Abstract
Heparin-binding epidermal growth factor-like growth factor (HB-EGF) is a cytoprotective agent in several organ systems but its roles in liver fibrosis are unclear. We studied the roles of HB-EGF in experimental liver fibrosis in mice and during hepatic stellate cell (HSC) activation. Thioacetamide (TAA; 100mg/kg) was administered by intra-peritoneal injection three times a week for 4 weeks to wild-type HB-EGF+/+ or HB-EGF-null (HB-EGF−/−) male mice. Livers were examined for histology and expression of key fibrotic markers. Primary cultured HSC isolated from untreated HB-EGF+/+ or HB-EGF−/− mice were examined for fibrotic markers and/or cell migration either during culture-induced activation or after exogenous HB-EGF (100 ng/ml) treatment. TAA induced liver fibrosis in both HB-EGF+/+ and HB-EGF−/− mice. Hepatic HB-EGF expression was decreased in TAA-treated HB-EGF+/+ mice by 37.6% (p < 0.05) as compared to animals receiving saline alone. HB-EGF−/− mice treated with TAA showed increased hepatic α-smooth muscle actin-positive cells and collagen deposition, and, as compared to HB-EGF+/+ mice, TAA-stimulated hepatic mRNA levels in HB-EGF−/− mice were, respectively, 2.1-, 1.7-, 1.8-, 2.2-, 1.2-, or 3.3-fold greater for α-smooth muscle actin, α1 chain of collagen I or III (COL1A1 or COL3A1), transforming growth factor-β1, connective tissue growth factor, or tissue inhibitor of metalloproteinase-1 (p < 0.05). HB-EGF expression was detectable in primary cultured HSC from HB-EGF+/+ mice. Both endogenous and exogenous HB-EGF inhibited HSC activation in primary culture, and HB-EGF enhanced HSC migration. These findings suggest that HB-EGF gene knockout in mice increases susceptibility to chronic TAA-induced hepatic fibrosis and that HB-EGF expression or action is associated with suppression of fibrogenic pathways in HSC.
Keywords: connective tissue growth factor, CTGF, HB-EGF, heparin-binding epidermal growth factor-like growth factor, hepatic stellate cells, liver fibrosis
Heparin-binding epidermal growth factor (EGF)-like growth factor (HB-EGF), a member of the EGF superfamily, is expressed by many cell types and is produced in multiple tissues such as lung, skeletal muscle, brain and heart (1, 2). HB-EGF participates in a variety of physiological and pathological processes including development, wound healing, blastocyst implantation, atherosclerosis, and tumor formation (2). Two recently established strains of HB-EGF knockout (HB-EGF−/−) mice (3, 4) have a relatively severe phenotype with a high incidence of neonatal death (5). Surviving HB-EGF−/− mice, however, grow normally and are fertile, but have a significantly shorter life span and exhibit defects that include enlarged and dysfunctional hearts, heart valve malformation including enlarged semilunar and atrioventricular valves, and thickened mesenchymal tissue and alveolar immaturity in the lungs (6). Impaired remodeling of HB-EGF−/− valves was not due to decreased apoptosis but rather to excessive proliferation of mesenchymal cells (3). In another conditional HB-EGF knockout mice, skin wound healing was retarded due to impaired keratinocyte migration (7, 8). On the other hand, over-expression of HB-EGF in pancreatic islets is associated with intra-islet fibrosis (9, 10).
Transgenic overexpression of HB-EGF in hepatocytes did not change liver/body weight ratios or the ratio of proliferating hepatocytes in adult mice but these parameters were both greater in transgenic mice after partial hepatectomy compared to wild type mice, supporting a role for HB-EGF in liver regeneration (11). In addition, hepatic expression of HB-EGF or transforming growth factor α (TGF-α) were increased after acute carbon tetrachloride (CCl4) injury in rats (12, 13), with Kupffer cells and sinusoidal endothelial cells being the prominent producers of HB-EGF. Kiso et al demonstrated that some hepatocytes in cirrhotic rat liver were positive for HB-EGF expression leading to the suggestions that ectopic expression of HB-EGF is associated with hepatocyte transformation during hepatocarcinogenesis (14).
As stated above, previous studies were designed to determine the role of HB-EGF in driving hepatocyte proliferation after acute injury or during tumorigenesis rather than to elucidate its potential contribution to pathways of hepatic fibrosis, especially in non-parenchymal liver cells. For example, there have been no published studies regarding the role of HB-EGF in liver fibrogenesis or activation of hepatic stellate cells (HSC), the latter of which play a key role in the development of liver fibrosis through their overt deposition of extracellular matrix components in response to the combined actions of transforming growth factor β1 (TGF-β1) and its downstream mediator, connective tissue growth factor (CTGF, also known as CCN2) (15–21). In the present studies, we have investigated the role of HB-EGF in HSC activation and liver fibrosis, including its modulation of TGF-β1 or CCN2 expression. We show that HB-EGF gene knockout in mice increases susceptibility to hepatic fibrosis in response to chronic liver injury induced by TAA or CCl4, and that HB-EGF expression or action is associated with suppression of fibrogenic pathways in HSC. These findings reveal a novel role of HB-EGF in HSC activation and liver fibrosis, and suggest that HB-EGF has potential therapeutic value for treating liver fibrosis.
MATERIALS AND METHODS
Mice
HB-EGF−/− and HB-EGF+/+ mice on a mixed C57BL/6J X 129/Sv background (B6;129-Hbegftm1Dcl/Mmnc) were a kind gift from Dr. David Lee (Chapel Hill, NC, USA). HB-EGF−/− mice were created by replacement of HB-EGF exons 1 and 2 with PGK-Neo, thus deleting the signal peptide and propeptide domains (4). The desired targeting events were verified by Southern blots of genomic DNA and exon-specific PCR, with Northern blots confirming absence of the respective transcripts. All animal procedures were approved by the Institutional Animal Care and Use Committee of The Research Institute at Nationwide Children’s Hospital (Columbus, OH, USA).
TAA administration
HB-EGF−/− or HB-EGF+/+ male mice, 6–8 weeks of age, received intra-peritoneal injection of either 100 mg/kg TAA (Sigma-Aldrich Co., St. Louis, MO, USA) in saline or saline alone three times per week for 4 weeks, and were sacrificed 72 hours after the last injection. Upon sacrifice, liver tissues were harvested either immediately and snap-frozen in liquid nitrogen for subsequent hepatic RNA extraction, or fixed with 4% paraformaldehyde (Sigma-Aldrich Co.) for histological analysis.
CCl4 administration
HB-EGF−/− or HB-EGF+/+ male mice received intra-peritoneal injection of 0.5 µl CCl4 (Sigma-Aldrich Co.) in 29.5 µl vegetable oil or 30 µl vegetable oil alone three times per week for 5 weeks. Seventy-two hours after the last injection, mice were sacrificed and livers were processed for histological evaluation.
Histology
Liver tissues were fixed with 4% paraformaldehyde in phosphate-buffered saline for 18 hours and then embedded in paraffin. Sections of 5 µm thickness were cut and stained with hematoxylin-eosin. For immunohistochemical detection of alpha-smooth muscle actin (α-SMA), slides were incubated with monoclonal mouse anti-α-SMA IgG (Dako, Glostrup, Denmark) followed by development with UltraTek reagents and AEC Chromogenic Substrates (all from ScyTek Laboratories, Logan, UT, USA) and hemotoxylin counterstain. Collagen was detected by staining sections with 0.1% Sirius Red (Sigma-Aldrich Co.). Photomicrographs were recorded with a Zeiss AxioCam HR Camera attached to a Zeiss Axioskop microscope (Carl Zeiss Vision GmbH, Germany). Protein staining for α-SMA, or collagen was analyzed with NIH image software ImageJ (version 1.34, US National Institute of Health).
