Abstract
Background:
Although electroconvulsive therapy (ECT) is used quite frequently among the bipolar patients in developing countries, very little data are available with regard to its effectiveness from the developing countries.
Aim:
A retrospective case note review was carried out of bipolar disorder patients who were given ECT.
Materials and Methods:
Details of demographic and clinical profile, indications for ECT, response patterns, adverse effects, etc. were recorded.
Results:
Among all the patients who received ECT, 18% were diagnosed to have bipolar disorder. ECT was administered most commonly for mania with psychotic symptoms, followed by severe depression with psychotic symptoms. Comorbid physical problems were seen in many patients. Nearly 90% of patients in both the subgroups showed more than 50% response (based on reduction in the standardized rating scales) with ECT. Few patients (22%) reported some kind of side effects.
Conclusions:
ECT is useful in the management of acute phase of mania and depression.
Keywords: Bipolar disorder, electroconvulsive therapy, mania, depression
INTRODUCTION
Prior to introduction of neuroleptics and mood stabilizers, electroconvulsive therapy (ECT) was one of the mainstays of treatment of both manic and depressive phases of bipolar affective disorder (BPAD). However, over the years, with the evolution of more and more mood stabilizers and neuroleptics, and controversies surrounding the use of ECT, its use has reduced in the treatment of BPAD. Various recent treatment guidelines for BPAD from the Western countries recommend the use of ECT very low in their treatment algorithms.[1–8]
It is now known that use of antidepressants in bipolar depression can lead to manic switches, mixed state induction and cycle acceleration.[9–12] Studies have also shown that ECT has equal efficacy and leads to similar symptomatic and functional recovery in unipolar and bipolar depression[13–17] and probably patients with bipolar depression respond faster than those with unipolar depression.[15–18] Efficacy of ECT in manic phase in terms of remission or marked clinical improvement has been reported to be about 80%.[19] It is also reported to be equally or more efficacious than psychotropic medications like lithium, chlorpromazine, and haloperidol.[20–27] In a recent review of the use of ECT in BPAD, the authors found 51 studies reporting its efficacy and safety. The authors noted that very few studies had a controlled design or were comparative prospective studies.[28]
Despite the emergence of newer mood stabilizers and atypical antipsychotics in the treatment of BPAD, there is an increasing population of treatment-resistant BPAD patients. These patients have rapid cycling, residual symptoms, suicide attempts, and severe impairment in socio-occupational functioning.[29] All these data suggest that ECT still has an important role in the management of BPAD.
A survey of practice of ECT in India showed that after schizophrenia, major depression (which includes both unipolar and bipolar depression) and mania are the most common indications for ECT[30] and a similar trend has also been reported for Asian countries by the same group of authors.[31] The survey from India showed that depression is the indication for ECT in about one-third of the patients (33.5%) and mania is an indication for 17.9% of patients receiving ECT[30] and similar percentages have been reported in the survey of practice of ECT in Asian countries.[31] However, very little data are available with regard to the use of ECT in bipolar depression and mania from the developing countries. In one of the earlier studies from our center, Sikdar et al.[25] showed that combination of chlorpromazine and ECT was significantly better than either treatment when given alone. In a recent study, Hiremani et al.[32] from Bangalore reported faster decline in mean Young Mania Ratings in patients of acute mania with bifrontal ECT compared with bitemporal ECT. Another study from Vellore examined the speed of improvement and remission in people with mania undergoing bilateral, brief-pulse, twice-weekly ECT at stimulus intensities administered just above and 2.5 times their individually titrated seizure threshold and reported both the interventions to be equally efficacious.[33]
The present study was an attempt at studying the clinical profile of BPAD patients who receive ECT and to study the effectiveness of ECT in patients with BPAD.
MATERIALS AND METHODS
Setting
This study was carried out at the Postgraduate Institute of Medical Education and Research, Chandigarh, a multispecialty teaching and tertiary-care referral hospital providing services to a major part of North India.
