Abstract
BACKGROUND:
A wide range of medications are now available for the treatment of asthma and selection of the optimal treatment combination of agents is essential.
OBJECTIVES:
This study was designed to evaluate a self-reported drug prescribing pattern for asthma among Nigerian doctors in general practice.
METHODS:
It was a cross-sectional survey conducted among general practitioners in six states of Nigeria.
RESULTS:
For acute severe asthma, 75.9% of the doctors prescribed intravenous methylxanthines, which was combined with oral or inhaled short-acting β2 agonists (SABA) by 56.3% of them. Systemic steroids were prescribed mainly via the intravenous route by 58.8% of them. Aberrant drugs such as antibiotics, antihistamines, and mucolytics were prescribed by 25.6% of them. For long-term, follow-up treatment of asthma, oral steroids, and oral SABA were commonly prescribed, while inhaled corticosteroids (ICS) and ICS/LABA (long acting beta agonists) were infrequently prescribed. Aberrant drugs such as analgesics, antimalaria, and antihistamines were prescribed by 22.8% of them. About 48% of the doctors had never attended any form of update training on asthma management, whereas, only 16.3% attended update training on asthma within the last year preceding this study. Awareness of international guidelines on asthma treatment was poor among them with only 16.4% being able to mention any correct guideline on asthma management.
CONCLUSION:
The poor anti-asthma prescribing behavior among these doctors is associated with a low level of participation at update training on asthma management and poor awareness of asthma guidelines. The Nigerian Medical Association and the Nigerian Thoracic Society should urgently address these problems.
Keywords: Asthma, drug prescription, general practitioners, Nigeria
Asthma is defined as a chronic inflammatory disease of the airways, characterized by an obstruction of airflow, which may be completely or partially reversed with or without specific therapy. The chronic airway inflammation is associated with airway hyperreactivity or bronchial hyperresponsiveness (BHR), which is defined as the tendency of the airways to narrow in response to various stimuli (e.g., environmental allergens and irritants).[1–3]
Asthma is a global public health problem that afflicts nearly 300 million people and causes more than 250,000 deaths annually.[1,4] It affects children and adults of all ages and its prevalence is increasing, particularly among children.[1] Although its prevalence is highest in industrialized countries, it is a greater economic and public health burden in the developing world. Surveys indicate that the majority of patients in the developed and developing countries do not receive optimal care, and are therefore, not well controlled. Poorly managed asthma may cause significant morbidity and mortality, but early treatment, proper administration of medication, and monitoring of the disease can decrease the frequency of exacerbation, hospitalization, and mortality rate. A wide range of different classes of medication are now available for the treatment of asthma and a selection of the optimal treatment combination of agents is essential to ensure that the disease is well-controlled.[5] This together with the complexity of asthma leads to the development of international guidelines[1,4] to assist the clinicians in the management of their asthma patients.
Even as several studies had been carried out to assess asthma management in many countries of the world,[6–9] there is paucity of data on the assessment of asthma management in Nigeria. As in many counties of the world, management of patients with asthma in Nigeria is largely performed by general practitioners (GPs). We are not aware of any previously published study on the assessment of asthma management among GPs in Nigeria. Furthermore, records of asthma patients referred to us by the GPs indicated that their management was not according to the internationally recommended guidelines. This study was therefore designed to evaluate the self-reported drug prescribing pattern for asthma among GPs in Nigeria.
Methods
This was a cross-sectional survey conducted from March to August 2010, among doctors in general practice in six states (three in the North and three in the South) of Nigeria. The states were selected for the convenience of the investigators.
Study site
Nigeria is the most populous black nation in the world, with a population of over 140 million people.[10] It is located in West Africa and is bounded in the North by the Niger republic, in the South by the Atlantic ocean, in the West by the Benin republic, and in the East by Cameroon.
Nigeria has no state-supported social welfare system. Medical care is wanting among a majority of the population. Despite several attempts by the government to reform the health sector, a majority of the population lack access to primary health care. Health facilities are often understaffed, underequipped, and low on medications. In spite of the introduction of the National Health Insurance Scheme (NHIS) more than five years ago, in 2005, only about 5.3 million (3.73%) of the population are covered by the scheme.[11] Those who are not covered by NHIS pay out of their pockets for medical care.
