Abstract
Nonmelanoma skin cancer (NMSC) represents the most common form of cancer in Caucasians, with continuing increase in incidence worldwide. Basal cell carcinoma (BCC) accounts for 75% of cases of NMSC, and squamous cell carcinoma (SCC) accounts for the remaining majority of NMSC cases. Whilst metastasis from BCC is extremely rare, metastasis from high-risk SCC may be fatal. In this article, we review the aetiology, diagnosis and management of NMSC.
KEYWORDS: Basal cell carcinoma, nonmelanoma skin cancer, squamous cell carcinoma
INTRODUCTION
Nonmelanoma skin cancer (NMSC) is the commonest cancer in Caucasians.[1] Basal cell carcinoma (BCC) accounts for 75% of cases, and is a slow-growing, locally invasive epidermal tumour with a metastatic rate of <0.1%.[2,3] Cutaneous squamous cell carcinoma (SCC) accounts for the majority of the remainder of cases of NMSC and arises from dysplastic epidermal keratinocytes.[4] In contrast to BCC, SCC has a significant recognised rate of metastasis (0.3–3.7%), the majority of which occur from within a subgroup of high-risk SCC.[5]
Incidence of NMSC has significantly increased up to 10% per annum, and currently 2–3 million new cases of NMSC are diagnosed worldwide every year.[6,7] Most countries do not have cancer registries for NMSC and reported figures are likely to be underestimated. Incidence rates of NMSC increase closer to the equator, with the highest reported rates in the northern territories of Australia.[8]
Relevant English language articles were searched for utilising PubMed search engine.
AETIOLOGY
Development of NMSC is due to a combination of environmental, genetic and phenotypical factors. One of the most important of these risk factors is the environmental exposure to ultraviolet (UV) light, evidenced by the increase in incidence in sunnier climates, the lower rates in darker skin types and the majority of tumours arising over sun-exposed skin. BCC has been more associated with intermittent and childhood sun exposure, with SCC more related to chronic UV exposure.[9–11] UV light is thought to induce direct DNA mutation via covalent bonding between adjacent pyrimidines (UVB) and formation of reactive oxygen species (UVA).[12] Use of tanning devices is associated with 2.5-fold increase in SCC risk and 1.5-fold increase in BCC risk.[13] Phototherapy, utilised in the treatment of various skin diseases, is also associated with increased risk of NMSC. This association is stronger with psoralen photochemotherapy than with narrowband UVB.[11]
Genetic mutations are an important cofactor in the development of NMSC. Discovery of the mutation of Patched gene on chromosome 9q22 underlying basal cell naevus syndrome, a genodermatosis associated with multiple BCC, has greatly forwarded the understanding of the genetics underpinning BCC. Patched1, the protein product of PTCH, is a cell surface receptor, inhibiting smoothened (SMO), a G-protein-coupled receptor. Cessation of SMO inhibition by patched 1 initiates a signal cascade that leads to the activation of transcription factor Gli1. Dysregulation of this pathway by either the loss of PTCH or uncontrolled expression of SMO results in cell proliferation and differentiation. Mutations of either PTCH or SMO have been found in 70% of sporadic human BCCs.[14–16] Other reported genes associated with the pathogenesis of BCC are Cytochrome 450 (CYP), glutathione S-transferase (GST) and p53. CYP and GST are known to detoxify mutagens, whilst p53 has an important function as a tumour suppressor gene regulating the cell cycle.[17–19]
Whilst sporadic BCC develops de novo, SCC arises from precursor lesions of actinic keratosis (AK) and Bowen's disease, and represents a multistep accumulation of genetic damage. Over 72% of SCC have been noted to develop within AK or actinically damaged skin, also known as background field cancerisation.[20,21] Significant histological and genetic mimicry exists between AK and SCC and errors of p53 signalling have been implicated in both. Mutations in p53 have been identified in 69% to over 90% of invasive SCC. Other reported mutations for SCC include WNT, Ras, p16INK4, NF-κB and c-Myc.[22,23]
Important phenotypic features associated with increased risk of NMSC include fair or red hair, blue eyes, increasing number of melanocytic naevi and Fitzpatrick skin type I.[22,24] Human papillomavirus has also been reported to be pathogenic for SCC and shown to prolong keratinocyte cell cycle, with increased degradation of p53.[25,26]
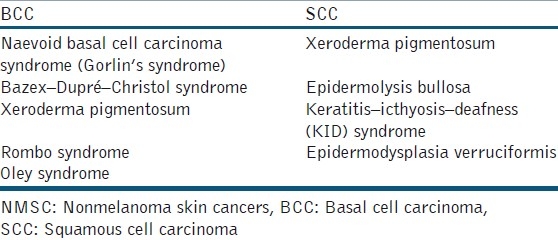
Particular attention must be held for organ transplant recipients (OTR) and immunosuppressed patients, who are strongly predisposed to NMSC. Incidence of SCC is increased 65–250 fold and that of BCC 10-fold in this group of patients.[27] The duration of immunosuppression is important, with incidence rates of 7% for NMSC after 1 year and 45% after 11 years. Following a primary SCC, the risk of developing a second NMSC within 5 years is 66%.[28] Furthermore, at presentation, the tumours are often more deeply invasive, with decreased histological differentiation and greater risk of metastasis.[29] Other risk factors for NMSC include genodermatoses [Table 1], age, skin post radiotherapy, arsenic exposure, haematological diseases (e.g. leukaemia, lymphoma) and chronic inflammation/ulcers.[5,30,31]
Table 1.