Assessment
All patients who attend the department usually undergo a detailed assessment under the supervision of a consultant. The family is generally involved in the assessment as well as subsequent treatment. All information is recorded in case notes. Diagnoses are based on International Statistical Classification of Diseases, Tenth Revision (ICD-10).[34]
Electroconvulsive therapy machine and administration
ECT is administered on both inpatient and outpatient basis. The consultant-in-charge of the patient makes the final decision about administering ECT after discussion with members of the treatment team. In complicated cases, a second opinion is usually sought from other consultants. The decision to administer ECT is taken individually in each patient, based on a review of his or her clinical status and previous treatment history. However, no mandatory guidelines regarding administration are followed. If ECT is clinically indicated, written informed consent is sought from patients and their relatives. Consenting patients undergo physical assessment and investigations as required and are also assessed by an anesthetist. If found fit, the patient is administered brief-pulse, bilateral, modified ECT. Modified ECT is administered using an indigenously manufactured brief-pulse, constant-energy/current machine (Medicaid Systems, Chandigarh, India). Electrical dose is calibrated in joules (range 36-135 J). The machine has settings for adjusting the duration of electric current passed (0.1-5 seconds with increments of 0.1 second), frequency between 20 and 90 Hz (settings of 20, 40, 50, 60, 70, and 90 Hz), and adjusting the pulse width from 0.1 to 1.5 seconds (0.1, 0.2, 0.5, 1, 1.2, and 1.5 seconds). Electroencephalographic (EEG) monitoring was introduced in 2009. Electrical dose is varied by changing the duration of current while keeping the frequency and pulse width constant. The initial duration of current is kept at 0.6 second. If the patient does not have an adequate seizure (motor seizure of 15-seconds duration or EEG seizure of 25 seconds), the duration is increased in increments of 0.1-0.2 seconds until the patient achieves a seizure of adequate duration. A maximum of three stimuli are usually given during the initial session to determine the seizure threshold. Electrical dose is adjusted in subsequent sessions to compensate for rise in seizure threshold and fall in seizure duration. ECT is administered thrice a week (Monday, Wednesday, and Saturday) by a trainee resident with the help of an anesthetist and supervised by senior residents and consultants. Atropine (0.2-0.3 mg)/glycopyrrolate (0.2-0.3 mg) is used as a premedication, thiopental sodium (150-450 mg) for induction, and succinylcholine (30-60 mg) for muscle relaxation. Earlier, cuff method was used to estimate seizure duration; however, recently EEG monitoring is done in addition to the cuff method for estimation of seizure duration. Motoric seizure of at least 15 seconds or an EEG seizure of 25 seconds is considered to be an effective ECT. Response to ECT is rated both clinically and on standardized scales such as the hamilton depression rating scale (HDRS) and the young mania rating scale (YMRS) for patients with affective disorders. ECT is stopped either when remission is achieved or when symptoms reach a plateau of improvement after two consecutive treatments. ECT is also usually discontinued if the patient does not respond to four to six treatments or if patients develop major complications (e.g. delirium) during ECT, which contraindicates further treatment. Treatment details are documented in the patient's case notes and in the ECT register, which is filled out by the trainee psychiatrist administering ECT and is checked weekly by the consultant in-charge of ECT services for completeness. All sedative/hypnotic agents are normally withdrawn or the dose is reduced before administration of ECT; other drugs are stopped only if they are judged to be interfering with ECT.
Procedure
The study was approved and given ethical clearance by the Departmental Research Review Committee. The ECT register was screened for patients who were diagnosed with BPAD at the time of administration of ECT, during the period of January 1999 to November 2008. The diagnoses of patients were also cross-checked for accuracy from the inpatient admission register and case notes. Eighty-five such patients were identified (some of them had received ECT on more than one occasion), but complete records of only 67 patients were available. Out of these, 37 were in the depressive phase and 30 were in the manic phase of their illness at the time of receiving ECT. Socio-demographic, clinical, and treatment data were extracted from these records.
Analysis
Descriptive statistics in terms of percentage were used for categorical variables; mean and SD were calculated for the continuous variables. Group comparisons were done using independent t-test for continuous variables and chi-square/Fisher exact test for categorical variables.
