Abstract
Background:
Studies have shown that women's ability to access contraceptive methods depend on their socio-economic, educational, professional status, and the health and well-being of their families and themselves. Therefore, the embarking of the Governments of the Caribbean on important initiatives relating to gynecological matters is very important and timely.
Aims:
This study aims to examine the perception, attitude and practice of Jamaican women towards the matter of pelvic examination.
Patients and Methods:
The current study used an extracted sample of 7,168 women in their reproductive years (15-49 yrs) from a study which was undertaken by the National Family Planning Board in 2002 on Reproductive Health. Data was analyzed using SPSS for Windows, Version 16.0 (SPSS Inc.; Chicago, Ill. USA). Logistic regression was used to analyze factors/variables pertaining to Pelvic examination.
Results:
The findings revealed that older women are more likely to have done a Pelvic examination compared to younger women (χ2 = 675.29, P < 0.001). Age, number of pregnancies that resulted in miscarriages, number of pregnancies that resulted in induced abortion, age of first sexual intercourse, number of years of schooling, area of residence and socio-economic class are statistically significant factors of Pelvic examinations in Jamaica. Therefore, the model had significant predictive power where (χ2 = 1022.79, P < 0.001).
Conclusion:
The multidimensional nature of the variables, which emerged in the current study, indicate that a multisectoral approach should be used to address low pelvic and Pap smear examination among Jamaican women.
Keywords: Miscarriages, pregnancy, contraception, pelvic examination, papanicolaou smear (Pap smear), Jamaica
Introduction
Research has shown that owing to women's unique reproductive capacities, their ability to access contraceptives impacts on their socio-economic, educational, professional status, health status and overall well-being[1]. The use of some contraceptive methods (for example, the intrauterine device, IUD) could result in gynecological concern (pelvic inflammatory disease). As a result, women's attitude towards such contraceptive result in myths and misconceptions such as the IUD (a) inhibits pregnancy; (b) increases the risk of ectopic pregnancy; and (c) is an abortificient[2]. However, it is imperative to note that there is slight risk of Pelvic Inflammatory Disease (PID) that is associated with women who use IUD[3]. Sexually active women in their reproductive years are mostly at risk, more so than those under 25 years old. This is because the cervix of teenagers and young women are not as fully mature as those who are older. Pelvic Inflammatory Disease usually occurs when bacteria moves from a woman's vagina or cervix into her reproductive organs. It is mostly associated with gonorrhea and Chlamydia[3]. It is not easily detected, and so a lack of early treatment could result in damage to the reproductive organs (for example, scar tissue to the fallopian tubes)[3].
Using a probability sample of 2,848 Jamaicans aged 15-74 years, Wilks and colleagues found that 93.3% of females aged 15-74 years old have had sexual relations, 8.4% reporting having 2+ sexual partners, 41% had sexual intercourse once per week, 82.9% had been pregnant. compared with 76.4% of females aged 15-24 years who indicated having had sexual intercourse and 40.6% reported having sex once per week. Despite the sexual practices of women in Jamaica, only 18% of those aged 15-74 years old had done a Papanicolaou smear (Pap smear) examination in the last 12 months, 18.0% between 1-2 years ago and 29.2% more than 3+ years ago, with 71.3% of females aged 15-24 years had never done a Pap smear examination[4]. Furthermore, Wilks et al. also found that 41.2% of women aged 15-74 years had used a condom during their last sexual intercourse[4]. Of which, 37.4% were aged 15-24 years, 33.2% aged 25-34 years, 25.2% aged 35-44 years, 18..7% aged 45-54 years, and 6.4% aged 55-64 years old. Thus inconsistent condom use which is among highly sexed females could result in PID and other disease causing pathogens.
Another reality noted by the World Health Organization (WHO) is that cancers are diagnosed more frequently in the developing world than the developed nations; and that cervical cancer is the second most prevalent of cancers among women[5]. In 2002, statistics on Jamaica revealed that malignant neoplasms (or cancers) were the leading cause of mortality[6], and that in 2007; cervical cancer was among the 5th leading cause of morality among Jamaican women[7]. In spite of South and Southeast Asia recording the largest number of new HIV infections, and Sub-Saharan Africa represents the highest rate of new infections, followed by Latin America and the Caribbean[8,9] as well as “more than 340 million new cases of the common bacterial and protozoal STIs (syphilis, gonorrhoea, Chlamydia, genital infections, trichomoniasis) occur every year throughout the world in men and women ages 15-49”[8], Jamaican females exhibit a low willingness to have a Pap smear or pelvic examination done even though they are highly sexed individuals, most have been pregnant at least once, and few of them consistently use a condom[4].