Selection of participants
There is no reliable healthcare database for Nigeria. Also, a national directory for doctors in Nigeria is still in the pipeline at the time of this study. Therefore, we had contact with the doctors at their working place. The participants were medical officers (doctors with only basic medical qualification without postgraduate medical training in general/family medicine), resident doctors (trainees in general/family practice), and Fellows in general/family practice (doctors with postgraduate medical training in general/family practice), from six states in Nigeria. They were recruited from public and private hospitals in the capital cities of the selected states. However, doctors from the Federal Medical Center Bida (Niger state) and Federal Medical Center Iddo (Ekiti state) were included in the survey, despite being outside the state capital. This was because the two centers were the Federal Tertiary Health Institutions in the affected states at the time of study. Only those who consented to participate in the study were recruited. These general practitioners treated asthma patients with acute exacerbation as well as those who were on outpatient follow-up.
Administration of questionnaires
A pre-tested, self-administered questionnaire was developed to obtain information from the recruited doctors. It was in English, the official language of the country. A pilot study was conducted and necessary corrections were made on the questionnaire. Information obtained with the corrected version of the questionnaire included age as on last birthday, gender, basic medical qualification obtained, with dates, additional medical qualification obtained, with dates, working status (medical officers, residents training in general/family practice and Fellows in general/family practice), state in which practice was located, and practice setting (private or public). They were also requested to list the drug(s) (with routes) they normally prescribed for acute severe asthma in an emergency and for long-term control of asthma, during follow-up visits. Acute severe asthma was defined as an exacerbation of asthma associated with one or more of the following: Inabilities: To complete a sentence in one breath, respiratory rate ≥25/minute, pulse rate ≥110/minute, and peak expiratory flow of 33–50%, best or predicted. Information was also obtained on what guided their choice of drugs as well as when last they attended any form of update training on asthma management.
Each of the consenting doctors completed a questionnaire. Those who participated in the pilot study were excluded from the survey because we assumed that they would have sought information on the items contained in the questionnaire. At each of the hospitals visited, questionnaires were distributed and collected back after about 30 minutes. The questionnaires were filled in the presence of the investigators. In some cases in which a participant was too busy, an appointment was rescheduled for a later date.
Data analysis was done using the SPSS version 13.0. The mean±standard deviation was calculated for the numerical variables. Percentages were calculated for the categorical variables and the Chi-squared (χ2) test was used to determine the significance of the observed differences. A P value of <0.05 was taken as significant.
Results
General characteristics
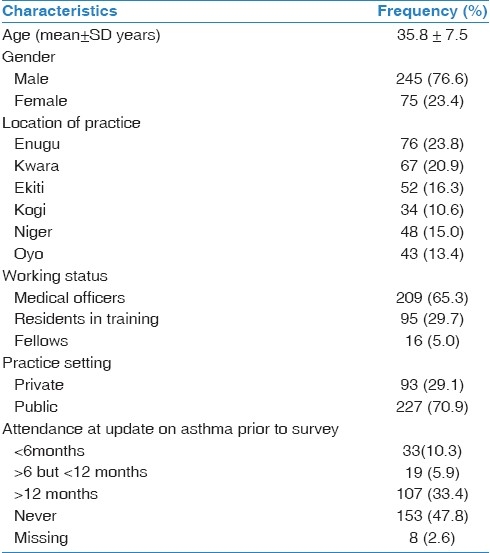
Out of the 334 GPs contacted, 320 (95.8%) participated in the survey. Their general characteristics are as shown in Table 1. Their mean age was 35.8±7.5 years with a range of 25 to 70 years. Most of them were males practicing in public hospitals. They had been practicing after a basic medical qualification, for a mean of 8.3±7.1 years, with a range of two to 41 years. The Fellows had been practicing, after postgraduate medical training, for an average of 9.0±7.7 years with a range of one to 28 years. Two hundred and nine (65.3%) were medical officers. Attendance at update training on asthma management was generally poor among the doctors. Only 52 (16.3%) of them had attended any form of update training on asthma management within the last year, prior to this survey. On the other hand, 153 (47.8%) of 312 doctors who responded to this item had never attended any form of update training on asthma management.
Table 1.
