Abstract
Purpose:
To determine the systemic associations in retinal arterial occlusions (RAO) in young Indian individuals less than 40 years of age.
Materials and Methods:
Case records of 32 patients (35 eyes) of less than 40 years, with non-traumatic RAO were analysed. All patients underwent detailed ophthalmic and systemic evaluation including hemogram, lipid profile, coagulation profile, vasculitis screening, carotid Doppler, echocardiogram.
Results:
In the study 21 were males and 11 were females. The age ranged from 11-39 years (Mean 27.6 ± 8.43). Nine (28%) patients were below 20 years of age. Among 35 eyes, 28 (80%) had central retinal artery occlusion (CRAO), three (8.6%) had branch retinal artery occlusion (BRAO), two (5.7%) each had cilio-retinal (CLAO) and hemi-retinal artery occlusion (HRAO). Vision ranged from no perception of light to 20/20. On systemic evaluation, in 21 (65.6%) patients a hypercoagulable state was responsible for the RAO. Conditions leading to a hypercoagulable state included hyperhomocysteinemia (21.9%), hyperlipidemia (15.6%), anticardiolipin antibody (6.2%), antiphospholipid antibody (6.2%), polycythemia, thrombocytosis, protein S deficiency, use of oral contraceptives and renal disorder (3.1% each). Six (18.7%) patients had cardiac valvular defects. Vasculitis screening was positive in three (9.4%) patients. Two (6.2%) had isolated systemic hypertension. In two (6.2%) patients no abnormality could be detected.
Conclusion:
The systemic associations of RAOs in the Indian population were distinctly different from those reported in the Western population. Hyperhomocysteinemia was the commonest association found. Whereas associations reported in the Western population such as cardiac abnormalities, coagulation disorders, hemoglobinopathies and oral contraceptive use were uncommon.
Keywords: Hyperhomocysteinemia, retinal arterial occlusions, systemic associations, young age
Retinal artery occlusion (RAO) is mostly seen in the elderly with clinical findings suggestive of atheromatous emboli.[1] Among the numerous anecdotal reports of central retinal artery occlusion (CRAO) the earliest by von Graefe in 1859 described CRAO in a patient of endocarditis and multiple systemic emboli.[2] An estimated 0.85 per 10,000 patients over the age of 40 years are affected.[3] However, RAO is uncommon in the young population.[4,5] Information regarding risk factors in this age group is scanty. Various isolated case reports have reported a diverse and multifactorial etiology which includes cardiac valvular disorders and various vascular inflammatory disorders.[6] Only two major case series have been reported in patients younger than 40 years.[4,5] No reports are available regarding the risk factors in the Asian population. This retrospective study was done for the purpose of determining the clinical profile and etiological factors of RAO in young Indian individuals less than 40 years of age.
Materials and Methods
A retrospective record analysis of patients less than 40 years of age with RAO, presenting at a tertiary referral hospital between January 2004 and January 2009 was done. Patients with questionable diagnosis, history of trauma, age more than 40 years and incomplete investigative details were excluded.
Patients underwent a comprehensive medical and ophthalmic history and examination along with fundus fluorescein angiography (FFA) and thorough physical examination and cardiac evaluation. Investigations were done according to associated history and clinical findings. These included hemogram with erythrocyte sedimentation rate (ESR), lipid profile, renal function tests, vasculitis screening profile (Anti ds-DNA antibody, antihistone antibody, ANA, c-ANCA, p-ANCA), homocysteine levels, antiphospholipid antibody (Ab), anticardiolipin Ab, coagulation profile (Prothrombin time, APTT, bleeding time, clotting time, protein C and S levels), syphilis serology, ELISA for HIV, carotid Doppler, echocardiography, electrocardiogram and CT/MRI/MRA brain as and when needed.
Results
Over a period of five years, 32 patients of non-traumatic RAO were identified and their case records were studied. The age ranged from 11 to 39 years (Mean 27.62 ± 8.43 years, Median 28 years). Most of the patients (n=14, 44%) were aged between 31-40 years while nine (28%) patients were between 21-30 years of age. Nine (28%) patients were less than 20 years of age. In our study there were 21 (65.6%) males and 11 (34.4%) females. Bilateral involvement was found in three (10%) patients, while the right eye was involved in 19 (59%) patients and left eye in 10 (31%) patients.