According to Berer, “Human beings are sexual by nature. If nothing else, one thing seems certain-people will never stop having sex or wanting to have sex”[10]. Despite the negative realities associated with risky sexual behavior, people will continue their involvement and engagement in sexual practices, and sometimes these will be risky. One of the ironies which emerged from the examination of data on reproductive health is a high knowledge of method of contraception, access to contraception and sexually transmitted infections, in particular HIV. However, there is low consistent usage of contraception, and in particular condom[4,11]. Thus, Pap smear and pelvic examination should be a part of the routine health care of women because they detect cancers, sexually transmitted infections and abnormalities that can result in cancer of the cervix, yet some women delay this exercise owing to fear of the unknown.
Previous studies which have examined reproductive health in the Jamaica have provided information on contraceptive use and knowledge, fertility, Pap smear examination, sexual activity[4,11], factors associated with cervical cancer screening[12–19], and Pap smear of older women[20], but little is known about the perception, attitude and practice of Jamaican women towards the matter of pelvic examination; and the factors which influence their attitude towards the practices (or not). Fletcher provides insight into the practice and perception of women in Jamaica[21]. He found that 9 out of every 10 women who died from cervical cancer was never screened, and continued that “Most women have heard of the Pap smear but believe its purpose is to detect rather than prevent cervical cancer”[21]. Jamaican females are not atypical as another study conducted on older women in Latin American and Caribbean Cities found that Pap smear examination was also low (from 21% in Bridgetown to 45% in Mexico City)[20].
Within the context of a sexually active female, particularly those who used condoms inconsistently during sexual activities, ignoring gynecological consultation could result in late detection of abnormal cells relating to viral and bacterial infections that severely affect the female reproductive organ, cases in point are infections associated with HPV/cervical cancer and PID. With regard to the former, the literature postulated that throughout the World, there were approximately 470,606 cases of cervical cancer and 233,372 deaths arising from malignant neoplasm of the cervix uteri (in 2000)[22]. In the Caribbean, however, there was an incidence rate of 35.78 and mortality rate of 16.84 (per 100,000) in the said year.[22] In Jamaica, cases of cervical cancer in the 2000s represent 43.4 per 100,000 populations[23]. This paper examines, therefore, the perception, attitude and practice of Jamaican women towards the matter of Pelvic examination. Assessments are made based on factors such as age, area of residence (urban versus rural) and socio-economic class.
Patients and Methods
This study used the 2002 Reproductive Health Survey (RHS) data on women ages 15-49 years. The sample was 7,168 women and represents a response rate of 91.8%. Stratified random sampling was used to design the sampling frame from which the sample was drawn. Using the 2001 Census sector (or sampling frame), a three stage sampling design was used. Stage 1 was the use of selection frame of 659 enumeration areas (or enumeration districts, EDs). This was calculated based on probability proportion to size. The health sector of Jamaica is classified into four health regions: South East Region - Kingston, St. Andrew, St. Thomas and St. Catherine; North East Region - Portland, St. Mary and St. Ann; Western Region - Trelawny, St. James, Hanover and Westmoreland; and Southern Region - St. Elizabeth, Manchester and Clarendon. The 2001 Census showed that region 1 comprised 46.5% of Jamaica compared to Region 2, 14.1%; Region 3, 17.6% and Region 4, 21.8%[11].
Stage 2 saw the clustering of households into primary sampling units (PSU). This constitutes an ED comprising 80 households. The previous sampling frame was updated between January and May 2002. The new sampling frame forms the basis upon which the sampling size was computed for the interviewers to use. Stage 3 was the final selection of one eligible female and male and this was done by the interviewer on visiting the household.
The Statistical Institute of Jamaica (STATIN) provided the interviewers and supervisors, McFarlane Consultants, who were trained to carry out the survey. The instrument was a 35-item questionnaire of 35 pages. This was administered during the period October 26, 2002 to May 9, 2003[11].
The data was weighted in order to accurately represent the population of women ages 15- 49 year old.
Statistical Methods
The Statistical Packages for the Social Sciences (SPSS) for Windows, Version 16.0 (SPSS Inc; Chicago, IL, USA) was used to analyze the data. Frequencies and means were computed on the sociodemographic characteristics, health conditions, pregnancy, papanicolaou (Pap) smear, pelvic examination and reasons for contraceptive choices. The researchers also performed χ2 tests to compare associations in particular sociodemographic variables, contraception, pregnancy, and Pelvic examination. Stepwise multiple logistic regressions were used to analyze factors that explain gynecological examination, in the last 12-months and Pap smear test done in the last 12-months. Where collinearity existed (r > 0.7), variables were entered independently into the model to determine those that should be retained during the final model construction[24]. To derive accurate tests of statistical significance, we used SUDDAN statistical software (Research Triangle Institute, Research Triangle Park, NC), and this was adjusted for the survey's complex sampling design.
