Abstract
Background:
HIV/AIDS is a problem in developing countries including Jamaica. There are several studies dealing with HIV/AIDS in Jamaica but given the increasing rate of the infection, ongoing studies are necessary.
Aims:
This study examines the sexual behavior and attitude of non-HIV testers in Jamaica in order to provide research evidence that will direct public health policies and interventions.
Materials and Methods:
This study extracts a sample of 1,192 participants who indicated not having done a HIV test from 1,800 respondents from a 2004 HIV/AIDS/STD National KABP Survey. A detailed questionnaire was developed and used to collect data from people ages 15-49 years old.
Results:
Some 20.3 % of the variances, which is self reported positive HIV test results, are a function of relationship status, using protection against HIV, having sex with a commercial sex worker, having STIs, the age at which the participant first had sex and age at last birthday. These findings hold across gender, occupational status and education. The majority (87.9%) of the participants said they had little or no chance of getting HIV, and 59.7% did not want to know their HIV status. However, 46.6% did not wear a condom the first time they had sex with current partner, 32% do not wear a condom with their current partner and 16.3% reported having had STIs.
Conclusion:
The existing HIV prevention programs need to be expanded and fortified to target young Jamaicans, particularly those who do not engage in safe sexual practices.
Keywords: Sexual behavior, HIV, non-HIV testing, attitude of non-HIV testers, reproductive health matters, consistent condom use, sexual relations with commercial sex worker, multiple sexual partnerships
Introduction
There are several studies dealing with sexual behavior, people's attitude towards HIV/AIDs and HIV testing[1–4]. In Zimbabwe, one study found that the prevalence of HIV among monogamous women was 21.8%[1]. Several factors increase the risk of HIV infection. These factors are the husbands having children with other women, more than five years age difference within couples, the woman's age, and the likelihood of the woman discussing monogamy with her husband in the next three months[1] as well as economic disparities between the sexes. In Zambia there is a sizable group of HIV positive neurology patients who suffer from myelopathy, neuropathy/radiculopathy, cerebrovascular diseases and infectious diseases[2]. A multi-country study including Thailand, South Africa, Tanzania and Zimbabwe, which used a sample of 14,818 in 48 communities, found that frequent discussions about HIV significantly influenced prior HIV testing[3]. A study in Vietnam, dealing with HIV risk behavior and the determinants among people living with HIV/AIDS, found that 82% of the participants were sexually active[4]. Some 20% of the participants reported having sex with multiple partners, and only one third of the participants consistently used a condom.
Jamaica manifests some of these problems relating to HIV/AIDS, HIV testing, and determinants of risky behaviors seen in other developing countries. Sexual risk taking behavior among working class women were influenced by being in a relationship with a physically violent intimate partner, attitudes towards children as resources, having multiple sexual partners, being economically vulnerable, the perception about men being providers[5] and the vetoing power of males on women's reproductive health matters. Choices and the lack of economic dependency are accounting for increasing HIV/AIDS/STDs in developing countries.
The risk of contracting HIV also affects the incarcerated where the rate of HIV infection among prisoners is higher than the incidence in the general population[6]. HIV/AIDS is viewed by some Jamaicans as a homosexual disease. The negative stigma of homosexuality and AIDS influences low levels of HIV testing[7]. There is nuanced sympathy for people living with HIV/AIDS. A majority of university students stated that they had no avoidance intentions towards their relatives and friends living with HIV/AIDS[8]. However, less than one-half of the students were sympathetic to gay and lesbians living with HIV/AIDS who were not their relatives or friends[9].
It is important to understand the cultural factors at the societal, family and individual levels that influence HIV risk among Jamaican youth[10]. In 2004, from a survey of Jamaican youth, males reported greater condom use (67.9%) during their last sexual intercourse with their most recent and regular partner compared to 57% in 1996[11]. There was no change in the use of condoms among adolescent females for the same period. The youth perceived that they were at a greater risk for HIV infection in 2004 compared 1996[11]. Despite the aforementioned fact, there are still many youths who are inconsistently using a condom, indicating the divide between knowledge and practice. Public health effort to improve the case management of sexually transmitted diseases now includes the private sector. Private medical practitioners are now receiving continuing medical education[12] to address the HIV/AIDS epidemic and youths’ reproductive health matters.