Response to electroconvulsive therapy
Extent of response to ECT was measured by the amount of reduction in average scores on rating scales (e.g. HDRS, YMRS) during the ECT course. The patients who had registered greater than 50% decrease (as is the norm in clinical trials) in rating scores were considered to have shown response.
RESULTS
Electroconvulsive therapy use in bipolar affective disorder
During the study period of about 10 years, 561 courses of ECT where administered, of which 101 (18%) were given to patients diagnosed with BPAD (16 patients with BPAD received more than one course) at the time of administration of ECT.
Socio-demographic profile
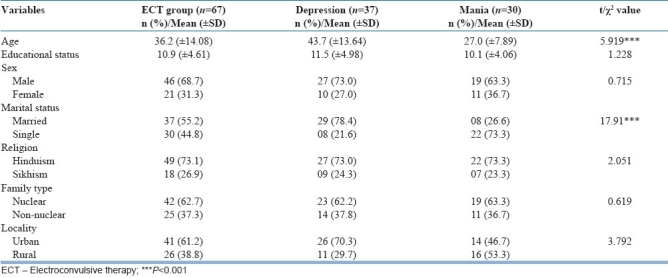
The mean age of the patients at the time of receiving ECT was 36.2 (SD 14.08) years. The mean age of patients who received ECT for mania was significantly less than that of those who received ECT for bipolar depression [Table 1]. There was no significant difference between the two groups (mania and depression) with regard to number of years of education, gender, religion, family type, and place of residence. Patients with mania were significantly more likely to be unmarried (22 vs. 6; χ2 =17.91, P<0.001) in comparison to patients with bipolar depression [Table 2].
Table 1.
Clinical profile of bipolar disorder patients receiving ECT
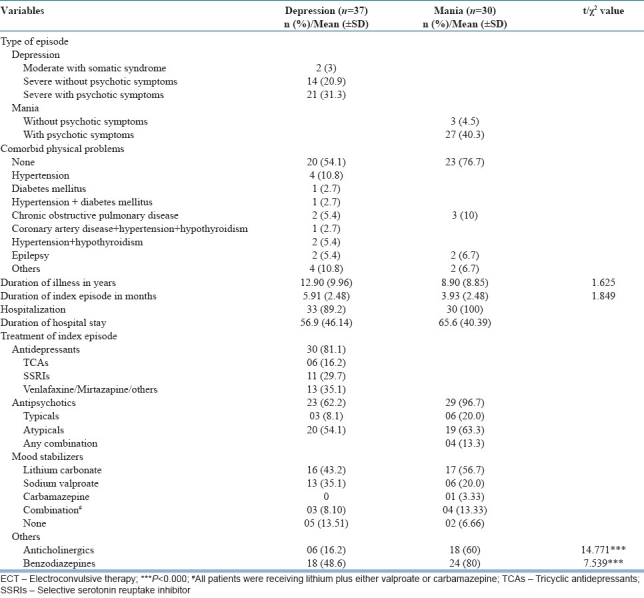
Table 2.
Socio-demographic profile of bipolar disorder patients who received ECT with respect to type of episode
Clinical profile
As shown in Table 1, ECT was administered most commonly for mania with psychotic symptoms (40.3%), followed by severe depression with psychotic symptoms (31%), severe depression without psychotic symptoms (21%), mania without psychotic symptoms (4.5%), and moderate depression with somatic syndrome (3%). The mean duration of illness at the time of administration of ECT was 11.20 (SD 9.63) years with no significant difference between those with mania and bipolar depression. The mean duration of the index episode was 5.04 (4.41) months. The duration of index episode was longer for patients with depression [Table 1]. Most were under inpatient care at the time of receiving ECT and the mean duration of hospital stay during the current episode was 56.9 days (SD=46.14) for patients with depression and 65.6 days (SD=40.39) for patients with mania. Less than half of the patients with depression (46%) and one-fourth of the patients with mania (23%) had a comorbid medical illness. The medical comorbidity in all the patients was treated in consultation with the concerned specialists before or while receiving ECT.