Isolation and culture of mouse primary HSC or hepatocytes
HSC were isolated from livers of untreated HB-EGF−/− or HB-EGF+/+ male mice, 6–8 weeks of age, as previously described by us (17). HSC were harvested by gradient centrifugation using OptiPrep™ (Invitrogen, Carlsbad, CA, USA), resuspended in Dulbecco’s minimum essential medium (DMEM)/F-12 (Mediatech, Inc., Manassas, VA, USA) containing 20% fetal bovine serum, 100 U/ml penicillin and 100 mg/ml streptomycin (all from Mediatech, Inc.), plated into plastic tissue culture dishes or tissue culture plates (Corning Incorporated, Corning, NY, USA), and maintained at 37°C in a humidified atmosphere of 5% CO2/95% air. The next day, cells were replaced with fresh DMEM/F-12 containing 10% fetal bovine serum, and medium replacement was then repeated every other day if applicable. Cells were analyzed by RT-PCR for expression of fibrosis markers after 24-hour treatment with 0–100ng/ml recombinant HB-EGF (22) in the presence or absence of 10 µg/ml Diphtheria toxin mutant CRM197 (BioAcademia, Inc., Ibaraki, Osaka, Japan), which blocks HB-EGF receptor binding and inhibits HB-EGF activity.
Hepatocytes were isolated from untreated HB-EGF WT male mice, 6–8 weeks of age, by a modification of previously described methodology (23). Hepatocytes were resuspended in DMEM containing 10% fetal bovine serum, 100 U/ml penicillin and 100 mg/ml streptomycin, plated on 60-mm BD Biocoat Collagen I Culture Dishes (BD Biosciences, Bedford, MA, USA), and maintained at 37°C in a humidified atmosphere of 5% CO2/95% air. Four hours later, the medium was replaced with serum-free DMEM supplemented with 7.5 µg/ml of hydrocortisone (Sigma-Aldrich Co.), 1X insulin-transferrin sodium selenite (ITS) solution (Mediatech, Inc.), 100 U/ml penicillin and 100 mg/ml streptomycin, and medium replacement was then repeated every other day if applicable.
Immunofluorescence
Cells grown on coverslips in 6-well tissue culture plates were fixed with ice-cold 100% methanol for 20 min at 4°C. After blocking with 5% BSA in phosphate-buffered saline (PBS), cells were incubated with primary antibody against HB-EGF (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA) in blocking solution for 1 hour at 37°C, followed by secondary Alex Fluor 488 goat anti-mouse IgG (Invitrogen) for 45 min at room temperature. The coverslips were mounted in 10% glycerol and photomicrographs were recorded with a Zeiss AxioCam Camera attached to a Zeiss Axiovert 25 microscope (Carl Zeiss MicroImaging GmbH, München, Germany).
Cell migration
Primary cultured HSC were plated into 6-well tissue culture plates in DMEM/F-12 containing 10% fetal bovine serum and grown to confluence. After pre-incubation in DMEM/F-12 containing 0.5% fetal bovine serum for 24 hours, the cultures were scratch-wounded with a 10-µl pipette tip, washed twice with phosphate buffer saline, and then incubated for 24 hours with 100 ng/ml recombinant HB-EGF in the presence or absence of 10 µg/ml CRM197. Photographs of the scraped area in each well were recorded using a Zeiss AxionCam Camera. Cell migration was quantified by the number of cells migrated to the scratched area after 24 hours.
RNA extraction and reverse transcription
Total cellular RNA was extracted using Trizol® Reagent (Invitrogen), and reverse transcribed to produce cDNA using Superscript® II Reverse Transcriptase (Invitrogen) and Oligo(dT)12–16 primers (Applied Biosystems, Foster City, CA, USA) according to the manufactures' directions.
Polymerase chain reaction (PCR) and quantitative real-time PCR