Despite the increased risk of contracting HIV owing to inconsistent and improper condom usage[8–11], many Jamaicans do not want to know their HIV status. A person knowing his or her HIV status allows the person to get the appropriate medical treatment if they are positive and prevent the spread of the virus through safe sexual practices. Douglas opined that the major cause of mortality among women of 15-44 years in the Caribbean is AIDS, and that 1 in every 50 Caribbean national was infected with HIV/AIDS[13], suggesting that there are some premature mortality arising owing to not being cognizant of one's HIV status.
Sexual relation is primarily the medium through which most people contract HIV/AIDS[14]. In 2007/2008, Wilks et al. conducted a study of some 2,848 Jamaicans between the ages of 15-74 years; they found that 3.4% of females reported having been infected with a STI in the studied period compared to 1.3% of males[15]. Although the prevalence of males having had STI is greater than that of females, which is concurred by Wilks et al study (males, 18.1%; females, 11.0%)[15], with the context that more males (having multiple partners in last 12 months, 41%) are promiscuous than females (8.4%)[15], there is a pending public health problem that is underlying the females allowing males to have vetoing power over their reproductive health issues and having male partners inconsistently using condoms. This reality requires immediate public health intervention. An extensive research of the literature found no study which has examined the attitude of non-HIV testers towards future HIV testing as well as their current attitude and sexual behavior. Within this context, the objectives of this paper are to (1) investigate the sexual behavior of non-HIV testers in Jamaicans, and (2) their attitudes towards future HIV testing.
Patients and Methods
Sample
The current study extracted a sample of 1,192 participants, from a nationally representative survey, who indicated that they had never had an HIV test done up to 2004. The HIV/AIDS/STD National KABP Survey comprised 1,800 participants 15-49 years of age who resided in Jamaica at the time of the survey (May-August, 2004)[16]. The data was collected by Hope Enterprises Limited on the behalf of the Ministry of Health[16]. A multi-staged sampling design was used to collect the data. Each of the 14 parishes in the country is stratified into electoral constituencies, with each constituency stratified into three areas - rural areas, parish capitals (urban areas) and main towns (semi-urban areas). The areas which comprised a constituency were then stratified into primary sampling units (PSUs) or electoral enumeration districts (EDs).
A random sample of each PSU was then selected based on probability proportional to size (PPS). Seventy-two EDs were selected for the study – 23 EDs in the urban areas, 25 EDs in the semi-urban areas, and 24 EDs in the rural areas. Twenty-five households were systematically chosen from each ED, and cluster sampling was carried out with all the people living in the household of the designated ages interviewed for the survey.
Data sources
A questionnaire was used to collect the data from the participants. Trained interviewers used face-to-face interviews to collect the data. The interviewers were trained for a 5-day period, of which 2 days were devoted to field practices. Interviewers were assigned to a team comprising two females, two males and a supervisor. Verbal consent was sought and given before the interviews commenced. The participants were informed of their right to confidentiality and their right to stop the interview at any time. No names, addresses or other personal information was collected from the participants to ensure anonymity. The instrument used in the survey utilized indicator measures and definitions consistent with UNAIDS and the USAID Priority Prevention Indicator.
Statistical analyses
Data were entered, stored and retrieved using SPSS for Windows, Version 16.0 SPSS Inc; Chicago, IL, USA). Descriptive statistics were generated for the socio-demographic variables. Multivariate logistic regressions were fitted using one outcome measure: self-reported confirmed positive HIV test results. We looked at correlation matrices in order to examine multicollinearity. Where collinearity existed (r > 0.7), variables were entered independently into the model to determine those that should be retained during the final model construction. A p-value < 0.05 (two-tailed) was used to establish statistical significance.
Results
Table 1 presents the demographic characteristics of sample. Of the sample (n=1192 participants), 54.4% was males, 42.9% were employed, and the majority had secondary level education.
Table 1.
