Abstract
This paper investigates one explanation for the consistent observation of a strong, negative correlation in the United States between income and obesity among women, but not men. We argue that a key factor is the gendered expectation that mothers are responsible for feeding their children. When income is limited and households face food shortages, we predict that an enactment of these gendered norms places mothers at greater risk for obesity relative to child-free women and all men. We adopt an indirect approach to study these complex dynamics using data on men and women of child-rearing age and who are household heads or partners in the 1999–2003 waves of the Panel Study of Income Dynamics (PSID). We find support for our prediction: Food insecure mothers are more likely than child-free men and women and food insecure fathers to be overweight or obese and to gain more weight over four years. The risks are greater for single mothers relative to mothers in married or cohabiting relationships. Supplemental models demonstrate that this pattern cannot be attributed to post-pregnancy biological changes that predispose mothers to weight gain or an evolutionary bias toward biological children. Further, results are unchanged with the inclusion of physical activity, smoking, drinking, receipt of food stamps, or Women, Infants and Children (WIC) nutritional program participation. Obesity, thus, offers a physical expression of the vulnerabilities that arise from the intersection of gendered childcare expectations and poverty.
Keywords: overweight, obesity, gender, food insecurity, parenting, income, USA
Scholars argue that it takes money to maintain a healthy weight in America’s obesogenic environment (Poston & Foreyt, 1999) because healthy food is relatively expensive and calorie-dense, nutrient-poor food is cheap (Drewnowski & Specter, 2004). Although weight is a function of both caloric intake and expenditure, materialist arguments focus on the costs of food and predict greater caloric intake and consequent body fat among low versus high income people (Glass & McAtee, 2006). In the U.S., there is a strong, negative correlation between income the likelihood of being overweight or obese, but only among women; this is not observed among men (for reviews, see McLaren, 2007; Sobal & Stunkard, 1989). This sex difference is puzzling, particularly to scholars who look beyond individual explanations to consider the role of shared environments for health because the majority of men and women live together (Casper & Bianchi, 2002) and share socioeconomic resources and weight-related behaviors (French et al., 2001; Mitchell et al., 2003). Given these commonalities, one would expect greater similarity between the sexes.
We hypothesize that the key distinction is not between all women and all men, but between mothers and non-mothers. We argue that the confluence of two factors – the experience of food insecurity and the gendered nature of childcare – intersect and contribute to the observed sex differences in the association of income and body weight. Food insecurity is highly correlated with poverty (Sarlio-Lähteenkorva & Lahelma, 2001) and occurs when a household faces budgetary constraints that limit the quantity or quality of food they can purchase (Wunderlich & Norwood, 2006). Yet food insecurity is a “managed process” (Radimer, 1990), meaning that families strategize and diligently work to avoid hunger. That responsibility, however, falls more heavily on women given traditional discourses about family life and “women’s work” that place greater expectations on women for feeding and nurturing their family, especially when children are present (DeVault, 1991). Given that food insecurity is correlated with poor dietary behavior and obesity (for a review, see Institute of Medicine, 2011), we assert that food insecurity mediates the association between income and weight, but that the management of food insecurity intersects with gender to create differential risks for obesity between mothers and non-mothers.
To investigate these dynamics, we study men and women of child rearing ages (i.e., 18 to 55) who are heads or partners of U.S. households in the 1999, 2001 and 2003 waves of the Panel Study of Income Dynamics (PSID). We test whether the association between household food insecurity and the likelihood of being overweight or obese differs across groups defined by sex and parenthood in cross-sectional models of weight status and longitudinal models of weight change. We also examine how partner co-residence further moderates these processes due to the gendered norms about parental custody (Coltrane & Adams, 2003) and the greater prevalence of food insecurity among single parents (Rose et al., 1998).
FOOD INSECURITY AND WEIGHT
Household food security exists along a continuum but can be categorized into a four-point ordered scale: food secure, food insufficiency, low food security, and very low food security (Bickel et al., 2000; Wunderlich & Norwood, 2006). Most Americans are food secure, but some face food insufficiency, meaning, they worry about having enough money to buy food for the month, but actually make no or few changes to their diet (Wunderlich & Norwood, 2006). Food insecurity occurs when those fears become a reality. Low food security, or not having the means to buy the kinds of food desired, reduces the quality and variety of people’s diets (Wunderlich & Norwood, 2006). Very low food security occurs when people do not have the means to buy the quantity of food needed and leads people to skip meals and reduce their food intake (Wunderlich & Norwood, 2006). Those with either “low food security” or “very low food security” are considered “food insecure” (Wunderlich & Norwood, 2006). In 2009, 14.7% of U.S. households were food insecure (Nord et al., 2010), while in 2003, the year corresponding to our study, the prevalence was 11.2% (Nord et al., 2004).
Because poverty predicts food insecurity (Sarlio-Lähteenkorva & Lahelma, 2001), there are several parallels found in research on the role of food security for body weight. Key among them are consistent sex differences, such that low food security is linked to being overweight (Adams et al., 2003; Dinour et al., 2007; Lyons et al., 2008; Townsend et al., 2001) and gaining 5 pounds or more in one year (Wilde & Peterman, 2006), but only among women. Very low food security is associated with being underweight, but again only for women (Wilde & Peterman, 2006).
Several studies suggest that food insecurity is linked to overweight and obesity due to management strategies people adopt in the face of economic constraints. Food insecure individuals are more likely to consume high-calorie but nutritionally-poor food to avoid feelings of hunger (Dixon et al., 2001; Drewnowski & Specter, 2004; Kirkpatrick & Tarasuk, 2008), eat irregular meals or skip breakfast (Kempson et al., 2002; Ma et al., 2003), and consume less milk, fruit and vegetables, especially later in the month (Tarasuk et al., 2007). According to public health and nutrition research, these dietary practices are associated with being overweight (Ledikwe et al., 2006; Ma et al., 2003) and weight gain (Berkey et al., 2003). In the next section, we detail how the management of food insecurity is gendered.
GENDER, CHILDCARE, AND FOOD INSECURITY MANAGEMENT
Traditional discourses about “family” life and “women’s work” since the industrial revolution include expectations that women are responsible for caring for their family members and managing household tasks (Rothman, 1978; Sokoloff, 1980). When children are present in the home, those responsibilities multiply (Hays, 1998) and the gendered division of household labor becomes more unequal (Coltrane, 2000). For example, there is greater gender equity in the total number of hours spent on housework in child-free cohabiting and married couples than among similar couples with children (Sanchez & Thomson, 1997; South & Spitze, 1994). Therefore, mothers are more likely to be subjected to, internalize, and reflect traditional gender expectations about their roles and responsibilities than child-free women.
A key feminine responsibility is “feeding the family,” which requires a series of tasks: meal planning, monitoring the supply of household provisions, shopping, cooking, and cleaning (DeVault, 1991). Beyond the practical goals, “feeding the family” also sustains children’s emotional needs for love, support and security (DeVault, 1991).
In food insecure homes, mothers work hard to prevent hunger amongst their children. In a qualitative study with frequently food insecure young mothers, all insisted that their children only experienced food insufficiency because they adopted several strategies to protect them (Stevens, 2010), including prioritizing their children’s needs over their own (McIntyre et al., 2003; Stevens, 2010). As DeVault notes “[t]hese women seem to be expressing a heightened sense of the more widespread notion that’s women’s own food is less important than that prepared for others” (1991, p. 199). As one woman in a cash-strapped household noted: “If it gets down to it, we buy to feed the kids” (DeVault, 1991, p. 191).
To manage food insecurity, mothers adopt a variety of strategies. Some strategies focus on grocery shopping, like buying in bulk, shopping at different stores to get the best prices, or using coupons (DeVault, 1991; Wiig & Smith, 2008). Other strategies involve mothers’ food intake. Food insecure mothers skip meals, wait to eat until later in the day, or eat less to spare their children from hunger and nutritional deprivation (Badun et al., 1995; DeVault, 1991; McIntyre et al., 2000; McIntyre et al., 2003). As a result, women in food insecure households are at risk of nutrient deficiencies in Vitamin A, folate, iron, and magnesium (Tarasuk & Beaton, 1999). We suspect that these behavioral patterns undergird the unexplained sex differences in the association between food insecurity and weight (Adams et al., 2003; Dinour et al., 2007; Lyons et al., 2008; Olson, 1999; Townsend et al., 2001; Wilde & Peterman, 2006) and why food insecurity is typically not correlated with children’s weight (Gundersen et al., 2009; Martin & Ferris, 2007), but for an exception see Gundersen and Kreider (2009). Unfortunately we do not have direct measures on people’s dietary behavior or food insecurity management practices to fully explore this sequence, but we do have the requisite data to test our primary hypothesis:
H1: There is a statistically significant association between food insecurity and being overweight or obese for mothers, but not child-free women or all men.