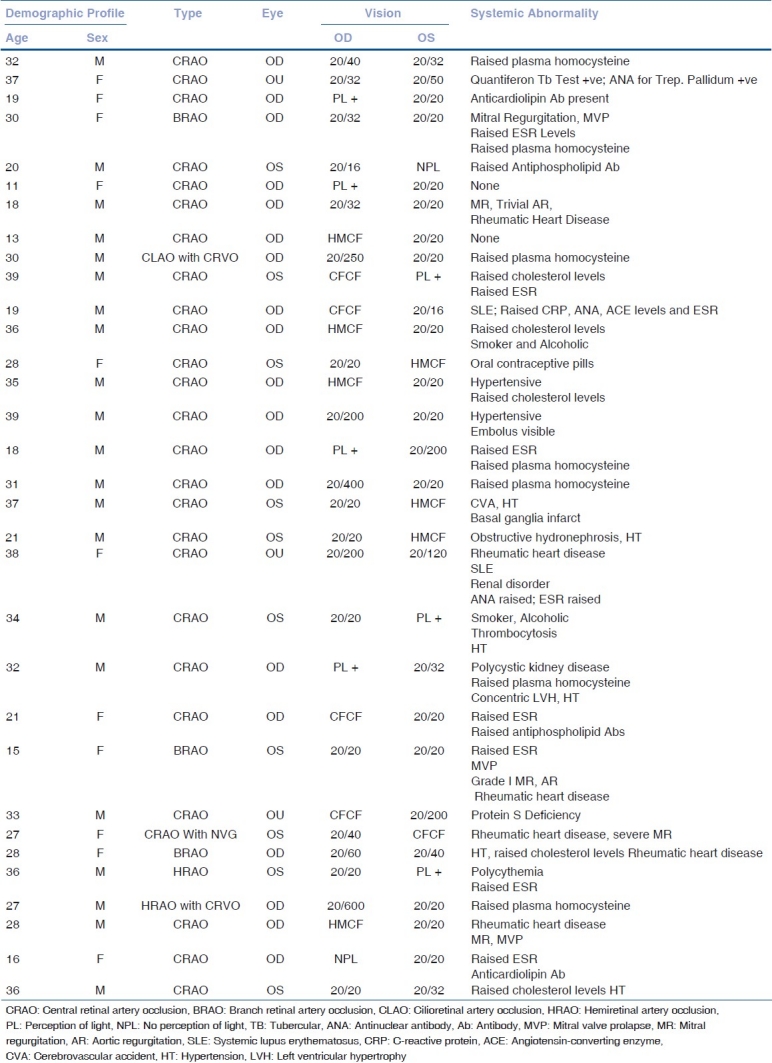
In 35 eyes with RAO, 28 (87.5%) had central retinal artery occlusion (CRAO), three (9.4%) had branch retinal artery occlusion (BRAO), two (6.2%) each had cilioretinal artery occlusion (CLAO) and hemiretinal artery occlusion (HRAO). The various associated systemic as well as ocular abnormalities are shown in Table 1.
Table 1.
Demographic profile and systemic abnormality in patients with retinal arterial occlusions
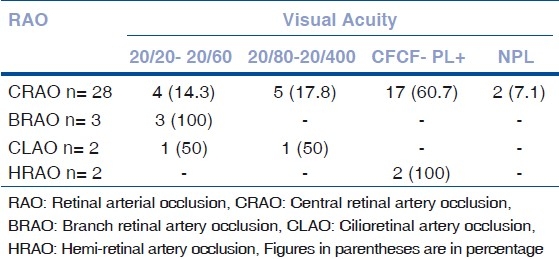
The visual acuity ranged from normal to no light perception [Table 2]. Out of the 28 eyes with CRAO, four eyes (14.3%) had good vision due to sparing of the cilioretinal artery. However, two eyes (7.2%) had no perception of light (NPL). All the three patients with BRAO had good vision between 20/20-20/60. Among the patients with CLAO, one patient had 20/32 vision due to foveal sparing while the second patient had poor vision due to associated central retinal vein occlusion (CRVO). Both the patients with HRAO had poor vision, due to choroidal infarction in one eye and associated CRVO in the other.
Table 2.