Characteristics of the responding general practitioners
Drug prescription for asthma
Drug prescription for asthma by the doctors is highlighted in Tables 2 and 3. For acute severe asthma, 243 (75.9%) doctors prescribed intravenous (IV) methylxanthines. The medical officers (P<0.001) and doctors in private practice (P<0.001) significantly prescribed IV methylxanthines, more than other categories of doctors. Inhaled short-acting β2 agonists (SABA) were prescribed by 160 (50.0%) doctors, especially by resident doctors who significantly (P<0.001) prescribed it more than other categories. Oral SABA was prescribed more by medical officers (P=0.006). Combination of IV methylxanthines and SABA (oral or inhaled) was prescribed by 180 (56.3%) doctors (not shown in the Tables). The doctors in the public and private settings did not differ significantly in the way they prescribed inhaled and oral SABA. Systemic steroids were prescribed for acute severe asthma, mainly via the IV route, by 188 (58.8%) doctors. Those in the private setting prescribed IV steroids significantly more than those in the public setting (P=0.005). Oral steroids were prescribed by 111 (34.7%) doctors, without any significant difference in the prescription pattern, according to the working status and practice setting of the physicians. As shown in Table 3, physicians in Enugu state were less likely to prescribe IV and oral steroids (P=0.006 and 0.002, respectively) for acute severe asthma than those in other states. There were no significant differences in the prescribing pattern of other drugs for acute severe asthma among all the states. Eighty-two (25.6%) doctors prescribed other drugs such as antibiotics, antihistamines, and mucolytics for acute severe asthma.
Table 2.
Drugs prescribed according to the working status and practice setting of the general practitioners
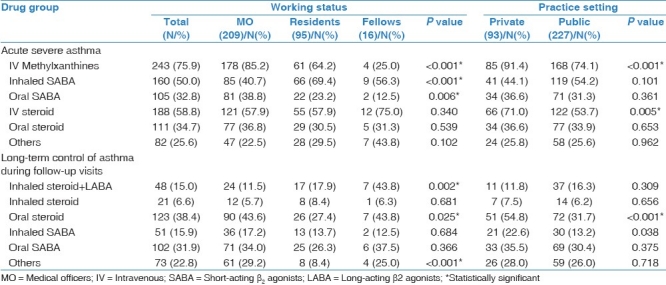
Table 3.
Drug prescribing pattern according to the location of the general practitioners
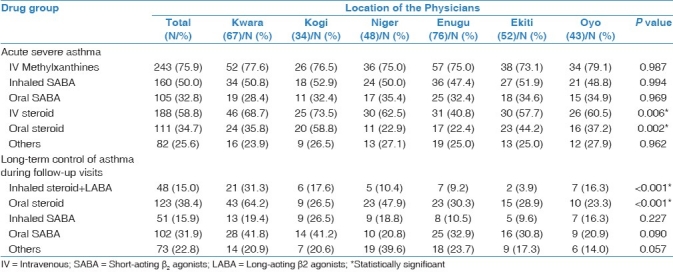
For long-term control of asthma during follow-up visits, 48 (15.0%) doctors prescribed combined inhaled corticosteroids plus long-acting β2 agonists (ICS/LABA). The Fellows (P=0.002) and doctors in Kwara state (P<0.001) prescribed it more than other categories of doctors. Inhaled steroids were prescribed by 21 (6.6%) doctors. Oral steroids were prescribed by 123 (38.4%) doctors, especially those in private practice (P<0.001) and in Kwara state (P<0.001). Seventy-three (22.8%) doctors prescribed various other drugs such as analgesics, antimalaria, and antihistamines.
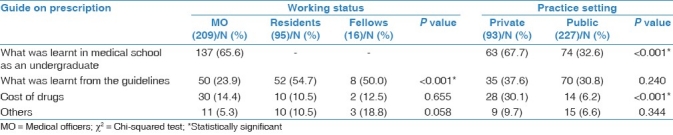
Table 4 shows the factors that guided the physicians in their choice of drugs. The major factor that guided the medical officers in their choice of drugs for asthma treatment was what they learnt as undergraduates in medical school (137; 65.6%). The resident doctors and the Fellows were not guided by this factor. Only 42 (13.1%) doctors were guided by the cost in their choice of drugs. Expectedly, more private practitioners were guided by cost than those in the public hospital. Fifty-two (54.7%) resident doctors, eight (50.0%) Fellows, and 50 (23.9%) medical officers were guided by recommendations from guidelines in their choice of drugs. However, just 18 (16.4%) of these 110 doctors were able to mention the correct guidelines.
Table 4.