Measures
Crowding is the total number of persons who dwell in a room (excluding kitchen, bathroom and verandah). Age is the number of years a person is alive up to his/her last birth day (in years). Contraceptive method comes from the question “Are you and your partner currently using a method of contraception …”, and if your answer is yes “Which method of contraceptive do you use?” Age at which participants began using contraception was taken from “How old were you when you first used contraception? Area of residence is measured from “In which area do you reside?” The options were rural, semi-urban and urban. Currently having sex is measured from “Have you had sexual intercourse in the last 30 days?” Education is measured from the question “How many years did you attend school?” Marital status is measured from the following question “Are you legally married now?”, “Are you living with a common-law partner (now; that is, are you living as man and wife now with a partner to whom you are not legally married?”, “Do you have a visiting partner, that is, a more or less steady partner with whom you have sexual relations?” and “Are you currently single?” Age at first sexual intercourse is measured from “At what age did you have your first intercourse?” Pelvic examination is taken from “Have you ever had a pelvic examination?” Pelvic examination is measured from the question “Have you ever had a gynecologic examination? Pap smear is measured using the question “A Pap Smear is a test for cancer of the cervix which is done during a pelvic examination by a doctor or nurse.” And, “How long has it been since your last Pap Smear, if ever? Pregnancy was assessed by “Are you pregnant now?” Religiosity was evaluated from the question “With what frequency do you attend religious services? The options range from at least once per week to only on special occasions (such as weddings, funerals, christening, et cetera). Subjective social class is measured from “In which class do you belong?” The options are lower, middle or upper social hierarchy.
Results
Table 1 presents information on the sociodemographic, pregnancy and health conditions of sample. The sample was 7,168 women (ages 15 – 49 years). Most women indicated that they had used at least one contraceptive method in the past (88.1%) and 63.8% claimed that they are currently using a contraceptive method. Fifty-five percentage of the sample dwelled in rural areas, 29.0% in semi-urban and 16.0% in urban zones. One-half of the sample indicated that their first sexual intercourse occurred at 17 years (Range = 29: 7, 36), with 25% starting at 15 years and 75% stated less than or equal to 19 years.
Table 1.
Sociodemographic characteristic of sample, n = 7,168
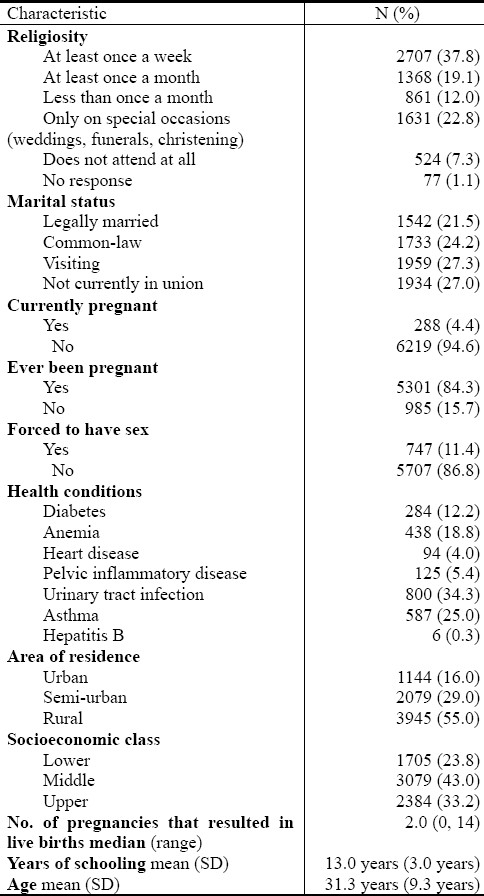
One half of the sample indicated that their first menarche began at 13 years old (range: 8 – 21 years old) while one quarter of the sample reported having that their first menarche at 12 years and three-quarter indicated that they began at 14 years old.
Table 2 examines information on Pelvic examinations and the reasons why some women have not done the test. Of the 7, 168 women surveyed, more than a half of them (56.9%) have not done a Pelvic examination, and 57.1% have not responded to the question on the last time one was done. Only 18.0% of the women have done an examination within the last 12 months. The data also showed that 37.3% have never done a papanicolaou test whilst 35.4% have done tests within the last 2 years. Most women have not had a non-menstrual discharge (83.0%) in the last 12 months. For the question pertaining to reasons for not having done a Pelvic examination, 35.9% of the sample cited “never thought of it”; 15.9% claimed “healthy and has no sign of gynecological problems; 11.8% claimed that it was “not recommended by doctor and 10.6% indicated that they “did not need to go”.
Table 2.