Sociodemographic characteristics of sample, n= 1192
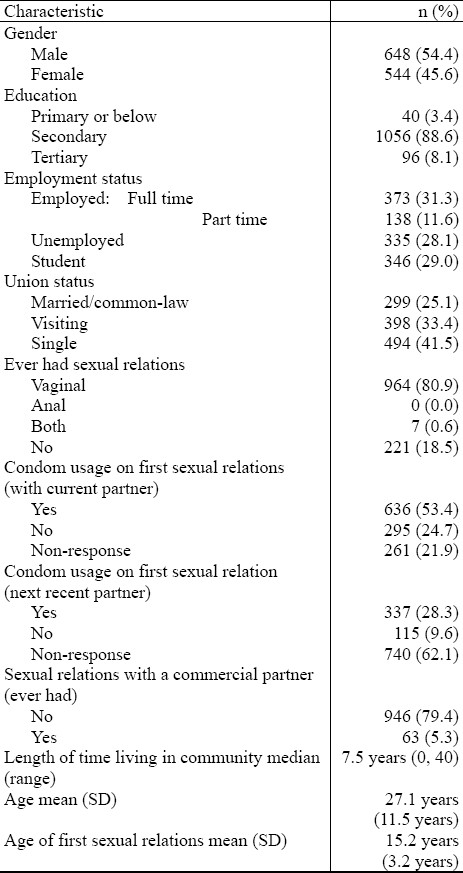
Of those who had never done a HIV test ( n=1192), 78.0% indicated that they would be willing to do this in the future; 16.3% have STI; 55.2% are currently and actively practicing a religion; 14.9% are laborers; 38.8% are household helpers and office attendants; 31.1% are security guards, hairdressers, taxi operators, machine operators and cosmetologist, 3.6% teachers, police officers, nurses and technicians; 6.8% clerks, 2.2% manager, assistant managers and heads of small businesses, 0.2% business executives, and 0.4% professionals (doctors, lawyers, architects, etc.).
When the participants were asked “What is the chance of [you] catching HIV?” 57.7% indicated none, 30.2% said little, 6.3% reported moderate and 5.8% remarked a good chance. However, 20.5% had sex with at least two partners in the last 4 weeks. Seventy-two percent had sexual relations with one partner. Only 53.4% used a condom the first time with their current partners, and 36.1% indicated that their current partner has other partner(s). Fewer than 70% of the sample indicated that their next most recent partner had other sexual partner(s).
A statistical difference was found between the mean number of sexual partners males had in the last 12 months (2.6, SD = 4.0) and females (existed between the mean age of sexual debut for males (14.2 years, SD = 3.2 years) and that of females (16.5 years, SD = 2.8 years) – t-test = -11.443, P < 0.0001.
Table 2 shows information on the reasons the participants gave for not using a condom by current, next recent and next most recent partner. The findings reveal that between 10% and 15% of the participants do not like using condoms with current, next recent or next most recent sexual partner(s), and between 3 to 5% of the participants stated that their partner objected to using a condom.
Table 2.
Reason for not using a condom by current, next recent and next most recent partner
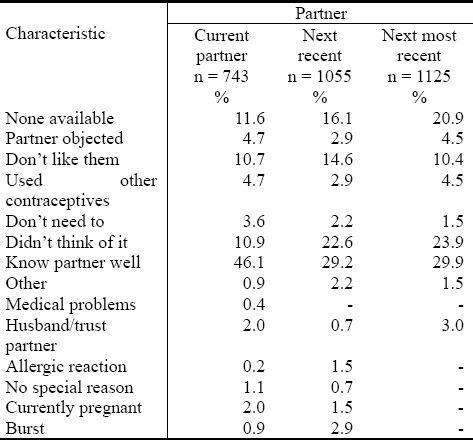
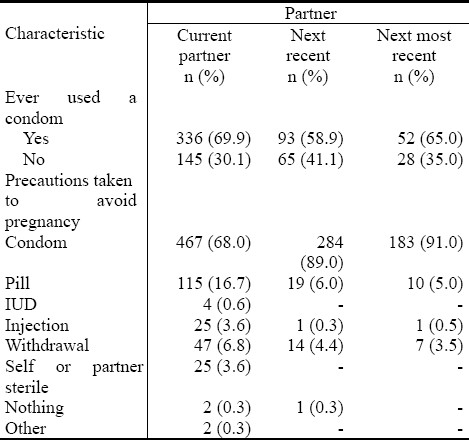
Table 3 provides condom usage (ever) and precautions taken to avoid pregnancy by current, next recent and next most recent partner. The percentage of participants who are using a condom with their current partner(s) is less (68%) compared to the next recent partner (89%) and the next most recent partner (91%).
Table 3.
Condom usage (ever) and precautions taken to avoid pregnancy by current, next recent and next most recent partner
Different reasons were given for the moderate-to-good chance of contracting the HIV virus. The reasons were; have different partners, 13.6%; spouse has many partners, 4.1%; do not use a condom, 7.6%; had blood transfusion, 1.3%; never too careful, 14.5%; and condom can burst, 8.0%.
When the participants were asked why they had not done a HIV test, 59.7% indicated that they do not want to know their status, 15.4% said they are not sexually active, 10.0% reported that they know that they do not have HIV, 5.0% reported that they are not interested, 0.5% remarked that they always practice safe sexual relations.