We know of only one paper about food insecurity and obesity that emphasizes parenthood. With a sample of parents (65% of whom were single mothers), Martin and Ferris (2007) found a positive association between food insecurity and obesity, but they did not explore whether there was a differential association between mothers and fathers. Therefore, the current analysis makes a significant contribution by offering an initial test of this hypothesis.
THE ROLE OF MARRIAGE AND COHABITATION
We predict that the living arrangements of heterosexual men and women further condition the differences between mothers and non-mothers. Prior research demonstrates that caretaking duties among separated parents are largely performed by the custodial parent, typically the mother (Furstenberg & Cherlin, 1994; Marsiglio et al., 2000). Therefore, the risks of overweight due to food insecurity should be exacerbated among single mothers and relatively lower for mothers in co-residential couple households. Likewise, single fathers should be at greater risk of obesity when they are food insecure. Unfortunately, we have too few single fathers in our data to fully explore this possibility because most single parents are single mothers (Casper & Bianchi, 2002), reflecting a “community division of labor” (DeVault, 1991, p. 193) whereby women routinely have custody after parents separate. Our second hypothesis is:
H2: The association between food insecurity and being overweight or obese is stronger for single mothers versus married or cohabiting mothers.
It is important to note, however, that the causal relationships between overweight, family formation, union dissolution, and household food security are complex. In fact, the causal process could work in the opposite direction: Overweight women may be less likely to form unions and bear children given feminine beauty ideals emphasizing thinness (Allon, 1982).
ALTERNATIVE EXPLANATIONS
We predict that food insecurity and its management increases the risks of overweight and obesity for mothers given the gendered expectations of childrearing. We recognize, however, that there are competing explanations and we do our best to address them.
First, one may agree with our prediction but disagree with our interpretation. One may consider any observed risks for mothers as reflecting, not childrearing, but biological risks of childbearing. If metabolic changes related to pregnancy predispose birth mothers to gain weight, then food insecure biological mothers would be at greater risk of overweight and obesity than “social” mothers. Such differences could also arise if, due to evolutionary pressures, mothers are more protective of their biological children (Daly & Wilson, 1980). To test whether the experience of pregnancy or biological kinship creates unique risks, we conduct two supplemental analyses. First, we restrict our sample to only women living with children (50% of the sample) and compare whether the risk of obesity for food insecure mothers is lower among women living with children they did not give birth to (i.e., they are adoptive, step, or foster mothers), controlling for the number of children present. Because most women live only with biological children, statistical power issues may limit our ability to detect a significant difference. Second, we restrict our sample to women who have ever given birth by 2003 and examine whether the risks of household food insecurity increase as parity increases, regardless of whether their children currently live with her and controlling for her age and other demographic characteristics. Because 89% of the women in our sample have given birth by 2003, power is less of a problem in these analyses. If metabolic changes associated with pregnancy undergird our findings, then one would expect those risks to accumulate with each birth and, thus, translate into a statistically significant interaction between parity and food insecurity among biological mothers.
Second, one might argue that the statistical association between food insecurity and overweight is a function of other sociodemographic factors besides income. Thus, we control for status characteristics, like age, education and race/ethnicity in all models.
Third, one might expect that other mediating factors explain these patterns, especially given that we do not have self-reported measures of energy intake or, even better, data from doubly-labeled water tests to measure their energy intake (Schoeller, 1990). We test several alternative mechanisms. Because food insecure mothers may have fewer opportunities for recreational physical activity, we test whether differences in self-reported physical activity reduce the association between food insecurity and weight among mothers. We also test whether the consumption of alcohol or smoking cigarettes explains the observed patterns. Because of the stresses associated with poverty and food insecurity (Huddleston-Casas et al., 2009), which would likely feel more threatening to parents, food insecure parents could be more likely to self-soothe themselves with alcohol and nicotine. Yet these behaviors are associated with weight status (Mokdad et al., 2003; Slattery et al., 1992). Lastly, given the longstanding debate about whether receiving food stamps (now officially the Supplemental Nutrition Assistance Program) increases the risks for overweight and obesity (Borjas, 2004; Gibson, 2003; Institute of Medicine, 2011), we test whether our results change with the inclusion of food stamps receipt. We also include a measure of participation in the Women, Infants and Children (WIC) nutritional program.
In sum, we bridge several empirical literatures to develop a new theoretical model about how gendered patterns of childcare intersect with household economics to increase the risk of overweight among poor, food insecure mothers. We recognize that there are several alternative explanations and, thus, do our best to test them with the available data. Our aim is to provide an initial examination of whether overweight and obesity are physical expressions of the vulnerabilities that arise from the intersection of gender, parenthood, and poverty.
DATA AND METHODS
Data
We use data from the Panel Study of Income Dynamics (PSID) because it is the only study that collects data on individuals’ weight, income, household food insecurity, and household composition. Unfortunately, PSID does not have information about individual’s energy intake and food insecurity management.
PSID is a longitudinal household-based study that began collecting data in 1968 for a nationally representative sample and an oversample of low-income, Southern households (Hill, 1992). The PSID contains longitudinal data for all individuals who were ever in a PSID household, even if they move out (Hill, 1992). Interviews since 1997 are conducted biennially. Given that the PSID has been fielded for almost 50 years, sample attrition could pose a problem, but several studies have found that attrition has not affected PSID’s representativeness (Becketti et al., 1988; Fitzgerald et al., 1998). PSID is not representative, however, of immigrant groups arriving in the U.S. after 1968.
We make several restrictions to arrive at our analytic sample. First, we must rely on data collected in 1999, 2001, and 2003, the years in which PSID collected data on both weight and food insecurity. Second, we restrict our analysis to those who were either the head of a PSID household or their marital or cohabiting partner in 1999, 2001, and 2003 (n = 9,935) because PSID only collects data on body weight for those individuals. While this provides for a consistent sample across the various models, it makes the sample more selective with regard to family structure stability. Our substantive findings are unchanged, however, in analyses where the data are multiply imputed to include anyone who meets the restrictions listed below and was ever in the PSID between 1999 and 2003, regardless of their relationship to the household head. Third, we restrict the analysis to heads and partners between the ages of 18 and 55 in 1999 (n = 8,151) to focus on adults most at risk for living with minor children and, thus, the hypothesized patterns. The next two restrictions eliminate outlier cases that would challenge the statistical homogeneity of our analysis. Fourth, we drop those who report being foreign born (n = 82) or who can be reasonably assumed to be foreign born because they have five or fewer years of completed schooling (and the minimum age of compulsory schooling in the United States is 16) (n = 51). These individuals are unique in both unobserved and observed ways (i.e., their means and correlations for food insecurity, number of children, marital status and weight differ significantly) because the PSID is not representative of immigrants. The absence of immigrants reduces the prevalence of food insecurity in the study (Borjas, 2004). Fifth, we omit women who are pregnant at the time of the 2003 interview (n=85). Specifically, we omit women reporting a live birth in the PSID’s Childbirth and Adoption History File within 9 months following their 2003 interview date. After these restrictions, our sample is 7,931 adults.
Missing data due to item non-response is relatively minor in these data. There are actually no missing data for people’s sex, age, partnership status, the number of co-residential children, urbanicity, and household income (because the PSID has imputed it). There is minor item non-response on food insecurity (n1999 = 9, n2001 = 11, n2003 = 20), self-rated health (n2003 = 86), race (n = 129), and women’s fertility histories (n = 36). The items with the most missing data are body mass index (n1999 = 379 [4% of the original 9,935 sample], n2001 = 257 [3%], n2003 = 305 [3%]) and education (n2003 = 596 [6%]). We utilize multiple imputation handle item non-response, which replaces missing values with predictions from information observed in the sample (Rubin, 1987). We use the supplemental program “ice” within STATA 11.0 (Royston, 2005a, b) to create five imputed data sets. The imputation models include all of the variables and their interactions that are used in the empirical models, as well as the respondent’s work status, occupation, and region (all in 2003), the number of adults in the household (in 1999, 2001, 2003), whether they live with a young child (ages 0–5; in 2003) and whether PSID imputed their income. We estimate the empirical models for each imputed data set and then combine the results, accounting for the variance within and between the imputed samples to calculate the coefficients’ standard errors (Rubin, 1987).