Gynecological examination of studied population
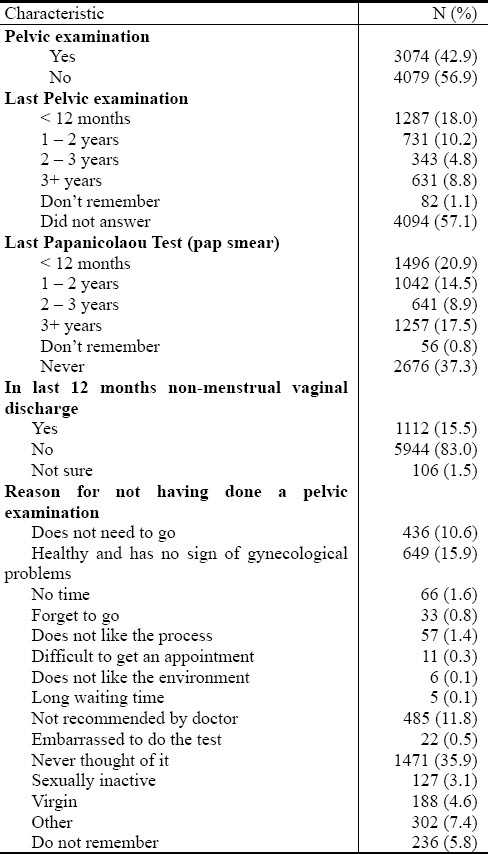
Table 3 shows information on Pelvic examinations by particular sociodemographic variables and contraception usage. There is a significant statistical difference among the mean age of women for those who have (or have not) done a Pelvic examination. Cross-tabulation provides a more detailed break-down of the percentage of women in particular age cohort who have done the examination15-19 years, 11.5%; 20-24 years, 29.9%; 25-29 years, 41.8%; 30-34 years, 51.1%; 35-39 years, 53.7%; 40-44 years, 55.6%; and 45-49 years, 57.4% (χ2 = 675.287, P-value< 0.0001). The findings highlight that older women are more likely to have done a Pelvic examination compared to younger women.
Table 3.
Pelvic examination by sociodemographic characteristics
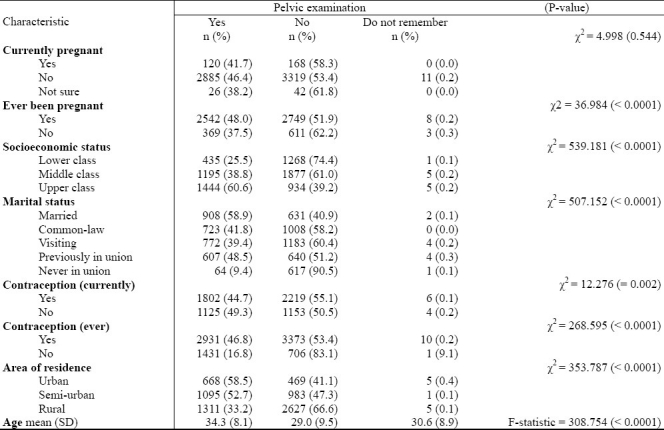
Figure 1 presents information on particular demographic characteristic of study population that had never done a pelvic examination or Pap smear. Based on the Figure, rural women in the reproductive ages were less likely to have done Pap smear or pelvic examinations as well as those ages 15-19 years, in a sexual union, and of the middle socio-economic stratum of society.
Fig. 1.
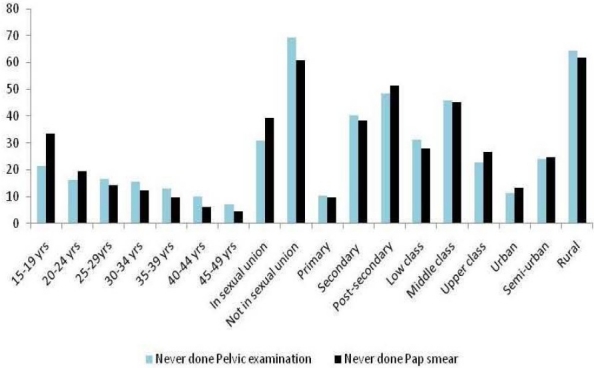
Particular demographic characteristic of study population who never did pelvic exams or Pap smear
Using logistic regression analyses, eight variables emerged as statistically significant factors of Pelvic examination in Jamaica (Table 4). The factors are age, number of pregnancy that resulted in live births, number of pregnancy that resulted in miscarriages, number of pregnancy that resulted in induced abortion, age at first sexual intercourse, number of years of schooling, area of residence and socioeconomic class. Furthermore, the model had statistically significant predictive power (model χ2 (DF = 8) = 1022.79, P< 0.0001; Hosmer and Lemeshow goodness of fit χ2 = 4.52, P = 0.912), and correctly classify 68.3% of the sample.
Table 4.