Factors that guided the general practitioners in their choice of drugs
Discussion
This survey has shown a huge gap in the knowledge of Nigerian doctors, in general practice, on the management of asthma patients. It shows that despite the availability of effective therapies and development of international guidelines to assist in the management of asthma patients, the prescribing practices of many of the doctors do not conform to internationally recommended guidelines. This finding is in agreement with previous studies in other countries, which have revealed a poor quality of drug prescription for asthma by doctors.[6–9]
Over 75% of the doctors reported that they usually prescribed IV methylxanthines for patients with acute severe asthma. This was sometimes prescribed in combination with oral or inhaled SABA by the doctors. This practice was in sharp contrast to the international guidelines.[1,4] Although methylxanthines were once a standard treatment for asthma in an emergency, it is now known that their use increases the risk of adverse events, without improving the outcomes. They were only recommended if inhaled SABA was not available.[1,12] In spite of these and other evidences that IV methylxanthines are less effective than inhaled SABA,[13,14] IV methylxanthines are still commonly used in emergency treatment of asthma even in combination with SABA. As they were prescribed with SABA by 56.3% of the doctors, it meant the doctors did not prescribe it because SABA was not available. Oral SABA was also commonly prescribed by the doctors. Oral administration of SABA was not recommended, as it had not been shown to be more effective than inhaled SABA and was associated with an increased frequency of side effects.[15]
In tandem with the international recommendations, systemic steroids were commonly prescribed for acute severe asthma by more than 90% of the doctors. However, almost 60% of them prescribed the IV formulation rather than the recommended oral steroids. The routine use of IV steroids would increase the cost of treatment and produce unwanted adverse effects, without any significant advantage over the oral steroids. On the other hand, the oral steroid was usually preferred in the absence of contraindications, because it was equally effective and less invasive.[16] Other agents like antibiotics, antihistamines, and mucolytics, which were not routinely recommended for acute exacerbations of asthma[1] were also prescribed by a quarter of the doctors. These agents increased the cost of prescription, produced unwanted adverse effects, and could delay the use of appropriate therapy.
A disturbing finding in this survey was the common prescription of oral steroids and oral SABA for long-term control of asthma during follow-up visits. Although oral steroids were effective in controlling symptoms and were cheap, their prolonged use could result in serious unwanted effects. Therefore, continuous treatment with oral steroids was generally avoided, except for the most difficult-to-control asthma.[1,4] Similarly, the regularly scheduled, daily use of SABA was not recommended, as it had no demonstrable benefits,[17] and might in fact be deleterious in some patients with asthma. The chronic use of SABA was associated with an increased risk of an acute exacerbation that required an emergency department visit or hospitalization.[18–20] Also, a decrease in lung function after stopping chronic use have been reported with a regular use of SABA.[21,22]
A more worrisome finding is the infrequent prescription of ICS (6.6%) and ICS/LABA (15.0%) for a long-term control of asthma, during follow-up visits. Several earlier studies have shown that inhaled steroids with or without inhaled LABA are the medications of choice for persistent asthma, as they are effective and have a low-rate of side effects.[23,24] Postma et al.,[25] reported that ICS monotherapy and ICS plus LABA effectively controlled daily symptoms in their asthma patients.
Generally, the cost of drugs does not seem to play a major role in the prescribing pattern of these doctors because only 42 (13.1%) of the physicians reported that that they were guided by cost in their choice of drugs. However, despite the fact that just 13.1% of the physicians were guided by cost, it is important to note that cost significantly influenced drug prescription among private practitioners, rather than those working in public health institutions [Table 4].
A factor that may explain the poor drug prescription for asthma by the doctors is their low level of participation in the update training on asthma. Almost half of the doctors (47.8%) had never attended any form of update training on asthma, whereas, only 16.3% attended any form of update within the last year preceding this survey. The low level of participation in asthma management programs has been reported in earlier studies.[26] One possible explanation for the poor participation of the doctors in the training on asthma management is the lack of well-organized, regular, continuing medical education in Nigeria, at the time the survey was carried out. This may explain why 65.6% of the medical officers relied on what they had learnt in medical school in the treatment of their patients, several years after graduation. We hope that this trend will change with the recent introduction of continuing medical education credits by the Medical and Dental Council of Nigeria for the renewal of practicing license with effect from year 2012.
Another equally important finding that may further account for the poor prescribing pattern of the doctors is their poor awareness of the international guidelines on asthma treatment. Although 110 (34.4%) doctors claimed that their prescriptions were guided by recommendations from guidelines, only a surprisingly low 16.4% of them were able to mention the correct guidelines. This may be related to the lack of locally available national asthma guidelines in Nigeria. Therefore, the Nigerian Thoracic Society should follow the good example set by the Saudi Thoracic Society,[27] in the development of simple-to-understand, updated national asthma guidelines, for use by the non-asthma physicians. This should be combined with an extensive asthma campaign to popularize the use of the guidelines among our doctors. The impact of such a campaign on physicians’ prescription practices was reported in an earlier study by Al-Shimemeri et al.[28]
The interpretation of the results of our study has some limitations. The results reflect the reported prescription of doctors willing to participate in the study. Secondly, due to inadequate resources, we surveyed doctors in the capital cities, thereby leaving out those in the more remote areas. Another limitation is the fact that the states have been selected based on the location of the investigators. These factors would most likely have introduced a selection bias. Another limitation is the fact that the results are based on a self-reported prescribing pattern by the doctors, who may have been biased in their report. Finally, the reported prescribing behavior of the Fellows must be interpreted with some caution, as few of them participated in this study.