Measures
Body Weight
We determine people’s weight classification in three steps. First, because PSID only has self-reported weight and because self-reported weight is generally biased downward among women and upward among men (Cawley & Burkhauser, 2006), we use the Cawley (2004; Cawley & Burkhauser, 2006) adjustments to improve the accuracy of our dependent variable. Specifically, we multiply respondents’ self-reported weight by race- and sex-specific coefficients from Cawley’s regressions of measured weight on self-reported weight. Second, we calculate their body mass index (BMI) [weight (kg)/height2 (m2)] from their self-reported height and their Cawley-adjusted self-reported weight. Third, we follow World Health Organization (2000) guidelines to classify BMI into the following weight categories: underweight (BMI < 18.5), normal weight (18.5 ≤ BMI < 25), overweight (25 ≤ BMI < 30) and obese (BMI ≥ 30). In the cross-sectional models, we predict whether a person is (1) normal weight or underweight, (2) overweight, or (3) obese in 2003. Because less than 2% of the sample is underweight, we cannot model underweight as a separate category. For the longitudinal models, we predict their weight change (in pounds) between 1999 and 2003, simply calculated as their Cawley-adjusted 2003 weight minus their Cawley-adjusted 1999 weight.
Household Food Insecurity
We use the U.S. Department of Agriculture’s Food Security Scale (Bickel et al., 2000). Respondents were asked a sequential series of 18 questions if they live with children and 10 questions if they do not. The different series are made equivalent (and thus orthogonal to the presence of children) in the final 10-point scale and categorical measure of food security. Following the USDA’s guidelines, households are classified as food insecure (=1) if they score a 2.2 or higher on the Food Security Scale (Bickel et al., 2000). We measure their household food insecurity in 2003 and create a longitudinal measure that counts the survey years with reported household food insecurity between 1999 and 2003 (values: 0, 1, 2, or 3).
Sex
Sex is a dichotomous indicator for whether the person is female (1 = yes) or male.
Children
PSID participants report the number of children between the ages of zero and 17 years currently in the household, regardless of their biological relationship to the household head or their partner. We create a dichotomous measure indicating children are present (=1) and a count of children present.
We use the PSID’s Childbirth and Adoption History (1985–2007) data to create two variables. First, among those living with children in 2003, we determine whether the woman gave birth to every child present and create a dichotomous variable equal to one if she did not. Because very few women live with a mix of biological and non-biological children (N = 14), the results primarily reflect whether women who did not give birth to any of the children present (N = 307) are different. Second, we calculate the total number of children a woman has ever borne.
In the longitudinal models, we use a variable that equals the difference between the number of children present in 2003 and 1999.
Partner co-residence
To compare adults in different residential relationships, we estimate models separately for those who are single and those who are who are living with a romantic partner, whether married or cohabiting.
Alternative mediating variables
Supplemental models include the following variables, reported in 2003: being a “current smoker” (=1), the number of alcoholic drinks consumed per day (0= none, 1= less than one a day, 2= 1 to 2 per day, 3= 3 to 4 a day, and 4= 5 or more a day), bouts of “heavy” physical activity during the last month (PSID-provided examples include aerobics, running, swimming, strenuous housework), bouts of “light” physical activity during the last month (PSID-provided examples include walking, golfing, gardening, bowling), receipt of food stamps in 2001 (=1), and receipt of WIC in 2002 (=1)
Control variables
To control for confounding variables, we include age (in years), education (in years of completed schooling), poor self-rated health (0 = “good,” “very good,” or “excellent,” 1 = “poor” or “fair”), disability status (1 = at least one limitation in the Activities of Daily Living Scale, 0 = none), and metropolitan residence (0 = non-metropolitan area, 1 = metropolitan area). Race is measured with three dichotomous variables to compare (1) non-Hispanic African Americans, (2) Hispanics, and (3) non-Hispanic other racial groups to non-Hispanic Whites (the reference category).
Analysis
For the cross-sectional analysis, we estimate several ordinal logistic regression models in STATA (v. 11) to predict 2003 weight categories. The results are substantively similar to those from multinomial logistic regression models. (Results available upon request). For the longitudinal models, we make an additional data restriction. We omit people who report gaining (n = 73 [averaged across imputations]) or losing (n = 50 [consistent across imputations]) at least 75 pounds in between 1999 and 2003 because such dramatic changes likely reflect a reporting error in either year or very unique weight-related experiences. We then use an OLS regression to predict their change in weight (in pounds) between 1999 and 2003.
All models include PSID 2003 sampling weights to account for the PSID’s attrition and oversampling of low-income Southern households and, thereby, make the findings generalizable to the 2003 U.S.-born population. For ease of presentation, we present results stratified by sex, but we estimate supplemental models using a pooled sample of men and women to directly test whether the interaction between food insecurity and the presence of children is significantly different by sex.
RESULTS
Table 1 presents weighted descriptive statistics for our full analytic sample and for men and women separately. Key among these is that over 60% of the sample is overweight or obese in both 1999 and 2003. On average, women are more likely to be overweight or obese in both years and women gain more weight between 1999 and 2003 (p <.01). In 1999, 6.8% of the sample was food insecure, while only 4.8% of the sample was food insecure in 2003. These estimates are lower than the national averages for these years, reflecting our restriction to U.S.-born individuals. As such, our tests rely on the comparison of small subpopulations. There are 174 food insecure men (101 are fathers) and 293 food insecure women (196 are mothers). In 2003, the average sample member was 39 years old, which partially accounts for the observed decline in the proportion living with children between 1999 and 2003. Half the sample lives with children in 2003 and women are slightly more likely than men to live with children (p < .05).
Table 1.
Sample Means and Percentages, Weighted and Adjusted for Sampling Design
| Full Sample (N = 7,931)
|
Women (N = 4,337)
|
Men (N =3,594)
|
||||
|---|---|---|---|---|---|---|
| 1999 | 2003 | 1999 | 2003 | 1999 | 2003 | |
| Weight, Cawley-adjusted self-report | ||||||
| Body Mass Index | 28.3 | 29.2 | 31.1 | 32.2 | 25.3 ‡ | 25.8 ‡ |
| Weight classificiation | ||||||
| Underweight | 1.1% | 1.0% | 0.2% | 0.1% | 2.0% ‡ | 2.0% ‡ |
| Normal weight (reference) | 34.7% | 30.1% | 17.9% | 13.9% | 53.7% ‡ | 48.4% ‡ |
| Overweight | 33.6% | 33.6% | 34.7% | 32.5% | 32.3% | 34.8% |
| Obese | 30.6% | 35.3% | 47.1% | 53.5% | 11.9% ‡ | 14.7% ‡ |
| Weight change (in pounds), 1999 – 2003 | 5.3 | 6.7 | 3.7 ‡ | |||
| Household food insecurity | 6.8% | 4.8% | 7.9% | 5.6% | 5.5% ‡ | 3.9% ‡ |
| Household income (in $1,000s) | -- | 79,892 | -- | 76,460 | -- | 83,783 ‡ |
| Female (=1) | -- | 53.1% | -- | -- | -- | -- |
| Children | ||||||
| Co-reside with children (=1) | 55.0% | 49.9% | 56.2% | 51.2% | 53.6% | 48.4% † |
| Number of children present | 1.0 | 0.9 | 1.1 | 1.0 | 1.0 | 0.9 |
| Relationship to co-residential children (among those living with children) | ||||||
| All borne by her | -- | -- | -- | 57.5% | -- | -- |
| Some or all not borne by her | -- | -- | -- | 42.5% | -- | -- |
| Number of children ever borne | -- | -- | -- | 2.03 | -- | -- |
| Age (range: 18 – 55 in 1999) | -- | 39.4 | -- | 39.3 | -- | 39.5 |
| Education in years (range: 6 – 17) | -- | 13.5 | -- | 13.4 | -- | 13.6 † |
| Married or cohabiting (=1) | -- | 73.3% | -- | 70.7% | -- | 76.3% ‡ |
| Poor or fair self-rated health (=1) | -- | 11.1% | -- | 12.4% | -- | 9.7% ‡ |
| Disabled (=1) | -- | 6.2% | -- | 7.2% | -- | 5.1% ‡ |
| Race/ethnicity | ||||||
| non-Hispanic White (reference) | -- | 80.1% | -- | 78.8% | -- | 81.8% ‡ |
| non-Hispanic African American | -- | 9.9% | -- | 11.4% | -- | 8.1% ‡ |
| Hispanic | -- | 6.1% | -- | 6.1% | -- | 6.1% |
| non-Hipanic other racial group | -- | 3.9% | -- | 3.7% | -- | 4.0% |
| Metropolitan residence (=1) | -- | 76.0% | -- | 76.3% | -- | 75.7% |
Note: Two-tailed tests of a signficant difference between men and women are noted as follows:
p < .05,
p < .01
Prior research has consistently found a linear, negative relationship between income and obesity among women, but not men. Given that this sex difference motivates our study, we first test whether we find similar patterns in these data. To do so, we examine coefficients from an OLS regression of standardized BMI (i.e., mean = 0, standard deviation = 1) in 2003 on standardized 2003 household income separately for men and women in models that include PSID sampling weights. We test for significant sex differences in this association in a supplemental model that includes men and women together and an interaction between household income and sex. For men, the standardized coefficient for household income is −0.01 and not statistically significant (p = .29), while for women it is −0.20 and statistically significant (p < .001). This sex difference is statistically significant (p < .000). We next explore the relationship between household income and the likelihood of being overweight or obese in 2003 in a similar manner, but using a logistic regression model and measuring income in its original metric in ten-thousand dollar units. Household income does not predict whether a man will be overweight or obese (p = .34), but the odds that a woman will be overweight or obese declines by .01 with every ten- thousand dollar increase in income (p < .0001). This sex difference is also statistically significant (p < .0001). Thus, we replicate prior research findings with these data.
