter trial using IVIg in STSS.[7]
A Cochrane review update,[15] which found 17 trials in adults (n=1958), concluded that polyclonal IVIg had a mortality benefit in adults (RR 0.77, 95% CI 0.68--0.87); however this was not reproduced when examining trials with low risk of bias. Current DoH guidance,[10] and recent drugs and therapeutics bulletin advice, do not recommend the use of IVIg in general sepsis.
IVIG cost is climbing and well over $50/g. ($10,000 for a 100 kg (220 lbs) person at 2 g/kg), this will necessitate careful appraisal of its cost benefit by each treating institution. Neilson et al.[16] showed, on the basis of a meta-analysis of studies undertaken in adult septic patients, that the addition of IgM-enriched IVIG to standard therapy has a positive association with reduced mortality. The increased cost equated to €5715-€28443/life saved which compares favorably with other recommendations for adjuvant therapies in sepsis. For example, the addition of APC had a cost implication of €100728-€120176/life saved. A further meta-analysis[11] demonstrated favorable comparisons with other current recommendations in sepsis, in relation to NNT and on an economic basis, e.g., IVIg in adults; NNT 9, RR (95% CI): 0.74 (0.62--0.89) compared to APC; NNT 16, RR (95% CI): 0.80 (0.69--0.94).[11,17]
There are no recommendations for the use of IVIg in the current surviving sepsis guidelines for adults, though it may be considered it pediatric septic shock.[18] The omission of IVIg from these adult guidelines was recently reviewed,[19] with the conclusion being that small trials of low quality formed the basis of positive results. In addition the largest RCT (SBITS trial described above)[14] failed to demonstrate benefit, with standard IgG IVIg in adult septic patients. However the potential benefit of IgM-enriched IVIg preparations has been shown in experimental sepsis models and meta-analyses,[11,13] with Kreyman et al.[13] raising the possibility of “significant benefit of IgM-enriched IVIg in adult and neonatal sepsis.” It is likely that further larger controlled RCT's concerning IgM-enriched IVIg in adult sepsis will be needed prior to concrete recommendations in international sepsis guidelines.
Conclusion
A UK perspective, we feel the limited worldwide supply and high cost implications, together with an inconclusive evidence base, warrant restricting its use to cases in which conventional therapy has failed.
The authors note
Pharmaceutical company Eli Lilly's recent decision to withdraw Xigris (drotrecogin alfa (activated)) from the market worldwide further to the 28-day mortality results from the PROWESS-SHOCK study. This was at a date 18 months after the case report.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Davies DH, McGeer A, Schwartz B, Green K, Cann D, Simor AE, et al. Invasive group A streptococcal infections in Ontario, Canada.Ontario Group A Streptococcal Study Group. N Engl J Med. 1996;335:547–54. doi: 10.1056/NEJM199608223350803. [DOI] [PubMed] [Google Scholar]
- 2.O’Loughlin RE, Roberson A, Cieslak PR, Lynfield R, Gershman K, Craig A, et al. The Epidemiology of Invasive Group A Streptococcal Infections and Potential Vaccine Implications, United States, 2000-2004. Clin Infect Dis. 2007;45:853–62. doi: 10.1086/521264. [DOI] [PubMed] [Google Scholar]
- 3.I.V. immunoglobulin therapy for infectious diseases. Drug Ther Bull. 2010;48:57–60. doi: 10.1136/dtb.2009.07.0032. [DOI] [PubMed] [Google Scholar]
- 4.Hoge CW, Schwartz B, Talkington DF, Breiman RF, MacNeill EM, Englender SJ. The changing epidemiology of invasive group A streptococcal infections and the emergence of streptococcal toxic shock-like syndrome: a retrospective population-based study. JAMA. 1993;269:384–9. [PubMed] [Google Scholar]