Visual status in patients with retinal arterial occlusion
Among the 32 patients with RAO, 94% patients complained of sudden, painless diminution of vision, 12.5% patients had severe headache while 9.4% had history of floaters. Only 3% patients reported transient diminution of vision. Relative afferent papillary defect (RAPD) was present in 65.6% of patients with RAO. One patient with CRAO also had 360° neo-vascularization of iris (NVI) with neovascular glaucoma (NVG).
All patients presented with common features of RAO which included retinal edema (80%), box-carring and retinal artery attenuation (77.1%), and cherry red spot (62.8%). Other features included disc pallor (31.4%), retinal hemorrhages (14.2%), disc edema (8.6%) and neovascularization (8.6%). Visible embolus was present only in one eye (2.8%). Table 3 lists the fundus findings.
Table 3.
Fundus findings in patients with retinal arterial occlusions
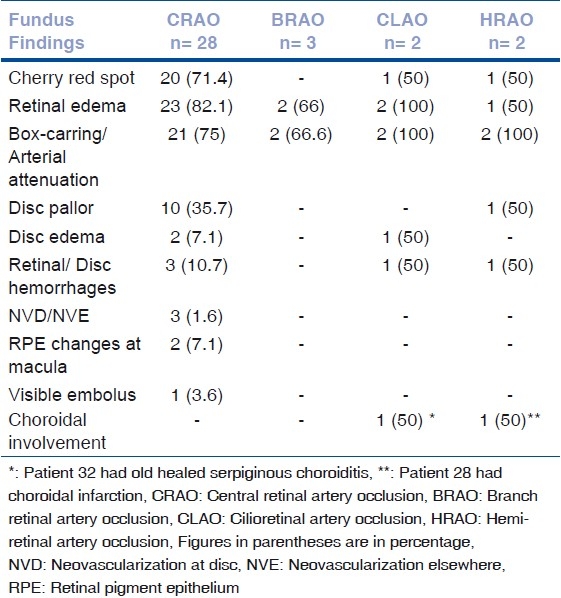
Table 4 illustrates the various systemic disorders present among these 32 patients. Hypercoagulable state was the most common, seen in 21 (65.6%) of 32 patients. Among all the disorders leading to hypercoagulable state, the commonest disorder noted was hyperhomocysteinemia in seven (21.9%) patients. Among these seven patients, in four patients no other abnormality was found except the hyperhomocysteinemia, despite extensive investigations. However, among the remaining three patients, one patient had associated raised ESR level, one patient had mitral valve prolapse (MVP), mitral regurgitation (MR) and a raised ESR and the third patient had a polycystic kidney, hypertension and left ventricular hypertrophy.
Table 4.
Systemic abnormalities in patients with retinal arterial occlusions*
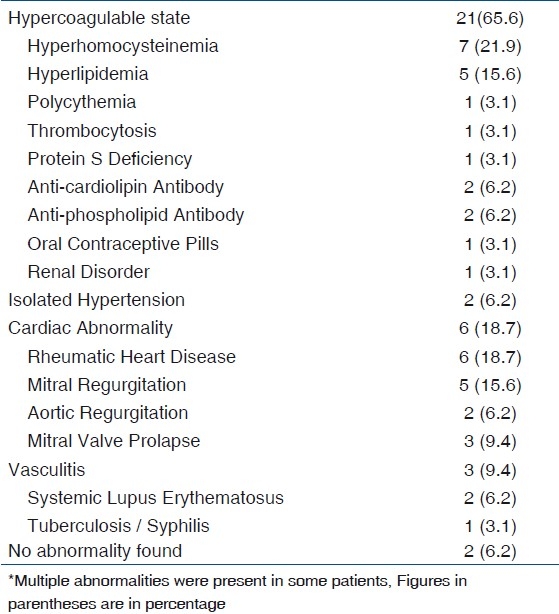
Hyperlipidemia was responsible for the hypercoagulable state in five patients (15.6%). Except for one, all the patients with hyperlipidemia also had hypertension. Among other entities leading to a hypercoagulable state, anticardiolipin antibody (Ab) and antiphospholipid antibody was present in two patients (6.2%) each. One patient (3.1%) each had polycythemia with hypertension, thrombocytosis with hypertension, obstructive hydronephrosis with hypertension and protein S deficiency. In our study, only one patient (3.1%) had a history of oral contraceptive pills (OCP) intake.
Isolated hypertension was noted in two patients (6.2%). Among these two patients, patient no. 15 had a visible embolus in the infero-temporal branch of the central retinal artery. Patient no. 18 had a history of cerebrovascular attack with basal ganglia infarcts reported on MRI scan.