Table 2 presents the results for our cross-sectional ordinal logistic regression models predicting individuals’ weight classifications in 2003. Model 1 presents the additive model and finds that, for both men and women, neither household food insecurity nor the presence of children predict being overweight. Model 2 provides the test of our hypothesis that mothers are at a higher risk for overweight and obesity when challenged with food insecurity relative to child-free women and all men. The results support our hypothesis. The coefficient for the interaction between household food insecurity and child co-residence among women is large in magnitude (e.g., comparable in size to the coefficients for being African American or Hispanic) and highly significant (p < .01). In fact, the likelihood that a woman is in a heavier weight classification is 202% (= [e1.106 −1]*100%) higher if she is a food insecure mother relative to child-free food secure woman. Moreover, by changing the reference category, we can see that the likelihood of being in a heavier weight classification is 177% (= [e1.02−1]*100%) higher for food insecure mothers versus food insecure child-free women (p < .05). Among men, the interaction between household food insecurity and the presence of children is not statistically significant. This sex difference is statistically significant (p < .01).
Table 2.
Coefficients from Cross-Sectional Ordinal Logistic Regression Models Predicting a Heavier Weight Classification in 2003 (N = 7,931)
| Women
|
Men
|
|||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Child present | −0.034 (0.085) | −0.085 (0.086) | −0.127 (0.084) | −0.122 (0.085) |
| Household food insecurity | 0.085 (0.214) | −0.487 (0.305) | −0.062 (0.218) | 0.027 (0.343) |
| Child present * Household food insecurity | -- | 1.106** (0.401) | -- | −0.150 ‡ (0.416) |
| Age | 0.013** (0.005) | 0.012** (0.005) | 0.003 (0.005) | 0.003 (0.005) |
| Married or cohabiting | −0.298** (0.099) | −0.303** (0.100) | 0.363** ‡ (0.117) | 0.363** ‡ (0.117) |
| Education | −0.132*** (0.019) | −0.130*** (0.019) | −0.062*** ‡ (0.019) | −0.062*** † (0.019) |
| Poor or fair health | 0.064 (0.165) | 0.076 (0.164) | 0.586*** † (0.158) | 0.589*** † (0.158) |
| Disabled | 0.309 (0.178) | 0.331 (0.178) | −0.057 (0.232) | −0.062 (0.233) |
| Race/ethnicity (reference: non-Hispanic White) | ||||
| African American | 1.295*** (0.117) | 1.287*** (0.117) | −0.440*** ‡ (0.122) | −0.441*** ‡ (0.122) |
| Hispanic | 1.537*** (0.237) | 1.503*** (0.237) | −0.350 ‡ (0.181) | −0.345 ‡ (0.181) |
| Other race | −0.042 (0.197) | −0.047 (0.198) | −0.248 (0.187) | −0.249 (0.187) |
| Metropolitan area | −0.158 (0.091) | −0.162 (0.091) | −0.025 ‡ (0.092) | −0.025 (0.092) |
Standard errors in parentheses
p< .05,
p< .01,
p< .001
Note: The ordered weight classifications are (1) Normal or Underweight, (2) Overweight, and (3) Obese. Models are weighted and adjusted for sampling design. Two-tailed tests of a significant difference between men and women are noted as follows:
p < .05,
p < .01
We also explore whether we find similar results using the number of children present in the home instead of a simple categorical indicator for any children. Although the results are in the anticipated direction, the interaction is not statistically significant for women (p = .35) or men (p = 0.62). We also explore whether we find similar results if we substitute the number of years of household food insecurity between 1999 and 2003 for the categorical indicator of household food insecurity in 2003. Similar to our initial results, we find that the risk of being overweight or obese increases as the years of household food insecurity increases among mothers (β = 0.338, p < .05), but not non-mothers. (Results for these two tests available upon request). Thus, with these initial tests, we find support for our first hypothesis: household food insecurity is associated with overweight and obesity among mothers, but not among child-free women or all men.
Table 3 tests this basic finding across various specifications to better ascertain the factors that undergird this differential risk for mothers. Panel A provides the test for Hypothesis 2 and examines whether the risks of food insecurity are greater among single mothers relative to married or cohabiting mothers. We stratify our sample not only by sex, but also by whether the person lives with a partner. Among married and cohabiting individuals, we do not find that food insecure mothers are more likely to be overweight or obese than food insecure, child-free women or food secure women. We do see this among single food insecure mothers. Therefore, as predicted, the risks of food insecurity are greater among single mothers. We do not find similar and statistically significant risks for food insecure, single fathers and the difference between single fathers and single mothers is not statistically significant. But our limited sample sizes for food insecure single fathers (n = 18) and food insecure single mothers (n = 104) limit the reliability of these sex comparisons.
Table 3.
Coefficients from Cross-Sectional Ordered Logistic Regression Models Predicting a Heavier Weight Classification in 2003 Under Different Specifications
| Women
|
Men
|
|||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Panel A. Separate Models by Relationship Status | ||||
| Married or Cohabiting in 2003 (N = 5,863) | ||||
| Child present | −0.071 (0.098) | −0.073 (0.099) | −0.050 (0.092) | −0.064 (0.093) |
| Household food insecurity | 0.620 (0.300) | 0.578 (0.480) | −0.324 † (0.257) | −0.738 † (0.484) |
| Child present * Household food insecurity | -- | 0.064 (0.596) | -- | 0.550 (0.549) |
| Single in 2003 (N = 2,068) | ||||
| Child present | 0.080 (0.169) | −0.074 (0.178) | −0.842*** ‡ (0.242) | −0.795** ‡ (0.251) |
| Household food insecurity | −0.271 (0.282) | −0.890* (0.370) | 0.519 † (0.399) | 0.600 † (0.465) |
| Child present * Household food insecurity | -- | 1.471** (0.543) | -- | −0.333 (0.855) |
| Panel B. Women Living with Children in 2003 (N = 2,592) | ||||
| Co-resides with children not borne by her | 0.263 (0.162) | 0.207 (0.164) | -- | -- |
| Household food insecurity | 0.749** (0.269) | 0.588* (0.283) | -- | -- |
| Co-resides with children not borne by her * HH food insecuritya | -- | 2.357* (1.073) | -- | -- |
| Number of children present | 0.066 (0.109) | 0.068 (0.109) | -- | -- |
| Panel C. Women Who Have Ever Had a Birth by 2003 (N = 3,844) | ||||
| Number of children ever born | 0.104* (0.042) | 0.109* (0.043) | -- | -- |
| Household food insecurity | 0.332 (0.222) | 0.576 (0.544) | -- | -- |
| Number of children ever born * Household food insecurity | -- | −0.095 (0.176) | -- | -- |
Standard errors in parentheses
p< .05,
p< .01,
p< .001
Note: The ordered weight classifications are (1) Normal or Underweight, (2) Overweight, and (3) Obese. Models are weighted and adjusted for sampling design. Two-tailed tests of a significant difference between men and women are noted as follows:
p < .05,
p < .01. Models include all control variables measured in 2003.
