Abstract
Thyroid associated orbitopathy, also known as Graves’ orbitopathy, is typically a self-limiting autoimmune process associated with dysthyroid states. The clinical presentation may vary from very mild disease to severe irreversible sight-threatening complications. Despite ongoing basic science and clinical research, the pathogenesis and highly effective therapeutic strategies remain elusive. The present article reviews the pathophysiology, clinical presentation, and management of this common, yet poorly understood disease, which remains a challenge to the ophthalmologist.
Keywords: Orbit, proptosis, thyroid
Graves’ disease is an autoimmune condition in which autoantibodies target the thyroid-stimulating hormone receptor (TSH-R) displayed on thyrocytes, inducing the production of excess thyroid hormone.[1] In addition to the hyperthyroidism, up to 40% of patients with Graves’ disease develop a manifestation localizing to the orbit, called thyroid associated orbitopathy (TAO) or Graves’ orbitopathy (GO).[2] The most significant pathological findings in TAO include glycosaminoglycan (GAG) deposition (accompanied by swelling resulting from the hydrophilic capacity of these macromolecules), fibrosis affecting the extraocular muscles, and adipogenesis in the orbit.[3–6] To date, there are no effective means of preventing the disease or reliably altering its course. Current therapeutic options include corticosteroids, external beam radiation and steroid-sparing immunosuppressive agents for reducing the inflammation during active disease, and surgery for correcting the residual abnormalities secondary to fibrosis in the inactive state of the disease. These interventions are aimed at the consequences of the disease rather than targeting its cause.[3,4] Unfortunately, these treatments do not prevent or reverse the pathological changes in the orbital tissues.[7] The present article reviews our current understanding of the disease and the management protocol.
Epidemiology
TAO is the most common disease affecting the orbit.[8] It is detectable in approximately 25% of unselected patients with Graves’ disease if eyelid signs are excluded, and 40% if eyelid signs are included.[9,10] TAO patients are older than patients with Graves’ hyperthyroidism without orbitopathy.[11] The estimated incidence of GO in the general population is 16 females and 3 males per 100,000 person years,[12] with severe forms accounting for no more than 3–5% of the cases. Tellez et al. reported a 6.4 times risk for development for orbitopathy in Europeans compared to Asians. They also found that the prevalence of TAO in patients with hyperthyroidism was significantly higher in Europeans (42%) compared to Asians (7.7%).[13]
Although TAO is more common in women, the proportion of men increases as severity increases. The female to male ratio was 9.3:1 in patients with mild ophthalmopathy, 3.2:1 in those with moderate ophthalmopathy, and 1.4:1 with severe ophthalmopathy.[9–12] The risk and severity of ophthalmopathy in patients with Graves’ disease may be increased by several other factors including tobacco use, genetics, type of treatment for hyperthyroidism, TSH receptor antibody levels, advanced age, and stress.[14] Cigarette smoking is the strongest modifiable risk factor for developing TAO. There is strong evidence for a causal association between smoking and development of TAO.[13,15]
Other related autoimmune diseases including myasthenia gravis, which is 50 times more common in patients with TAO when compared to normal population, signify worse prognosis.[14] Similarly, patients with TAO and diabetes mellitus seem to have a higher incidence of dysthyroid optic neuropathy (DON).[16,17]
Pathogenesis
Autoimmunity
The increase in size of the extraocular muscles and orbital fat results from interaction between orbital fibroblast, cytokines, immune cells, autoantibodies, environmental and genetic factors.[18] The question of which antigen(s) are involved in TAO is still unknown, but because of the unique association of TAO with hyperthyroidism, it is hypothesized that the thyroid and orbital tissue share a common antigen. These antigens could be throglobulin, the TSH receptor, insulin like growth factor (IGF-1) receptor, or extraocular muscle antigens.
Lehman and colleagues summarized a plausible pathway for fibroblast activation in TAO.[19] They proposed that binding and activation of orbital fibroblasts by autoantibodies triggers thyroid eye disease. Activated orbital fibroblasts release chemokines that recruit T-lymphocytes into the orbit. These lymphocytes then interact with fibroblasts, potentially activating each other, further promoting cytokine production and secretion of T-cell activating factors. The interaction of fibroblasts with T cells results in the deposition of extracellular matrix molecules, fibroblast proliferation, and adipogenesis [Fig. 1].
Figure 1.