Six patients (18.7%) had cardiac abnormality due to the presence of rheumatic heart disease. Valvular disease was present in all these patients. None of the patients had atrial myxoma.
Vasculitis was seen in three patients (9.4%). Systemic lupus erythematosus (SLE) was the causative factor in two patients while one patient with vasculitis tested positive for both Quantiferon tubercular test and antinuclear antibody (ANA) for Treponema pallidum.
In two patients (6.2%) no abnormality could be detected despite extensive investigations.
Discussion
The most common cause of RAO is embolic obstruction, with carotid artery being the commonest source of endogenous emboli. Other mechanisms include exogenous emboli, thrombotic, vasospastic and vasculitic events. Usually, RAO occurs in the mean age group of 60-65 years and predominantly affects males.[7,8] A few studies also show that RAOs occur in young patients and the etiology is multifactorial.[4,5] Our study shows males to be more affected (65.6%) than females (34.4%). Brown et al.,[4] showed a nearly equal number of males and females involved while Greven et al.,[5] showed a female predominance.
In our study, hypercoagulable state was found to be a major cause responsible for 65.6% of retinal artery occlusions. Among all the conditions leading to a hypercoagulable state, hyperhomocysteinemia was the commonest cause found in 21.9% patients. Homocysteine is an amino acid derived from methionine, which can be converted into cysteine. The metabolic pathways involving homocysteine require vitamin B12, vitamin B6 and folate for proper functioning. Various reports on hyperhomocysteinemia depict that arterial as well as venous vessels are involved in the disease.[9,10] The mechanism by which homocysteine causes vascular occlusion is presumed to be involving endothelial damage with increased endothelial tissue factor expression, activation of coagulation cascade, increased platelet adhesiveness and conversion of low-density lipoprotein cholesterol into smaller forms.[11] In most of the premature arteriosclerotic patients with hyperhomocysteinemia, methionine loading test shows a low cystathione synthase activity.[12] Elevated homocysteine and low methionine were found to be the risk factors for retinal venous occlusions in Indian population.[13] Unlike studies by Brown et al.,[4] and Greven et al.,[5] our study shows a larger number of patients with hyperhomocysteinemia. Table 5 shows the comparative data.
Table 5.
Comparison with other studies
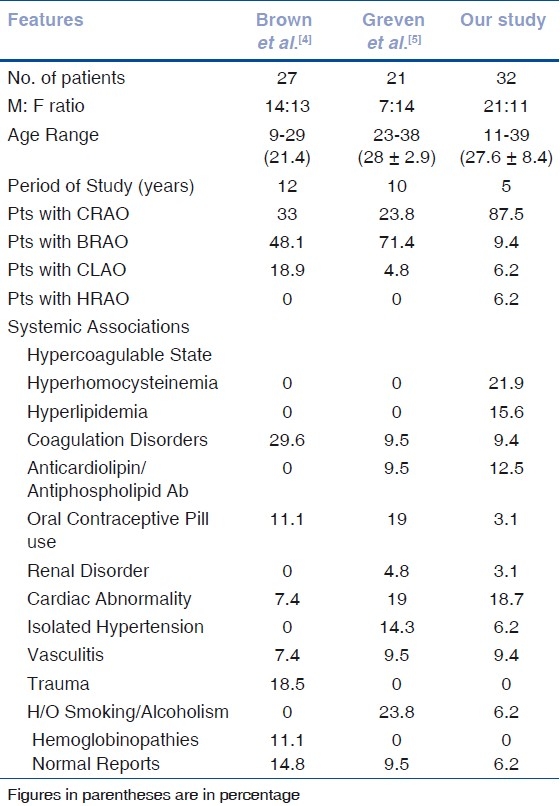
Hyperlipidemia was found in 15.6% patients in our study while there were none in either of the other two studies. High plasma lipoprotein concentration is an independent risk factor for atherosclerosis and thrombosis.[14] Impaired fibrinolysis and atherogenesis induced by lipoprotein-A may play a role in the pathophysiology of CRAO.[15]
Coagulation disorders also play role in the pathogenesis of vascular occlusions. In their study Brown and associates[4] found 29.6% patients with coagulation disorder while in the study by Greven et al.,[5] 9% patients had coagulation disorders. In our study also 9% patients had coagulation disorders. Protein C and S are vitamin K-dependent plasma proteins that inhibit the clotting cascade at Factors V and VIII level. These can be inherited as autosomal dominant disorders or acquired due to liver disease.[16,17] Platelet coagulant activity has been related to RAO in the absence of other predisposing factors like HT and hyperlipoproteinemia.[18] The patients included in our study had protein S deficiency, thrombocytosis and polycythemia.