In spite of these limitations, this study has shown that poor anti-asthma-prescribing behavior among Nigerian doctors in general practice is associated with the low level of participation at the update training on asthma management, and poor awareness of asthma guidelines. Therefore, the Nigerian Medical Association should expedite action on the development of the recently introduced continuing medical education in the country, while the Nigerian Thoracic Society should urgently develop and circulate widely, national asthma guidelines that are fully adapted to the prevailing situation in Nigeria.[28]
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Global initiative for asthma (GINA) Pocket guide for asthma management and prevention: A pocket guide for physicians and nurses based on the global strategy for asthma management and prevention. Medical communication resources, inc. 2008 [Google Scholar]
- 2.Murphy KR. Asthma: Versatile treatment for a variable disease. J Asthma. 2005;42:149–57. [PubMed] [Google Scholar]
- 3.Fanta CH. Asthma. N Engl J Med. 2009;300:1002–14. doi: 10.1056/NEJMra0804579. [DOI] [PubMed] [Google Scholar]
- 4.Ait-Khalid N, Enarson DA, Chiang CY, Marks G, Bissell K. Management of asthma: A guide to the essentials of good clinical practice. 3rd ed. Paris, France: International Union Against Tuberculosis and Lung Disease; 2008. [PubMed] [Google Scholar]
- 5.Verleden GM, DeVuyst P. Assessment of asthma severity and treatment by GPs in Belgium: An asthma drug utilization research study (ADUR) Respir Med. 2002;96:170–7. doi: 10.1053/rmed.2001.1242. [DOI] [PubMed] [Google Scholar]
- 6.Jepson G, Butler T, Gregory D, Jones K. Prescribing patterns for asthma by general practitioners in six European countries. Respir Med. 2000;94:578–83. doi: 10.1053/rmed.2000.0782. [DOI] [PubMed] [Google Scholar]
- 7.Lagerlov P, Veninga CC, Muskova M, Hummers-Pradier E, Lundborg CS, Andrew M, et al. Asthma management in five European countries: Doctors’ knowledge, attitudes and prescribing behavior. Eur Respir J. 2000;15:25–9. [PubMed] [Google Scholar]
- 8.Koffi N, Kouassi B, Ngom AK, Kone MS, Danguy EA. Evaluation of management of asthma African adults, National survey among general physicians from Ivory Coast. Rev Mal Respir. 2001;18:531–6. [PubMed] [Google Scholar]
- 9.Hussain SF, Zahlid S, Khan JA, Haqqee R. Asthma management by general practitioners in Pakistan. Int J Tuberc Lung Dis. 2004;8:414–7. [PubMed] [Google Scholar]
- 10.National Population Commission of Nigeria. [Last Accessed on 2011 Feb];Final census results. 2006 Available from: http://www.population.gov.ng/ [Google Scholar]
- 11.Nigerian Health Watch: What hope for the National Health Insurance Scheme in 2010. [Last Accessed on 2011 Jan]. Available from: http://www.nigerianhealthwatch.com/2010/01/what-hope-for-national-health-insurance.html .