Logistic regression: Explanatory variables of every done pelvic examination, n = 5,388
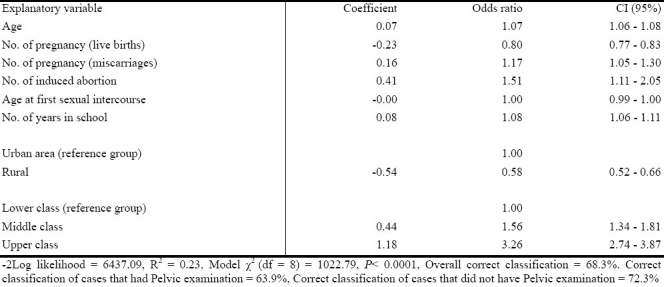
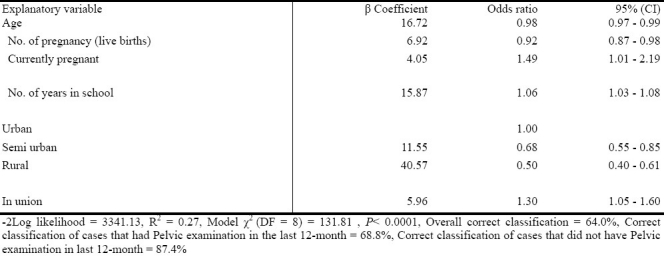
Table 5 examines factors that account for Pelvic examination of women in the last 12-months. From the logistic regression analyses, six factors explain why women (ages 15-49 years) have had a Pelvic examination in the past 12 months. The model had statistically significant predictive power model (χ2 (DF = 7) = 131.81, P< 0.0001; Hosmer and Lemeshow goodness of fit χ2 = 3.06, P = 0.912), and correctly classify 64.0% of the sample.
Table 5.
Logistic regression: Explanatory variables of those who had a pelvic examination in last 12 months, n = 5,388
Papanicolaou smear (Pap smear) examination (in the last 12 months) is explained by six factors. The six factors account for 25% of the variability in Pap smear examination (Table 6). The findings revealed that urban women are more likely to have had a Pap smear examination in the last 12 months compared to rural women (ages 15-49 years). The model had a statistically significant predictive power (model χ2 (DF = 7) = 182.2, P< 0.0001; Hosmer and Lemeshow goodness of fit χ2 = 6.31, P = 0.713), and correctly classify 76.6% of the sample.
Table 6.
Logistic regression: Explanatory variables of those who had a Pap smear in last 12 months, n = 5,388
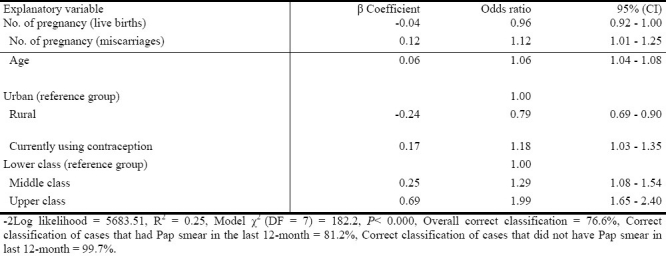
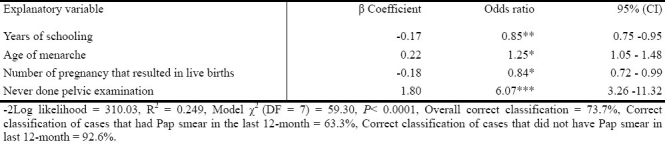
Table 7 presents information on factors which account for why the study population has never done a Pap smear examination. Using logistic regression analyses, four variables emerged as statistically significant factors of why women of the reproductive ages have never done a Pap smear examination (Table 7): education (years of schooling, OR = 0.85, 95% CI = 0.75 – 0.95), age of menarche (OR = 1.25, 95% CI = 1.05 – 1.48), number of pregnancies which resulted in live birth(s) (OR = 0.84, 95% CI = 0.72 – 0.99), and never done a pelvic examination (OR = 6.07, 95% CI = 3.26 – 11.32).
Table 7.
Logistic regression: Explanatory variables of those who had not done Pap smear, n = 5,388
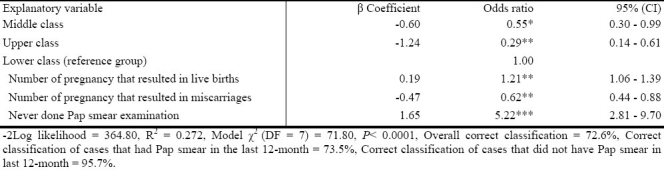
Using logistic regression analyses, four variables emerged as statistically significant predictors of why the study population had never done a pelvic examination (Table 8): social class, number of pregnancies which resulted in live birth(s), number of pregnancies that resulted in miscarriages, and never done a Pap smear examination. The model had statistical significant predictive power (model Model χ2 (DF = 7) = 71.80, P< 0.0001), and almost 73% of the sample was correctly classified (Table 8).
Table 8.