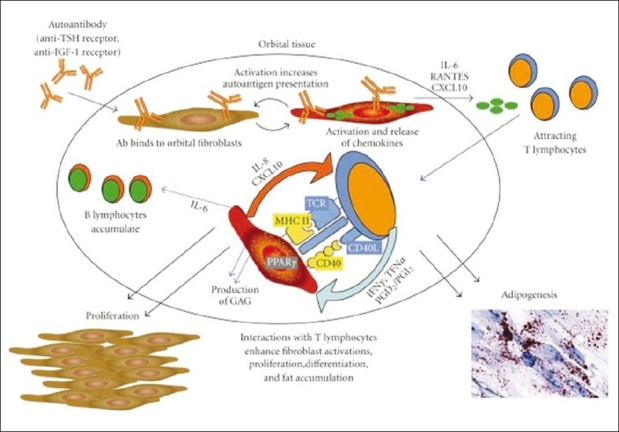
According to Lehmann et al.,[18] TED is triggered by binding and activation of orbital fibroblasts by autoantibodies. Activated orbital fibroblasts release chemokines which recruit T lymphocytes into the orbit. These lymphocytes then interact with fibroblasts, potentially activating each other, further promoting cytokine production and secretion of T cell activating factors by the fibroblasts. The interactions of fibroblasts with T cells result in the deposition of extracellular matrix molecules, fibroblast proliferation, and fat accumulation
Smoking
Smoking increases the incidence and severity of GO. Graves’ disease patients who smoke have a 5 times higher risk of developing TAO than those who do not.[14] Cawood and colleagues have established that orbital fibroblasts when exposed to cigarette extract have a dose-dependent statistically significant increase in GAGs’ production and adipogenesis.[20] There is evidence to suggest that smoking cessation reduces the risk of worsening of the orbitopathy, increasing the chance of having a favorable response to treatment.[21]
Genetic predisposition
Genetic factors may play a role in the pathogenesis of Graves’ disease. Twenty to sixty percent of affected individuals have a positive family history of thyroid disease. A population-based study of Danish monozygotic twins showed a 35% concordance rate.[22] Patients with Graves’ disease also express certain human leukocyte antigens (HLAs) more often than control subjects without the disease. HLA-B8, DR3, and DQA1*0501 haplotypes may increase susceptibility to the disease, and HLA-DR β1*07 may offer protection.[23] Akaishi et al.[24] studied the frequency of the class II major histocompatibility complex (MHC) HLA alleles in 81 Brazilian TAO patients and 161 normal controls. TAO patients with major extraocular muscle involvement were found to have a higher frequency of the HLA-DRB1*16 allele, whereas patients with minor extraocular muscle involvement were found to have a higher frequency of the HLA-DRB1*03 allele.
Clinical Manifestations
Approximately 80% of cases of TAO occur in association with hyperthyroidism, yet the onset may not coincide with the onset of the hyperthyroid state. In relation to hyperthyroidism, TAO may present well before the onset of thyroid dysfunction, during thyroid dysfunction, or when the patient is euthyroid following therapy.[25] Five to ten percent of patients with TAO do not develop hyperthyroidism and are called euthyroid TAO,[2] and 10% of TAO patients have primary autoimmune hypothyroidism.[26]
The most frequent sign in TAO is eyelid retraction, which affects 90–98% of patients[27,28] and frequently varies with attentive gaze[29] (Kocher's sign). Contour of the retracted upper eyelid often shows lateral flare, an appearance that is almost pathognomic for TAO.[30] Lid retraction is multifactorial and is due to increased sympathetic stimulation of Muller's muscle, contraction of the levator muscle, and scarring between the lacrimal gland fascia and levator, which specifically gives rise to the lateral flare.[31,32] The excursion of the upper eyelid often lags behind eyeball movement on vertical downward pursuit (lid lag) and remains high. Another common finding in patients with TAO is incomplete eyelid closure (lagophthalmos). Most patients develop exposure symptoms (foreign body senation, grittiness, photophobia, and lacrimation). These are secondary to the wide palpebral aperture combined with poor blinking, leading to increased tear evaporation.[33]
The inflammation and secondary GAG deposition previously described, causes tissue swelling resulting in proptosis, visible edema, and erythema. In the muscles, this leads to dysfunction due to failure of relaxation limiting movement, causing diplopia.
Orbital swelling at the apex can cause pressure on the optic nerve leading to DON. DON is only seen in severe disease with crowding of the orbit apex by enlarged extraocular muscles and it affects only 5% of clinical TAO patients.[14] Less common signs include superior limbic keratoconjunctivitis.
Disease Activity and Severity
During the course of TAO, the disease passes through several phases. From the onset, the first phase involves worsening of symptoms and signs in the active/inflammatory phase. Phases of gradual improvement in the inflammatory signs and symptoms follow until eventually no further changes occur. Permanent abnormalities in both function and appearance may remain in the stable inactive state.
Over the past decade, the concepts of disease severity and activity pertaining to thyroid eye disease have been defined more explicitly, although difficulties in definition and assessment remain. “Active” disease implies the presence of inflammatory features and suggests the potential for response to anti-inflammatory treatments. “Inactive” disease defines the phase when no inflammation is present, yet residual fibrosis and its secondary effects persist. In the inactive phase, only surgical treatment can alter the outcome [Fig. 2a and b].
Figure 2.