“HH” is an abbreviation for “Household.”
Panels B and C in Table 3 explore whether the greater risk of obesity among food insecure mothers is related to pregnancy-specific metabolic changes that predispose biological mothers to be heavier. Panel B focuses on women living with children in 2003; all other individuals are omitted from these models. The models test whether mothers who did not give birth to the children they live with are less likely to be overweight relative to those mothers who did, while controlling for the number of children present. In Model 1, we confirm that all food insecure mothers are more likely to be overweight or obese, but their biological relationship to those children is not, on average, predictive of being overweight or obese. In Model 2, we test whether the risks of food insecurity for being overweight or obese are greater for those living with only biological children. If either pregnancy-specific metabolic changes or evolutionary-based preferences for biological children were driving our results, then we would expect the coefficient for the interaction between household food insecurity and living with non-biological children to be statistically significant and negative. Although the interaction is statistically significant, it has the opposite sign. The risks of food insecurity for being in a heavier weight category are actually greater if the mother is not biologically related to all of the children present.
To further test whether pregnancy-related metabolic changes explain the associations observed in Table 2, Panel C in Table 3 examines these patterns among women who have ever given birth, regardless of whether those children currently live with them or not and controlling for the mothers’ social and demographic characteristics. Model 1 demonstrates that the likelihood a mother is overweight or obese increases with parity. Interestingly, current household food insecurity among all women who have ever given birth is not predictive of overweight. Model 2 reveals, however, that the experience of household food insecurity does not interact with a woman’s parity to generate additional risks for being overweight or obese. Therefore, based on the results in Panels B and C of, we conclude that metabolic changes associated with pregnancy do not explain why food insecure mothers are at greater risk of being overweight or obese.
Although the evidence is consistent with our theoretical explanation that food insecure mothers adopt strategies that strive to protect their children, but that create risks for being overweight or obese, we do not have direct measures of these behaviors to test this. Instead, we test alternative mediating pathways and see if, with the inclusion of other indicators, the magnitude or statistical significance of our key finding changes. Table 4 presents the results from a series of models that test whether the risk of being overweight or obese for food insecure mothers differs with the inclusion of physical activity (Model 3), smoking and alcohol consumption (Model 4), and food stamps and WIC participation (Model 5). Model 6 includes all six hypothesized mediating pathways. Across all models, the interaction of food insecurity and the presence of children is statistically significant and essentially the same magnitude as reported in Table 2. The interaction for men is never statistically significant.
Table 4.
Coefficients from Cross-Sectional Ordered Logistic Regression Models Predicting a Heavier Weight Classification in 2003 with the Inclusion of Indicators for Alternative Mediating Pathways
| Women
|
Men
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 3 | Model 4 | Model 5 | Model 6 | Model 3 | Model 4 | Model 5 | Model 6 | ||||||
| Child present | −0.087 (0.086) | −0.130 (0.087) | −0.106 (0.086) | −0.152 (0.088) | −0.135 (0.086) | −0.151 (0.087) | −0.117 (0.086) | −0.164 (0.087) | |||||
| Household food insecurity | −0.493 (0.302) | −0.454 (0.314) | −0.502 (0.302) | −0.476 (0.308) | 0.028 (0.347) | 0.119 (0.344) | 0.029 (0.344) | 0.119 (0.350) | |||||
| Child present * HH food insecuritya | 1.119** (0.402) | 1.117** (0.409) | 1.012* (0.400) | 1.041* (0.410) | −0.169 ‡ (0.420) | −0.159 ‡ (0.406) | −0.130 ‡ (0.420) | −0.174 ‡ (0.413) | |||||
| Physical Activity | |||||||||||||
| Frequency of light activity | −0.003 (0.002) | -- | -- | −0.003 (0.002) | −0.001 (0.002) | -- | -- | −0.001 (0.002) | |||||
| Frequency of heavy activity | −0.012** (0.005) | -- | -- | −0.012** (0.005) | −0.009* (0.004) | -- | -- | −0.010* (0.004) | |||||
| Substance use | |||||||||||||
| Alcohol consumption | -- | −0.301*** (0.059) | -- | −0.289*** (0.059) | -- | −0.072 ‡ (0.049) | -- | −0.070 ‡ (0.049) | |||||
| Smoking | -- | −0.447*** (0.105) | -- | −0.455*** (0.106) | -- | −0.744*** ‡ (0.104) | -- | −0.757*** ‡ (0.105) | |||||
| Means-Tested Nutrition Program Participation | |||||||||||||
| Food stamps | -- | -- | 0.314 (0.208) | 0.317 (0.208) | -- | -- | −0.215 ‡ (0.240) | −0.085 ‡ (0.231) | |||||
| WIC | -- | -- | 0.469 (0.244) | 0.443 (0.246) | -- | -- | 0.061 † (0.233) | 0.076 † (0.228) | |||||
Standard errors in parentheses
p< .05,
p< .01,
p< .001
Note: The ordered weight classifications are (1) Normal or Underweight, (2) Overweight, and (3) Obese. Models are weighted and adjusted for sampling design. Two-tailed tests of a significant difference between men and women are noted as follows:
p < .05,
p < .01. Models include all control variables measured in 2003.
“HH” is an abbreviation for “Household.”
We next estimate our longitudinal models. Because of the selection process into child birth, adoption and forming a blended family with non-biological children, we not only estimate our longitudinal models for the full sample, but also on a sub-sample of individuals already living with children in 1999. If selection into child co-residence were a key factor, then we should find larger estimates for the interaction between household food insecurity and changes in the number of children in the full sample.
It is important to note that these models are vulnerable to issues of power. First and foremost, the interactions in these longitudinal models create more combinations of rare events. As such, we consider p-values of less than .10 as statistically significant. Also, it is unknown whether a four-year window is a sufficient time frame to observe shifts in weight as a function of the combination of food insecurity and childcare among women. Finally, there is the potential for differential ceiling effects. In 1999, 30% of women in the sample are already obese, whereas only 12% of men are obese in 1999. Similarly food insecure women are already heavier in 1999 than food secure women.
Table 5 displays the results for OLS regression models of weight change between 1999 and 2003 after omitting those who gain or lose 75 pounds or more over this four-year period. In Model 1, we see that increases in the number of children are not, on average, predictive of weight gain for either women or men in the full sample. Similar patterns are observed for women in the sub-sample restricted to those living with children in 1999. Yet men living with children in 1999 are predicted to lose weight as the number of children increases. Years of food insecurity is associated with weight loss, but this association is only statistically significant among women in the full sample and men living with children in 1999.
Table 5.
Coefficients from OLS Regression Models Predicting Weight Change (in Pounds; 2003–1999) Based on the Change in the Number of Children Present (2003–1999) and Count of Years of Food Insecurity (1999, 2001, 2003)
| Full Sample (N = 7,808)a
|
Living with Children in 1999 (N = 4,904)a
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Women
|
Men
|
Women
|
Men
|
|||||
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Change in count of children | 0.184 (0.467) | −0.274 (0.487) | −0.397 (0.383) | −0.619 (0.405) | −0.145 (0.569) | −0.873 (0.607) | −0.887+ (0.515) | −1.012+ (0.545) |
| Years of food insecurity | −1.690* (0.854) | −1.298 (0.868) | −1.062 (0.803) | −0.922 (0.804) | −1.645 (1.035) | −0.789 (1.047) | −1.649+ (0.919) | −1.495 ! (0.918) |
| Change in child count * Years of food insec. | -- | 1.911* (0.949) | -- | 1.153* (0.565) | -- | 2.549** (0.953) | -- | 0.520 ! (0.626) |
Standard errors in parentheses
p<.10,
p< .05,
p< .01,
p< .001
Note: Models are weighted and adjusted for sampling design. Two-tailed tests of a significant difference between men and women are noted as follows:
p <.10,
p < .05,
p < .01. Models include all control variables measured in 2003.