The primer sequences were as follows: α-SMA: 5’-TTC GTT ACT ACT GCT GAG CGT GAG A-3' (sense) and 5’-AAA GAT GGC TGG AAG AGG GTC-3' (antisense) (200 bp); β-actin: 5’-TGT TAC CAA CTG GGA CGA CA-3' (sense) and 5’-CTT TTC ACG GTT GGC CTT AG-3' (antisense) (130 bp); CCN2: 5’-CCA GGA AGT AAG GGA CAC GA-3' (sense) and 5’-GGT TCT CAC TTT GGT GGG AT-3' (antisense) (148 bp); α1 chain of collagen I (COL1A1): 5’-CCA AGG GTA ACA GCG GTG AA-3' (sense) and 5’-CCT CGT TTT CCT TCT TCT CCG-3' (antisense) (124 bp); α1 chain of collagen III (COL3A1): 5’-AAC GGA GCT CCT GGC CCC AT-3' (sense) and 5’-CCA TCA CTG CCC CGA GCA CC-3' (antisense) (113 bp); TGF-β1: 5’-GGT TCA TGT CAT GGA TGG TGC-3' (sense) and 5’-TGA CGT CAC TGG AGT TGT ACG-3' (antisense) (130 bp); and TIMP-1: 5’-GCA TCT CTG GCA TCT GGC ATC-3' (sense) and 5’-GCG GTT CTG GGA CTT GTG GGC-3' (antisense) (294 bp). Primers were validated by PCR and products were confirmed by 1.5 % agrose gel electrophoresis using ethidium bromide staining. To measure gene expression, first strand cDNA products mixed with primers and SYBR® Green PCR Master Mix reagent (Applied Biosystems) were subjected to quantitative real-time PCR on an Applied Biosystems 7500 Real-Time PCR System, and the cycling parameters were: 50°C for 2 min, 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1min. Samples were run in triplicate, and expression values were normalized to housekeeping gene β-actin primers using the ΔΔCt method.
Statistical Analysis
Data are presented as mean ± S.D. Statistical analysis was performed using ANOVA one-way test, with p < .05 considered to be statistically significant.
RESULTS
Enhanced susceptibility of HB-EGF−/− mice to liver fibrosis induced by chronic injury
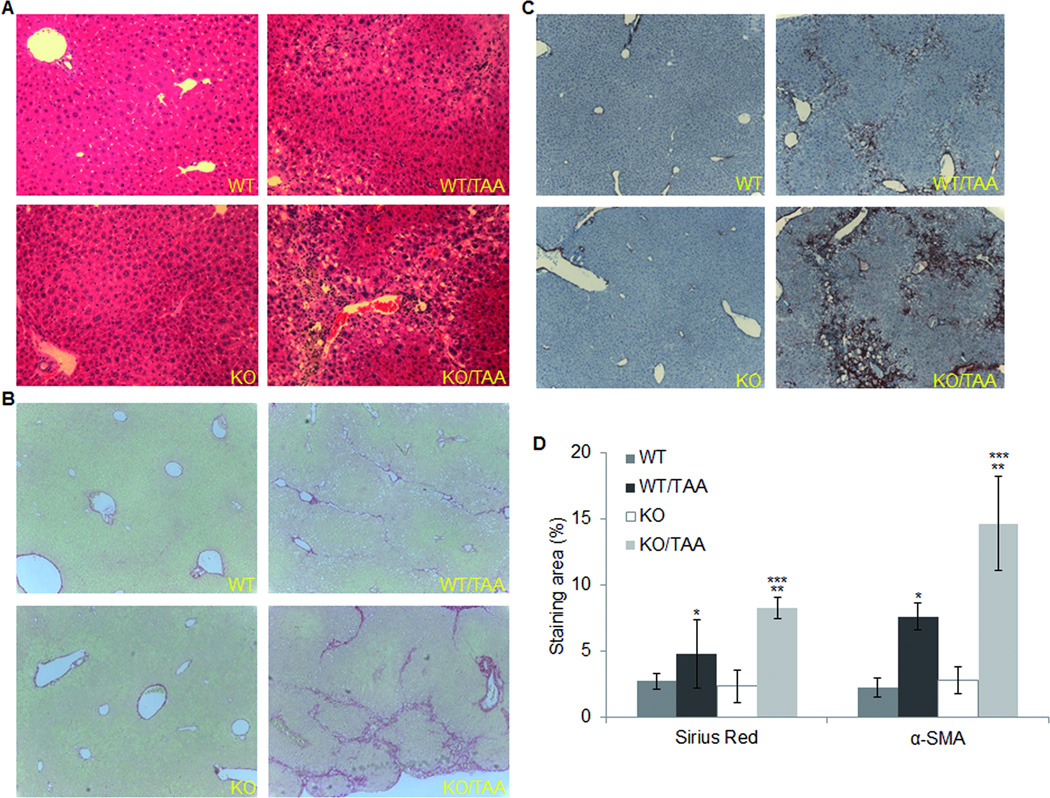
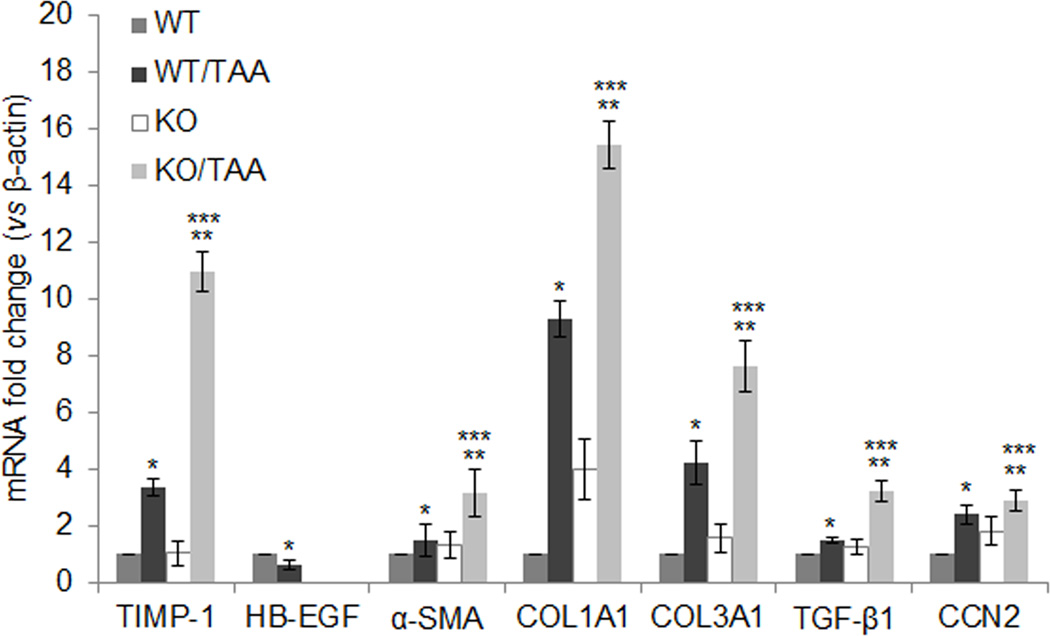
No differences in liver histology were evident between HB-EGF−/− and HB-EGF+/+ mice treated with saline alone (Fig. 1A). Compared to these controls, chronic administration of TAA induced liver fibrosis in either HB-EGF+/+ or HB-EGF−/− mice (Fig. 1), as shown by a 1.7- or 3.6-fold increase respectively in collagen deposition (p < 0.05) (Fig. 1D and Table S1) and a 3.3- or 10.6-fold increase respectively in TIMP-1 gene expression (p < 0.05) (Fig. 2). After chronic TAA administration in HB-EGF+/+ mice, hepatic HB-EGF gene expression decreased by 37.6% (p < 0.05) (Fig. 2), showing that suppression of HB-EGF expression was associated with onset and/or progression of liver fibrosis.
Fig. 1. Histology.
HB-EGF+/+ (WT) or HB-EGF−/− (KO) mice were injected with TAA three times per week for 4 weeks. Liver tissues were removed, fixed, and sections of 5 µm were stained with H&E (A), Sirius Red (B), or with an α-SMA antibody (C). Sirius Red or α-SMA staining was analyzed with NIH image software ImageJ (D). Data are the mean ± S.D. of each group (n=3, 4 or 5) with triplicate determinations. *p < 0.05 vs WT, **p < 0.05 vs KO, ***p < 0.05 vs WT/TAA.
Fig. 2. Fibrogenic gene expression in liver.
HB-EGF WT or KO mice were injected with TAA for 4 weeks and hepatic total RNA was extracted. Samples were subjected to quantitative real-time PCR for determination of hepatic expression of TIMP-1, HB-EGF, α-SMA,COL1A1, COL3A1, TGF-β1, or CCN2 mRNA. Data are the means ± S.D. of each group (n=3, 4 or 5) with triplicate determinations. *p < 0.05 vs WT, **p < 0.05 vs KO, ***p < 0.05 vs WT/TAA.
Chronic TAA administration resulted in a 1.9- or 1.7-fold higher level of, respectively, α-SMA immunoreactivity (p < 0.05; Fig. 1D) or collagen staining (p < 0.05; Fig. 1D) in HB-EGF−/− mice versus HB-EGF+/+ mice. As compared to HB-EGF+/+ mice, TAA-stimulated hepatic mRNA levels in HB-EGF−/− mice were, respectively, 2.1-, 1.7-, 1.8-, 2.2-, 1.2-, or 3.3-fold greater for α-SMA, COL1A1, COL3A1, TGF-β1, CCN2 or TIMP-1 (Fig. 2). Collectively these data show that absence of HB-EGF gene expression in murine experimental fibrosis resulted in enhanced production of α-SMA-positive cells, collagen deposition and expression of pro-fibrotic genes.
To verify that the inhibitory effect of HB-EGF was not restricted to TAA-induced liver fibrosis, HB-EGF WT and KO mice alternatively received CCl4 for 5 weeks and livers were processed for histological evaluation. HB-EGF KO mice demonstrated more collagen deposition as shown by Sirius Red staining (Fig. S1), suggesting enhanced susceptibility of HB-EGF KO mice to CCl4-induced fibrosis.
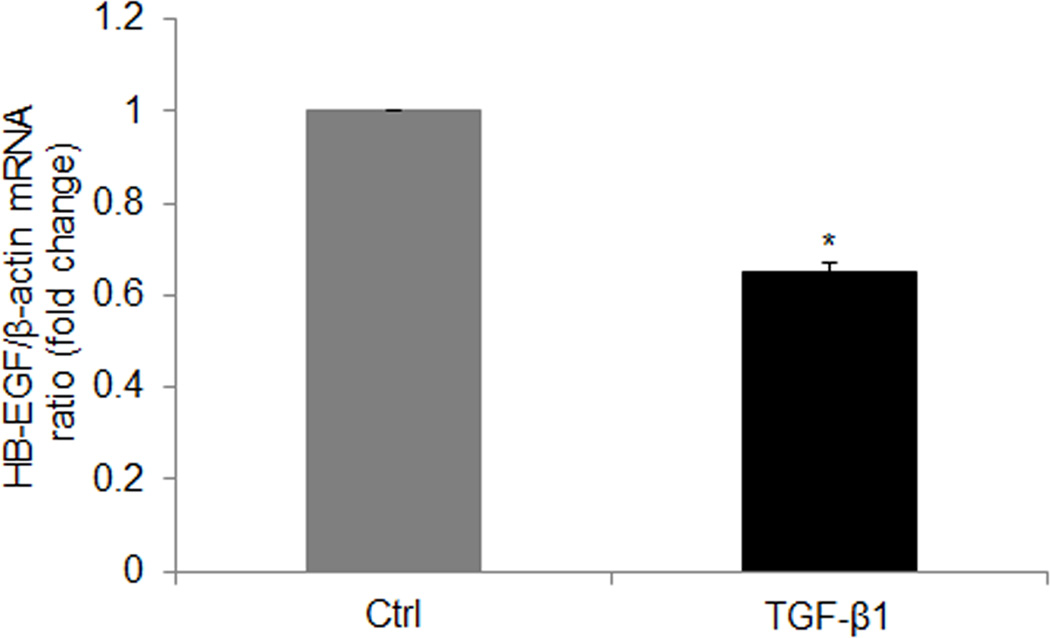
Gene expression of HB-EGF in primary cultures of hepatocytes or HSC
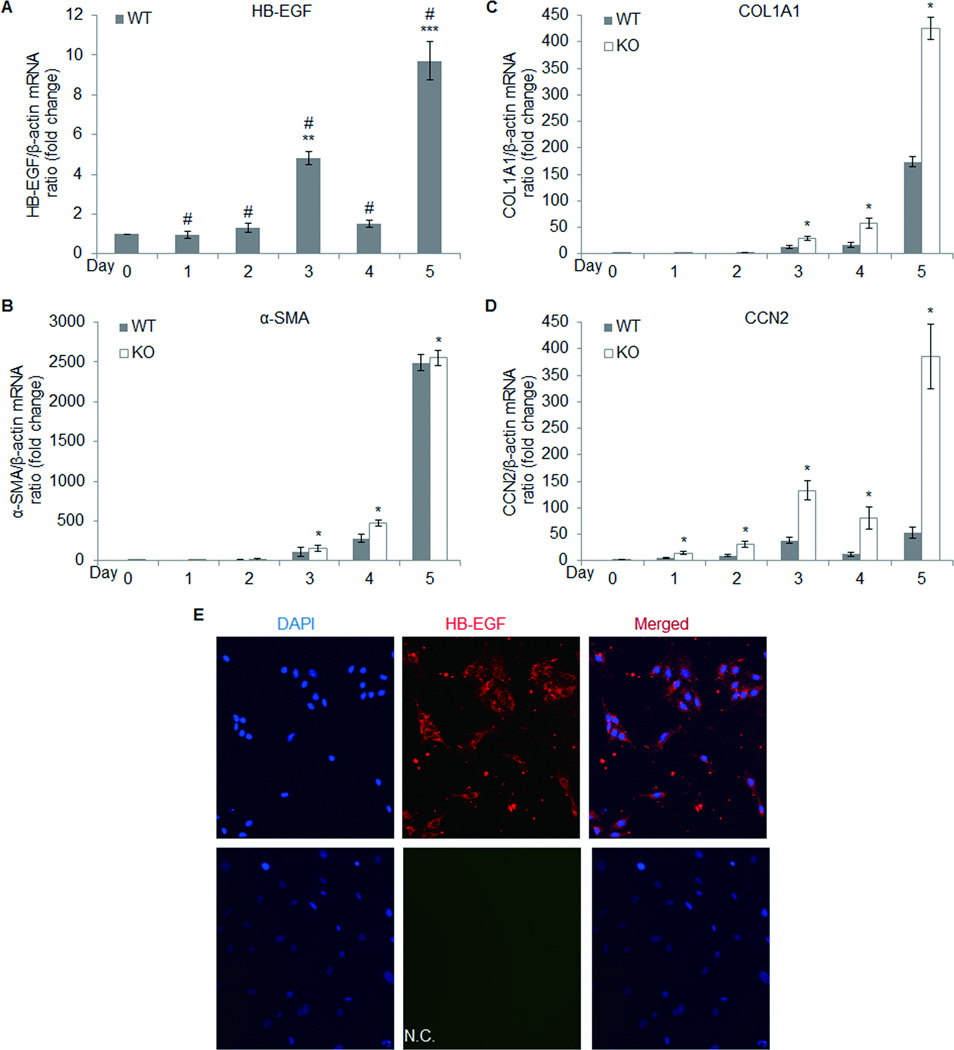