(a) Image of a patient with inactive disease showing no inflammation but severe eye lid retraction; (b) image of a patient showing active disease as manifested by eyelid hyperemia, eyelid edema, conjunctval injection, and caruncular edema
Hence, activity refers to presence of inflammation while severity of GO describes the degree of functional or cosmetic deficit at any stage.[31] It is important to determine the phase of GO for formulating an appropriate management plan. This is because immunomodulation therapy can be only effective while there is active inflammation.[8,31]
Vision, Inflammation, Strabismus, and Appearance Classification for Grave's Orbitopathy
One of the challenges in GO is to classify and grade its various clinical manifestations. Most ophthalmologists are familiar with Dr. Werner's NO SPECS classification that graded various symptoms and signs associated with the disease.[34] In 1987, Drs Bahn and Gorman emphasized the importance of using objective and reproducible criteria when evaluating therapies.[35] In 1989, Mourits, Koorneef, Wiersinga, and colleagues in The Netherlands introduced a Clinical Activity Score (CAS) to stage and grade the inflammatory phase of the disease.[36]
Dolman and Rootman devised a classification system based on the International working group's suggestion based on four disease endpoints that can be used in the office setting to record changes and to guide and assess therapy.[37] These clinical points include Vision, Inflammation, Strabismus, and Appearance (VISA)/exposure; these can be remembered by the acronym VISA. Each section records subjective and measurable objective inputs that aid in planning ancillary testing and treatment. The VISA classification helps direct appropriate management for patients with GO in a logical sequence, depending on which aspects of the disease are affecting them at any point in the course of their disease [Table 1].
Table 1.
Vision, Inflammation, Strabismus, and Appearance Classification
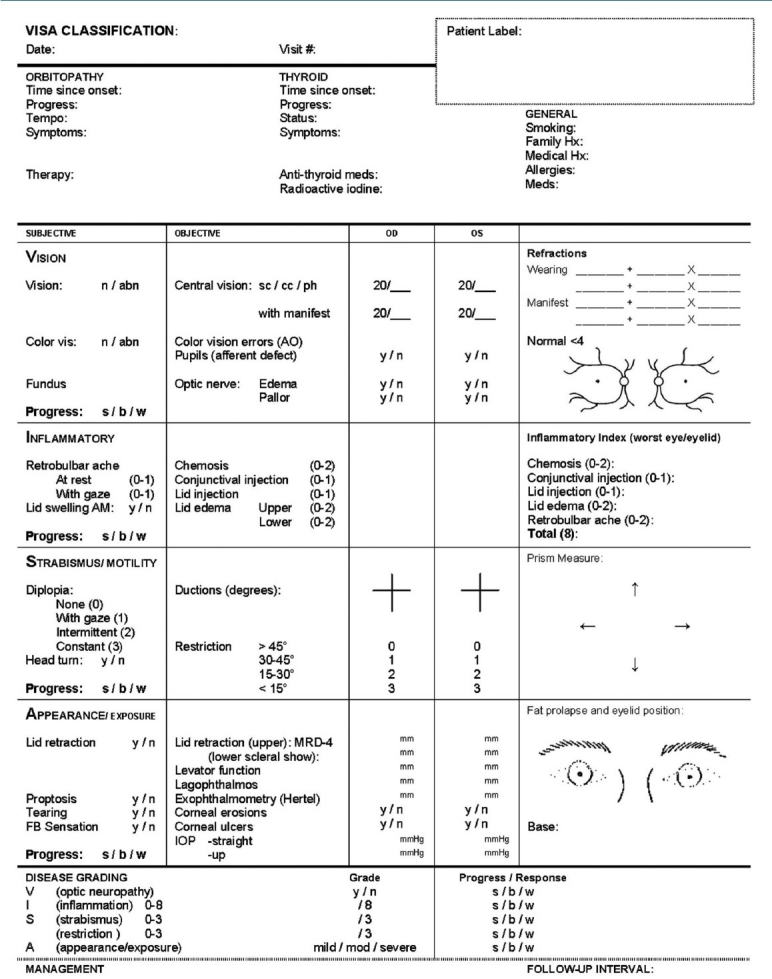
Vision
The primary goal of this section is to rule out optic neuropathy. Subjectively, this is described early on as episodes of graying out with and without color desaturation. On examination, abnormalities in visual acuity, color vision assessment, relative afferent papillary defect, or peripheral visual field assessment may be detected.
Inflammation
The CAS, described and validated by Mourits and the Amsterdam Orbitopathy group, was modified and used to grade the severity of activity. The CAS includes pain, redness, swelling, and impaired visual function, which may signal acute inflammation. The CAS consists of two conjunctival signs, two eyelid signs, and two orbital signs. Each of these signs is assigned points depending on the severity at presentation [Table 1]. The maximum score is thus 8. The worst scores from any of the four eyelids are recorded. A score of 3 or less is considered as inactive and 4 or more is active eye disease and thus is supposedly more likely to respond to immunosuppression. The disadvantage of CAS is it is still very subjective in nature with a large inter-observer variation. The advantage of CAS is it is inexpensive and can be done instantly in a clinic.
Strabismus
The symptoms for strabismus include a progression from no diplopia, diplopia in horizontal or vertical gaze, intermittent diplopia in primary gaze, and constant diplopia in primary gaze. Ocular ductions can be graded from 0° to >45° in four directions, using the Hirschberg principle. Strabismus can be measured objectively by prism cover testing in different gaze directions.