DIAGNOSIS
The diagnosis of NMSC in classical cases can be made clinically. With the exception of BCC of the superficial subtype, the majority of NMSC arises over sun-exposed skin.[32] SCC tends to present as rapidly growing pink or red nodules, which may be hyperkeratotic or ulcerated [Figure 1]. The clinical features of BCC depend upon the subtype. Nodular BCC is the commonest subtype accounting for over 60% of cases of BCC, and presents as pink nodules, with rolled edges, surface telangiectasia and ulceration or crusting [Figure 2]. Superficial BCCs account for up to 20% of cases and are found often on the trunk over sun-protected sites.[33] Appearing as pink scaly macules or thin plaques, they may be mistaken for Bowen's disease, psoriasis, discoid eczema or tinea corporis. Morphoeic BCC appears as subtle scar-like plaques, with ill-defined margins [Figure 3]. Pigmented BCC occurs more commonly in patients from the Far East and may be mistaken for nodular melanoma.
Figure 1.

Cutaneous squamous cell carcinoma
Figure 2.

Nodular basal cell carcinoma
Figure 3.

Morphoeic basal cell carcinoma on nasal tip
Dermoscopy has been used as an aid for diagnosis of BCC, with leaf-like areas, blue-grey blotches, wheel-spoke like areas, and arborising blood vessels seen on examination.[34] Skin biopsy, in addition to confirmation of diagnosis, allows stratification of tumours into high- and low-risk malignancies.
MANAGEMENT OF NMSC
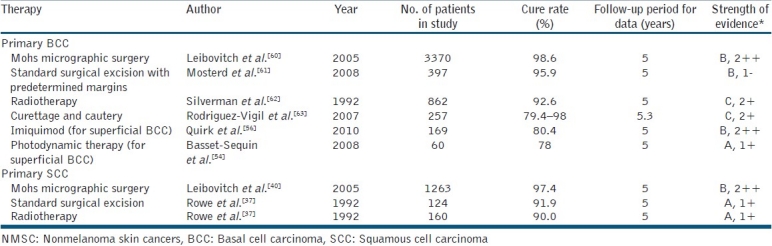
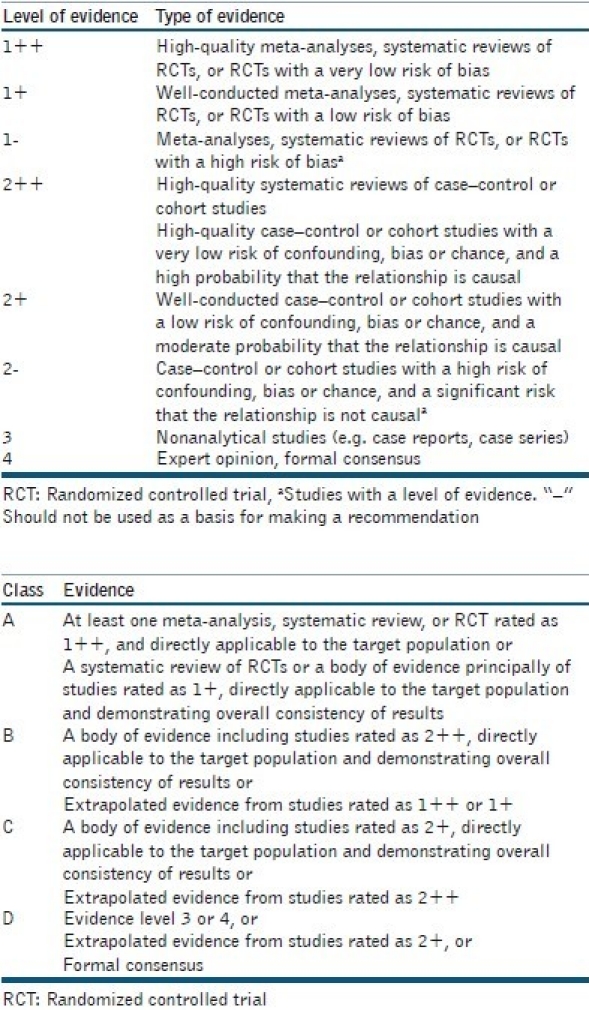
High-quality, well-designed, evidence-based studies with 5-year follow-up data are found infrequently for NMSC. Choice of treatment in NMSC is dependent on the risk stratification of the tumour, patient preference or suitability, and availability of local services. High-risk tumours have greater risk of recurrence and require more aggressive treatment. Table 2 lists the factors associated with high-risk NMSC. The gold standard treatment for high-risk BCC and SCC is Mohs micrographic surgery (MMS). If MMS is not available, excision with predetermined wide margins or radiotherapy may be considered. Topical treatment is usually reserved for the management of patients with low-risk BCC. Significant published evidence in the treatment of NMSC has been highlighted in Table 3.