Previous data have shown that HB-EGF is produced by Kupffer cells, sinusoidal endothelial cells, and under-stimulated or abnormal hepatocytes (24, 25). We extended these studies to show that HB-EGF was expressed by normal cultured mouse primary hepatocytes but that the level of HB-EGF mRNA was decreased by 35% after treatment of the cells with 2 ng/ml TGF-β1 (eBioscience, Inc., San Diego, CA, USA) (p < 0.05; Fig. 3). Since hepatocytes are the principal hepatic cell type, this phenomenon was consistent with the overall decreased tissue expression of HB-EGF in fibrotic liver (Fig. 2). On the other hand, since HSC play a pivot role in fibrogenesis even though they are present in the liver at much lower frequency than hepatocytes, we also examined the role of HB-EGF in HSC function. To do this, HSC were isolated from untreated HB-EGF+/+ male mice at 6–8 weeks of age and allowed to grow in culture for up to 5 days. HSC cultures demonstrated typical characteristics as we have previously reported (17) and also stained positively for glial fibrillary acidic protein (GFAP), a well-characterized HSC marker (Fig. S2). As shown in Fig. 4A, HB-EGF mRNA expression increased significantly during the first 5 days of culture, corresponding to the period during which the cells autonomously self-activated and acquired an α-SMA-positive myofibroblastic phenotype (data not shown). HB-EGF mRNA expression levels were correlated with those of CCN2 mRNA, including a transient decrease in expression on Day 4 (Fig. 4A, D). By Day 5 of culture, the presence of low levels of HB-EGF protein in the cells was demonstrable by immunofluorescence (Fig. 4E). Expression of mRNA for α-SMA or COL1A1 increased on successive days over the same time period (Fig. 4B, C and Table S2).
Fig. 3. Effect of exogenous recombinant TGF-β1 on HB-EGF gene expression in primary cultured hepatocytes.
Hepatocytes isolated from untreated HB-EGF WT mice were cultured for 2 days. Cells were pre-incubated in DMEM containing 0.5% fetal bovine serum for 24 hours, followed by treatment of the cells with 2 ng/ml recombinant human TGF-β1 for an additional 24 hours. RNA was isolated and analyzed by quantitative real-time PCR to determine HB-EGF expression. Data are the mean ± S.D. of three experiments with triplicate determinations. *p < 0.05 vs control.
Fig. 4. Fibrogenic gene expression in primary cultured HSC.
Stellate cells isolated from untreated HB-EGF WT or KO mice were cultured for 5 days. Total cellular RNA extracted from each day of culture was subjected to quantitative real-time PCR to determine expression of HB-EGF (A), α-SMA (B), COL1A1 (C) or CCN2 (D). Wild type cells grown on coverslips for 5 days were fixed and processed to detect HB-EGF protein by immunofluorescence (E). Data are the mean ± S.D. of three experiments with triplicate determinations. # p < 0.05 vs Day 0; **p < 0.05 vs Day 1 or Day 2; ***p < 0.05 vs Day 1, 2, 3 or Day 4; *P < 0.05 vs WT. N.C., negative control or without anti-HB-EGF antibody.
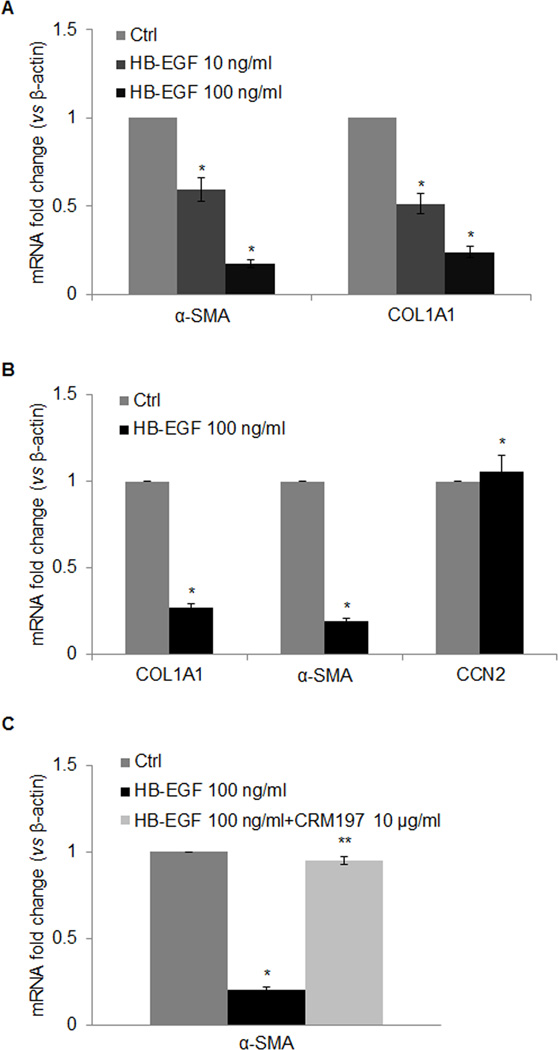
HB-EGF inhibits α-SMA or COL1A1 expression in primary cultured HSC
When HSC were cultured for 5 days, the cells from untreated HB-EGF−/− mice expressed higher mRNA levels for α-SMA (Fig. 4B), COL1A1 (Fig. 4C) or CCN2 (Fig. 4D) than those from untreated HB-EGF+/+ mice, showing that endogenous HB-EGF expression suppresses HSC activation and fibrogenesis (p < 0.05). Additionally, expression of α-SMA or COL1A1 was significantly decreased by treatment of Day 3 HSC from either untreated B6;129-Hbegftm1Dcl/Mmnc HB-EGF+/+ mice (Fig. 5B) or healthy male wild type Balb/c mice (Fig. 5A) with recombinant HB-EGF (p < 0.05), although this treatment did not significantly alter CCN2 gene expression in the same cells. Importantly, the inhibitory effect of HB-EGF on α-SMA or COL1A1 gene expression was reversed by 10 µg/ml CRM197, a specific HB-EGF inhibitor (Fig. 5C). Incubation of HB-EGF+/+ HSC with exogenous recombinant HB-EGF inhibited endogenous HB-EGF gene expression by 60.4% (p < 0.05; Fig. 6).
