Abstract
Scleral fixated intraocular lens (SFIOL) is a safe and effective option for managing optical aphakia. Suture related complications like suture erosion, suture breakage, endophthalmitis, etc. are unique to SFIOL. The knots can be covered by partial thickness flaps or they can be rotated into scleral tissues without flaps to reduce the complications. We performed a recently described novel technique which obviates the need for knot and scleral flaps in securing the SFIOL. This novel 2-point Ab externo knotless technique may reduce the knot related problems. Twenty-three eyes undergoing this knotless SFIOL procedure were analyzed for intraoperative and postoperative complications. Twenty-two eyes either maintained or improved on their preoperative vision. All patients had a minimum follow-up of 24 months.
Keywords: Complications, knotless scleral fixated intraocular lens, technique
In the absence of capsule support, the problem of optical aphakia can be surgically managed by implanting an anterior chamber intraocular lens (IOL), attaching the IOL to the iris, or fixing the IOL into the posterior chamber by a transscleral suture. Scleral fixated IOL (SFIOL) is a safe and effective option for the visual rehabilitation of an aphakic eye with inadequate posterior capsule support.[1,2] Suture related complications are unique to SFIOL. To avoid erosion of the knots through conjunctiva, scleral flaps can be used to cover the knots[3] or they can be rotated into scleral tissue without flaps.[4] The partial thickness scleral flaps can atrophy over time and expose the prolene knot. Endophthalmitis has been reported and remains a real risk in patients undergoing SFIOL.[5] The possible causes of dislocation of a 10-0 prolene scleral sutured posterior chamber IOL (PCIOL) include suture degradation,[6] suture breakage,[4] slippage of the haptic from the suture,[4] or erosion of the suture through the tissue.[7] Szurman has recently described a novel technique of securing the SFIOL, which obviates the need of any external knot and scleral flaps.[8] The aim of this study was to perform this procedure in patients undergoing SFIOL in our institute and to analyze the complications associated with this procedure.
Materials and Methods
We retrospectively reviewed the records of 22 patients (23 eyes) who had knotless SFIOL. The following details were recorded: age, gender, pre- and postoperative best-corrected visual acuity (BCVA), indication for surgery and detailed slit-lamp and fundus examination. The main outcome measures were intraoperative and postoperative complications and final BCVA.
The intraocular procedures associated with the knotless SFIOL implantation included anterior vitrectomy and lensectomy in 3 eyes of 2 patients of Marfans syndrome, vitrectomy and lensectomy in 5 patients with dislocation of the lens, anterior vitrectomy in 11 eyes with post-surgical aphakia and IOL removal and vitrectomy in 4 patients with dislocated/ subluxated IOL.
A scleral tunnel incision centered at the 12 o’ clock position, with a width of 6–7 mm, was made in all cases. A double-armed 10-0 polypropylene suture (6002 PP, Aurolab, Madurai, India), with straight needle was used. One straight needle was passed perpendicularly through the full thickness sclera, 1.5 mm behind the limbus at 3 o’ clock position in a direction parallel to the iris, and was retrieved in the hollow of a 26-G needle on the opposite side. The stretched prolene suture was pulled out of the eye through a previously made sclerocorneal tunnel. The suture was then cut in the middle, and the two suture ends were passed through the corresponding eyelet of the SFIOL and tied. The lens was then inserted into the ciliary sulcus, and the sutures pulled to secure the IOL. The corneoscleral wound was closed with interrupted 10/0 nylon sutures (840 2N, Aurolab, India). The needle ends of the 10/0 prolene suture were then bent and ‘Z’ shaped intrascleral passes with at least five indentations were made to secure the IOL [Fig. 1]. The suture was then cut without making any knot and covered by the conjunctiva [Fig. 2]. The IOLs implanted were Aurolab SC6530 (Aurolab, India) single-piece polymethylmethacrylate (PMMA) lenses with eyelets. The optic diameter was 6.5 mm and the overall diameter was 13 mm.
Figure 1.
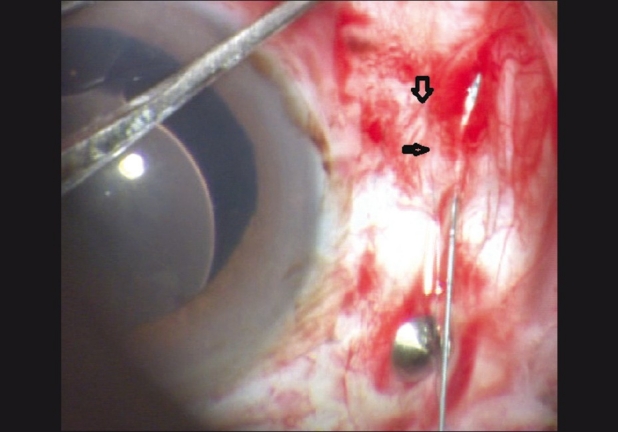
Snapshot showing the 10/0 prolene suture being passed intrasclerally to anchor the SFIOL
Figure 2.