Table 2.
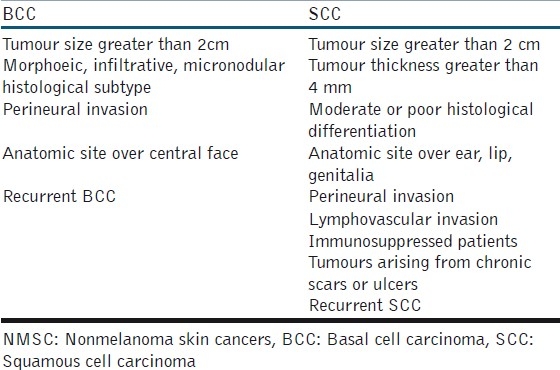
Table 3.
Published evidence on treatment of NMSC
Mohs micrographic surgery
MMS was first developed by Frederic Mohs in 1941.[35] In standard surgical excision (SE) with predetermined margins, less than 1% of the excision margin is examined. With the technique of MMS, 100% of the peripheral and deep margin is analysed by the operating surgeon to allow confirmation with certainty the presence or absence of any residual tumour. Once complete clearance is achieved, the wound is repaired by method of secondary intention healing, direct closure, local skin flap or skin graft [Figures 4 and 5]. Especially in high-risk NMSC or recurrent NMSC, MMS has been shown to have greater cure rate than any other treatment modality. Rowe and colleagues performed a meta-analysis of all published literature on the treatment of BCC and SCC. MMS was reported to provide a 5-year cure rate of 99% for previously untreated BCC and 97% for SCC.[36,37] Numerous subsequent studies have reported similar high cure rates for NMSC with MMS.[38–41] Of note, a randomised controlled study by Smeets et al. comparing MMS with SE for BCC found equally high cure rates with both modalities and no statistical difference in efficacy between the two treatments. However, for recurrent tumours, MMS was still found to be significantly more efficacious.[42]
Figure 4a.

BCC right temple
Figure 5a.

BCC right dorsal ear
Figure 4b.

Complete tumour clearance with Mohs surgery
Figure 4c.

Repair of Mohs defect with a rhombic transposition flap
Figure 4d.

Wound at 3 months post surgery
Figure 5b.

Wound post Mohs surgery repaired with skin graft
Figure 5c.

Wound 3 months post surgery and skin graft repair
Standard excision with predetermined margins
SE with predetermined margins of normal skin has been shown to provide 5-year cure rates over 98% for BCC and 92% for SCC.[31,37] For BCC less than 2 cm diameter, in an elegant prospective study of 117 patients, Wolf et al. marked skin around the tumour in concentric rings of increasing diameter prior to excision with MMS. Once the tumour had been entirely removed with MMS, they examined to see what SE with predetermined margin would have been required to completely excise the tumour. The study found that standard excision with 3 mm margin of normal skin around the BCC would have provided a histological clearance rate of 85%, and with 4-mm-wide margins, 98% of BCCs would have achieved histological cure.[43] Thus, United Kingdom guidelines suggest a 4–5 mm excision margin of BCC less than 2 cm diameter and of non-morphoeic subtype.[31]
For SCC, in a similar study, Brodland et al. reported 141 patients treated with MMS and found that tumours 2 cm diameter or less were completely excised with a 4-mm margin in greater than 95% of cases. Tumours over 2 cm diameter required a 6-mm excision margin to provide greater than 95% complete histological cure.[44] For high-risk SCC [Table 2], the National Comprehensive Cancer Network (NCCN) guidelines suggest in the absence of MMS or a pathology service able to provide examination of 100% of the excised margin, tumours should be excised with 1 cm margin of normal skin.[45]
Radiotherapy
Radiotherapy is an effective treatment modality for select patients with NMSC unable to undergo surgery, as efficacy is overall lower than with MMS or SE with predetermined margins. In a meta-analysis by Rowe et al., radiotherapy was found to have an overall 5-year cure rate of 91.3% for BCC, and in a similar study the 5-year cure rate was found to be 90% for SCC.[36,37]
Adjuvant radiotherapy may be beneficial postoperatively for tumours with perineural invasion or as palliative treatment when complete margin excision is not attainable due to extensive disease.[46]
Radiotherapy has been shown to increase the risk of subsequent BCC and SCC by threefold and should not be considered in younger patients, and is contraindicated in patients with genodermatoses susceptible for developing skin cancer.[47] Complications include long-term skin atrophy and necrosis.