More than three-fourths of the patients with bipolar depression (81%) were receiving antidepressants concurrently with ECT for the index episode. About two-thirds of the patients with current episode of bipolar depression and almost all patients with current episode mania (97%) were receiving antipsychotics. Atypical antipsychotics were prescribed more often than typical agents; olanzapine (30.3%) and risperidone (21.2%) were the most often prescribed antipsychotics. Nearly three-fourths of the patients in both the groups were receiving only one conventional mood stabilizer (lithium carbonate, sodium valproate, or carbamazepine) at the time of receiving ECT. Anticholinergics and benzodiazepines were significantly more often prescribed in patients with mania (χ2 =14.771, P<0.000 and χ2 =7.539, P<0.000, respectively) [Table 1].
Administration of electroconvulsive therapy
As shown in Table 3, most of the patients in both the groups had more than one indication for ECT. All patients with moderate depression were administered ECT because of treatment resistance. Overall, ECT was considered treatment of choice in about 80% of patients with bipolar depression and 53% of patients with mania. The mean number of ECTs received by patients with bipolar depression was slightly less than that of those received by patients with mania.
Table 3.
Details of ECT administration in bipolar patients
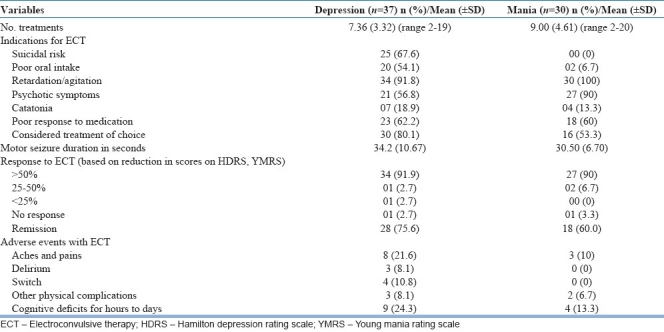
Response to electroconvulsive therapy
Nearly 90% of patients in both the subgroups showed more than 50% response (based on reduction in the standardized rating scales) with ECT. Remission (defined as decrease in the HDRS score to less than 8 and decrease in YMRS score to less than 7) occurred in two-thirds of patients with bipolar depression and slightly more than half of patients with mania [Table 3]. In terms of diagnostic subtype, the response rate was highest for severe depression with psychotic symptoms (100%) followed by mania with psychotic symptoms (92.6%). However, in terms of remission rates, it was the lowest for mania with psychotic symptoms (52.2%). In terms of response to ECT in patients with and without poor response to medication, there was no significant difference (89.7% with treatment resistance responded compared to 96.2% without treatment resistance).
Adverse effects
About 22% of the patients with depression and 10% patients with mania reported aches and pains after ECT [Table 3]. Other complications were less frequent. About one-fifth of the total patients reported subjective cognitive deficits lasting for hours to days after ECT, the most common being memory loss. About 24% of the patients with depression had cognitive deficits lasting for days (n=7; 18.9%), followed by hours (n=2; 5.4%). Among patients with mania, only 13.3% had cognitive deficits lasting for days. Delirium and switch of polarity occurred only in the patients with depression (n=3, 8.1% and n=4, 10.8%, respectively). Out of the three cases which developed delirium, two were on lithium and one was not receiving any mood stabilizer.
Correlational analysis
In the bipolar mania group, there was no correlation between remission and age, baseline YMRS scores, duration of illness, duration of current episode, total number of ECT treatments, energy used in terms of joules, and duration of seizure. However, in the depression group, there was negative correlation between remission and duration of current episode (Spearman rho=–0.437*; P<0.05), but not with any other variable described above.