Appearance/exposure
Objective measures of appearance change include eyelid retraction, proptosis, and documentation of redundant skin and fat prolapse. Measures of exposure include corneal staining or ulceration. Photographs can document the appearance changes.
Orbital Imaging
Computed tomography (CT) is the most commonly utilized imaging technique for evaluating GO. CT is more sensitive than magnetic resonance imaging (MRI) in identifying enlarged extraocular muscles.[38] Findings on CT scanning may include muscle belly enlargement that typically spares the tendinous insertions, an apparent increase in orbital fat volume, and crowding of the optic nerve at the orbital apex.
Imaging studies may be particularly helpful when radiation therapy or decompressive surgery is planned, as they allow the degree of extraocular muscle and orbital fat involvement to be defined and sinus and skull base anatomy to be delineated clearly before intervention.
Treatment
General considerations
From the endocrine perspective, the goal of treatment for patients with Graves’ disease is the achievement of a euthyroid state. Patients should be counseled regarding the risks of smoking and the benefits of smoking cessation.
The decision on whether ophthalmopathy must be treated and requires what type of treatment relies on activity and severity of the disease [Table 2]. The sequence of the sections (V-I-S-A) described earlier reflects the order in which the problems should be managed.
Table 2.
Suggested treatment for Graves Ophthalmopathy as function of disease severity and activity
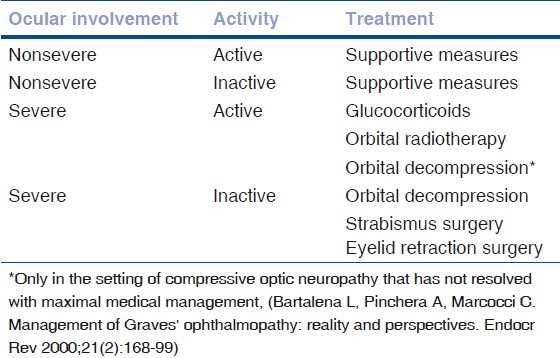
Vision dysfunction from optic neuropathy is the first priority and, depending on whether inflammation is present, might be treated with corticosteroids, radiotherapy, and/or orbital decompression. Inflammation is the next priority and may be treated with conservative measures, corticosteroids, steroid-sparing immunosuppressives and/or radiotherapy. Strabismus and appearance changes are usually managed medically and expectantly (with patching or Fresnel prisms) until the signs of inflammation and disease progression have subsided. Once this has occurred, strabismus can be managed with ground-in prisms or surgery, whereas proptosis, eyelid retraction, dermatochalasis, and fat prolapse can be managed surgically [Fig. 3].
Figure 3.
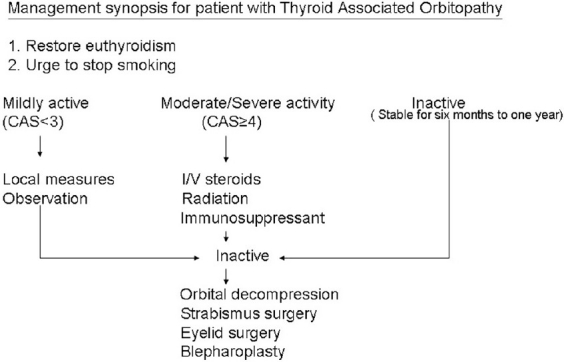
Management synopsis for patients with thyroid orbitopathy
Most patients with Graves’ disease have mild ocular manifestation. Simple local supportive measures are usually sufficient to obtain symptomatic relief [Table 3].
Table 3.
Local supportive measures for Thyroid associated Orbitopathy
Glucocorticoids
Glucocorticoids have been employed with the rationale for their anti-inflammatory and immunosuppressive actions.[39] In a review by Rajendram et al., glucocorticoids’ response rate has been found to range from 63 to 77%.[40] Higher effectiveness and fewer side effects of intravenous glucocorticoids compared to oral have resulted in IV steroids as the mainstay of treatment.[41,42] The cumulative dose of IV steroids should be no more than 6–8 g.[14] Some centers recommended routine liver assessment during treatment with IV steroids to rule out liver toxicity during and after treatment. Recurrences are not infrequent, thus repeated dosing is often required.