Curettage and cautery
Curettage and cautery (C and C) involves removing epidermis and dermis containing tumour tissue with a sharp ring curette instrument prior to charring of the base of the wound with electrocautery. This process can be repeated immediately once or twice and provides an effective treatment of low-risk NMSC. Silverman et al. retrospectively reviewed 2314 primary BCCs treated with C and C and found tumours less than 5 mm provided a cure rate of 91% at 5 years.[48] However, with increasing diameter, cure rates significantly decreased. A prospective trial reported high cure rates for low-risk BCC with the combination of curettage and then cryosurgery to the wound in place of cautery. At 5-year follow-up of 94 superficial BCC (sBCC) treated, only one recurrence was noted.[49]
For SCC, Rowe et al. reported an overall 5-year cure rate of 96% in a retrospective study of the published literature.[50] However, with high-risk SCC, the cure rate is lower, and hence C and C for NMSC is recommended only for low-risk tumours.
Cryosurgery
Cryosurgery involves the delivery of liquid nitrogen to freeze and then thaw the target tumour tissue, inducing local cellular destruction. Significant variation in the duration of the freeze and the number of freeze-thaw cycles for cryosurgery exists in the literature in the treatment of NMSC. High cure rates have been reported for NMSC. Kuflik reported 99% 5-year cure rate for 415 BCC cases treated with cryosurgery and 100% 5-year cure rate for 132 treated SCC cases.[51]
High-risk NMSC is associated with lower cure rates, and cryosurgery is recommended for low-risk BCC. Cryosurgery is not recommended for SCC as these tumours have a potential for metastasis, and a more definitive therapy such as surgery, radiotherapy or C and C (for low-risk SCC) is advocated. Treatment with cryosurgery will also manifest a hypopigmented scar, which may have a cosmetically inferior outcome compared to the other treatment modalities.
Photodynamic therapy
Photodynamic therapy (PDT) is an effective therapy for sBCC or low-risk nodular BCC of less than 2 mm thickness. PDT involves the topical application of 5-aminolaevulinic acid (ALA) or methyl aminolaevulinic (MAL). Following uptake of the drug into the tumour cells preferentially, conversion into protoporphyrin IX (PpIX) occurs. The BCC is then illuminated with 410 nm blue or 630 nm red light with activation of PpIX and production of a cytotoxic reaction for tumour destruction.[52]
It is accepted that PDT provides excellent cosmetic results in comparison to other treatment modalities; however, little published evidence is present for long-term response. The majority of studies report upon 1–2 year follow-up data showing cure rates over 90% for sBCC.[53] Basset-Seguin et al. performed a multicentre randomised study comparing 114 sBCC treated with MAL-PDT against 105 sBCC treated with a double freeze-thaw cycle of cryosurgery. Five-year cure rates for PDT were found to be 78% and 80% for cryosurgery.[54] PDT is an excellent choice of treatment for sBCC, but is not recommended for high-risk BCC or any SCC.
Imiquimod
Imiquimod is a topical immunomodulator, activating cytotoxic T cell against tumour cells via binding to cell surface toll receptor 7 and/or 8.[55] Imiquimod is an effective treatment for sBCC, though most studies report on short-term follow-up data only. Quirk et al. performed a prospective, open-label multicentre study of 169 sBCC treated with 5% imiquimod cream daily for 6 weeks. Five-year follow-up data showed 84% cure rate.[56] The main side effects of the treatment are erythema, crusting, pain, flu-like symptoms and ulceration which can be severe. Topical imiquimod is not recommended for SCC as recurrence rates are too high.
Topical 5-fluorouracil
5-fluorouracil (5FU) is a pyrimidine antimetabolite that inhibits DNA synthesis. Topical treatment has been reported for sBCC. Romagaso et al. published a small study of 17 sBCC showing 90% histological cure rate at 16 weeks. However, strength of evidence is lacking and topical 5FU is not the recommended first-line treatment of sBCC.[57]
MANAGEMENT OF IMMUNOSUPPRESSED PATIENTS
OTR or patients on long-term immunosuppression who develop NMSC have higher risk of tumour recurrence and must be monitored closely, ideally in dedicated renal transplant dermatology clinics. Patients developing multiple SCC may benefit from the introduction of low-dose acitretin to reduce the number of new tumours. Immunosuppression should be maintained at the lowest effective doses. For OTR, transfer of immunosuppression from calcineurin inhibitors to mammalian target of rapamycin (mTOR) inhibitors such as sirolimus may be of benefit, with single agent immunosuppression used in preference to muti-drug combined immunosuppression.[48,58]
PROGNOSIS
Patient with BCC are at 10 times risk of developing a further BCC in comparison to the general population.[59] Despite this increased risk, no long-term follow-up is required for BCC once the primary tumour has been cured.