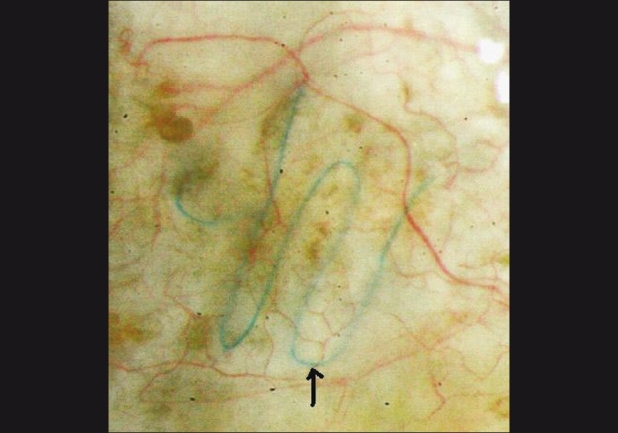
The arrow in the slit-lamp photograph pointing to the 10/0 prolene suture covered by the conjunctiva lying in a zigzag pattern in a case that underwent knotless SFIOL
Results
Twenty-three eyes of 22 patients with a follow-up of at least 24 months were included in this study.
In 16 eyes (70%), no intraoperative complications occurred. Seven eyes (30%) developed complications. The intraoperative complications included mild, transient vitreous hemorrhage in two eyes. The IOL haptic during insertion touched the ciliary body and caused vitreous hemorrhage with hemorrhagic choroidal detachment in one eye, which needed vitrectomy and choroidal drainage. Early complications (before 2 weeks) included pupillary capture of the optic of the IOL in one eye, which was managed by dilatation and constriction of the pupil, and raised intraocular pressure in two eyes, which needed anti-glaucoma medication for 2 weeks. Late complication (after 2 weeks) included cystoid macular edema in one eye, which resolved in 10 weeks.
The preoperative BCVA was maintained or improved in 22 eyes. The eye requiring vitrectomy and choroidal drainage had decrease in vision. The prolene suture was well covered by the conjunctiva in all cases.
Discussion
Thirteen eyes achieved a postoperative Snellen BCVA of 20/40 or better. Szurman performed this knotless technique on 22 patients (14 IOLs, 5 iris prosthesis, 3 iris diaphragm) with excellent results.[8] The technique used in this study leaves no external knot, thus reducing the risk of suture exposure and irritation and endophthalmitis. In an observational case series by Vote et al., 17 eyes (27.9%) had spontaneous suture breakage with several eyes having multiple episodes.[9]
Drews,[10] in his report published almost 25 years ago, noted that polypropylene may fail after a prolonged period in the eye. The deterioration was most marked with sutures buried in actively metabolizing ocular tissue. There is a possibility that a knotless polypropylene suture lying flush under the conjunctiva may be less prone to degrade and erode through the sclera. This case series of patients who underwent this new sutured IOL technique has the largest number of patients with the longest average follow-up. Ninety-five percent of the patients who had this Ab externo 2-point knotless fixation of the SFIOL did well after the surgery. In conclusion, the procedure was safe to perform and had mild self-limiting complications. As most of the suture-related complications occur years after the SFIOL procedure, larger trials with longer follow-up are needed to confirm these conclusions.
References
- 1.Donaldson KE, Gorscak JJ, Budenz DL, Feuer WJ, Benz MS, Forster RK. Anterior chamber and sutured posterior chamber intra ocular lenses in eyes with poor capsular support. J Cataract Refract Surg. 2005;31:903–9. doi: 10.1016/j.jcrs.2004.10.061. [DOI] [PubMed] [Google Scholar]
- 2.Bading G, Hillenkamp J, Sachs HG, Gabel VP, Framme C. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral- fixated sutured posterior chamber lens implantation. Am J Ophthalmol. 2007;144:371–7. doi: 10.1016/j.ajo.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 3.Lewis JS. Ab externo sulcus fixation. Ophthalmic Surg. 1991;22:692–95. [PubMed] [Google Scholar]
- 4.Lewis JS. Sulcus fixation without flaps. Ophthalmology. 1993;100:1346–50. doi: 10.1016/s0161-6420(93)31477-6. [DOI] [PubMed] [Google Scholar]
- 5.Heilskov T, Joondeph BC, Olsen KR, Blankenship GW. Late endophthalmitis after transscleral fixation of a posterior chamber intraocular lens. Arch Ophthalmol. 1989;107:1427. doi: 10.1001/archopht.1989.01070020501017. [DOI] [PubMed] [Google Scholar]
- 6.Price MO, Price FW, Jr, Werner L, Berlie C, Mamalis N. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 2005;31:1320–6. doi: 10.1016/j.jcrs.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 7.Kim J, Kinyoun JL, Saperstein DA, Porter SL. Subluxation of transscleral sutured posterior chamber intraocular lens (TSIOL) Am J Ophthalmol. 2003;136:382–4. doi: 10.1016/s0002-9394(03)00229-0. [DOI] [PubMed] [Google Scholar]
- 8.Szurman P, Petermeier K, Jaissle GB, Spitzer MS, Bartz-Schmidt KU. [Injector implantation of a scleral-fixated intraocular lens] Ophthalmologe. 2006;103:1020–26. doi: 10.1007/s00347-006-1406-8. [DOI] [PubMed] [Google Scholar]
- 9.Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol. 2006;141:308–12. doi: 10.1016/j.ajo.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 10.Drews RC. Quality control, and changing indications for lens implantation. The Seventh Binkhorst Medal Lecture-1982. Ophthalmology. 1983;90:301–10. doi: 10.1016/s0161-6420(83)34556-5. [DOI] [PubMed] [Google Scholar]