Radiation therapy
Evidence regarding the efficacy of radiation therapy in the management of GO is limited, owing to methodologic weaknesses of available studies. The rationale for the use of radiotherapy for TAO resides both in its nonspecific anti-inflammatory effect and in the high radiosensitivity of lymphocytes infiltrating the orbit.[43] Orbital radiotherapy is effective in patients who have active eye disease with recent progression. Patients with inactive GO do not respond to irradiation.[44] The most common delivered dose is 20 Gy per eye; this cumulative dose is fractionated over a 2-week period. Orbital radiotherapy may be associated with transient exacerbations of inflammation, but this can typically be avoided with co-coverage with glucocorticoids. With modern techniques, there seems to be no increased risk of cataract, or secondary malignancies, and only a remote risk of retinopathy.[45] In patients with diabetes mellitus, irradiation should be considered as a relative contraindication. Even though the efficacy of radiation therapy has been recently questioned, it remains widely used.[46]
Steroid-sparing immunosuppressive drugs
The autoimmune nature of TAO prompted the attempt to use steroid-sparing immunosuppressive drugs for this disease. Cyclosporine has been thoroughly evaluated in the management of GO. It affects both cell-mediated and humoral immune reactions. But the effect of cyclosporine given as monotherapy was inferior to prednisone. A few controlled studies have proven that the use of cyclosporine in combination with prednisone is more effective than monotherapy with prednisone alone.[47,48] Regular monitoring for side effects during the course of cyclosporine is required while a patient is on treatment.
Methotrexate is given in doses of 5–25 mg once per week. It does not have randomized controlled trial data, but a case series[49] and the authors’ experience suggest this to be a promising drug.
Surgical Intervention
The indications for surgical intervention in thyroid-related orbitopathy include optic neuropathy, diplopia, corneal exposure, and cosmesis. Broadly speaking, surgical procedures may be directed toward orbital decompression, strabismus repair, and the correction of eyelid abnormality. Traditionally, orbital decompression, if required, is performed initially, followed by strabismus surgery and then eyelid repair. This is because the nature and degree of strabismus may change after orbital surgery, and lid position may be altered following strabismus repair.
The timing of surgery is of significance. Decompression may be necessary on an urgent basis for compressive optic neuropathy or severe proptosis with corneal ulceration refractory to other treatment measures. Yet, most decompression surgery is performed when a patient has been stable in the inactive state for at least 6–8 months.[14]
Orbital decompression
Any surgical procedure that enlarges the bony orbit and/or removes the orbital fat is defined as orbital decompression. A customized decompression depending on the specifics of each patient provides the highest quality of care. At present, the medial wall, the orbital floor, and/or the lateral wall continue to be addressed during bony decompression surgery [Fig. 4a and b].[14] Preserving the medial orbital strut between the ethmoid cavity and the orbital floor may minimize the risk of globe dystopia and diplopia.[50] The combination of bony decompression associated with fat removal has been gaining popularity in view of the low risks associated with fat decompression.[51,52]
Figure 4.
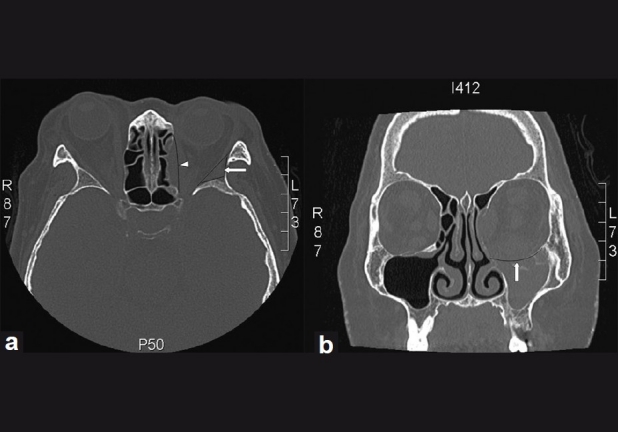
(a) CT scan showing the part of the posterolateral wall removed in lateral wall decompression (white arrow) and the medial wall osteotomy (white arrow head); (b) CT scan showing the orbital floor osteotomy (white arrow) for inferior wall decompression
Eye muscle surgery
Ocular motility disorders in GO are typically due to a restrictive myopathy, and thus are typically non-concomitant. Usually, in TAO, extraocular muscle involvement is characterized by accumulation of inflammatory cells and fluid. Later, the muscle is replaced by fibrous tissue, which makes the muscle stiff and inextensible. Due to the often incomitant nature of stabismus, surgery in TAO is often aimed at resolution of diplopia in primary position and downgaze. Surgery should be performed on a patient who does not have active thyroid disease for at least 6 months, and typically involves release of the restricted muscle by recession rather than resection. The use of adjustable sutures is strongly recommended due to the variability in fibrosis, resulting in unpredictable results.
Eyelid surgery
The most common indication for lid surgery is upper lid retraction. Treatment consists of a graded Muller's and levator aponeurosis weakening. Criterion for successful correction is covering of 1–2 mm of the superior cornea. Lower lid lengthening is indicated in lower lid retraction. Recession of lower lid retractors alone is insufficient to correct more than 1 mm of lid retraction and an interposition graft or spacer is needed if there is significant lower lid retraction.
Blepharoplasty
Blepharoplasty is the final surgical procedure in the rehabilitation of the TAO patient. Skin excision in the lower lid should be done carefully to avoid ectropion and/or lower lid retraction.