95% of recurrences for SCC occur within 5 years, with 70–80% of these recurrences occurring within the first 2 years. The NCCN recommends 3–6 monthly follow-up for 2 years and then 6–12 months for further 3 years. Sentinel lymph node biopsy has been reported to identify early microscopic lymph node metastasis, but is yet to show survival advantage, and further studies in this area required.[48,63]
APPENDIX 1
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Alam M, Nanda S, Mittal BB, Kim NA, Yoo S. The use of brachytherapy in the treatment of nonmelanoma skin cancer: A review. J Am Acad Dermatol. 2011;65:377–88. doi: 10.1016/j.jaad.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 2.Ting PT, Kasper R, Arlette JP. Metastatic basal cell carcinoma: Report of two cases and literature review. J Cutan Med Surg. 2005;9:10–5. doi: 10.1007/s10227-005-0027-1. [DOI] [PubMed] [Google Scholar]
- 3.Lo JS, Snow SN, Reizner GT, Mohs FE, Larson PO, Hruza GJ. Metastatic basal cell carcinoma: Report of twelve cases with a review of the literature. J Am Acad Dermatol. 1991;24:715–9. doi: 10.1016/0190-9622(91)70108-e. [DOI] [PubMed] [Google Scholar]
- 4.Macbeth AE, Grindlay DJ, Williams HC. What's new in skin cancer. An analysis of guidelines and systematic reviews published in 2008-2009? Clin Exp Dermatol. 2011;36:453–8. doi: 10.1111/j.1365-2230.2011.04087.x. [DOI] [PubMed] [Google Scholar]
- 5.Samarasinghe V, Madan V, Lear JT. Management of high-risk squamous cell carcinoma of the skin. Expert Rev Anticancer Ther. 2011;11:763–9. doi: 10.1586/era.11.36. [DOI] [PubMed] [Google Scholar]
- 6.Schulze HJ, Cribier B, Requena L, Reifenberger J, Ferrándiz C, Garcia Diez A, et al. Imiquimod 5% cream for the treatment of superficial basal cell carcinoma: Results from a randomized vehicle-controlled phase III study in Europe. Br J Dermatol. 2005;152:939–47. doi: 10.1111/j.1365-2133.2005.06486.x. [DOI] [PubMed] [Google Scholar]
- 7. [Last accessed on 2012 Jan 7]. Available from: http://www.who.int/uv/faq/skincancer/en/index1.html .
- 8.Tran H, Chen K, Shumack S. Epidemiology and aetiology of basal cell carcinoma. Br J Dermatol. 2003;149(Suppl 66):50–2. doi: 10.1046/j.0366-077x.2003.05622.x. [DOI] [PubMed] [Google Scholar]
- 9.Kricker A, Armstrong BK, English DR, Heenan PJ. Does intermittent sun exposure cause basal cell carcinoma. A case-control study in Western Australia? Int J Cancer. 1995;60:489–94. doi: 10.1002/ijc.2910600411. [DOI] [PubMed] [Google Scholar]
- 10.Rosso S, Zanetti R, Martinez C, Tormo MJ, Schraub S, Sancho-Garnier H, et al. The multicentre south European study ‘Helios’. II: Different sun exposure patterns in the aetiology of basal cell and squamous cell carcinomas of the skin. Br J Cancer. 1996;73:1447–54. doi: 10.1038/bjc.1996.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zak-Prelich M, Narbutt J, Sysa-Jedrzejowska A. Environmental risk factors predisposing to the development of basal cell carcinoma. Dermatol Surg. 2004;30:248–52. doi: 10.1111/j.1524-4725.2004.30089.x. [DOI] [PubMed] [Google Scholar]
- 12.Samarasinghe V, Madan V, Lear JT. Focus on basal cell carcinoma. J Skin Cancer. 2011;2011:328615. doi: 10.1155/2011/328615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smeets NW, Kuijpers DI, Nelemans P, Ostertag JU, Verhaegh ME, Krekels GA, et al. Mohs’ micrographic surgery for treatment of basal cell carcinoma of the face–results of a retrospective study and review of the literature. Br J Dermatol. 2004;151:141–7. doi: 10.1111/j.1365-2133.2004.06047.x. [DOI] [PubMed] [Google Scholar]
- 14.Xie J, Murone M, Luoh SM, Ryan A, Gu Q, Zhang C, et al. Activating smoothened mutations in sporadic basal-cell carcinoma. Nature. 1998;391:90–2. doi: 10.1038/34201. [DOI] [PubMed] [Google Scholar]