Logistic regression: Explanatory variables of those who had never done a pelvic examination n = 5,388
Discussion
The findings of this research have stated the various reasons why the subjects refrained from pelvic examination. This form of examination is used to detect early onset of abnormal cells in the cervix uteri, which could result in cervical cancer for example. Schools of thought have argued on the subject matter, and it is noted that (a) lower educational attainment was negatively associated with accessing cervical screening, particularly in Barbados and Trinidad and Tobago;[25] (b) unemployment did not facilitate pap smear because of cost; and (b) women from larger household size were less likely to have a Pap smear done[25].
In the current study the prevalence of Pap smear examination was greater than that in a research conducted in Latin American and the Caribbean Cities found that Pap smear examination from 21% in Bridgetown to 45% in Mexico City[20]. In this study, it was revealed that 21 out of every 100 females in the reproductive ages had done a Pap smear in the last 12 months, and that 18 out of every 100 had done a pelvic examination. The rationales forwarded by the study population for not having done a pelvic examination included never thought of it (36%); healthy (16%) and does not need to do one (11%). The findings in the current research showed some dissimilarity between factors which account for having done a Pap smear or pelvic examination and having never done either. A critical finding which emerged from this work is a female who is of the reproductive age who had never done a Pap smear will 6.1 times more likely not do a pelvic examination, and one who had never done a pelvic examination is 5.2 times more likely not do a Pap smear. Although females in the study were sexually active, most have been pregnant, the age at first sexual intercourse was in the adolescence years, and some had multiple partners, not doing a Pap smear or pelvic examination means that they will be ignorant of their pelvic inflammatory disease status.
In relation to PID, it is evidenced that “about 20% of affected women become infertile, 20% develop chronic pelvic pain, and 10% of those who conceive have an ectopic pregnancy”[26]. Where sexually transmitted infections such as Chlamydia and gonococcal infections are untreated, these could result in PID, ectopic pregnancy, infertility and neonatal infection[27]. From a sample of 767 family planning clients in Kingston Jamaica, who were screened for agents of gonorrhea, Chlamydia and trichomoniasis and syphilis, detections were found mainly in persons who mostly under the age of 25 years old had multiple partners in the past year. That study, (in making reference to the World Health Organization's risk inclusive algorithm), noted that for cervical infection, this was “least accurate (a positive predictive value of 14%). The weighted-risk algorithm was least accurate (a positive predictive value of 23%), while the interview-alone and the rapid risk assessment were slightly less accurate (positive predictive values of 20%)”[27].
The use of contraception, particularly condoms, has the capacity to not only reduce fertility rate (from 3 children per women in 1993 to 2.5 children per woman in 2002 in Jamaica) but also incidences of PID and HPV and other related STI bacteria/virus. Overall contraceptive prevalence in Jamaica is 85.3%, with condom (72.7%) being the most utilized among women aged 15-49[4]. According to Wilks and colleagues, 1 in every 2 female aged 15-24 years have been pregnant compared with 22 out of every 25 aged 25-34 years old, 48 out of every 50 aged, and 49 out of every 50 aged 45-54 years[4]. Those statistics revealed that there is a disparity between prevalence of condom use and consistent condom use. Simply put, inconsistent condom use is great among Jamaican women, suggesting that they are exposed to HIV/AIDS and other sexually transmitted infections (STIs).
It is anticipated that in meeting the Millennium Development Goal 5 (to combat HIV/AIDS) under the ambit of the National 2030 Plan[28], as well as meeting the 1994 program of action of the International Conference on Population and Development 6 (to reduce the spread of HIV infection and minimize its impact)[29], HIV prevalence will be 0.8% between ages 15-24 year olds in 2010, requiring approximately US$10.64 million in annual resources for Jamaica[30]. It is imperative to note that HIV prevalence rate between 15-49 year olds is 1.2 (in 2004)[31]. Earlier it was argued that cost was an impediment to accessing gynecological service, particularly Pap smear. Scholars have pointed out that “poverty makes it difficult to learn about HIV/AIDS or to purchase condoms or drugs”[32]. Other barriers are perception of risk, as well as power relations between men and women[33], for example, out of 3,151 cases, 1.4% women (15-49 year olds) expressed fear of side effects from contraceptive methods, while 0.7 claimed that their partner did not support the use of contraception[11].
Part of the goals of the ICPD is to reduce unmet need for family planning service, including contraceptives by 2015. This involves changes in attitudes that prevent women and girls from exercising their RH rights[34], as well as being knowledgeable about proper and ideal RH care such as gynecological consultations. This study realized, however (based on Table 2) that despite cost and education, attitude towards Pelvic examination influences RH care and treatment. One insightful scholar posited that “quality of care can only be achieved where quality has been defined by both the users and providers of services and where women are actively involved….”[35].