DISCUSSION
ECT is an effective treatment for many psychiatric disorders and compared to the Western countries, it is used more frequently in India probably to reduce the duration of hospital stay.[25,35] Although some surveys have reported that mania is one of the common indications for ECT in India and other developing countries,[30,31] there is lack of data from the developing countries with regard to its effectiveness in BPAD. The present study attempted to fill this void, although its findings are limited by its retrospective nature and the small number of patients derived from one particular teaching hospital psychiatric unit in North India. Nevertheless, certain trends regarding the administration of ECT among patients with bipolar disorder were discernible. The patients with bipolar disorder who received ECT constituted 18% of the entire ECT courses administered over the 10-year period. This figure is less than that reported in two surveys of use of ECT, involving India and other Asian countries.[30,31] The possible reason for lower percentage in our study could be more stringent criteria for considering ECT. As is evident from our findings, almost all patients were tried on combination of mood stabilizer, antipsychotic, antidepressants and benzodiazepines, depending on the need prior to considering them for ECT. It is quite possible that many of the patients would respond to pharmacotherapy and only a subgroup of patients is left out for consideration for ECT.
The socio-demographic profile of patients with bipolar disorder who received ECT is typical of bipolar patients attending our clinic, as reported in some of our earlier studies,[36–38] suggesting that ECT is administered purely on the basis of clinical indication. In the current study, more than two-thirds of the patients who received ECT were males. This is in line with some of the Western studies.[39,40] This finding is also in line with higher male to female ratio among patients of all age groups being treated with ECT in India.[30] The treatment profile of patients receiving ECT is also in line with previous studies from our center[37,38] and is suggestive of our prescription patterns.
The exclusive use of bilateral ECT in all the patients is in line with the trend of almost exclusive use of bilateral ECT among patients in developing countries.[30,31,41,42]
Our findings suggest that among bipolar depressed patients, ECT is usually administered to those with severe psychotic illness and those who do not respond well to medications. Other indications included suicidal risk, poor oral intake, and severe behavioral disturbances such as retardation, agitation, or catatonia. These findings with regards to indications for ECT are in concurrence with the existing literature.[43–45] Despite the severe nature of the illness, the response to ECT was good. About 90% of patients in depression group showed more than 50% response and three-fourths of them achieved remission. Remission rates in bipolar depression noted in the present study are similar to those reported by Kho et al.[46] In their effort to identify the predictors of response to ECT in unipolar and bipolar depression, Kho et al.[46] reported that the medication treatment failure was not a predictor of response to ECT. Our finding of lack of significant difference in those with and without poor response to medication also supports the assertion of Kho et al.[46] Further, findings of our correlation analysis are also supported by Kho et al.[46] who found that duration of current episode predicted remission. This finding suggests that clinicians should not wait for too long to evaluate the efficacy of pharmacotherapy in bipolar depression, as it would reduce the chances of remission with ECT too.
With regard to mania, about 90% of patients with mania showed more than 50% response and three-fifths of patients with mania achieved remission. The response rate with respect to mania in the current study is in line with the existing literature[19] and some of the recent findings from India.[32]
One of the major concerns with the use of ECT is its adverse effects, especially those involving memory. The benign profile of adverse effects and the relative absence of serious side effects among bipolar patients in this study confirmed that when used with due caution, ECT is a safe option. Of the three cases which developed delirium, two were on lithium. When we see this figure in light of total patients receiving lithium (2 out of 40), only 5% of patients on lithium developed delirium. This figure is less than the figure of 10% reported by Jha et al.[47]
Our study is limited by its retrospective design, small sample size, and lack of comparison group.