- 15.Johnson RL, Rothman AL, Xie J, Goodrich LV, Bare JW, Bonifas JM, et al. Human homolog of patched, a candidate gene for the basal cell nevus syndrome. Science. 1996;272:1668–71. doi: 10.1126/science.272.5268.1668. [DOI] [PubMed] [Google Scholar]
- 16.Gailani MR, Stahle-Backdahl M, Leffell DJ, Glynn M, Zaphiropoulos PG, Pressman C, et al. The role of the human homologue of Drosophila patched in sporadic basal cell carcinomas. Nat Genet. 1996;14:78–81. doi: 10.1038/ng0996-78. [DOI] [PubMed] [Google Scholar]
- 17.Lear JT, Heagerty AH, Smith A, Bowers B, Payne CR, Smith CA, et al. Multiple cutaneous basal cell carcinomas: Glutathione S-transferase (GSTM1, GSTT1) and cytochrome P450 (CYP2D6, CYP1A1) polymorphisms influence tumour numbers and accrual. Carcinogenesis. 1996;17:1891–6. doi: 10.1093/carcin/17.9.1891. [DOI] [PubMed] [Google Scholar]
- 18.Lear JT, Smith AG, Strange RC, Fryer AA. Detoxifying enzyme genotypes and susceptibility to cutaneous malignancy. Br J Dermatol. 2000;42:8–15. doi: 10.1046/j.1365-2133.2000.03339.x. [DOI] [PubMed] [Google Scholar]
- 19.Ramachandran S, Fryer AA, Smith AG, Lear JT, Bowers B, Hartland AJ, et al. Basal cell carcinomas: Association of allelic variants with a high- risk subgroup of patients with the multiple presentation phenotype. Pharmacogenetics. 2001;11:247–54. doi: 10.1097/00008571-200104000-00008. [DOI] [PubMed] [Google Scholar]
- 20.McGillis ST, Fein H. Topical treatment strategies for nonmelanoma skin cancer and precursor lesions. Semin Cutan Med Surg. 2004;23:174–83. doi: 10.1016/j.sder.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 21.de Lima Vazquez V, Sachetto T, Perpetuo NM, Carvalho AL. Prognostic factors for lymph node metastasis from advanced squamous cell carcinoma of the skin of the trunk and extremities. World J Surg Oncol. 2008;6:73. doi: 10.1186/1477-7819-6-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boukamp P. Nonmelanoma skin cancer: What drives tumor development and progression? Carcinogenesis. 2005;26:1657–67. doi: 10.1093/carcin/bgi123. [DOI] [PubMed] [Google Scholar]
- 23.Kathpalia VP, Mussak EN, Chow SS, Lam PH, Skelley N, Time M, et al. Genome-wide transcriptional profiling in human squamous cell carcinoma of the skin identifies unique tumor-associated signatures. J Dermatol. 2006;33:309–18. doi: 10.1111/j.1346-8138.2006.00075.x. [DOI] [PubMed] [Google Scholar]
- 24.Naldi L, DiLandro A, D’Avanzo B, Parazzini F. Host-related and environmental risk factors for cutaneous basal cell carcinoma: Evidence from an Italian case-control study. J Am Acad Dermatol. 2000;42:446–52. doi: 10.1016/s0190-9622(00)90217-2. [DOI] [PubMed] [Google Scholar]
- 25.Michel A, Kopp-Schneider A, Zentgraf H, Gruber AD, de Villiers EM. E6/E7 expression of human papillomavirus type 20 (HPV-20) and HPV-27 influences proliferation and differentiation of the skin in UV-irradiated SKH-hr1 transgenic mice. J Virol. 2006;80:11153–64. doi: 10.1128/JVI.00954-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bouwes Bavinck JN, Neale RE, Abeni D, Euvrard S, Green AC, Harwood CA, et al. Multicenter study of the association between betapapillomavirus infection and cutaneous squamous cell carcinoma. Cancer Res. 2010;70:9777–86. doi: 10.1158/0008-5472.CAN-10-0352. [DOI] [PubMed] [Google Scholar]
- 27.Euvrard S, Kanitakis J, Claudy A. Skin cancers after organ transplantation. N Eng J Med. 2003;348:1681–91. doi: 10.1056/NEJMra022137. [DOI] [PubMed] [Google Scholar]
- 28.Euvard S, Kanitakis J, Decullier E, Butnaru AC, Lefrançois N, Boissonnat P, et al. Subsequent skin cancers in kidney and heart transplant recipients after the first squamous cell carcinoma. Transplantation. 2006;81:1093–100. doi: 10.1097/01.tp.0000209921.60305.d9. [DOI] [PubMed] [Google Scholar]