Conclusion
TAO is a self-limiting autoimmune disease associated mainly with hyperthyroidism, but also with hypothyroid and euthyroid states. There are two distinct stages of the disease, an active inflammatory stage followed by inactive quiescent stage. There are no effective means of preventing the disease or reliably altering its course. Current therapeutic options include local supportive measures, corticosteroids, external beam radiation and steroid-sparing immunosuppressive agents for reducing the inflammation during active disease, and surgery for correcting the residual abnormalities secondary to fibrosis in the inactive state of the disease.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Prabhakar BS, Bahn RS, Smith TJ. Current perspective on the pathogenesis of Graves’ disease and ophthalmopathy. Endocr Rev. 2003;24:802–35. doi: 10.1210/er.2002-0020. [DOI] [PubMed] [Google Scholar]
- 2.Burch HB, Wartofsky L. Graves’ ophthalmopathy: Current concepts regarding pathogenesis and management. Endocr Rev. 1993;14:747–93. doi: 10.1210/edrv-14-6-747. [DOI] [PubMed] [Google Scholar]
- 3.Bahn RS, Heufelder AE. Pathogenesis of Graves’ ophthalmopathy. N Engl J Med. 1993;329:1468–75. doi: 10.1056/NEJM199311113292007. [DOI] [PubMed] [Google Scholar]
- 4.Feldon SE, Weiner JM. Clinical significance of extraocular muscle volumes in Graves’ ophthalmopathy: A quantitative computed tomography study. Arch Ophthalmol. 1982;100:1266–9. doi: 10.1001/archopht.1982.01030040244006. [DOI] [PubMed] [Google Scholar]
- 5.Nunery WR, Nunery CW, Martin RT, Truong TV, Osborn DR. The risk of diplopia following orbital floor and medial wall decompression in subtypes of ophthalmic Graves’ disease. Ophthal Plast Reconstr Surg. 1997;13:153–60. doi: 10.1097/00002341-199709000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Smith TJ, Hoa N. Immunoglobulins from patients with Graves’ disease induce hyaluronan synthesis in their orbital fibroblasts through the self-antigen, insulin-like growth factor-I receptor. J Clin Endocrinol Metab. 2004;89:5076–80. doi: 10.1210/jc.2004-0716. [DOI] [PubMed] [Google Scholar]
- 7.Wiersinga WM, Prummel MF. Pathogenesis of Graves’ ophthalmopathy--Current understanding. J Clin Endocrinol Metab. 2001;86:501–3. doi: 10.1210/jcem.86.2.7338. [DOI] [PubMed] [Google Scholar]
- 8.Rootman J. A Multidisciplinary Approach. Hagerstown: Lippincott Williams and Wilkins; 2003. Diseases of the Orbit. [Google Scholar]
- 9.Bartalena L, Pinchera A, Marcocci C. Management of Graves’ ophthalmopathy: Reality and perspectives. Endocr Rev. 2000;21:168–99. doi: 10.1210/edrv.21.2.0393. [DOI] [PubMed] [Google Scholar]
- 10.Wiersinga WM, Bartalena L. Epidemiology and prevention of Graves’ ophthalmopathy. Thyroid. 2002;12:855–60. doi: 10.1089/105072502761016476. [DOI] [PubMed] [Google Scholar]
- 11.Perros P, Kendall-Taylor P. Natural history of thyroid eye disease. Thyroid. 1998;8:423–5. doi: 10.1089/thy.1998.8.423. [DOI] [PubMed] [Google Scholar]
- 12.Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, et al. The incidence of Graves’ ophthalmopathy in Olmsted County, Minnesota. Am J Ophthalmol. 1995;120:511–7. doi: 10.1016/s0002-9394(14)72666-2. [DOI] [PubMed] [Google Scholar]
- 13.Tellez M, Cooper J, Edmonds C. Graves’ ophthalmopathy in relation to cigarette smoking and ethnic origin. Clin Endocrinol (Oxf) 1992;36:291–4. doi: 10.1111/j.1365-2265.1992.tb01445.x. [DOI] [PubMed] [Google Scholar]
- 14.Wiersinga WM, Kahaly GJ. Graves orbitopathy: A multidisciplinary approach. Basel: Karger; 2007. [Google Scholar]
- 15.Hagg E, Asplund K. Is endocrine ophthalmopathy related to smoking? Br Med J. 1987;295:634–5. doi: 10.1136/bmj.295.6599.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalmann R, Mourits MP. Diabetes mellitus: A risk factor in patients with Graves’ orbitopathy. Br J Ophthalmol. 1999;83:463–5. doi: 10.1136/bjo.83.4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neigel JM, Rootman J, Belkin RI, Nugent RA, Drance SM, Beattie CW, et al. Dysthyroid optic neuropathy. The crowded orbital apex syndrome. Ophthalmology. 1988;95:1515–21. doi: 10.1016/s0161-6420(88)32978-7. [DOI] [PubMed] [Google Scholar]