Eight percent of the participants stated that they were forced to have sexual relations, 7.0% indicated that they had forced someone to have sexual intercourse and 1.7% remarked that physical force was used in the process. Significantly more males (12.5%) had forced someone compared to 2.5% of females (χ2 = 32.946, P < 0.0001). However, 35.9% of females indicated that physical force was used in the process of forced sexual relations compared to 6.7% of males (χ2 = 17.485, P < 0.0001). Furthermore, no statistical association existed between ′were you forced to have sexual intercourse?′ based on the gender of the participants – males, 9.3% and females, 10.1% (χ2 = 0.190, P = 0.669). In addition, significantly more people with STI were forced to have sexual relations (15.5%) compared to those who were not forced (7.0%) – χ2 = 12.894, P < 0.0001.
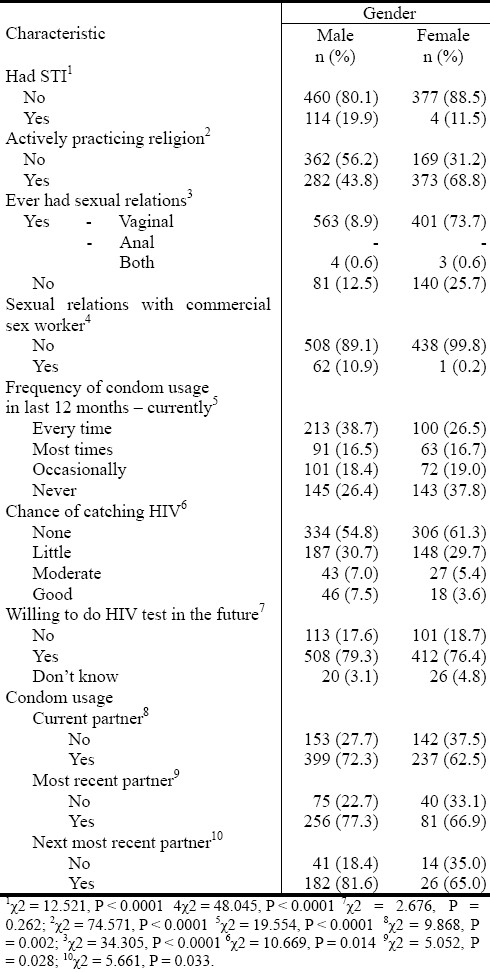
Table 4 examines particular demographic characteristics of the participants based on gender.
Table 4.
Some demographic characteristic by gender of participants
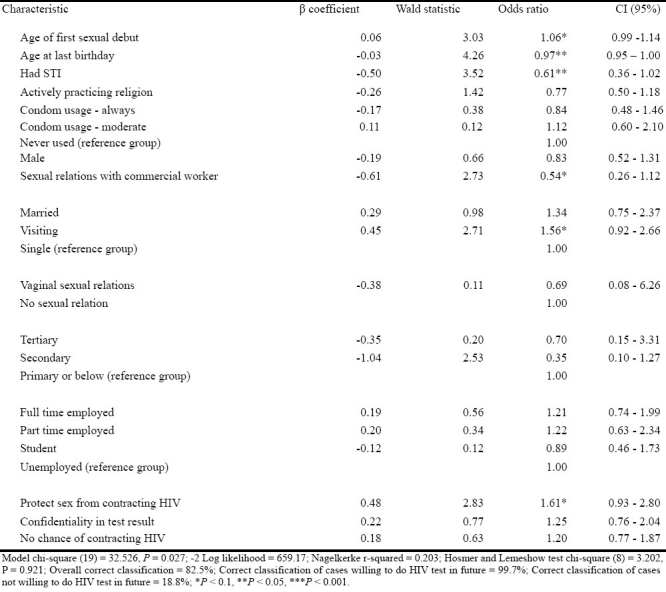
The results of the multivariate logistic regression model, shown in Table 5, were significant (Model χ2 = 32.526, P = 0.027). Table 5 indicates that 20.3% of the variances accounted for by the independent variables used in the regression analyses: age of first sexual debut, age at last birthday, having had STI, sex with commercial worker, union status, and protecting self from the possibility of contracting the HIV virus. The model had statistically significant predictive power (Model χ2 = 32.526, P = 0.027; Hosmer and Lemeshow goodness of fit (χ2 = 3.202, P = 0.921), and correctly classified 82.5% of the sample (Table 5).
Table 5.