Individuals who lost or gained 75 or more pounds between 1999 and 2003 are omitted from these analysis.
Model 2 includes the interaction between changes in the number of children present and the count of years of food insecurity. We find a significant positive association for both women and men in the full sample and a significant positive association for women in the sub-sample of people living with children in 1999. It is important to note that the magnitude of the interaction is larger for women already living with children in 1999 than for all women. Thus, selection into biological or social motherhood is not the key factor. For men, however, the interaction is larger in the full sample and, thus, selection might underlie these results.
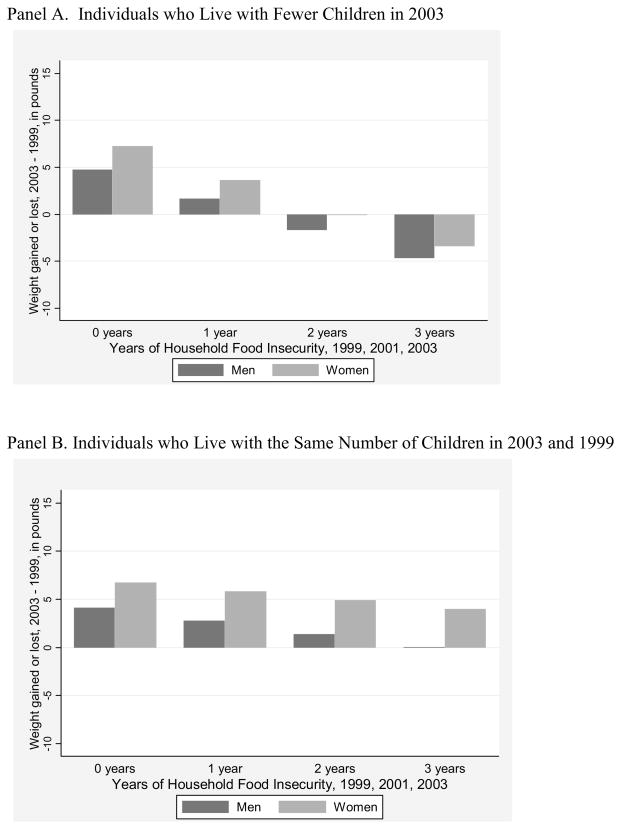
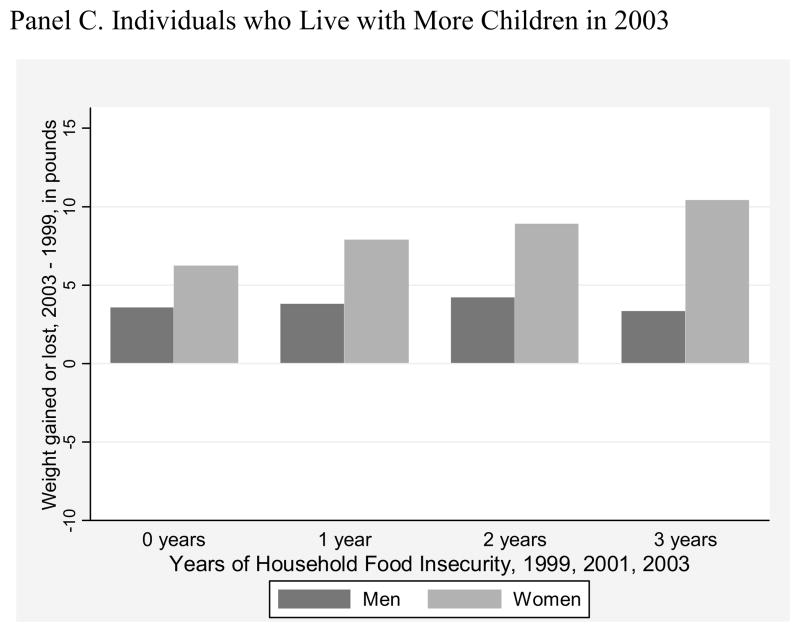
Given the unexpected statistically significant interaction for men in the full sample, we graph the predicted probabilities from this model in Figure 1. The predicted probabilities are calculated by letting the number of children, years of household food insecurity, and their interaction to freely vary, but we set all other variables to their means or modal categories. For ease of presentation, Panel A shows the patterns when individuals live with fewer children in 2003, Panel B shows the patterns when the number of children is unchanged, and Panel C shows the patterns when individuals live with more children in 2003. In each panel, the y-axis is the number of pounds gained or lost between 1999 and 2003 and the x-axis is the years of food insecurity. The dark bars are for men and the lighter bars are for women.
Figure 1.
Predicted Change in Weight 1999 and 2003 Depending on Changes in the Number of Co-residential Children and Years of Food Insecurity
Panels A and B reveal similar patterns for both men and women. Whether the number of co-residential children declines (Panel A) or remains the same (Panel B), men and women gain the most weight (i.e., 5 pounds for men and 7 pounds for women) if they are never food insecure. The amount of weight they gain, however, declines as the years of food insecurity increases. In fact, in Panel A, men and women who live with fewer children in 2003 and experience 3 years of food insecurity actually lose weight (i.e., 4 pounds for men and 3 pounds for women). Panel C, which shows the patterns for individuals who live with more children in 2003, is revealing. For men living with more children in 2003, their weight gain over this period (approximately 4 pounds) is insensitive to increases in the number of years of food insecurity. Among women who live with more children in 2003, however, the amount of weight they gain increases as their years of food insecurity increases. Those who are never food insecure gain 6 pounds and those who are food insecure for 3 years gain 10 pounds. Although this is only a four-pound difference, we see that as childcare responsibilities increase in conjunction with greater exposure to household food insecurity, women gain more weight. For men, this significant interaction translates into them being less likely to lose weight as they gain children and increase their years of household food insecurity. Therefore, the longitudinal results buttress our cross-sectional findings.
DISCUSSION
This manuscript explores whether the sex differences in overweight and obesity related to food insecurity, and income more broadly, can be better characterized as differences between mothers and non-mothers. In support of Hypothesis 1, we find that food insecure mothers are more likely to be overweight and obese than their food insecure, but child-free female counterparts. In contrast, food insecure fathers are not at greater risk of being overweight or obese. These risks of motherhood do not appear to be the result of metabolic changes associated with pregnancy per se, nor do they diminish with the inclusion of self-reported physical activity, smoking, drinking, food stamps receipt, and WIC participation. Furthermore, the longitudinal findings suggest that women are at risk of gaining weight as they gain childcare responsibilities and additional years of household food insecurity.
The combined risks of childcare and household food insecurity are particularly problematic for single mothers, as we predicted in Hypothesis 2. Single mothers are not only more at risk of experiencing food insecurity than their married or cohabiting counterparts, but the consequences of household food insecurity for their weight are greater. At the individual-level, this likely reflects the challenges of being both the sole provider and caretaker within a household. But there is an important cultural dimension as well. Most single parent families are headed by women because of traditional, gendered views of childcare. Together, these individual and cultural factors place single mothers at greater risk of poverty, food insecurity, and obesity.
This study is not without limitations. Because of the PSID’s design, our findings are representative of US-born individuals and cannot speak to the risks for immigrant mothers, an important and growing segment of the US population. Because immigrants have higher rates of food insecurity (Borjas, 2004), our sample has a lower rates of food insecurity than is found in official reports. This, in turn, limits our power for some analyses given that we interact household food insecurity (5% of the sample), sex (50% is female), and co-residence with children (50% of the sample) in all models. In light of these power limitations it is somewhat surprising that we can detect statistically significant differences for single mothers, women living with some non-biological children, and for all mothers in our longitudinal analyses. Our sample is also restricted to individuals who head their own household (either alone or with a partner) over these four years. Our findings may not be applicable to those who live in subfamilies or with their parents, though we find substantively similar results when we relax this requirement. We prefer the results presented here that use this sample restriction because the decision to move in with someone else is likely endogenous to the processes we are interested in (i.e., the management of poverty and food insecurity) and thus deserves greater attention and direct investigation. A key limitation is that we only have indirect evidence that mothers adopt strategies to protect their children, but place themselves at greater risk of obesity. Finally, we cannot claim to have uncovered a causal relationship, even in the longitudinal models, because we have observational data. For a stronger test, we also ran fixed effects models to examine changes over time. The interaction between household food insecurity and the presence of children was not statistically significant for men or women in these models (see Appendix Table 1). Thus, unobserved factors may be contributing to the patterns we observe. However, fixed effects models place even greater demands on power and this may partially explain the absence of a significant effect. We encourage scholars to conduct additional research and collect data with larger samples and direct measures of individual’s dietary behavior to better adjudicate the relationship between household food insecurity, motherhood, and weight.