Previous studies which have examined factors that account for increased cancer screening utilization in Latin American and Caribbean countries have highlighted that these include health insurance, marital status, frequency of doctor visits, high education, high income, high functional and sexual partner approval[12–19]. However, while these provide some understanding of Pap smear or pelvic examination along with the additional factors which emerged from this study, we now know issues which account for females’ unwillingness to do such medical examination as a part of a comprehensive physical medical check-up. This research found that the number of pregnancies which resulted in live birth(s), having never done a Pap smear or pelvic examination, and age of menarche positive influence female unwillingness to include Pap smear or pelvic examination as a part of medical check-up. Within the context that most females in Jamaica (ages 15-74 years) have been pregnant and that 51% have been pregnant at least 3 times[2], coupled with their risky sexual behavior and inconsistent contraceptive usage[4,11] it follows that a low willingness to do cervical screening could not be stopped by merely understanding why females do Pap smear or pelvic examinations.
The high prevalence of cervical cancers in Jamaica can be explained by the findings of the current study, and any policy which is geared towards cervical cancers reduction must understand why women do not do Pap smears or pelvic examinations; in order to address this public health problem. As part of a policy objective the various Governments of the Caribbean (including Jamaica) have embarked upon very important initiatives relating to gynecological matters. Based on the current findings, a public intervention program is needed to directly address perception, attitude and practices of women in rural areas, middle class, with post-secondary level education and in a sexual union as they are least likely to do a pelvic or Pap smear examination. We also know that the issues which associate with those who had never done a Pap smear and pelvic examination must be included in the public health intervention program.
Conclusion
The rationales provided for the low decisions in pelvic examination were being healthy, not recommended by medical practitioner, and never thought of it among other reasons. The factors associated with ever ‘done pelvic examination and having done a pelvic examination’ in the last 12 months are somewhat different, and the multidimensional nature of the variables indicate that a multisectoral approach should be used in addressing low pelvic and Pap smear examination among Jamaican women. In addition, we are recommending that the age for Pap smear examination be lowered to 15 or 20 years old instead of the Jamaican Ministry of Health's figure of 25-54 years because of early sexual initiation of females (in their adolescence years), inconsistent condom usage, early median age at first menarche and the frequency of sexual activities among those 15-24 years old.
Acknowledgement
The researchers would like to note that while this study used secondary data from the Jamaica Survey of Living Conditions, none of the errors in this paper should be ascribed to the Planning Institute of Jamaica or the Statistical Institute of Jamaica, but to the researchers.
Footnotes
The authors have no conflict of interest to report.
References
- 1.Position Statement on contraception. Washington D.C: Association of Reproductive Health Professionals; 2009. Association of Reproductive Health Professionals. [Google Scholar]
- 2.Health matters: Dispelling common myths about intrauterine contraception. Washington D.C: Association of Reproductive Health Professionals; 2009. Reproductive Health Professionals. [Google Scholar]
- 3.Fact Sheet. Pelvic Inflammatory Disease. USA: Centre for Disease Control and American Social Health Association; 2007. Centre for Disease Control and American Social Health Association. [Google Scholar]
- 4.Wilks R, Younger N, Tulloch-Reid M, McFarlane S, Francis D. Jamaica health and lifestyle survey 2007-8. Kingston: Tropical Medicine Research Institute, University of the West Indies, Mona; 2008. [Google Scholar]
- 5.Comprehensive cervical cancer control: A guide to essential practice. Geneva: WHO; 2006. World Health Organization (WHO) [PubMed] [Google Scholar]
- 6.Health in the Americas 2007 Volume II – Countries. Scientific and Technical Publication No. 622. Washington DC: PAHO; 2007. Pan American Health Organization (PAHO) [Google Scholar]
- 7.Demographic statistics, 2007. Kingston: STATIN; 2008. Statistical Institute of Jamaica (STATIN) [Google Scholar]
- 8.A Measure of Survival. Calculating Women's Sexual and Reproductive Risk. Washington DC: Population Action International; 2007. Population Action International. [Google Scholar]
- 9.World health statistics. Geneva: WHO; 2009. World Health Organization (WHO) [Google Scholar]
- 10.Berer M. Sexuality, rights and social justice. Reproductive Health Matters. 2004;12(23):6–11. doi: 10.1016/s0968-8080(04)23130-5. [DOI] [PubMed] [Google Scholar]