Fig. 5. Effect of HB-EGF on fibrogenic gene expression in HSC primary culture.
Stellate cells isolated from untreated healthy Balb/c wild type mice (A) or B6;129-Hbegftm1Dcl/Mmnc HB-EGF WT mice (B, C) were cultured for 3 days. Cells were pre-incubated in DMEM/F-12 containing 0.5% fetal bovine serum for 24 hours, followed by treatment with recombinant human HB-EGF for an additional 24 hours with (C) or without (A, B) 10 µg/ml CRM197 prior to analysis of mRNA expression of α-SMA, COL1A1 or CCN2 by quantitative real-time PCR. Data are the mean ± S.D. of three experiments with triplicate determinations. *p < 0.05 vs control (Ctrl); **p < 0.05 vs HB-EGF.
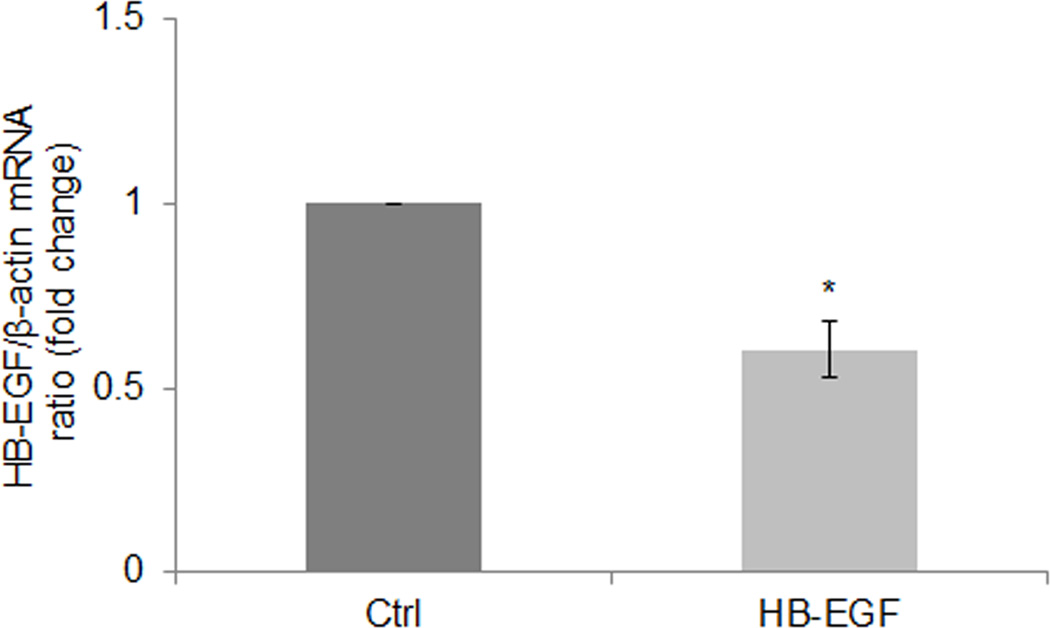
Fig. 6. Effect of exogenous recombinant HB-EGF on endogenous HB-EGF gene expression in primary cultured HSC.
Stellate cells isolated from untreated HB-EGF WT mice were cultured for 3 days. Cells were pre-incubated in DMEM/F-12 containing 0.5% fetal bovine serum for 24 hours, followed by treatment with 100ng/ml recombinant human HB-EGF for an additional 24 hours. HB-EGF mRNA expression was analyzed by quantitative real-time PCR. Data are the mean ± S.D. of three experiments with triplicate determinations. *p < 0.05 vs control (Ctrl).
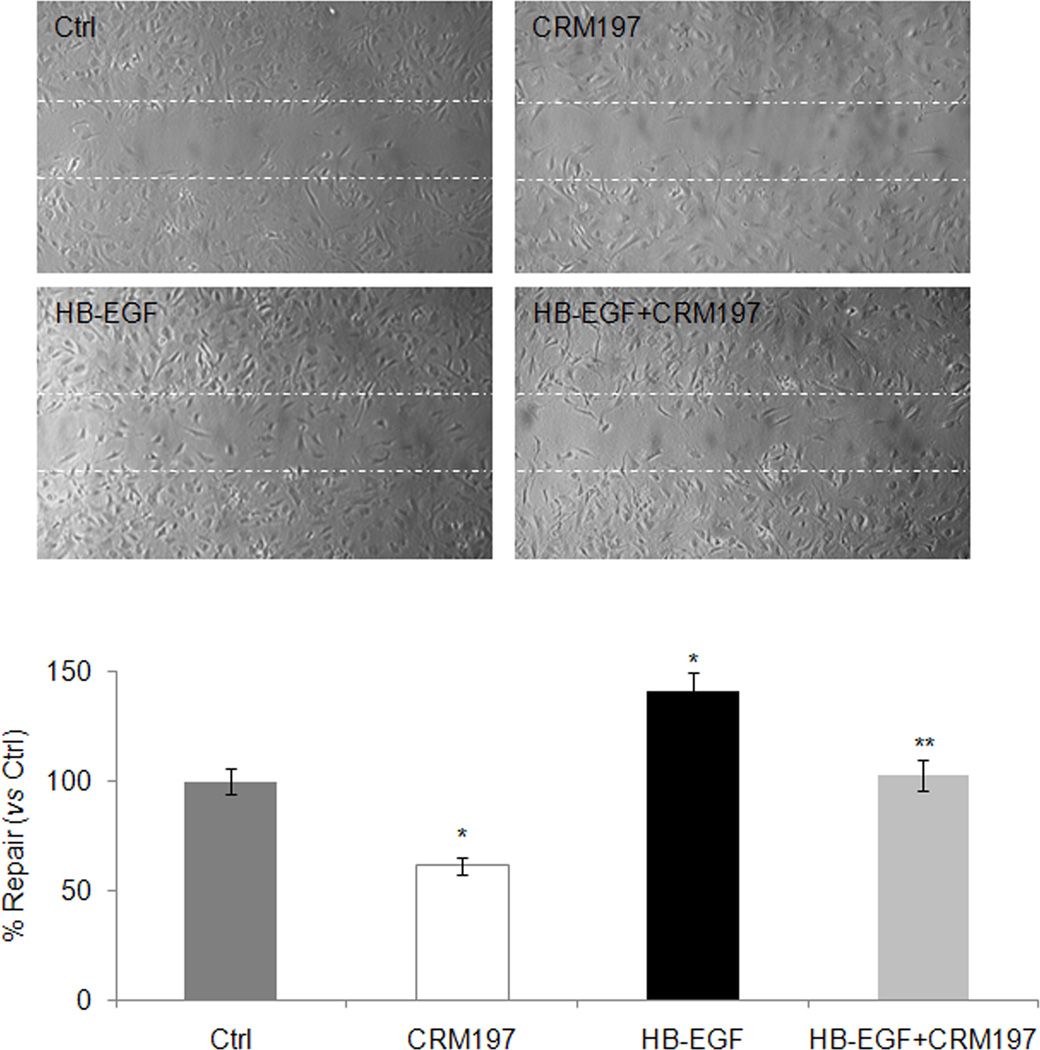
HB-EGF enhances HSC migration
Scratch wounding of confluent HSC resulted in a reproducibly exposed area into which the remaining cells could migrate. While a few cells migrated into this zone over the next 24 hours, the rate of HSC migration was significantly stimulated by addition of 100 ng/ml recombinant HB-EGF and this effect was blocked in the presence of 10 µg/ml CRM197 (Fig. 7).
Fig. 7. Effect of exogenous recombinant HB-EGF on HSC migration.
Primary cultured HSC isolated from HB-EGF WT mice were cultured for 5 days, detached by digestion with trypsin, and plated into 6-well tissue culture plates. After pre-incubation in DMEM/F-12 containing 0.5% fetal bovine serum for 24 hours, the cultures were scratch-wounded with a 10-µl pipette tip, and incubated with 100 ng/ml recombinant HB-EGF with or without 10 µg/ml CRM197 for an additional 24 hours. The bar chart shows the number of cells in the scratched area (% versus control). Each bar represents mean ± S.D. from three experiments. Photomicrographs are representative of three experiments. Dotted line indicates wound margin. *p < 0.05 vs Ctrl; **P < 0.05 vs HB-EGF. Ctrl, control.