Logistic regression analyses: Variables of willing to do HIV test in the future, n = 950
No statistical existed between ‘would you be willing to do a HIV test in the future?’ and whether the individual was forced to have sexual intercourse – χ2 = 0.444, P = 0.801: yes to be willing, 9.3%; no to be willing, 11.0%; and don’t know, 9.4%.
Discussion
Sexual relation is mainly the medium through which most people contract HIV/AIDS[17]. This study provides invaluable insights into those who have done a HIV test and their sexual behavior and attitude towards future HIV testing. From the findings, clearly, people are linking a low risk of contracting the HIV virus with having one sexual partner. Based on the perception of respondents in this sample, they are omitting the close association between inconsistent condom usage, not knowing the HIV status of current and past partners, and having unprotected sexual intercourse in a heterosexual way with high risk of contracting the HIV virus.
Other issues which emerged from the current work are (1) the low probability of those who have had sex with commercial sex workers willingness to consider doing a HIV test in the future, (2) the inverse association between having had a STI and the likeliness of wanting to do a HIV test in the future, and (3) negative association between age of respondents and wanting to do a HIV test in the future. Within the context that 16.3% of the sample; having had STIs, 58% indicated a low risk of contracting the HIV virus, 6.2% having had sexual relations with a commercial sex worker, 50.3% consistently using a condom, and 60% not wanting to know their HIV status, and notion that HIV/AIDS being a homosexual disease[7], there is a need to execute immediate public health interventions to address these findings.
More programs promoting safe sexual practices are definitely needed because between 10 % and 15 % of the participants did not use a condom during sexual intercourse with their current, next recent and next most recent partner(s). What is worse is that; 3-5% of the participants stated that their partner objected to them using a condom. Moreover, 32% of the participants do not wear a condom with their current partner compared to the 11% who do not wear a condom with their next recent partner. Not wearing a condom increases the risk of contracting and spreading HIV[17]. Some 16.3% of the participants have STIs. Despite these risks, only 49.1% of the participants gave several reasons (participant or spouse having multiple partners, condom failure, negligence, blood transfusion, not wearing a condom) for a moderate to good chance of contracting HIV. More than one- half of the participants gave no reasons for a good to moderate chance of contracting HIV. It is not surprising then, that 59.7% of the participants did not want to know their HIV status, which creates a problem in the reduction of HIV infection since more than 10% reported that they did not use a condom and 36.1% reported that their current partner has other partners. Another explanation which accounts for high risk of contracting STIs and HIV/AIDS, despite the current respondents’ perception of their seemingly low risk, is women's acquiescence to the vetoing power of men in reproductive health decisions. A research conducted by WHO showed that some women opined that reproductive health decisions are made by their partner because “he looks after me”[18], suggesting a rationale for inconsistent condom use.
A related problem is sexual intercourse through coercion. Significantly more men compared to women declared that they had coerced someone to have sex. Similarly, a greater proportion of women (35.9%) stated that physical force was used in coerced sexual intercourse compared to men (6.7%). Participants who experienced coerced sexual relations are less likely to use a condom because of the powerful influence of the situational context in which they find themselves. This possibility increases the risk of these participants contracting HIV. The data supports this assumption because a significant majority of the participants who were forced to have sex had STIs compared to those who were not forced. Within the context that “HIV is more easily passed from infected males to females than in the reverse and it is predicted that proportionately more cases will occur in females than in males in Jamaica in the future”[19], and females being coerced to have sexual intercourse. If this abusive practice is occurring without the use of condoms, it will be accounting for greater risk of HIV infection in the future.
An important issue which must be addressed in public health intervention is financial inadequacies of females which account for them relishing their reproductive health choices, often carte blanche to males. Jamaica is a middle-income developing country with the prevalence of poverty rate being 9.9% in 2007 (urban poverty rate, 6.2%; semi-urban poverty rate, 4.0%; rural poverty rate, 15.3%; prevalence of poverty among males, 7.2%; prevalence of poverty among females, 8.0%)[20]. Economic deprivation of females more than males can also be explained by the unemployment rates, and earnings. The unemployment rate for females was almost 2.3 times more than that of males (6.2)[21], indicating that if this economic inequity continues, females will relinquish their reproductive health choices to males as they are providing the economic livelihood. In 2004, the Economic and Social Survey of Jamaica[21], publication showed that on an average the earnings of males (mean wage = $2.4 million) was 2 times more than that of females ($ 1.7 million); and that 76 per cent of senior positions were held by males although 54 per cent of executive and managerial positions were held by females[21]. Poverty and unemployment, therefore, are explanations of why people become engaged in risky activities as well as take short-term health risks; in order to earning a living as they seek a change for the better. It is this belief in socio-economic development that spurs women to relinquish their reproductive health choices to men as they perceive men, as having the economic resources to make an improvement in their current status, even if it is temporary.