In conclusion, the results of our study suggest that ECT is usually used in those patients with bipolar disorders who are severely ill and poorly responsive to medications. Patients with either polarity respond well to ECT, and the response to ECT in bipolar depression is predicted by duration of current episode.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder (revision) Am J Psychiatry. 2002;159(suppl 4):1–50. [PubMed] [Google Scholar]
- 2.Goodwin GM, Young AH. The British Association for Psychopharmacology guidelines for treatment of bipolar disorder: A summary. J Psychopharmacol. 2003;17(suppl 4):3–6. [PubMed] [Google Scholar]
- 3.Grunze H, Kasper S, Goodwin G, Bowden C, Baldwin D, Licht RW, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of bipolar disorders, Part I: Treatment of bipolar depression. World J Biol Psychiatry. 2002;3:115–24. doi: 10.3109/15622970209150612. [DOI] [PubMed] [Google Scholar]
- 4.Grunze H, Kasper S, Goodwin G, Bowden C, Baldwin D, Licht RW, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders, Part II: Treatment of mania. World J Biol Psychiatry. 2003;4:5–13. doi: 10.3109/15622970309167904. [DOI] [PubMed] [Google Scholar]
- 5.Kusumakar V, Yatham LN, Haslam DR, Parikh SV, Matte R, Silverstone PH, et al. Treatment of mania, mixed state, and rapid cycling. Can J Psychiatry. 1997;42(suppl 2):79S–86S. [PubMed] [Google Scholar]
- 6.Malhi GS, Mitchell PB, Salim S. Bipolar depression: Management options. CNS Drugs. 2003;17:9–25. doi: 10.2165/00023210-200317010-00002. [DOI] [PubMed] [Google Scholar]
- 7.Sachs GS, Printz DJ, Kahn DA, Carpenter D, Docherty JP. The expert consensus guideline series: Medication treatment of bipolar disorder 2000. Postgrad Med. 2000 Spec. No. 1-104. [PubMed] [Google Scholar]
- 8.Suppes T, Rush AJ, Dennehy EB, Crismon ML, Kashner TM, Toprac MG, et al. Texas Medication Algorithm Project, phase 3 (TMAP-3): Clinical results for patients with a history of mania. J Clin Psychiatry. 2003;64:370–82. doi: 10.4088/jcp.v64n0403. [DOI] [PubMed] [Google Scholar]
- 9.Altshuler LL, Post RM, Leverich GS, Mikalauskas K, Rosoff A, Ackerman L. Antidepressant-induced mania and cycle acceleration: A controversy revisited. Am J Psychiatry. 1995;152:1130–8. doi: 10.1176/ajp.152.8.1130. [DOI] [PubMed] [Google Scholar]
- 10.Ghaemi SN, Hsu DJ, Soldani F, Goodwin FK. Antidepressants in bipolar disorder: the case for caution. Bipolar Disord. 2003;5:421–33. doi: 10.1046/j.1399-5618.2003.00074.x. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg JF, Truman CJ. Antidepressant-induced mania: An overview of current controversies. Bipolar Disord. 2003;5:407–20. doi: 10.1046/j.1399-5618.2003.00067.x. [DOI] [PubMed] [Google Scholar]
- 12.Post RM, Altshuler L, Frye MA, Suppes T, Rush AJ, Keck PE, et al. Rate of switch in bipolar patients prospectively treated with second-generation antidepressants as augmentation to mood stabilizers. Bipolar Disord. 2001;3:259–65. [PubMed] [Google Scholar]
- 13.Abrams R, Taylor MA. Unipolar and bipolar depressive illness: Phenomenology and response to electroconvulsive therapy. Arch Gen Psychiatry. 1974;30:320–1. doi: 10.1001/archpsyc.1974.01760090038006. [DOI] [PubMed] [Google Scholar]
- 14.Black DW, Winokur G, Nasrallah A. ECT in unipolar and bipolar disorders: A naturalistic evaluation of 460 patients. Convuls Ther. 1986;2:231–7. [PubMed] [Google Scholar]
- 15.Daly JJ, Prudic J, Devanand DP, Nobler MS, Lisanby SH, Peyser S, et al. ECT in bipolar and unipolar depression: Differences in speed of response. Bipolar Disord. 2001;3:95–104. doi: 10.1034/j.1399-5618.2001.030208.x. [DOI] [PubMed] [Google Scholar]