DISCUSSION
The EGF family comprises EGF, TGF-α, HB-EGF, amphiregulin (AR) and betacellulin, the latter three of which contain unique structural components that allows the proteins to bind to heparin-like molecules on cell surfaces in addition to the classic avian erythroblastosis oncogene B (ErbB)-type EGF receptors. Collectively, these proteins play fundamental roles in development, cell proliferation, differentiation, and tumor formation. HB-EGF was first identified in the conditioned medium of cultured human macrophages and is synthesized as a 208-residue bioactive transmembrane precursor protein (proHB-EGF) which undergoes extracellular proteolytic cleavage to yield a 14–20 kDa soluble growth factor (sHB-EGF) (26–28). HB-EGF is produced in multiple cell types in response to hypoxia or tissue damage and it acts as a potent mitogen and chemoattractant (29).
HB-EGF expression is increased in hepatic endothelial cells or Kupffer cells following acute exposure to hepatotoxins (11–13) while its production by hepatocytes is increased after partial hepatectomy or in biopsies of human hepatocellular carcinoma (2, 30) and its enhanced expression has been associated with the development or progression of human and rat hepatocarcinoma (14). Whereas these previous reports linked increased hepatic HB-EGF expression to either wound healing or tumorigenesis, studies of the role of HB-EGF in hepatic fibrosis have not previously been reported. In addressing this question in these studies, we found that the well-documented model of TAA-induced liver fibrosis was actually associated with a 35% decrease in hepatic HB-EGF gene expression in wild type mice and that, further, expression of HB-EGF by primary cultured hepatocytes was inhibited by TGF-β1, the latter of which is a well-characterized inhibitor of epithelial function in addition to acting as a stimulator of fibrogenic pathways in mesenchymal cells. While hepatic HB-EGF expression was readily detected by RT-PCR of isolated RNA, both HB-EGF mRNA and protein levels were present at low levels in wild type mice (and even less so in fibrotic animals) and were beyond our technical abilities to detect by, respectively, in situ hybridization or immunohistochemistry (data not shown). Nonetheless, the knockout model provided important confirmatory data in as much that, as assessed by collagen deposition, the presence of α-SMA-positive cells, and mRNA expression of fibrogenic markers (TGF-β1, CCN2, α-SMA, COL1A1, COL3A1, TIMP-1), chronic TAA administration caused more severe liver fibrosis in HB-EGF knockout mice than their wild-type counterparts. Taken together, these data showed that total hepatic HB-EGF mRNA expression was reduced during experimental fibrosis and that the fibrotic response was exacerbated in the absence of HB-EGF. These findings are consistent with one another and indicate that hepatic HB-EGF expression is associated with a suppression of liver fibrosis.
The association between HB-EGF and fibrosis is novel and was thus investigated further in HSC since this cell type plays a key role in fibrogenic pathways. During chronic injury, HSC differentiate into α-SMA-positive cells that are perpetually activated and unrelentingly deposit fibrillar collagens and other extracellular matrix components in the interstitial spaces, resulting in accumulation of scar tissue and loss of hepatic function (15, 20). Our studies showed that HSC are a bone fide source of HB-EGF and that during culture-induced activation, HSC expression of HB-EGF mRNA increases as does that of fibrosis-related markers such as α-SMA, COL1A1 and CCN2 (17). Whereas this pattern of increased HB-EGF expression during HSC activation might appear to contradict the finding of decreased HB-EGF expression in fibrotic liver in vivo, we further showed that culture-induced mRNA expression of α-SMA, COL1A1 or CCN2 was higher in HB-EGF−/− HSC as compared to HB-EGF+/+ HSC. These results suggest that under normal circumstances, HB-EGF acts to dampen activation of fibrogenic pathways in HSC. Indeed, this possibility was supported by the finding that addition of recombinant HB-EGF to Day 3 HSC from wild type mice resulted in an inhibition of α-SMA or COL1A1 mRNA production. Thus even though total hepatic HB-EGF expression decreases after fibrosing injury in vivo and activation of HSC in vitro is associated with increased HB-EGF expression, the results of gene knockout unequivocally establish hepatic HB-EGF as a natural suppressor of the fibrotic response in as much as (i) the severity of fibrosis was greater in HB-EGF−/− mice; (ii) activated HSC from HB-EGF−/− mice demonstrated enhanced α-SMA or collagen mRNA production; and (iii) HSC activation and collagen production were inhibited by exposure of the cells to exogenous HB-EGF. Finally, CRM197, a specific inhibitor of HB-EGF, can reverse the effect of HB-EGF on HSC activation.
While HB-EGF was inhibitory for HSC α-SMA or collagen mRNA production, we demonstrated that exogenous HB-EGF stimulated HSC migration. Thus it is plausible that the increased hepatic HB-EGF production and release by hepatocytes or Kupfer cells reported in previous tissue injury studies (11–13, 25, 26) serves not only as a direct stimulus for parenchymal cell proliferation but also as chemotactic stimulus for HSC which allows them to migrate to sites of injury and participate in the wound healing process. We propose that as a fibrotic environment subsequently develops, HB-EGF may then serve to limit the extent or degree of fibrosis through its ability to attenuate activation and fibrogenesis in HSC, a possibility that is supported by the finding that HB-EGF reduced basal or TGF-β1-stimulated α-SMA expression in the human MRC-5 fibroblast cell line (31). Thus, spatiotemporal HB-EGF gene regulation and protein production may be very critical to restoration of normal liver structure and function after liver injury, as shown in other organ systems (31, 32).
Of interest were the findings that basal or TAA-induced CCN2 expression was higher in livers from HB-EGF−/− mice as compared to those from HB-EGF+/+ mice, and that CCN2 expression was significantly greater in HB-EGF−/− HSC as compared to HB-EGF+/+ HSC during culture-induced activation of the cells. These data show that endogenous HB-EGF production is coupled to CCN2 production in HSC. This is further supported by the correlation in expression between HB-EGF and CCN2 during culture-induced activation including a reproducible but as yet unexplained decrease in expression for both molecules on Day 4 (see Fig 4A, B). Over this same time-frame, α- SMA or collagen expression continued to rise (Fig 4C, D) suggesting that certain time-points during HSC activation or fibrogenesis may be less dependent on CCN2 than others. This notion is consistent with previous studies in human fibroblasts which documented both CCN2-dependent and –independent mechanisms of collagen expression (33, 34) as well as the recognition that CCN2 functions in a highly complex and contextual manner to drive fibrogenic pathways (35, 36).
Whereas CCN2 was dependent on endogenous HB-EGF, exogenously added HB-EGF on the other hand did not regulate CCN2 production even though it was effective in inhibiting α-SMA or collagen expression. These results suggest either that HB-EGF-mediated CCN2 suppression in HSC changes in accordance with, but does not cause, concomitant suppression in α-SMA or collagen expression, or that the distinct actions of exogenous versus endogenous HB-EGF in suppression of CCN2 expression point to fundamentally discrete signaling pathways for each form of HB-EGF. Indeed the ability of endogenous membrane bound proHB-EGF to bind and activate signal-transducing receptors on adjacent cells in a juxtracrine fashion has been well documented and is distinct from the actions of the soluble form of HB-EGF. Since, in our studies, exogenous sHB-EGF inhibited endogenous HB-EGF gene expression in HB-EGF+/+ HSC, CCN2 production may be more directly regulated by endogenous HB-EGF than exogenous HB-EGF. Hence, while the precise mechanisms underlying HB-EGF action and CCN2 production have yet to be elucidated, our data are supportive of differential signaling and functions of sHB-EGF and proHB-EGF in HSC, as is apparent in other cell types (7, 37–40). A similar explanation may underlie the relatively small (but significant) difference in α-SMA expression between HB-EGF+/+ HSC versus HB-EGF−/− HSC over the first 5 days of culture as compared to the pronounced effects of exogenous HB-EGF on α-SMA expression in HB-EGF+/+ HSC. Thus, the role of HB-EGF in fibrosis is multi-faceted and involves complex mechanisms that require further investigation.
We have previously shown that CCN2 production in HSC is stimulated by endogenous TGF-β (41, 42). While this stimulatory role has largely been attributed to direct effects of TGF-β on the CCN2 promoter (42), it is also possible that TGF-β in part exerts a suppressive effect on HB-EGF expression causing a similar enhancement in CCN2 levels as seen in HB-EGF−/− mice. Indeed, evidence for TGF-β -mediated suppression of HB-EGF expression was obtained in this study (albeit in hepatocytes) and future studies will need to address the HB-EGF-TGF-β axis in HSC in detail. Also, in HB-EGF−/− mice or HSC, the lack of activation or stimulation of downstream targets of HB-EGF rather than HB-EGF itself may account for all or some of the differential responses as compared to HB-EGF+/+ mice or HSC, a possibility to be addressed in follow-up studies.