- 11.Reproductive Health Survey Final Report 1997, 2002. Kingston: National Family Planning Board; 1999, 2005. National Family Planning Board. [Google Scholar]
- 12.Sepulveda C, Prado R. Effective cervical cytology screening programmes in middle-income countries: the Chilean experience. Cancer Detect Prev. 2005;29:405–411. doi: 10.1016/j.cdp.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 13.Mendoza-Sassi R, Beria JU. Prevalence of having a regular doctor, associated factors, and the effect on health services utilization: A Population-based Study in Southern Brazil. Cad Saude Publica. 2003;19:1257–1266. doi: 10.1590/s0102-311x2003000500004. [DOI] [PubMed] [Google Scholar]
- 14.Bingham A, Bishop A, Coffey P, et al. Factors affecting utilization of cervical cancer prevention services in low-resource settings. Salud Publica Mex. 2003;45:S408–416. doi: 10.1590/s0036-36342003000900015. [DOI] [PubMed] [Google Scholar]
- 15.Watkins MM, Gabali C, Winkleby M, Gaona E, Lebaron S. Barriers to cervical screening in rural Mexico. Int J Gynecol Cancer. 2002;12:475–479. doi: 10.1046/j.1525-1438.2002.01170.x. [DOI] [PubMed] [Google Scholar]
- 16.Aguilar-Perez JA, Leyva-Lopez AG, Angulo-Najera D, Salinas A, Lazcano-Ponce EC. Tamizaje en cáncer cervical: conocimiento de la utilidad y uso de citología cervical en México. Rev Saude Publica. 2003;37:100–106. doi: 10.1590/s0034-89102003000100015. [DOI] [PubMed] [Google Scholar]
- 17.Reyes-Ortiz CA, Freeman J, Peláez M, Markides KS, Goodwin JS. Mammography use among older women of seven Latin American and the Caribbean cities. Prev Med. 2006;42:375–380. doi: 10.1016/j.ypmed.2006.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reyes-Ortiz CA, Camacho ME, Amador LF, Velez LF, Ottenbacher K, Markides KS. Education, literacy and cancer screening among Latin American and Caribbean older adults. Cancer Control. 2007;14:388–395. doi: 10.1177/107327480701400409. [DOI] [PubMed] [Google Scholar]
- 19.Bessier P, Aung M, Jolly P. Factors affecting uptake of cervical cancer screening among clinic attendees in Trelawny, Jamaica. Cancer Control. 2007;14:396–404. doi: 10.1177/107327480701400410. [DOI] [PubMed] [Google Scholar]
- 20.Reyes-Ortiz CA, Velez LF, Camacho ME, et al. Health insurance and cervical cancer screen among older women in Latin American and Caribbean cities. Int J of Epidemiol. 2008;37:870–878. doi: 10.1093/ije/dyn096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fletcher H. Screening for cervical cancer in Jamaica. Caribb Health. 1999;2:9–11. [PubMed] [Google Scholar]
- 22.In: Pan American Health Organization. Cancer prevention. Cervical cancer in Latin America and the Caribbean: Fact Sheet 2001. PAHO Regional Office of the World Health Organization; 2001. International Agency for Research on Cancer, Globocan. [Google Scholar]
- 23.Rawlins J, Crawford T. Women's health in the English-Speaking Caribbean: The case of Trinidad and Tobago. Social and Economic Studies. 2006;55:1–31. [Google Scholar]
- 24.Polit DF. Data analysis and statistics for nursing research. Stamford: Appleton & Lange Publisher; 1996. [Google Scholar]
- 25.Rawlins J, Crawford T, editors. Caribbean Epidemiology Centre. Women's health in the English-Speaking Caribbean: The case of Trinidad and Tobago. Social and Economic Studies. 2006;55:1–31. [Google Scholar]
- 26.Ross J. Extracts from “Clinical Evidence” Pelvic inflammatory disease. BMJ. 2001;322:658–659. doi: 10.1136/bmj.322.7287.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ward E, Spruyt A, Fox L, et al. Strategies for detection of sexually transmitted infection among family planning clients in Jamaica. Guttmacher. 2001:27. [Google Scholar]
- 28.Vision 2030 Jamaica. National Development Plan. Kingston: PIOJ; 2009. Planning Institute of Jamaica (PIOJ) [Google Scholar]
- 29.International Conference on Population and Development. Countdown 2015. Sexual and Reproductive Health and Rights for All. Family Care International; International Planned Parenthood Federation; Population Action International. 2004 [Google Scholar]
- 30.Country profiles for population and reproductive health: Policy developments and indicators 2003. United Nations Population Fund, Population Reference Bureau; 2003. United Nations Population Fund, Population Reference Bureau. [Google Scholar]
- 31.World Population Data Sheet, 2005. Washington D.C: Population Reference Bureau; 2005. Population Reference Bureau. [Google Scholar]
- 32.Fact Sheet. How Reproductive Health Services and Key Supplies are Key to HIV/AIDS Prevention. Washington D.C: Population Action International; 2004. Population Action International. [Google Scholar]
- 33.United Nations Population Fund (n.d.) Condom Programming: Preventing HIV/AIDS. (Accessed on March 23, 2010 at http://www.unfpa.org/hiv/programming.htm. )
- 34.United Nations Population Fund. Donor Support for Contraceptives and Condoms for STI/HIV Prevention. United Nations Population Fund. 2008 [Google Scholar]
- 35.Commitments to Sexual and Reproductive Health and Rights for All: Framework for Action. New York: Family Care International; 1995. Family Care International. [Google Scholar]