WHO stated that, on a yearly basis, there are approximately 340 million new cases of STIs and 5 million new cases of HIV infection[22]. Clearly, inconsistent condom usage can account for an increase in STI/HIV, indicating that the attitude of non-HIV testers in this sample is reinforcing the pending public health problems that need to be addressed with some degree of urgency. A study by Henry-Lee found that reasons given by Jamaican women for inconsistent contraceptive use or even discontinuation were (1) cost of contraception, and (2) long waiting queues at clinics (3)[23]. She contended that scheduling of appointments could reduce the long waiting time at the clinics[23]. While Henry-Lee is correct about using appointments to reduce waiting at clinics, but the vetoing supremacy of males in the reproductive health decisions of females could account for their non-return to the clinics. Due to the economic disparity, poverty, low education, low income, and inconsistent condom usage, many people do not want to know their HIV status yet they believe that they are at a low risk of contracting the virus. Furthermore, significantly more females than males who have never had a HIV test indicated that they are not at risk of contracting the HIV virus, yet statistically more males than females consistently use a condom.
Clearly, there is a denial among Jamaicans of their probability of contracting the HIV virus as people still perceive that the virus is a homosexual disease. A study by Dunkle et al.[24] showed that more people that have had heterosexual intercourse had contracted the HIV virus in Zambia and Rwanda[24] than those who are engaged homosexual relationships. Dunkle et al.'s work[24] provide some understanding of the rationale behind Jamaicans reluctance to have a HIV test done even though they may be in heterosexual relations, as the predominant cultural belief is that it is a homosexual disease. One researcher noted that “Among Jamaican males, there is a substantial peer group pressure to engage in sex in order to avert the stigma of homosexuality, and sexual initiation may occur as early as the age of 8 years”[25] indicating the dominance of the culture in causing or reverting to particular and even potentially deleterious actions. The irony here is that Caribbean men are socialized to be promiscuous and indulge in premarital sexual relations[25–28], which is evident in the male-to-female HIV prevalence ratio (1.3:1)[29–32], but if they are infected with HIV as a direct consequence of their sexual behavior, they will be scoffed at for having being homosexual.
The public health dilemma of HIV infection is that we have been estimating a probability of prevalence among Jamaicans[29–31]. The Jamaican Ministry of Health estimated that 65% of those persons who are infected with HIV are unaware of their status, and this reiterates the rationale for public health intervention programs. Due to the sobering reality that people do not want to know their HIV status owing to the stigmatization associated with the virus. Currently the nation is not seeing the economic impact of HIV/AIDS, which may justify why non-HIV testers were not researched on their sexual behavior and attitude towards HIV testing. Research findings are in on non-HIV testers, and these should be integrated with public health intervention so as to effectively address some of the present challenges of non-HIV testing in the Jamaica and in the wider developing nations.
World Bank revealed that over 95% of persons living with HIV/AIDS were in low and middle income countries[32]. Of this figure over 20 million of these persons have died from AIDS in 2002. This HIV/AIDS epidemic has reduced life expectancy by more than ten years in many countries[32]. Gebre postulated that the Caribbean countries have the highest incidence rates of HIV/AIDS in the Americas and the second highest prevalence rates in the world among adults aged 15 – 44 years[33]. Statistics have showed that between 270,000 to 780,000 adults are living with HIV in the region, which is about 2.3%. Almost 9453 cases of AIDS were reported in Jamaica and of this amount 1100 of these cases were identified in 2004. This is an estimated 1.6% of the adult population that has been infected with HIV[33]. According to WHO, 60% of global mortality is caused by chronic illness[34], suggesting that HIV/AIDS will substantially influence the economic and social development of developing countries in the future and that we can no longer allow risky health practices to continue unabated.
In 2006, the reasons persons have given for non-HIV testing were (1) they do not want to hear their status (11%), (2) 1.3% perceived seronegative status, (3) 1.0% stated that they were not sexually active and (4) had no partner, 0.7% said that they were not interested in doing an HIV test[35]. Based on the findings of the current study the prevalence of Jamaicans not wanting to know their HIV status has increased exponentially, which speaks to the rise of inconsistent condom usage, increase in STIs, increase in premarital sexual relations and promiscuity. Those are the rationales which should vehemently dictate the urgency of HIV/AIDS registry in seeking to thoroughly understand this threat and how to effectively tailor intervention that the spread of STIs and HIV/AIDS can be reduced.