- 18.Garrity JA, Bahn RS. Pathogenesis of graves ophthalmopathy: Implications for prediction, prevention, and treatment. Am J Ophthalmol. 2006;142:147–53. doi: 10.1016/j.ajo.2006.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lehmann GM, Garcia-Bates TM, Smith TJ, Feldon SE, Phipps RP. Regulation of lymphocyte function by PPARgamma: Relevance to thyroid eye disease-related inflammation. PPAR Res. 2008;2008:895901. doi: 10.1155/2008/895901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cawood TJ, Moriarty P, O’Farrelly C, O’Shea D. Smoking and thyroid-associated ophthalmopathy: A novel explanation of the biological link. J Clin Endocrinol Metab. 2007;92:59–64. doi: 10.1210/jc.2006-1824. [DOI] [PubMed] [Google Scholar]
- 21.Krassas GE, Wiersinga W. Smoking and autoimmune thyroid disease: The plot thickens. Eur J Endocrinol. 2006;154:777–80. doi: 10.1530/eje.1.02157. [DOI] [PubMed] [Google Scholar]
- 22.Brix TH, Kyvik KO, Christensen K, Hegedus L. Evidence for a major role of heredity in Graves’ disease: A population-based study of two Danish twin cohorts. J Clin Endocrinol Metab. 2001;86:930–4. doi: 10.1210/jcem.86.2.7242. [DOI] [PubMed] [Google Scholar]
- 23.Lee HB, Rodgers IR, Woog JJ. Evaluation and management of Graves’ orbitopathy. (6).Otolaryngol Clin North Am. 2006;39:923–42. doi: 10.1016/j.otc.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 24.Akaishi PM, Cruz AA, Silva FL, Rodrigues Mde L, Maciel LM, Donadi EA. The role of major histocompatibility complex alleles in the susceptibility of Brazilian patients to develop the myogenic type of Graves’ orbitopathy. Thyroid. 2008;18:443–7. doi: 10.1089/thy.2007.0194. [DOI] [PubMed] [Google Scholar]
- 25.Wiersinga WM, Smit T, van der Gaag R, Koornneef L. Temporal relationship between onset of Graves’ ophthalmopathy and onset of thyroidal Graves’ disease. J Endocrinol Invest. 1988;11:615–9. doi: 10.1007/BF03350193. [DOI] [PubMed] [Google Scholar]
- 26.Gleeson H, Kelly W, Toft A, Dickinson J, Kendall-Taylor P, Fleck B, et al. Severe thyroid eye disease associated with primary hypothyroidism and thyroid-associated dermopathy. Thyroid. 1999;9:1115–8. doi: 10.1089/thy.1999.9.1115. [DOI] [PubMed] [Google Scholar]
- 27.Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, et al. Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol. 1996;121:284–90. doi: 10.1016/s0002-9394(14)70276-4. [DOI] [PubMed] [Google Scholar]
- 28.Saks ND, Burnstine MA, Putterman AM. Glabellar rhytids in thyroid-associated orbitopathy. Ophthal Plast Reconstr Surg. 2001;17:91–5. doi: 10.1097/00002341-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Velasco e Cruz AA, Vagner de Oliveira M. The effect of Mullerectomy on Kocher sign. Ophthal Plast Reconstr Surg. 2001;17:309–15. doi: 10.1097/00002341-200109000-00002. discussion 15-6. [DOI] [PubMed] [Google Scholar]
- 30.Koornneef L. Eyelid and orbital fascial attachments and their clinical significance. Eye (Lond) 1988;2:130–4. doi: 10.1038/eye.1988.26. [DOI] [PubMed] [Google Scholar]
- 31.Dickinson AJ, Perros P. Controversies in the clinical evaluation of active thyroid-associated orbitopathy: Use of a detailed protocol with comparative photographs for objective assessment. Clin Endocrinol (Oxf) 2001;55:283–303. doi: 10.1046/j.1365-2265.2001.01349.x. [DOI] [PubMed] [Google Scholar]
- 32.Frueh BR, Musch DC, Garber FW. Lid retraction and levator aponeurosis defects in Graves’ eye disease. Ophthalmic Surg. 1986;17:216–20. [PubMed] [Google Scholar]
- 33.Gilbard JP, Farris RL. Ocular surface drying and tear film osmolarity in thyroid eye disease. Acta Ophthalmol (Copenh) 1983;61:108–16. doi: 10.1111/j.1755-3768.1983.tb01401.x. [DOI] [PubMed] [Google Scholar]
- 34.Werner SC. Classification of the eye changes of Graves’ disease. Am J Ophthalmol. 1969;68:646–8. doi: 10.1016/0002-9394(69)91246-x. [DOI] [PubMed] [Google Scholar]
- 35.Bahn RS, Gorman CA. Choice of therapy and criteria for assessing treatment outcome in thyroid-associated ophthalmopathy. Endocrinol Metab Clin North Am. 1987;16:391–407. [PubMed] [Google Scholar]