Antiphospholipid antibody syndrome occurs in people with either lupus anticoagulant or antibodies to phospholipids.[19] A study by Suvajach et al.,[20] showed that ocular arterial and venous occlusions were common in patients with antiphospholipid antibody syndrome and they suggest that all young patients with retinal artery occlusion should be investigated for the same. In our study 12.5% patients had antiphospholipid antibodies and anticardiolipin antibodies while Greven and associates[5] reported 9.5% patients with antiphospholipid antibodies.
Use of oral contraceptive pills (OCP) and hormonal therapy are associated with numerous ocular disorders, retinal vascular occlusion among them.[21,22] The use of OCP is more frequent in the Western population, therefore studies by Brown et al.,[4] and Greven et al.,[5] show a larger number of female patients with RAO and a history of OCP use (11.1% and 19% respectively) as compared to our study (3.1%).
A case report on idiopathic renal infarction causing CRAO has been published even though much data to support the role of kidney disorders causing retinal vascular occlusion is unavailable.[23] A comparable number of patients in our study (3.1%) and in that by Greven et al.,[5] (4.8%) were found to have renal disorder leading to RAO.
Cardiac causes for the occurrence of RAO have been documented. Cardiac abnormalities were found in six (18.7%) patients in our study. Among them mitral regurgitation was found in five (15.6%) and mitral valve prolapse in three (9.4%) patients. These have been implicated as etiological factors for vascular occlusions.[24] The vascular occlusion follows a calcific, platelet or fibrinous embolus. But none of our patients with cardiac abnormality had any visible embolus. Rheumatic heart disease (RHD) has also been considered as an etiological factor predisposing to retinal vascular occlusions.[25,26] In our study 18.7% patients had RHD.
RAO secondary to vasculitis has been encountered in many conditions. A study by Au and O’day has shown presence of retinal artery occlusion in 4.5% patients of systemic lupus erythematosus (SLE).[27] They further suggest that the incidence of retinal arterial occlusion was greater than venous occlusion (P=0.0338). Vasculitis was diagnosed to be the etiological factor in 9.4% patients in our study as compared to 7.4% and 9.5% in the other two studies.[4,5]
Smoking and alcoholism are considered as risk factors in the development of emboli causing retinal arterial occlusions. In a study by Hayreh and associates,[28] in patients who smoked, a high prevalence of RAO was seen. In this subgroup of patients, CRAO was common in males while BRAO was common in females.
Sickle cell disease is a major cause of thromoboembolic events in young patients.[29] It is imperative to do a hemoglobin electrophoresis in all young patients with RAO. Though sickle cell trait is a benign condition numerous case reports and studies show that under stress, hypoxia due to trauma or concomitant systemic disease it becomes a pathological factor.[30] Though none of the patients in our study had hemoglobinopathies 11% patients in the study by Brown and associates[4] had sickle cell disease.
Studies have shown that isolated hypertension is a major risk factor leading to vascular occlusions.[31,32] It is more pronounced in the elderly age group but the younger generation too is being affected with increased incidence of retinal vascular occlusions.[33] Our study had 6.2% patients with isolated hypertension as compared to 14.6% patients in the study by Greven and associates.[5]
Despite extensive investigations, in two patients (2.6%) there was no evidence of any systemic or ocular abnormality which could be accounted for the presence of retinal artery occlusion.