- 29.Smith KJ, Hamza S, Skelton H. Histologic features in primary cutaneous squamous cell carcinomas in immunocompromised patients focusing on organ transplant patients. Dermatol Surg. 2004;30:634–41. doi: 10.1111/j.1524-4725.2004.30149.x. [DOI] [PubMed] [Google Scholar]
- 30.Parren LJ, Frank J. Hereditary tumour syndromes featuring basal cell carcinomas. Br J Dermatol. 2011;165:30–4. doi: 10.1111/j.1365-2133.2011.10334.x. [DOI] [PubMed] [Google Scholar]
- 31.Telfer NR, Colver GB, Morton CA British Association of Dermatologists. Guidelines for the management of basal cell carcinoma. Br J Dermatol. 2008;159:35–48. doi: 10.1111/j.1365-2133.2008.08666.x. [DOI] [PubMed] [Google Scholar]
- 32.Madan V, Lear JT, Szeimies RM. Nonmelanoma skin cancer. Lancet. 2010;375:673–85. doi: 10.1016/S0140-6736(09)61196-X. [DOI] [PubMed] [Google Scholar]
- 33.Arits AH, Sclangan MH, Nelemans PJ, Kelleners-Smeets NW. Trends in the incidence of basal cell carcinoma by histopathological subtype. J Eur Acad Dermatol Venereol. 2011;25:565–9. doi: 10.1111/j.1468-3083.2010.03839.x. [DOI] [PubMed] [Google Scholar]
- 34.Altamura D, Menzies SW, Argenziano G, Zalaudek I, Soyer HP, Sera F, et al. Dermatoscopy of basal cell carcinoma: Morphologic variability of global and local features and accuracy of diagnosis. J Am Acad Dermatol. 2010;62:67–75. doi: 10.1016/j.jaad.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 35.Mohs F. Chemosurgery: A microscopically controlled method of cancer excision. Arch Surg. 1941;42:279–95. [Google Scholar]
- 36.Rowe DE, Carroll RJ, Day CL., Jr Long-term recurrence rates in previously untreated (primary) basal cell carcinoma: Implications for patient follow-up. J Dermatol Surg Oncol. 1989;15:315–28. doi: 10.1111/j.1524-4725.1989.tb03166.x. [DOI] [PubMed] [Google Scholar]
- 37.Rowe DE, Carroll RJ, Day CL., Jr Prognostic factors for local recurrence, metastasis, and survival rates in squamous cell carcinoma of the skin, ear, and lip. Implications for treatment modality selection. J Am Acad Dermatol. 1992;26:976–90. doi: 10.1016/0190-9622(92)70144-5. [DOI] [PubMed] [Google Scholar]
- 38.Malhotra R, Huilgol SC, Huynh NT, Selva D. The Australian Mohs database, part II: Periocular basal cell carcinoma outcome at 5-year follow-up. Ophthalmology. 2004;111:631–6. doi: 10.1016/j.ophtha.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 39.Paoli J, Daryoni S, Wennberg AM, Mölne L, Gillstedt M, Miocic M, et al. 5-year recurrence rates of Mohs micrographic surgery for aggressive and recurrent facial basal cell carcinoma. Acta Derm Venereol. 2011;91:689–93. doi: 10.2340/00015555-1134. [DOI] [PubMed] [Google Scholar]
- 40.Leibovitch I, Huilgol SC, Selva D, Hill D, Richards S, Paver R. Cutaneous squamous cell carcinoma treated with Mohs micrographic surgery in Australia I.Experience over 10 years. J Am Acad Dermatol. 2005;53:253–60. doi: 10.1016/j.jaad.2005.02.059. [DOI] [PubMed] [Google Scholar]
- 41.Pugliano-Mauro M, Goldman G. Mohs surgery is effective for high-risk cutaneous squamous cell carcinoma. Dermatol Surg. 2010;36:1544–53. doi: 10.1111/j.1524-4725.2010.01576.x. [DOI] [PubMed] [Google Scholar]
- 42.Smeets NW, Krekels GA, Ostertag JU, Essers BA, Dirksen CD, Nieman FH, et al. Surgical excision vs Mohs’ micrographic surgery for basal-cell carcinoma of the face: Randomised controlled trial. Lancet. 2004;364:1766–72. doi: 10.1016/S0140-6736(04)17399-6. [DOI] [PubMed] [Google Scholar]
- 43.Wolf DJ, Zitelli JA. Surgical margins for basal cell carcinoma. Arch Dermatol. 1987;123:340–4. [PubMed] [Google Scholar]
- 44.Brodland DG, Zitelli JA. Surgical margins for excision of primary cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1992;27:241–8. doi: 10.1016/0190-9622(92)70178-i. [DOI] [PubMed] [Google Scholar]
- 45.NCCN Guidelines™ and Clinical Resources. [Last accessed on 2012 Jan 7]. Available from: http://www.nccn.org/professionals/physiciangls/f_guidelines.asp .