Recent reports showed that over-expression of HB-EGF in pancreatic islets led to intra-islet fibrosis (9, 10). Further studies are needed to explain the pro-fibrotic role of HB-EGF in the pancreas versus its anti-fibrotic action in the liver but this difference may reflect the use of distinct genetic models (transgenic versus knockout), the presence (liver) or absence (pancreas) of a noxious insult (e.g. CCl4), and/or distinct modes of injury or repair in the liver versus the pancreas, including functional differences between the stellate cells in each organ systems (43–45).
Like HB-EGF, AR contains an N-terminal heparin-binding domain which functionally engages heparan sulfate proteoglycans on the cell surface or in extracellular matrix. Chronic administration of CCl4 induced less liver fibrosis in AR-knockout mice than in wild type mice (46). Additionally, AR-knockout mice showed impaired proliferative responses after partial liver hepatectomy (5), exhibited signs of chronic liver damage in the absence of any noxious treatment, and died faster than wild type mice in response to lethal doses of Fas-agonist antibody (4347). Collectively, these data show that HB-EGF and AR are functionally distinct despite their structural similarity and that the actions of these EGF family members after liver injury are complex, multi-faceted, and non-redundant.
In summary, the present studies indicate that HB-EGF gene knockout in mice increases susceptibility to hepatic fibrosis in response to chronic TAA-induced liver injury and that HB-EGF expression or action is associated with suppression of fibrogenic pathways in HSC. The present studies reveal a novel role of HB-EGF in HSC function and liver fibrosis, and suggest that manipulation of HB-EGF production or action may have therapeutic value for limiting hepatic fibrosis.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Dr. David Lee (Chapel Hill, NC, USA) for supplying HB-EGF KO and WT mice, and Yan Chen and Amanda Darbyshire for mouse breeding and genotyping.
Funding: This work was supported by NIH grants R01 AA016003 (to D.R.B.) and R01 GM61193 and R01 DK074611 (to G.E.B.).
Abbreviations
- α-SMA
alpha-smooth muscle actin
- AR
amphiregulin
- CCl4
carbon tetrachloride
- CCN2
connective tissue growth factor, also known as CTGF
- COL1A1
α1 chain of collagen I
- COL3A1
α1 chain of collagen III
- DMEM
Dulbecco’s minimum essential medium
- EGF
epidermal growth factor
- HB-EGF
Heparin-binding epidermal growth factor (EGF)-like growth factor
- HSC
hepatic stellate cells
- ITS
insulin-transferrin sodium selenite solution
- PBS
phosphate-buffered saline
- PCR
Polymerase chain reaction
- pro-HB-EGF
HB-EGF precursor protein
- sHB-EGF
soluble HB-EGF
- TGF-α
transforming growth factor alpha
- TGF-β1
transforming growth factor beta1
Footnotes
DISCLOSURE/CONFLICT OF INTEREST
No.
Supplementary information is available at Laboratory Investigation's website.
REFERENCES
- 1.Abraham JA, Damm D, Bajardi A, Miller J, Klagsbrun M, Ezekowitz RA. Heparin-binding EGF-like growth factor: characterization of rat and mouse cDNA clones, protein domain conservation across species, and transcript expression in tissues. Biochem Biophys Res Commun. 1993;190(1):125–133. doi: 10.1006/bbrc.1993.1020. [DOI] [PubMed] [Google Scholar]
- 2.Miyamoto S, Yagi H, Yotsumoto F, Kawarabayashi T, Mekada E. Heparin-binding epidermal growth factor-like growth factor as a new target molecule for cancer therapy. Adv Exp Med Biol. 2008;622:281–295. doi: 10.1007/978-0-387-68969-2_23. [DOI] [PubMed] [Google Scholar]
- 3.Iwamoto R, Yamazaki S, Asakura M, et al. Heparin-binding EGF-like growth factor and ErbB signaling is essential for heart function. Proc Natl Acad Sci U S A. 2003;100(6):3221–3226. doi: 10.1073/pnas.0537588100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson LF, Qiu TH, Sunnarborg SW, et al. Defective valvulogenesis in HB-EGF and TACE-null mice is associated with aberrant BMP signaling. EMBO J. 2003;22(11):2704–2716. doi: 10.1093/emboj/cdg264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miyamoto S, Fukami T, Yagi H, Kuroki M, Yotsumoto F. Potential for molecularly targeted therapy against epidermal growth factor receptor ligands. Anticancer Res. 2009;29(3):823–830. [PubMed] [Google Scholar]
- 6.Nishi E, Klagsbrun M. Heparin-binding epidermal growth factor-like growth factor (HB-EGF) is a mediator of multiple physiological and pathological pathways. Growth Factors. 2004;22(4):253–260. doi: 10.1080/08977190400008448. [DOI] [PubMed] [Google Scholar]
- 7.Higashiyama S, Iwabuki H, Morimoto C, Hieda M, Inoue H, Matsushita N. Membrane-anchored growth factors, the epidermal growth factor family: beyond receptor ligands. Cancer Sci. 2008;99(2):214–220. doi: 10.1111/j.1349-7006.2007.00676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shirakata Y, Kimura R, Nanba D, et al. Heparin-binding EGF-like growth factor accelerates keratinocyte migration and skin wound healing. J Cell Sci. 2005;118(Pt 11):2363–2370. doi: 10.1242/jcs.02346. [DOI] [PubMed] [Google Scholar]
- 9.Blaine SA, Ray KC, Branch KM, Robinson PS, Whitehead RH, Means AL. Epidermal growth factor receptor regulates pancreatic fibrosis. Am J Physiol Gastrointest Liver Physiol. 2009;297(3):G434–G441. doi: 10.1152/ajpgi.00152.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Means AL, Ray KC, Singh AB, et al. Overexpression of heparin-binding EGF-like growth factor in mouse pancreas results in fibrosis and epithelial metaplasia. Gastroenterology. 2003;124(4):1020–1036. doi: 10.1053/gast.2003.50150. [DOI] [PubMed] [Google Scholar]
- 11.Kiso S, Kawata S, Tamura S, et al. Liver regeneration in heparin-binding EGF-like growth factor transgenic mice after partial hepatectomy. Gastroenterology. 2003;124(3):701–707. doi: 10.1053/gast.2003.50097. [DOI] [PubMed] [Google Scholar]
- 12.Kiso S, Kawata S, Tamura S, et al. Expression of heparin-binding EGF-like growth factor in rat liver injured by carbon tetrachloride or D-galactosamine. Biochem Biophys Res Commun. 1996;220(2):285–288. doi: 10.1006/bbrc.1996.0397. [DOI] [PubMed] [Google Scholar]
- 13.Webber EM, FitzGerald MJ, Brown PI, Bartlett MH, Fausto N. Transforming growth factor-α expression during liver regeneration after partial hepatectomy and toxic injury, and potential interactions between transforming growth factor-α and hepatocyte growth factor. Hepatology. 1993;18(6):1422–1431. [PubMed] [Google Scholar]
- 14.Kiso S, Kawata S, Tamura S, et al. Expression of heparin-binding epidermal growth factor-like growth factor in the hepatocytes of fibrotic rat liver during hepatocarcinogenesis. J Gastroenterol Hepatol. 1999;14(12):1203–1209. doi: 10.1046/j.1440-1746.1999.02007.x. [DOI] [PubMed] [Google Scholar]
- 15.Friedman SL. Stellate cells: a moving target in hepatic fibrogenesis. Hepatology. 2004;40(5):1041–1043. doi: 10.1002/hep.20476. [DOI] [PubMed] [Google Scholar]