Conclusion
We found major differences in the causative factors responsible for retinal arterial occlusions in young Indian patients as compared to those seen in the Western population. The commonest cause of retinal arterial occlusion in young adults of Indian origin was found to be hyperhomocysteinemia. This was conspicuously absent in the two reported series from the Western population. The highly prevalent nutritional deficiency in the Indian subcontinent is likely responsible for the hyperhomocysteinemia. Ethnic variations may also be responsible. In contrast, coagulation disorders, cardiac abnormalities, hemoglobinopathies and oral contraceptive use were cited as the major causes of retinal arterial occlusions in the Western population. Further studies are warranted to analyze these ethnic differences in detail. It would be interesting to see whether any genetic predisposition to hyperhomocysteinemia and retinal arterial occlusions exists in the Indian population.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Kollarits CR, Lubow M, Hissong SL. Retinal Strokes: I: Incidence of carotid atheromata. JAMA. 1972;222:1273–5. doi: 10.1001/jama.222.10.1273. [DOI] [PubMed] [Google Scholar]
- 2.Von Graefe A. Ueber Embolie der Arteria centralis retinae als Ursache plotzlicher Erblindung. Albrecht von Graefes Arch Ophthalmol. 1859;5:136–57. [Google Scholar]
- 3.Rumelt S, Dorenboim Y, Rehany U. Aggressive systematic treatment for central retinal artery occlusion. Am J Ophthalmol. 1999;128:733–8. doi: 10.1016/s0002-9394(99)00359-1. [DOI] [PubMed] [Google Scholar]
- 4.Brown GC, Magargal LE, Shields JA, Goldberg RE, Walsh PN. Retinal arterial obstruction in children and young adults. Ophthalmology. 1981;88:18–25. doi: 10.1016/s0161-6420(81)35080-5. [DOI] [PubMed] [Google Scholar]
- 5.Greven CM, Slusher MM, Weaver RG. Retinal arterial occlusion in young adults. Am J Ophthalmol. 1995;120:776–83. doi: 10.1016/s0002-9394(14)72731-x. [DOI] [PubMed] [Google Scholar]
- 6.Gold D. Retinal arterial occlusion. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977;83:392–408. [PubMed] [Google Scholar]
- 7.Brown GC, Magargal LE. Central retinal artery occlusion and visual acuity. Ophthalmology. 1982;89:14–9. doi: 10.1016/s0161-6420(82)34853-8. [DOI] [PubMed] [Google Scholar]
- 8.Karjalainen K. Occlusion of the central retinal artery and retinal branch arterioles: A clinical, tonographic and fluorescein angiographic study of 175 patients. Acta Ophthalmol. 1971;109:1–95. [PubMed] [Google Scholar]
- 9.Vd Berg W, Verbraak FD, Bos PJ. Homocyteinuria presenting as central retinal artery occlusion and longstanding thromboembolic disease. Br J Ophthalmol. 1990;74:696–7. doi: 10.1136/bjo.74.11.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mukuno K, Matsui K, Haraguchi H. Ocular manifestations of homocysteinuria, report of two cases. Nippon Ganka Gakkai Zasshi. 1967;71:66–73. [PubMed] [Google Scholar]
- 11.Den Heijer M, Rosendaal FR, Blom HJ, Gerrits WB, Bos GM. Hyperhomocysteinemia and venous thrombosis: A meta-analysis. Thromb Haemost. 1998;80:874–7. [PubMed] [Google Scholar]
- 12.Clarke R, Daly L, Robinson K, Naughten E, Cahalane S, Fowler B, et al. Hyperhomocysteinemia: An independent risk factor for vascular disease. N Engl J Med. 1991;324:1149. doi: 10.1056/NEJM199104253241701. [DOI] [PubMed] [Google Scholar]
- 13.Narayanasamy A, Subramaniam B, Karunakaran C, Ranganathan P, Sivaramakrishnan R, Sharma T, et al. Hyperhomocysteinemia and low methionine stress are risk factors for central retinal venous occlusion in an Indian population. Invest Ophthalmol Vis Sci. 2007;48:1441–6. doi: 10.1167/iovs.06-0905. [DOI] [PubMed] [Google Scholar]
- 14.Gronemeyer A, Arsène S, Le Lez ML, Rateau J. Central retinal artery occlusion or branch retinal artery occlusion in the young associated with high lipoprotein (a) levels. J Fr Ophtalmol. 2002;25:727–30. [PubMed] [Google Scholar]