- 46.LeBoeuf NR, Schmults CD. Update on the management of high-risk squamous cell carcinoma. Semin Cutan Med Surg. 2011;30:26–34. doi: 10.1016/j.sder.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 47.Licher MD, Karagas MR, Mott LA, Spencer SK, Stukel TA, Greenberg ER. Therapeutic ionizing radiation and the incidence of basal cell carcinoma and squamous cell carcinoma. Arch Dermatol. 2000;136:1007–11. doi: 10.1001/archderm.136.8.1007. [DOI] [PubMed] [Google Scholar]
- 48.Huang CC, Boyce SM. Surgical margins of excision for basal cell carcinoma and squamous cell carcinoma. Semin Cutan Med Surg. 2004;23:167–73. doi: 10.1016/j.sder.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 49.Peikert JM. Prospective trial of curettage and cryosurgery in the management of non-facial, superficial, and minimally invasive basal and squamous cell carcinoma. Int J Dermatol. 2011;50:1135–8. doi: 10.1111/j.1365-4632.2011.04969.x. [DOI] [PubMed] [Google Scholar]
- 50.Sheridan AT, Dawber RP. Curettage, electrosurgery and skin cancer. Australas J Dermatol. 2000;41:19–30. doi: 10.1046/j.1440-0960.2000.00383.x. [DOI] [PubMed] [Google Scholar]
- 51.Kuflik EG. Cryosurgery for skin cancer: 30-year experience and cure rates. Dermatol Surg. 2004;30:297–300. doi: 10.1111/j.1524-4725.2004.30090.x. [DOI] [PubMed] [Google Scholar]
- 52.Morton CA, McKenna KE, Rhodes LE British Association of Dermatologists Therapy Guidelines and Audit Subcommittee and the British Photodermatology Group. Guidelines for topical photodynamic therapy: Update. Br J Dermatol. 2008;159:1245–66. doi: 10.1111/j.1365-2133.2008.08882.x. [DOI] [PubMed] [Google Scholar]
- 53.Stebbins WG, Hanke CW. MAL-PDT for difficult to treat nonmelanoma skin cancer. Dermatol Ther. 2011;24:82–93. doi: 10.1111/j.1529-8019.2010.01381.x. [DOI] [PubMed] [Google Scholar]
- 54.Basset-Seguin N, Ibbotson SH, Emtestam L, Tarstedt M, Morton C, Maroti M, et al. Topical methyl aminolaevulinate photodynamic therapy versus cryotherapy for superficial basal cell carcinoma: A 5 year randomized trial. Eur J Dermatol. 2008;18:547–53. doi: 10.1684/ejd.2008.0472. [DOI] [PubMed] [Google Scholar]
- 55.Karve SJ, Feldman SR, Yentzer BA, Pearce DJ, Balkrishnan R. Imiquimod: A review of basal cell carcinoma treatments. J Drugs Dermatol. 2008;7:1044–51. [PubMed] [Google Scholar]
- 56.Quirk C, Gebauer K, De’Ambrosis B, Slade HB, Meng TC. Sustained clearance of superficial basal cell carcinomas treated with imiquimod cream 5%: Results of a prospective 5-year study. Cutis. 2010;85:318–24. [PubMed] [Google Scholar]
- 57.Romagosa R, Saap L, Givens M, Salvarrey A, He JL, Hsia SL, et al. A pilot study to evaluate the treatment of basal cell carcinoma with 5-fluorouracil using phosphatidyl choline as a transepidermal carrier. Dermatol Surg. 2000;26:338–40. doi: 10.1046/j.1524-4725.2000.99227.x. [DOI] [PubMed] [Google Scholar]
- 58.Stasko T, Brown MD, Carucci JA, Euvrard S, Johnson TM, Sengelmann RD, et al. Guidelines for the management of squamous cell carcinoma in organ transplant recipients. Dermatol Surg. 2004;30:642–50. doi: 10.1111/j.1524-4725.2004.30150.x. [DOI] [PubMed] [Google Scholar]
- 59.Kwasniak LA, Garcia-Zuazaga J. Basal cell carcinoma: Evidence-based medicine and review of treatment modalities. Int J Dermatol. 2011;50:645–58. doi: 10.1111/j.1365-4632.2010.04826.x. [DOI] [PubMed] [Google Scholar]
- 60.Leibovitch I, Huilgol SC, Selva D, Richards S, Paver R. Basal cell carcinoma treated with Mohs surgery in Australia II. Outcome at 5-year follow-up. J Am Acad Dermatol. 2005;53:452–7. doi: 10.1016/j.jaad.2005.04.087. [DOI] [PubMed] [Google Scholar]
- 61.Mosterd K, Krekels GA, Nieman FH, Ostertag JU, Essers BA, Dirksen CD, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: A prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008;9:1149–56. doi: 10.1016/S1470-2045(08)70260-2. [DOI] [PubMed] [Google Scholar]
- 62.Silverman MK, Kopf AW, Gladstein AH, Bart RS, Grin CM, Levenstein MJ. Recurrence rates of treated basal cell carcinomas. Part 4: X-ray therapy. J Dermatol Surg Oncol. 1992;18:549–54. doi: 10.1111/j.1524-4725.1992.tb03508.x. [DOI] [PubMed] [Google Scholar]
- 63.Rodriguez-Vigil T, Vázquez-López F, Perez-Oliva N. Recurrence rates of primary basal cell carcinoma in facial risk areas treated with curettage and electrodesiccation. J Am Acad Dermatol. 2007;56:91–5. doi: 10.1016/j.jaad.2006.07.007. [DOI] [PubMed] [Google Scholar]