- 36.Mourits MP, Koornneef L, Wiersinga WM, Prummel MF, Berghout A, van der Gaag R. Clinical criteria for the assessment of disease activity in Graves’ ophthalmopathy: A novel approach. Br J Ophthalmol. 1989;73:639–44. doi: 10.1136/bjo.73.8.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dolman PJ, Rootman J. VISA Classification for Graves orbitopathy. Ophthal Plast Reconstr Surg. 2006;22:319–24. doi: 10.1097/01.iop.0000235499.34867.85. [DOI] [PubMed] [Google Scholar]
- 38.Polito E, Leccisotti A. MRI in Graves orbitopathy: Recognition of enlarged muscles and prediction of steroid response. Ophthalmologica. 1995;209:182–6. doi: 10.1159/000310609. [DOI] [PubMed] [Google Scholar]
- 39.Bartalena L, Marocci C, Bogazzi F, Bruno-Bossio G, Pinchera A. Glucocorticoid therapy of Graves’ ophthalmopathy. Exp Clin Endocrinol. 1991;97:320–7. doi: 10.1055/s-0029-1211086. [DOI] [PubMed] [Google Scholar]
- 40.Rajendram R, Lee RW, Potts MJ, Rose GE, Jain R, Olver JM, et al. Protocol for the combined immunosuppression and radiotherapy in thyroid eye disease (CIRTED) trial: A multi-centre, double-masked, factorial randomised controlled trial. Trials. 2008;9:6. doi: 10.1186/1745-6215-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kahaly GJ, Pitz S, Hommel G, Dittmar M. Randomized, single blind trial of intravenous versus oral steroid monotherapy in Graves’ orbitopathy. J Clin Endocrinol Metab. 2005;90:5234–40. doi: 10.1210/jc.2005-0148. [DOI] [PubMed] [Google Scholar]
- 42.Macchia PE, Bagattini M, Lupoli G, Vitale M, Vitale G, Fenzi G. High-dose intravenous corticosteroid therapy for Graves’ ophthalmopathy. J Endocrinol Invest. 2001;24:152–8. doi: 10.1007/BF03343835. [DOI] [PubMed] [Google Scholar]
- 43.Kahaly GJ, Roesler HP, Kutzner J, Kutzner J, Pitz S, Müller-Forell W, et al. Radiotherapy for thyroid-associated orbitopathy. Exp Clin Endocrinol Diabetes. 1999;107(Suppl 5):S201–7. doi: 10.1055/s-0029-1212186. [DOI] [PubMed] [Google Scholar]
- 44.Bartalena L, Marcocci C, Pinchera A. Orbital radiotherapy for Graves’ ophthalmopathy. J Clin Endocrinol Metab. 2004;89:13–4. doi: 10.1210/jc.2003-031769. [DOI] [PubMed] [Google Scholar]
- 45.Marcocci C, Bartalena L, Rocchi R, Marino M, Menconi F, Morabito E, et al. Long term safety of orbital radiotherapy for Grave's ophthalmopathy. J Clin Endocrinol Metab. 2003;88:3561–6. doi: 10.1210/jc.2003-030260. [DOI] [PubMed] [Google Scholar]
- 46.Bartley GB, Gorman CA. Perspective – Part 1: Then Mayo orbital radiotherapy for Graves’ ophthalmopathy (ORGO) study: Lessons learnt. Ophthal Plast Reconstr Surg. 2002;18:170–2. doi: 10.1097/00002341-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 47.Kahaly G, Schrezenmeir J, Krause U, Schweikert B, Meuer S, Muller W, et al. Cyclosporine and prednisone v. prednisone in treatment of Graves’ ophthalmopathy: A controlled, randomized and prospective study. Eur J Clin Invest. 1986;16:415–22. doi: 10.1111/j.1365-2362.1986.tb01016.x. [DOI] [PubMed] [Google Scholar]
- 48.Prummel MF, Mourits MP, Berghout A, Krenning EP, van der Gaag R, Koornneef L, et al. Prednisone and cyclosporine in the treatment of severe Graves’ ophthalmopathy. N Engl J Med. 1989;321:1353–9. doi: 10.1056/NEJM198911163212002. [DOI] [PubMed] [Google Scholar]
- 49.Smith JR, Rosenbaum JT. A role for methotrexate in the management of non-infectious orbital inflammatory disease. Br J Ophthalmol. 2001;85:1220–4. doi: 10.1136/bjo.85.10.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Goldberg RA, Shorr N, Cohen MS. The medical orbital strut in the prevention of postdecompression dystopia in dysthyroid ophthalmopathy. Ophthal Plast Reconstr Surg. 1992;8:32–4. doi: 10.1097/00002341-199203000-00005. [DOI] [PubMed] [Google Scholar]
- 51.Goldberg RA. The evolving paradigm of orbital decompression surgery. Arch Ophthalmol. 1998;116:95–6. doi: 10.1001/archopht.116.1.95. [DOI] [PubMed] [Google Scholar]
- 52.Unal M, Leri F, Konuk O, Hasanreisoglu B. Balanced orbital decompression combined with fat removal in Graves ophthalmopathy: Do we really need to remove the third wall? Ophthal Plast Reconstr Surg. 2003;19:112–8. doi: 10.1097/01.IOP.0000056145.71641.F5. [DOI] [PubMed] [Google Scholar]