- 12.Parameswaran K, Benda J, Rowe BH. Addition of intravenous aminophylline to β2-agonists in adults with acute severe asthma. Cochrane Database Sys Rev. 2000;4:CD002742. doi: 10.1002/14651858.CD002742. [DOI] [PubMed] [Google Scholar]
- 13.Reed CE, Hunt LW. The emergency visit and management of athma. Ann Intern Med. 1990;112:801–2. doi: 10.7326/0003-4819-112-11-801. [DOI] [PubMed] [Google Scholar]
- 14.Milgrow H, Bender B. Current issues in the use of theophylline. Am Rev Respr Dis. 1993;147:553–9. doi: 10.1164/ajrccm/147.6_Pt_2.S33. [DOI] [PubMed] [Google Scholar]
- 15.Lazarus SC. Emergency treatment of asthma. N Engl J Med. 2010;363:755–64. doi: 10.1056/NEJMcp1003469. [DOI] [PubMed] [Google Scholar]
- 16.Raho D, Alfaro C, Sipsey J, Glowsky MM, Sharma OP. Are intravenous corticosteroids required in status asthmatics? JAMA. 1998;260:527–9. [PubMed] [Google Scholar]
- 17.Dennis SM, Sharp SJ, Vickers MR, Frost CD, Crompton GK, Barnes PJ, et al. Regular inhaled salbutamol and asthma control: The TRUST randomized trial.Therapy Working Group of the National Asthma Task Force and the MRC General practice Research Framework. Lancet. 2000;355:1675–9. doi: 10.1016/s0140-6736(00)02238-8. [DOI] [PubMed] [Google Scholar]
- 18.Schatz M, Nakahiro R, Crawford W, Mendoza G, Mossen D, Stilbolt TB. Asthma quality-of-care markers using administrative data. Chest. 2005;128:1968–73. doi: 10.1378/chest.128.4.1968. [DOI] [PubMed] [Google Scholar]
- 19.Wraight JM, Hancox RJ, Herbison GP, Cowan JO, Flannery EM, Taylor DR. Bronchodilator tolerance: The impact of increasing bronchoconstriction. Eur Respir J. 2003;21:810–5. doi: 10.1183/09031936.03.00067503. [DOI] [PubMed] [Google Scholar]
- 20.Wraight JM, Smith AD, Cowan JO, Flannery EM, Herbison GP, Taylor DR. Adverse effecs of short-acting β-agonists: Potential impact when anti-inflammatory therapy is inadequate. Respirology. 2004;9:215–21. doi: 10.1111/j.1440-1843.2004.00557.x. [DOI] [PubMed] [Google Scholar]
- 21.VanSchayck CP, Cloosterman SG, Bijl-Hofland ID, Van den Hoogen H, Folgening HT, VanWeel C. Is the increase in bronchial responsiveness or FEV1 shortly after cessation of β2-agonists reflecting a real deterioration of the disease in allergic asthmatic patients? A comparison between short-acting and long-acting β2 -agonists. Respir Med. 2002;96:155–62. doi: 10.1053/rmed.2001.1243. [DOI] [PubMed] [Google Scholar]
- 22.Hancox RJ, Cowan JO, Flannery EM, Herbison GP, Mclachlan CR, Taylor DR. Bronchodilator tolerance and rebound bronchoconstriction during regular inhaled β-agonist treatment. Respir Med. 2000;94:767–71. doi: 10.1053/rmed.2000.0820. [DOI] [PubMed] [Google Scholar]
- 23.Greenstone IR, NiChroinin Mn, Masse V, Danish A, Magdalinos H, Zhang X, et al. Combination of inhaled long acting β2 -agonists and inhaled steroids versus high dose of inhaled steroids in children and adults with persistent asthma. Cochrane Database Syst Rev. 2005;4:ID005533. doi: 10.1002/14651858.CD005533. [DOI] [PubMed] [Google Scholar]
- 24.Masoli M, Weatheral M, Holt S, Bealey R. Moderate dose inhaled corticosteroids plus salmeterol versus higher doses of inhaled corticosteroids in symptomatic asthma. Thorax. 2005;60:730–4. doi: 10.1136/thx.2004.039180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Postma DS, O’Byrne PM, Pedersen S. Comparison of the effect of low-dose Ciclesonide and fixed-dose fluticasone propionate and salmeterol combination on long-term asthma control. Chest. 2011;139:311–8. doi: 10.1378/chest.09-1735. [DOI] [PubMed] [Google Scholar]
- 26.Sarrel EM, Mandelberg A, Cohen HA, Kahan E. Compliance of primary care doctors with asthma guidelines and related education. Isr Med Assoc J. 2002;4:403–6. [PubMed] [Google Scholar]
- 27.Al-Moamary MS, Al-Hajjaj MS, Idrees MM, Zeitouni MO, Alanezi MO, Al-Jahdali H, et al. The Saudi initiatives for asthma. Ann Thorac Med. 2009;4:216–33. doi: 10.4103/1817-1737.56001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Shimemeri A, Al-Ghadeer H, Giridhar H, Al-Jahdali H, Al-moamary M, Khan J, et al. Impact of an extensive asthma education campaign for physicians on their drug prescription practices. Ann Thorac Med. 2006;1:20–5. [Google Scholar]