- 15.Murata M, Saito T, Takahashi S, Ichinose A. Plasma lipoprotein (a) levels are high in patients with central retinal artery occlusion. Thromb Res. 1998;91:169–75. doi: 10.1016/s0049-3848(98)00082-6. [DOI] [PubMed] [Google Scholar]
- 16.Griffin JH, Evatt B, Zimmerman TS, Kleiss AJ, Wideman C. Deficiency of protein C in congenital thrombotic disease. J Clin Invest. 1981;68:1370–3. doi: 10.1172/JCI110385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Comp PC, Esmon CT. Recurrent venous thromboembolism in patients with a partial deficiency of protein S. N Engl J Med. 1984;311:1525–8. doi: 10.1056/NEJM198412133112401. [DOI] [PubMed] [Google Scholar]
- 18.Walsh PN, Kansu T, Savino PJ, Schatz NJ, Magargal LE, Goldberg RE, et al. Platelet coagulant activities in arterial occlusive disease of the eye. Stroke. 1979;10:589–94. doi: 10.1161/01.str.10.5.589. [DOI] [PubMed] [Google Scholar]
- 19.DeWitt LD, Caplan LR. Antiphospholipid antibodies and stroke. AJNR Am J Neuroradiol. 1991;12:454–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Suvajac G, Stojanovich L, Milenkovich S. Ocular manifestations in antiphospholipid syndrome. Autoimmun Rev. 2007;6:409–14. doi: 10.1016/j.autrev.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Villatte-Cathelineau B. The eye and hormones: Vascular disorders associated with combined oral contraceptives and pregnancy. Contracept Fertil Sex. 1985;13:147–52. [PubMed] [Google Scholar]
- 22.Friedman S, Golan A, Shoenfeld A, Goldman J. Acute opthalmologic complications during the use of oral contraceptives. Contraception. 1974;10:685–92. doi: 10.1016/0010-7824(74)90107-3. [DOI] [PubMed] [Google Scholar]
- 23.Chen YJ, Chen WL, Tsai WC, Tsao YT. Sentinel central retinal artery occlusion: A forme fruste of idiopathic renal infarction. Am J Emerg Med. 2009;27:253. doi: 10.1016/j.ajem.2008.06.027. [DOI] [PubMed] [Google Scholar]
- 24.Wilson LA, Keeling PW, Malcolm AD, Russell RW, Webb-Peploe MM. Visual complications of mitral leaflet prolapse. Br Med J. 1977;2:86–8. doi: 10.1136/bmj.2.6079.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Willetts GS. Recurrent rheumatic chorea and optic atrophy after occlusion of central retinal artery. Br Med J. 1961;2:688. doi: 10.1136/bmj.2.5253.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tillett A, Edelsten C. Branch retinal artery occlusion: A case complicating acute rheumatic fever and dental abscess. Hosp Med. 2000;61:360–1. doi: 10.12968/hosp.2000.61.5.1339. [DOI] [PubMed] [Google Scholar]
- 27.Au A, O’Day J. Review of severe vaso-occlusive retinopathy in systemic lupus erythematosus and the antiphospholipid syndrome: Associations, visual outcomes, complications and treatment. Clin Exp Ophthalmol. 2004;32:87–100. doi: 10.1046/j.1442-9071.2004.00766.x. [DOI] [PubMed] [Google Scholar]
- 28.Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: Associated systemic and ophthalmic abnormalities. Ophthalmology. 2009;116:1928–36. doi: 10.1016/j.ophtha.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liem RI, Calamaras DM, Chhabra MS, Files B, Minniti CP, Thompson AA. Sudden-onset blindness in sickle cell disease due to retinal artery occlusion. Pediatr Blood Cancer. 2008;50:624–7. doi: 10.1002/pbc.21152. [DOI] [PubMed] [Google Scholar]
- 30.Reynolds SA, Besada E, Winter-Corella C. Retinopathy in patients with sickle cell trait. Optometry. 2007;78:582–7. doi: 10.1016/j.optm.2007.04.100. [DOI] [PubMed] [Google Scholar]
- 31.Nagy V, Takacs L, Steiber Z, Pfliegler G, Berta A. Thrombophilic screening in retinal artery occlusion patients. Clin Ophthalmol. 2008;2:557–61. doi: 10.2147/opth.s1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rudkin AK, Lee AW, Chen CS. Vascular risk factors for central retinal artery occlusion. Eye (Lond) 2010;24:678–81. doi: 10.1038/eye.2009.142. [DOI] [PubMed] [Google Scholar]
- 33.Schmidt D, Hetzel A, Geibel-Zehender A, Schulte-Mönting J. Systemic diseases in non-inflammatory branch and central retinal artery occlusion: An overview of 416 patients. Eur J Med Res. 2007;12:595–603. [PubMed] [Google Scholar]