- 16.Friedman SL. Mechanisms of hepatic fibrogenesis. Gastroenterology. 2008;134(6):1655–1669. doi: 10.1053/j.gastro.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang G, Brigstock DR. Integrin expression and function in the response of primary culture hepatic stellate cells to connective tissue growth factor (CCN2) J Cell Mol Med. 2011;15(5):1087–1095. doi: 10.1111/j.1582-4934.2010.01072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iredale J. Defining therapeutic targets for liver fibrosis: exploiting the biology of inflammation and repair. Pharmacol Res. 2008;58(2):129–136. doi: 10.1016/j.phrs.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 19.Rachfal AW, Brigstock DR. Connective tissue growth factor (CTGF/CCN2) in hepatic fibrosis. Hepatol Res. 2003;26(1):1–9. doi: 10.1016/s1386-6346(03)00115-3. [DOI] [PubMed] [Google Scholar]
- 20.Reeves HL, Friedman SL. Activation of hepatic stellate cells--a key issue in liver fibrosis. Front Biosci. 2002;7:d808–d826. doi: 10.2741/reeves. [DOI] [PubMed] [Google Scholar]
- 21.Shi-Wen X, Leask A, Abraham D. Regulation and function of connective tissue growth factor/CCN2 in tissue repair, scarring and fibrosis. Cytokine Growth Factor Rev. 2008;19(2):133–144. doi: 10.1016/j.cytogfr.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 22.Davis KM, Brigstock DR, Johnson PR, et al. Production of glycosylated heparin-binding EGF-like growth factor in HeLa cells using vaccinia virus. Protein Expr Purif. 1996;8(1):57–67. doi: 10.1006/prep.1996.0074. [DOI] [PubMed] [Google Scholar]
- 23.Stoehr SA, Isom HC. Gap junction-mediated intercellular communication in a long-term primary mouse hepatocyte culture system. Hepatology. 2003;38(5):1125–1135. doi: 10.1053/jhep.2003.50418. [DOI] [PubMed] [Google Scholar]
- 24.Kiso S, Kawata S, Tamura S, et al. Role of heparin-binding epidermal growth factor-like growth factor as a hepatotrophic factor in rat liver regeneration after partial hepatectomy. Hepatology. 1995;22(5):1584–1590. [PubMed] [Google Scholar]
- 25.Sakuda S, Tamura S, Yamada A, et al. NF-κB activation in non-parenchymal liver cells after partial hepatectomy in rats: possible involvement in expression of heparin-binding epidermal growth factor-like growth factor. J Hepatol. 2002;36(4):527–533. doi: 10.1016/s0168-8278(01)00310-5. [DOI] [PubMed] [Google Scholar]
- 26.Besner G, Higashiyama S, Klagsbrun M. Isolation and characterization of a macrophage-derived heparin-binding growth factor. Cell Regul. 1990;1(11):811–819. doi: 10.1091/mbc.1.11.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davis-Fleischer KM, Besner GE. Structure and function of heparin-binding EGF-like growth factor (HB-EGF) Front Biosci. 1998;3:d288–d299. doi: 10.2741/a241. [DOI] [PubMed] [Google Scholar]
- 28.Higashiyama S, Abraham JA, Miller J, Fiddes JC, Klagsbrun M. A heparin-binding growth factor secreted by macrophage-like cells that is related to EGF. Science. 1991;251(4996):936–939. doi: 10.1126/science.1840698. [DOI] [PubMed] [Google Scholar]
- 29.El-Assal ON, Besner GE. Heparin-binding epidermal growth factor-like growth factor and intestinal ischemia-reperfusion injury. Semin Pediatr Surg. 2004;13(1):2–10. doi: 10.1053/j.sempedsurg.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 30.Ito Y, Takeda T, Higashiyama S, et al. Expression of heparin binding epidermal growth factor-like growth factor in hepatocellular carcinoma: an immunohistochemical study. Oncol Rep. 2001;8(4):903–907. doi: 10.3892/or.8.4.903. [DOI] [PubMed] [Google Scholar]
- 31.Kirkland G, Paizis K, Wu LL, Katerelos M, Power DA. Heparin-binding EGF-like growth factor mRNA is upregulated in the peri-infarct region of the remnant kidney model: in vitro evidence suggests a regulatory role in myofibroblast transformation. J Am Soc Nephrol. 1998;9(8):1464–1473. doi: 10.1681/ASN.V981464. [DOI] [PubMed] [Google Scholar]
- 32.Marikovsky M, Breuing K, Liu PY, et al. Appearance of heparin-binding EGF-like growth factor in wound fluid as a response to injury. Proc Natl Acad Sci U S A. 1993;90(9):3889–3893. doi: 10.1073/pnas.90.9.3889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ricupero DA, Rishikof DC, Kuang PP, Poliks CF, Goldstein RH. Regulation of connective tissue growth factor expression by prostaglandin E2. Am J Physiol. 1999;277(Pt 1):L1165–L1171. doi: 10.1152/ajplung.1999.277.6.L1165. [DOI] [PubMed] [Google Scholar]
- 34.Ricupero DA, Romero JR, Rishikof DC, Goldstein RH. Des-Arg10-kallidin engagement of the B1 receptor stimulates type I collagen synthesis via stabilization of connective tissue growth factor mRNA. J Biol Chem. 2000;275(17):12475–12480. doi: 10.1074/jbc.275.17.12475. [DOI] [PubMed] [Google Scholar]
- 35.Brigstock DR. Connective tissue growth factor (CCN2, CTGF) and organ fibrosis: lessons from transgenic animals. J Cell Commun Signal. 2010;4(1):1–4. doi: 10.1007/s12079-009-0071-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cicha I, Goppelt-Struebe M. Connective tissue growth factor: context-dependent functions and mechanisms of regulation. Biofactors. 2009;35(2):200–208. doi: 10.1002/biof.30. [DOI] [PubMed] [Google Scholar]
- 37.Higashiyama S. Metalloproteinase-mediated shedding of heparin-binding EGF-like growth factor and its pathophysiological roles. Protein Pept Lett. 2004;11(5):443–450. doi: 10.2174/0929866043406562. [DOI] [PubMed] [Google Scholar]
- 38.Higashiyama S, Nanba D. ADAM-mediated ectodomain shedding of HB-EGF in receptor cross-talk. Biochim Biophys Acta. 2005;1751(1):110–117. doi: 10.1016/j.bbapap.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 39.Iwamoto R, Mekada E. Heparin-binding EGF-like growth factor: a juxtacrine growth factor. Cytokine Growth Factor Rev. 2000;11(4):335–344. doi: 10.1016/s1359-6101(00)00013-7. [DOI] [PubMed] [Google Scholar]
- 40.Miyamoto S, Hirata M, Yamazaki A, et al. Heparin-binding EGF-like growth factor is a promising target for ovarian cancer therapy. Cancer Res. 2004;64(16):5720–5727. doi: 10.1158/0008-5472.CAN-04-0811. [DOI] [PubMed] [Google Scholar]
- 41.Chen L, Charrier AL, Leask A, French SW, Brigstock DR. Ethanol-stimulated differentiated functions of human or mouse hepatic stellate cells are mediated by connective tissue growth factor. J Hepatol. 2011;55(2):399–406. doi: 10.1016/j.jhep.2010.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leask A, Chen S, Pala D, Brigstock DR. Regulation of CCN2 mRNA expression and promoter activity in activated hepatic stellate cells. J Cell Commun Signal. 2008;2(12):49–56. doi: 10.1007/s12079-008-0029-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buchholz M, Kestler HA, Holzmann K, et al. Transcriptome analysis of human hepatic and pancreatic stellate cells: organ-specific variations of a common transcriptional phenotype. J Mol Med. 2005;83(10):795–805. doi: 10.1007/s00109-005-0680-2. [DOI] [PubMed] [Google Scholar]
- 44.Erkan M, Weis N, Pan Z, et al. Organ-, inflammation- and cancer specific transcriptional fingerprints of pancreatic and hepatic stellate cells. Mol Cancer. 2010;9(1):88. doi: 10.1186/1476-4598-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhao L, Burt AD. The diffuse stellate cell system. J Mol Histol. 2007;38(1):53–64. doi: 10.1007/s10735-007-9078-5. [DOI] [PubMed] [Google Scholar]
- 46.Perugorria MJ, Latasa MU, Nicou A, et al. The epidermal growth factor receptor ligand amphiregulin participates in the development of mouse liver fibrosis. Hepatology. 2008;48(4):1251–1261. doi: 10.1002/hep.22437. [DOI] [PubMed] [Google Scholar]
- 47.Berasain C, Garcia-Trevijano ER, Castillo J, et al. Novel role for amphiregulin in protection from liver injury. J Biol Chem. 2005;280(19):19012–19020. doi: 10.1074/jbc.M413344200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.