- 16.Grunhaus L, Schreiber S, Dolberg OT, Hirshman S, Dannon PN. Response to ECT in major depression: Are there differences between unipolar and bipolar depression? Bipolar Disord. 2002;4:91–3. doi: 10.1034/j.1399-5618.4.s1.40.x. [DOI] [PubMed] [Google Scholar]
- 17.Zornberg GL, Pope HG. Treatment of depression in bipolar disorder: New directions for research. J Clin Psychopharmacol. 1993;13:397–408. [PubMed] [Google Scholar]
- 18.Perris C, d’Elia G. A study of bipolar (manic-depressive) and unipolar recurrent depressive psychoses: IX: Therapy and prognosis. Acta Psychiatr Scand. 1966;194(Suppl):153–71. [PubMed] [Google Scholar]
- 19.Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: A review of 50 years experience. Am J Psychiatry. 1994;151:169–76. doi: 10.1176/ajp.151.2.169. [DOI] [PubMed] [Google Scholar]
- 20.Thomas J, Reddy B. The treatment of mania: A retrospective evaluation of the effects of ECT, chlorpromazine, and lithium. J Affect Disord. 1982;4:85–92. doi: 10.1016/0165-0327(82)90038-6. [DOI] [PubMed] [Google Scholar]
- 21.Alexander RC, Salomon M, Ionescu-Pioggia M, Cole JO. Convulsive therapy in the treatment of mania: McLean Hospital 1973-1986. Convuls Ther. 1988;4:115–25. [PubMed] [Google Scholar]
- 22.Black DW, Winokur G, Nasrallah A. Treatment of mania: A naturalistic study of electroconvulsive therapy versus lithium in 438 patients. J Clin Psychiatry. 1987;48:132–9. [PubMed] [Google Scholar]
- 23.Strömgren LS. Electroconvulsive therapy in Aarhus, Denmark, in 1984: Its application in nondepressive disorders. Convuls Ther. 1988;4:306–13. [PubMed] [Google Scholar]
- 24.Small JG, Klapper MH, Kellams JJ, Miller MJ, Milstein V, Sharpley PH, et al. Electroconvulsive treatment compared with lithium in the management of manic states. Arch Gen Psychiatry. 1988;45:727–32. doi: 10.1001/archpsyc.1988.01800320037004. [DOI] [PubMed] [Google Scholar]
- 25.Sikdar S, Kulhara P, Avasthi A, Singh H. Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry. 1994;164:806–10. doi: 10.1192/bjp.164.6.806. [DOI] [PubMed] [Google Scholar]
- 26.Mukherjee S, Debsikdar V. Unmodified electroconvulsive therapy of acute mania: A retrospective naturalistic study. Convuls Ther. 1992;8:5–11. [PubMed] [Google Scholar]
- 27.Mukherjee S, Sackeim HA, Lee C. Unilateral ECT in the treatment of manic episodes. Convuls Ther. 1988;4:74–80. [PubMed] [Google Scholar]
- 28.Versiani M, Cheniaux E, Landeira-Fernandez J. Efficacy and safety of electroconvulsive therapy in the treatment of bipolar disorder: A systematic review. J ECT. 2011;27:153–64. doi: 10.1097/YCT.0b013e3181e6332e. [DOI] [PubMed] [Google Scholar]
- 29.Isasi AG, Echeburúa E, Limiñana JM, González-Pinto A. How effective is a psychological intervention program for patients with refractory bipolar disorder? A randomized controlled trial. J Affect Disord. 2010;126:80–7. doi: 10.1016/j.jad.2010.03.026. [DOI] [PubMed] [Google Scholar]
- 30.Chanpattana W, Kunigiri G, Kramer BA, Gangadhar BN. Survey of the practice of electroconvulsive therapy in teaching hospitals in India. J ECT. 2005;21:100–4. doi: 10.1097/01.yct.0000166634.73555.e6. [DOI] [PubMed] [Google Scholar]
- 31.Chanpattana W, Kramer BA, Kunigiri G, Gangadhar BN, Kitphati R, Andrade C. A survey of the practice of electroconvulsive therapy in Asia. J ECT. 2010;26:5–10. doi: 10.1097/YCT.0b013e3181a74368. [DOI] [PubMed] [Google Scholar]