Appendix Table 1.
Coefficients from OLS Fixed Effects Regression Models Predicting Weight, 1999 – 2003
| Women
|
Men
|
|||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Number of children present | −0.150 (0.315) | −0.177 (0.328) | 0.173 (0.238) | 0.167 (0.243) |
| Household food insecurity | −0.619 (0.807) | −0.966 (1.292) | −1.284 (0.758) | −1.365 (1.038) |
| Number of children * Household food insecurity | -- | 0.213 (0.576) | -- | 0.054 (0.472) |
Standard errors in parentheses
p< .05,
p< .01,
p< .001
Note: This model has 3 explanatory variables, 7,808 individuals (N), and 3 time points (T). The total number of observations equals N * T = 23,424, while the degrees of freedom lost equals N+K−1 = 7,810.
These caveats aside, our research makes a significant contribution by demonstrating that that the documented sex difference in the relationship between food insecurity and weight is better characterized as a difference between mothers and non-mothers. The results are consistent with our arguments, derived from prior research on food insecurity, that mothers adopt numerous, but unhealthy strategies to protect their children when the family faces threats to their food supply. These findings, thus, provide a new lens by which to consider our commonly held biases against overweight women. Obesity is highly stigmatized (Dejong, 1980; Puhl & Brownell, 2003) and people frequently characterize those who are overweight as lazy and stupid (Crandall & Schiffhauer, 1998). To the extent that poor, food insecure mothers are at greater risk of obesity, the prior literature suggests that it is certainly not attributable to sloth or absent-mindedness. Instead, we suspect that their active management and protection of their children creates risks for obesity and weight gain. Beyond drawing our attention to the generally hidden work of poor mothers, these results demonstrate that our socially constructed roles and responsibilities can generate risks for individual health and well-being.
Research Highlights.
The gendered nature of childcare explains why poverty and household food insecurity predicts overweight and obesity among American women, but not men.
Food insecure mothers are more likely to be overweight or obese and gain excess weight over time.
Results cannot be attributed to post-pregnancy biological changes that predispose mothers to gain weight.
Food insecurity is not associated with being overweight or obese or gaining excess weight among fathers or child-free women and men.
The intersection of gender, parenthood and poverty create risks for overweight and obesity among food insecure American mothers.
Acknowledgments
Funding for this research was provided by NICHD grant R01-HD050144 (PI: G.D. Sandefur). We thank Michelle Frisco and Jason Houle, the Robert Wood Johnson Foundation Health & Society Scholars Program Working Group on Gender and Health at Columbia University, and anonymous reviewers for their valuable comments.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Molly A. Martin, Email: mmartin@pop.psu.edu, Pennsylvania State University
Adam Lippert, Pennsylvania State University.
References
- Adams EJ, Grummer-Strawn L, Chavez G. Food Insecurity is Associated with Increased Risk of Obesity in California Women. Journal of Nutrition. 2003;133:1070–1074. doi: 10.1093/jn/133.4.1070. [DOI] [PubMed] [Google Scholar]
- Allon N. The Stigma of Overweight in Everyday Life. In: Wolman B, editor. Psychological Aspects of Obesity: A Handbook. New York: Van Nostrand; 1982. pp. 130–174. [Google Scholar]
- Badun C, Evers S, Hooper M. Food security and nutritional concerns of parents in an economicallly disadvantaged community. Journal of the Canadian Dietetic Association. 1995;56(2):75–80. [Google Scholar]
- Becketti S, Gould W, Lillard L, Welch F. The PSID after fourteen years: An evaluation. Journal of Labor Economics. 1988;6(4):472–492. [Google Scholar]
- Berkey CS, Rockett HR, Gillman MW, Field AE, Colditz GA. Longitudinal study of skipping breakfast and weight change in adolescents. International Journal of Obesity and Related Metabolic Disorders. 2003;27(10):1258–1266. doi: 10.1038/sj.ijo.0802402. [DOI] [PubMed] [Google Scholar]
- Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. Alexandria, VA: U.S. Department of Agriculture, Agriculture, Food and Nutrition Service; 2000. [Google Scholar]
- Borjas G. Food insecurity and public assistance. Journal of Public Economics. 2004;88(7–8):1421–1443. [Google Scholar]
- Casper LM, Bianchi SM. Continuity and Change in the American Family. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Cawley J. The Impact of Obesity on Wages. Journal of Human Resources. 2004;39(2):451–474. [Google Scholar]
- Cawley J, Burkhauser RV. NBER Working Paper. Cambridge, MA: 2006. Beyond BMI: The Value of More Accurate Measures of Fatness and Obesity in Social Science Research; p. 12291. [DOI] [PubMed] [Google Scholar]
- Coltrane S. Research on Household Labor: Modeling and Measuring the Social Embeddedness of Routine Family Work. Journal of Marriage and Family. 2000;62(4):1208–1233. [Google Scholar]
- Coltrane S, Adams M. The Social Construction of the Divorce ‘Problem’: Morality, Child Victims, and the Politics of Gender. Family Relations. 2003;52(4):363–372. [Google Scholar]
- Crandall C, Schiffhauer K. Anit-Fat Prejudice: Beliefs, Values, and American Culture. Obesity Research. 1998;6:458–460. doi: 10.1002/j.1550-8528.1998.tb00378.x. [DOI] [PubMed] [Google Scholar]
- Daly M, Wilson M. Discriminative Parental Solicitude: A Biological Perspective. Journal of Marriage and Family. 1980;42(2):277–288. [Google Scholar]
- Dejong W. The Stigma of Obesity: The Consequences of Naïve Assumptions Concerning the Causes of Physical Deviance. Journal of Health and Social Behavior. 1980;21:75–87. [PubMed] [Google Scholar]
- DeVault ML. Feeding the Family. Chicago: University of Chicago Press; 1991. [Google Scholar]
- Dinour LM, Bergen D, Yeh MC. The Food Insecurity-Obesity Paradox: A Reivew of the Literature and the Role Food Stamps May Play. Journal of the American Dietetic Association. 2007;107(11):1952–1961. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Winkleby MA, Radimer KL. Dietary intakes and serum nutrients differ between adults from food-insufficient and food-sufficient families: Third National Health and Nutrition Examination Survey, 1988–1994. Journal of Nutrition. 2001;131(4):1232–1246. doi: 10.1093/jn/131.4.1232. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. American Journal of Clinical Nutrition. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- Fitzgerald J, Gottschalk P, Moffitt R. An Analysis of Sample Attrition in Panel Data: The Michigan Panel Study of Income Dynamics. Journal of Human Resources. 1998;33(2):251–299. [Google Scholar]
- French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annual Review of Public Health. 2001;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- Furstenberg FF, Cherlin AJ. Divided Families: What Happens to Children when Parents Part. Cambridge, MA: Harvard University Press; 1994. [Google Scholar]
- Gibson D. Food Stamp Program participation is positively related to obesity in low income women. Journal of Nutrition. 2003;133:2225–2231. doi: 10.1093/jn/133.7.2225. [DOI] [PubMed] [Google Scholar]
- Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Social Science & Medicine. 2006;62(7):1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- Gundersen C, Garasky S, Lohman BJ. Food Insecurity is Not Associated with Childhood Obesity as Assessed Using Multiple Measures of Obesity. Journal of Nutrition. 2009;139(6):1173–1178. doi: 10.3945/jn.109.105361. [DOI] [PubMed] [Google Scholar]
- Gundersen C, Kreider B. Bounding the Effects of Food Insecurity on Children’s Health Outcomes. Journal of Health Economics. 2009;28(5):971–983. doi: 10.1016/j.jhealeco.2009.06.012. [DOI] [PubMed] [Google Scholar]