Conclusion
The time has come for the government to require HIV and AIDS to be reportable by name, and a national HIV/AIDS registry be kept in order to monitor the epidemic in Jamaica. While the researchers recognize the stigmatization surrounding the disease, the issue of privacy, discrimination, and understand that this may result in the continuation of the low willingness of people to become tested for HIV; the findings are far reaching and cannot be allowed to continue into the indefinite future.
Acknowledgement
The authors would like to extend their appreciation to the Jamaican Ministry of Health that commissioned the data collection, Hope Enterprise Limited that collected the data and the Sir Author Lewis Institute which made it available to us for use.
The authors report no conflict of interest with this work.
The researchers would like to note that while this study used secondary data from the Jamaican Ministry of Health (MoHJ), none of the errors in this paper should be ascribed to the MoHJ, but to the researchers.
References
- 1.Hageman KM, Dube HMB, Mugurunqi O, Gavin LE, Hader SL, St. Louis ME. Beyond monogamy: Opportunities to further reduce risks for HIV infection among married women with only one lifetime partner. AIDS and Behavior. 2010;14:113–124. doi: 10.1007/s10461-009-9603-5. [DOI] [PubMed] [Google Scholar]
- 2.Siddiqi OK, Atadzhanov M, Birbeck GL, Koralnik IJ. The spectrum of neurological disorders in Zambian tertiary care hospital. J of the Neurological Sci. 2010;290:1–5. doi: 10.1016/j.jns.2009.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hendriksen ES, Hlubinka D, Chariyalert S, et al. Keep talking about it: HIV/AIDS-related communication and prior HIV testing in Tanzania, Zimbabwe, South Africa, and Thailand. AIDS and Behavior. 2009;13:1213–1221. doi: 10.1007/s10461-009-9608-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thanh DC, Hien NT, Tuan NA, Thang BD, Long NT, Fylkesnes K. HIV risk behaviors and determinants among people living with HIV/AIDS in Vietnam. AIDS and Behavior. 2009;13:1151–1159. doi: 10.1007/s10461-008-9451-8. [DOI] [PubMed] [Google Scholar]
- 5.Le Franc E, Wyatt GE, Chambers C, Eldemire D. Working women's sexual risk taking in Jamaica. Social Science & Medicine. 1996;42:1411–1417. doi: 10.1016/0277-9536(95)00289-8. [DOI] [PubMed] [Google Scholar]
- 6.Andrinopoulos KM. Examining HIV/AIDS within the context of incarceration in Jamaica. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2008;69:2260. [Google Scholar]
- 7.White RC, Carr R. Homosexuality and HIV/AIDS stigma in Jamaica. Culture, Health & Sexuality. 2005;79:347–359. doi: 10.1080/13691050500100799. [DOI] [PubMed] [Google Scholar]
- 8.Norman LR, Carr R, Uche C. The role of sympathy on avoidance intention toward person's iving with HIV/AIDS in Jamaica. AIDS Care. 2006;18:1032–1039. doi: 10.1080/09540120600578409. [DOI] [PubMed] [Google Scholar]
- 9.Norman L, Carr R, Jimenez J. Sexual stigma and sympathy: Attitudes toward persons living with HIV in Jamaica. Culture, Health & Sexuality. 2006;8:423–433. doi: 10.1080/13691050600855748. [DOI] [PubMed] [Google Scholar]
- 10.Hutchinson MK, Jemmott LS, Wood EB, et al. Culture specific factors contributing to HIV risk among Jamaican adolescents. JANAC: J of the Association of Nurses in AIDS Care. 2007;18:35–47. doi: 10.1016/j.jana.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Norman L, Figueroa JP, Wedderburn M, Byfield L, Bourne D, Gebre Y. Trends in HIV risk perception, condom use and sexual history among Jamaican youth, 1996-2004. Int J Adolescent Med Health. 2007;19:199–207. doi: 10.1515/ijamh.2007.19.2.199. [DOI] [PubMed] [Google Scholar]
- 12.Green M, Hoffman IF, Brathwaite A, et al. Improving sexually transmitted disease management in the private sector: The Jamaica experience. AIDS. 1998;12:S67–S72. [PubMed] [Google Scholar]