- 32.Hiremani RM, Thirthalli J, Tharayil BS, Gangadhar BN. Double-blind randomized controlled study comparing short-term efficacy of bifrontal and bitemporal electroconvulsive therapy in acute mania. Bipolar Disord. 2008;10:701–7. doi: 10.1111/j.1399-5618.2008.00608.x. [DOI] [PubMed] [Google Scholar]
- 33.Mohan TS, Tharyan P, Alexander J, Raveendran NS. Effects of stimulus intensity on the efficacy and safety of twice-weekly, bilateral electroconvulsive therapy (ECT) combined with antipsychotics in acute mania: A randomised controlled trial. Bipolar Disord. 2009;11:126–34. doi: 10.1111/j.1399-5618.2009.00668.x. [DOI] [PubMed] [Google Scholar]
- 34.The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. 10th ed. Geneva: World Health Organization; 1992. World Health Organization. [Google Scholar]
- 35.Agarwal AK, Andrade C, Reddy MV. The practice of ECT in India I. Indian J Psychiatry. 1992;34:285–97. [PMC free article] [PubMed] [Google Scholar]
- 36.Chakrabarti S, Gill S. Coping and its correlates among caregivers of patients with bipolar disorder: A preliminary study. Bipolar Disord. 2002;4:50–60. doi: 10.1034/j.1399-5618.2002.01167.x. [DOI] [PubMed] [Google Scholar]
- 37.Pradhan BK, Chakrabarti S, Nehra R, Mankotia A. Cognitive functions in bipolar affective disorder and schizophrenia: Comparison. Psychiatry Clin Neurosci. 2008;62:515–25. doi: 10.1111/j.1440-1819.2008.01844.x. [DOI] [PubMed] [Google Scholar]
- 38.Nehra R, Chakrabarti S, Kulhara P, Sharma R. Caregiver-coping in bipolar disorder and schizophrenia: A re-examination. Soc Psychiatry Psychiatr Epidemiol. 2005;40:329–36. doi: 10.1007/s00127-005-0884-3. [DOI] [PubMed] [Google Scholar]
- 39.Ciapparelli A, Dell’Osso L, Tundo A, Pini S, Chiavacci MC, DiSacco I, et al. Electroconvulsive therapy in medication-nonresponsive patients with mixed mania and bipolar depression. J Clin Psychiatry. 2001;62:552–5. doi: 10.4088/jcp.v62n07a09. [DOI] [PubMed] [Google Scholar]
- 40.Macedo-Soares MB, Moreno RA, Rigonatti SP, Lafer B. Efficacy of electroconvulsive therapy in treatment-resistant bipolar disorder: A case series. J ECT. 2005;21:31–4. doi: 10.1097/01.yct.0000148621.88104.f1. [DOI] [PubMed] [Google Scholar]
- 41.Little JD. ECT in the Asia Pacific region: What do we know? J ECT. 2003;19:93–7. doi: 10.1097/00124509-200306000-00007. [DOI] [PubMed] [Google Scholar]
- 42.Odejide AO, Ohaeri JU, Ikuesan BA. Electroconvulsive therapy in Nigeria. Convuls Ther. 1987;3:31–9. [PubMed] [Google Scholar]
- 43.Grunze H. Reevaluating therapies for bipolar depression. J Clin Psychiatry. 2005;66:17–25. [PubMed] [Google Scholar]
- 44.Kellner CH, Fink M, Knapp R, Petrides G, Husain M, Rummans T, et al. Relief of expressed suicidal intent by ECT: A consortium for research in ECT study. Am J Psychiatry. 2005;162:977–82. doi: 10.1176/appi.ajp.162.5.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maletzky BM. The first-line use of electroconvulsive therapy in major affective disorders. J ECT. 2004;20:112–7. doi: 10.1097/00124509-200406000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Kho KH, Zwinderman AH, Blansjaar BA. Predictors for the efficacy of electroconvulsive therapy: Chart review of a naturalistic study. J Clin Psychiatry. 2005;66:894–9. doi: 10.4088/jcp.v66n0712. [DOI] [PubMed] [Google Scholar]
- 47.Jha AK, Stein GS, Fenwick P. Negative interaction between lithium and electroconvulsive therapy: A case-control study. Br J Psychiatry. 1996;168:241–3. doi: 10.1192/bjp.168.2.241. [DOI] [PubMed] [Google Scholar]