- Hays S. The Cultural Contradictions of Motherhood. New Haven, CT: Yale University Press; 1998. [Google Scholar]
- Hill MS. The Panel Study of Income Dynamics: A User’s Guide. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Huddleston-Casas C, Charnigo R, Simmons LA. Food insecurity and maternal depression in rural, low-income families: a longitudinal investigation. Public Health Nutrition. 2009;12:1133–1140. doi: 10.1017/S1368980008003650. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Hunger and Obesity: Understanding a Food Insecurity Paradigm: Workshop Summary. Washington, D.C: The National Academies Press; 2011. [PubMed] [Google Scholar]
- Kempson KM, Keenan DP, Sadani PS, Ridlen S, Rosato NS. Food management practices used by people with limited resources to maintain food sufficiency as reported by nutrition educators. Journal of the American Dietetic Association. 2002;102(12):1795–1799. doi: 10.1016/s0002-8223(02)90385-8. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick SI, Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. Journal of Nutrition. 2008;138(3):604–612. doi: 10.1093/jn/138.3.604. [DOI] [PubMed] [Google Scholar]
- Ledikwe JH, Blanck HM, Khan LK, Serdula MK, Seymour JD, Tohill BC, et al. Dietary energy density is associated with energy intake and weight status in US adults. American Journal of Clinical Nutrition. 2006;83(6):1362–1368. doi: 10.1093/ajcn/83.6.1362. [DOI] [PubMed] [Google Scholar]
- Lyons AA, Park J, Nelson CH. Food Insecurity and Obesity: A Comparison of Self-Reported and Measured Height and Weight. American Journal of Public Health. 2008;98(4):751–757. doi: 10.2105/AJPH.2006.093211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y, Bertone ER, Stanek EJ, III, Reed GW, Hebert JR, Cohen NL, et al. Association between eating patterns and obesity in a free-living US adult population. American Journal of Epidemiology. 2003;158(1):85–92. doi: 10.1093/aje/kwg117. [DOI] [PubMed] [Google Scholar]
- Marsiglio W, Amato P, Day RD, Lamb ME. Scholarship on Fatherhood in the 1990s and Beyond. Journal of Marriage and Family. 2000;62(4):1173–1191. [Google Scholar]
- Martin KS, Ferris AM. Food Insecurity and Gender are Risk Factors for Obesity. Journal of Nutrition Education and Behavior. 2007;39(1):31–36. doi: 10.1016/j.jneb.2006.08.021. [DOI] [PubMed] [Google Scholar]
- McIntyre L, Connor SK, Warren J. Child Hunger in Canada: Results of the 1994 National Longitudinal Survey of Children and Youth. Canadian Medical Association Journal. 2000;163(8):961–965. [PMC free article] [PubMed] [Google Scholar]
- McIntyre L, Glanville NT, Raine KD, Dayle JB, Anderson B, Battaglia N. Do low-income lone mothers compromise their nutrition to feed their children? Canadian Medical Association Journal. 2003;168(6):686–691. [PMC free article] [PubMed] [Google Scholar]
- McLaren L. Socioeconomic Status and Obesity. Epidemiological Reviews. 2007 doi: 10.1093/epirev/mxm001. (Advanced Access) [DOI] [PubMed] [Google Scholar]
- Mitchell BD, Rainwater DL, Hsueh WC, Kennedy AJ, Stern MP, MacCluer JW. Familial Aggregation of Nutrient Intake and Physical Activity: Results from the San Antonio Family Heart Study. Annals of Epidemiology. 2003;13(2):128–135. doi: 10.1016/s1047-2797(02)00255-7. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- Nord M, Andrews M, Carlson S. Household Food Security in the United States, 2003. Washington, D.C: U.S. Department of Agriculture, Economic Research Service; 2004. [Google Scholar]
- Nord M, Coleman-Jensen A, Andrews M, Carlson S. Household Food Security in the United States, 2009. Washington, D.C: US Department of Agriculture, Economic Research Service; 2010. [Google Scholar]
- Olson CM. Nutrition and Health Outcomes Associated with Food Insecurity and Hunger. Journal of Nutrition. 1999;129:521–524. doi: 10.1093/jn/129.2.521S. [DOI] [PubMed] [Google Scholar]
- Poston WS, 2nd, Foreyt JP. Obesity is an environmental issue. Atherosclerosis. 1999;146(2):201–209. doi: 10.1016/s0021-9150(99)00258-0. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Brownell KD. Psychosocial Origins of Obesity Stigma: Toward Changing a Powerful and Pervasive Bias. Obesity Reviews. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- Radimer KL. Understanding Hunger and Developing Indicators to Assess It. Ithaca, NY: Cornell University; 1990. [Google Scholar]
- Rose D, Gundersen C, Oliveira V. Technical Bulletin #1869. Washington, DC: U.S. Department of Agriculture, Economic Research Service; 1998. Socio-Economic Determinants of Food Insecurity in the United States: Evidence from the SIPP and CSFII Datasets. [Google Scholar]
- Rothman SM. Woman’s Proper Place: A History of Changing Ideas and Practices, 1870 to the Present. New York: Basic; 1978. [Google Scholar]
- Royston P. Multiple imputation of missing values: update. Stata Journal. 2005a;5(2):1–14. [Google Scholar]
- Royston P. Multiple imputation of missing values: Update of ice. Stata Journal. 2005b;5(4):527–536. [Google Scholar]
- Rubin D. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- Sanchez L, Thomson E. Becoming Mothers and Fathers: Parenthood, Gender, and the Division of Labor. Gender and Society. 1997;11(6):747–772. [Google Scholar]
- Sarlio-Lähteenkorva S, Lahelma E. Food Insecurity is Associated with Past and Present Economic Disadvantage and Body Mass Index. Journal of Nutrition. 2001;141:2880–2884. doi: 10.1093/jn/131.11.2880. [DOI] [PubMed] [Google Scholar]
- Schoeller DA. How Accurate is Self-Reported Dietary Energy Intake? Nutrition Reviews. 1990;48(10):373–379. doi: 10.1111/j.1753-4887.1990.tb02882.x. [DOI] [PubMed] [Google Scholar]
- Slattery ML, McDonald A, Bild DE, Caan BJ, Hilner JE, Jacobs JDR, et al. Associations of body fat and its distribution with dietary intake, physical activity, alcohol, and smoking in blacks and whites. American Journal of Clinical Nutrition. 1992;55:943–949. doi: 10.1093/ajcn/55.5.943. [DOI] [PubMed] [Google Scholar]
- Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychological Bulletin. 1989;105:260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- Sokoloff NJ. Between Money and Love: The Dialectics of Home and Market Work. New York: Praeger; 1980. [Google Scholar]
- South SJ, Spitze G. Housework in Marital and Nonmarital Households. American Sociological Review. 1994;59(3):327–347. [Google Scholar]
- Stevens CA. Exploring Food Insecurity Among Young Mothers (15–24 Years) Journal for Specialists in Pediatric Nursing. 2010;15(2):163–171. doi: 10.1111/j.1744-6155.2010.00235.x. [DOI] [PubMed] [Google Scholar]
- Tarasuk V, Beaton GH. Women’s Dietary Intakes in the Context of Household Food Insecurity. Journal of Nutrition. 1999;129:672–679. doi: 10.1093/jn/129.3.672. [DOI] [PubMed] [Google Scholar]
- Tarasuk V, McIntyre L, Li J. Low-Income Women’s Dietary Intakes are Sensitive to the Depletion of Household Resources in One Month. Journal of Nutrition. 2007;137:1980–1987. doi: 10.1093/jn/137.8.1980. [DOI] [PubMed] [Google Scholar]
- Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. Journal of Nutrition. 2001;131(6):1738–1745. doi: 10.1093/jn/131.6.1738. [DOI] [PubMed] [Google Scholar]
- Wiig K, Smith C. The art of grocery shopping on a food stamp budget: factors influencing the food choices of low-income women as they try to make ends meet. Public Health Nutrition. 2008;12:1726–1734. doi: 10.1017/S1368980008004102. [DOI] [PubMed] [Google Scholar]
- Wilde PE, Peterman JN. Individual Weight Change is Associated with Household Food Security Status. Journal of Nutrition. 2006;136:1395–1400. doi: 10.1093/jn/136.5.1395. [DOI] [PubMed] [Google Scholar]
- Wunderlich GS, Norwood JL, editors. Food Insecurity and Hunger in the United Stated: An Assessment of the Measure. Washington, DC: National Academies Press; 2006. [Google Scholar]