- 13.Douglas DL. Perspectives on HIV/AIDS in the Caribbean. In: Morgan O, editor. Health issues in the Caribbean. Kingston: Ian Randle; 2005. pp. xv–xxi. [Google Scholar]
- 14.Barnett T, Whiteside A. AIDS in the twenty-first century: Disease and globalization. London: Palgrave MacMillan; 2002. p. 11. [Google Scholar]
- 15.Wilks R, Younger N, Tulloch-Reid M, McFarlane S, Francis D. Jamaica health and lifestyle survey 2007-8. Kingston: Tropical Medicine Research Institute, University of the West Indies, Mona; 2008. [Google Scholar]
- 16.HIV/AIDS Knowledge, Attitudes and Behaviour Survey, 2008. Kingston: Jamaica, Ministry of Health, National HIV/STI Programme; 2008. Hope Enterprise Limited. [Google Scholar]
- 17.Steiner MJ, Cates W. Are condoms the answer to rising rates of non-HIV sexually transmitted infections.? Yes. BMJ. 2008;36:184. doi: 10.1136/bmj.39402.488727.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reproductive health research at WHO: a new beginning. Biennial Report 1998-1999. Geneva: WHO; 2000. World Health Organization (WHO) p. 31. [Google Scholar]
- 19.Bain B. HIV/AIDS – the rude awakening/stemming the tide. In: Morgan O, editor. Health issues in the Caribbean. Kingston: Ian Randle Publisher; 2005. pp. 62–71. [Google Scholar]
- 20.Jamaica Survey of Living Conditions, 2007. Kingston: PIOJ, STATIN; 2008. Planning Institute of Jamaica (PIOJ), Statistical Institute of Jamaica (STATIN) [Google Scholar]
- 21.Economic and social survey, 1990-2007. Kingston: PIOJ; 1991-2008. Planning Institute of Jamaica (PIOJ) [Google Scholar]
- 22.Sexual and reproductive health – laying the foundation for a more just world through research and action: Biennial report 2004-2005. Geneva: WHO; 2006. Planning Institute of Jamaica (PIOJ) [Google Scholar]
- 23.Henry-Lee A. Women's reasons for discontinuing contraceptive use within 12 months: Jamaica. Reproductive Health Matters. 2001;9:213–220. doi: 10.1016/s0968-8080(01)90030-8. [DOI] [PubMed] [Google Scholar]
- 24.Dunkle K, Stephenson R, Karita E, et al. New heterosexually transmitted HIV infections in married or cohabiting couples in Urban Zambia and Rwanda: An analysis of survey and clinical data. The Lancet. 2008;371:2183–91. doi: 10.1016/S0140-6736(08)60953-8. [DOI] [PubMed] [Google Scholar]
- 25.Drayton VLC. Contraceptive use among Jamaican teenage mothers. Pan Am J Public Health. 2002;11:150–157. doi: 10.1590/s1020-49892002000300003. [DOI] [PubMed] [Google Scholar]
- 26.Jagdeo T. The dynamics of adolescents fertility in the Caribbean. St. John's, Antigua: Caribbean Family Planning Affiliation; 1992. [Google Scholar]
- 27.Chevannes B. Sexual behavior of Jamaicans: a literature review. Soc Econ Stud. 1993;42:1–45. [Google Scholar]
- 28.Chevannes B. Learning to be a man: Culture, socialization and gender identity in five Caribbean communities. Kingston, Jamaica: The University of the West Indies Press; 2001. [Google Scholar]
- 29.Health in the Americas 2007, volume II – countries. Washington D.C: PAHO; 2007. Pan American Health Organization (PAHO) [Google Scholar]
- 30.The Jamaica road map to scaling up universal access to HIV prevention, care, and treatment support services. Kingston: MoH; 2006. Jamaica, Ministry of Health (MoH) [Google Scholar]
- 31.Annual report, 1997-2008. Kingston: MoH; 1998-2009. Jamaica, Ministry of Health (MoH) [Google Scholar]
- 32.World Bank. Public health at a glance: HIV/AIDS update. [Accessed April 17, 2010]. at http://web.worldbank.org/WBSITE/EXTERNAL/TOPICS/EXTHEALTHNUTRITIONANDPOPULATION .
- 33.Gebre Y. National HIV/STD prevention and control facts and figures, Jamaica. AIDS Report, 2004. Kingston, Jamaica: epidemiology Unit, Ministry of Health; 2005. [Google Scholar]
- 34.Preventing chronic diseases a vital investment. Geneva: WHO; 2005. World Health Organization. [Google Scholar]
- 35.Norman LR. HIV testing practices in Jamaica. HIV Medicine. 2006;7:231–242. doi: 10.1111/j.1468-1293.2006.00368.x. [DOI] [PubMed] [Google Scholar]