- 5.Streptococcal Toxic-Shock Syndrome (STSS), 2010 Case Definition. CSTE Position Statement Number: 09-ID-60. Centers for Disease Control and Prevention. [Last accessed as on 2011 Aug 9]. Available from: http://www.cdc.gov/
- 6.Kivity S, Katz U, Daniel N, Nussinovitch U, Papageorgiou N, Shoenfeld Y. Evidence for the use of intravenous immunoglobulins- a review of the literature. Clin Rev Allergy Immunol. 2010;38:201–69. doi: 10.1007/s12016-009-8155-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Darenberg J, Ihendyane N, Sjölin J, Aufwerber E, Haidl S, Follin P, et al. Intravenous immunoglobulin G therapy in streptococcal toxic shock syndrome: A European randomised, double-blind, placebo-controlled trial. Clin Infect Dis. 2003;37:333–40. doi: 10.1086/376630. [DOI] [PubMed] [Google Scholar]
- 8.Kaul R, McGeer A, Norrby-Teglund A, Kotb M, Schwartz B, O’Rourke K, et al. Intravenous immunoglobulin therapy for streptococcal toxic shock syndrome- a comparative observational study. The Canadian Streptococcal Study Group. Clin Infect Dis. 1999;28:800–7. doi: 10.1086/515199. [DOI] [PubMed] [Google Scholar]
- 9.Shah SS, Hall M, Srivastava R, Subramony A, Levin JE. Intravenous immunoglobulin in children with streptococcal toxic shock syndrome. Clin Infect Dis. 2009;49:1369–76. doi: 10.1086/606048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.IVIg Guideline Development Group of the IVIg expert Working Group. Clinical Guidelines for Immunoglobulin Use. Department of Health Clinical guidelines for Immunoglobulin use, United Kingdom (DHUK) (2nd ed) 2008 May; [Google Scholar]
- 11.Turgeon AF, Hutton B, Fergusson DA, McIntyre L, Tinmouth AA, Cameron DW, et al. Meta-analysis: intravenous immunoglobulin in critically ill adult patients with sepsis. Ann Intern Med. 2007;146:193–203. doi: 10.7326/0003-4819-146-3-200702060-00009. [DOI] [PubMed] [Google Scholar]
- 12.Laupland KB, Kirkpatrick AW, Delaney A. Polyclonal intravenous immunoglobulin for the treatment of severe sepsis and septic shock in critically ill adults: A systematic review and meta-analysis. Crit Care Med. 2007;35:2686–92. [PubMed] [Google Scholar]
- 13.Kreymann KG, de Heer G, Nierhaus A, Kluge S. Use of polyclonal immunoglobulins as adjunctive therapy for sepsis or septic shock. Crit Care Med. 2007;35:2677–85. [PubMed] [Google Scholar]
- 14.Werdan K, Pilz G, Bujdoso O, Fraunberger P, Neeser G, Schmieder RE, et al. Score-based immunoglobulin G therapy of patients with sepsis: The SBITS study. Crit Care Med. 2007;35:2693–701. [PubMed] [Google Scholar]
- 15.Alejandria MM, Lansang MA, Dans LF, Mantaring JB. Intravenous immunoglobulin for treating sepsis and septic shock. [Last assessed as on 2010 Jan 3];Cochrane Database Syst Rev. 2002 1:CD001090. doi: 10.1002/14651858.CD001090. [DOI] [PubMed] [Google Scholar]
- 16.Neilson AR, Burchardi H, Schneider H. Cost-effectiveness of immunoglobulin M-enriched immunoglobulin (Pentaglobulin) in the treatment of severe sepsis and septic shock. J Crit Care. 2005;20:239–50. doi: 10.1016/j.jcrc.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 17.Berlot G, Bacer B, Piva M, Lucangelo U, Viviani M. Immunoglobulins in sepsis. Advances in Sepsis. 2007;6:41–6. [Google Scholar]
- 18.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:1394–6. doi: 10.1097/01.CCM.0000298158.12101.41. published correction appears. [DOI] [PubMed] [Google Scholar]
- 19.Esen F, Tugrul S. IgM-enriched Immunoglobulins in Sepsis. (Chapter) In: Vincent JL, editor. Intensive Care Medicine Annual Update. New York: Springer-Verlag; 2009. pp. 102–110. Section III, DOI: 101007/978-0-387-92278-2_10. [Google Scholar]


