Abstract
In the past, polypharmacy was referred to the mixing of many drugs in one prescription. Today polypharmacy implies to the prescription of too many medications for an individual patient, with an associated higher risk of adverse drug reactions (ADRs) and interactions. Situations certainly exist where the combination therapy or polytherapy is the used for single disease condition. Polypharmacy is a problem of substantial importance, in terms of both direct medication costs and indirect medication costs resulting from drug-related morbidity. Polypharmacy increases the risk of side effects and interactions. Moreover it is a preventable problem. A retrospective study was carried out at Bhopal district (Capital of Madhya Pradesh, India) in the year of September-November 2009 by collecting prescriptions of consultants at various levels of health care. The tendency of polypharmacy was studied and analyzed under the various heads in the survey. Available data suggests that polypharmacy is a widespread problem, and physician, clinical pharmacists and patients are all responsible. These risks can be minimized through identifying the prevalence of this potential problem in a high-risk population and by increasing awareness among patients and healthcare professionals. Physicians and clinical pharmacists have the potential to combating this problem through a variety of interventions such as reducing the number of medications taken, reducing the number of doses taken, increasing patient adherence, preventing ADRs, improving patient quality of life and decreasing facility and drug costs.
Keywords: Adverse drug reactions, clinical survey, inappropriate medication, polypharmacy, preventions
INTRODUCTION
Although the term polypharmacy has evolved over time and is often used to mean many different things in different situations, its basic definition is quite simple, more drugs are prescribed or taken than are clinically appropriate.[1] The specific number of drugs taken is not itself indicative of polypharmacy as all of the drugs may be clinically necessary and appropriate for the patient; however, as the number of prescribed drugs increases, so do the chances of Polypharmacy.[2] A 2002 US survey indicated that 25% of the overall population takes five or more medications per week.[3] When specifically considering the population 65 years of age and older, this percentage increases to about 50%, with 44% of men and 57% of women taking five or more medications per week and 12% of both sexes taking 10 or more prescriptions per week.[4] The most worrisome consequence of polypharmacy is the occurrence of adverse drug reactions (ADRs), but increased drug costs and patient quality of life are also significant issues.[5,6] The elderly population, which often suffers from multiple chronic diseases requiring multiple medications, continues to increase. These patients are much more likely to experience Polypharmacy and its negative consequences, especially ADRs.[7–11]
ADRs are one of the most troubling issues surrounding medication use in the elderly, as this patient population is more likely to have poor outcomes than others.[12] ADRs affect approximately 10-20% of hospitalized patients and around 7% of the general population; this number increases when the population of interest is limited to the elderly.[13,14]
Definitions of polypharmacy
The term polypharmacy refers to the group of medications one person may be taking. It comes from two Greek root words: poly, meaning many, and pharmakeia meaning medicines or drugs. It is generally used when that one person is taking too many medications, or when the drugs have been prescribed by many doctors, and may not have been coordinated well. The definition of polypharmacy is still controversial.[15–17] One simple definition is based on the total number of different medications a patient takes concurrently.[18] Topical and herbal medications are generally excluded of this definition as they are often not included in the traditional methods of assessing prescription quality.[19]
Considering the large number of polypharmacy concepts, there is need of an agreement in relation to this definition to evaluate its frequency, control its occurrence and to identify the risk of adverse reactions associated with polypharmacy.[20] There are several reasons for polypharmacy:
As the population ages, polypharmacy increases. The elderly often required multiple medications to treat multiple health-related conditions.[21]
Patient with multiple comorbid medical conditions also required numerous medications to treat each condition. It is not unreasonable for patient with multiple comorbid medical conditions to be on 6-9 medications to reduce his or her long-term risk for those conditions, i.e, diabetes conditions and coronary events.[22]
A recent hospitalization also puts patients at risk of polypharmacy. Medicines are started and stopped quite frequently during patient hospital stay.
Multiple doctors are prescribing medications for the same patient. Once a patient starts a medication, it is never discontinued.
Lack of patient education is the most common reason. Doctors do not inform patients or patients do not ask questions.
Polypharmacy is associated with suboptimal and inappropriate prescribing. Many medications that have an increased tendency to cause problems for older patients have been labeled as inappropriate drugs for this segment of the population. The simplest definition of an inappropriate drug is one that has greater potential to harm than to benefit the patient. It is difficult to state that any given drug should not be used in an elderly patient under any circumstances. High-risk medications do not cause problems in all elderly patients, but they do have an increased potential to cause problems.
Beers et al,[23] developed the following criteria for classifying a drug as inappropriate for use in elderly patients:
Specific medications or classes of medications that should not be used routinely in elderly persons. This may be due to lack of proven drug effect, a high likelihood of adverse drug effects, the potential for severe adverse effects, or a high potential for interaction with another drug or class of drugs.
Excessive dosages of medications used in elderly patients. Some medications for elderly patients are safe when used in lower doses but increase the risk of problems when used in higher doses.
Excessive dosing frequencies that would make compliance difficult for elderly patients. Because elderly patients tend to take multiple medications, it is best to prescribe medications that have once-daily dosing when possible.
Extended duration of use of medications that were intended to be used for a limited time. Some medications, prescribed initially for a limited time, become unnecessary and therefore inappropriate if taken for long term.
Polypharmacy may occur when additional drugs are prescribed to treat the adverse effects of other drugs. This is known as the ‘prescribing cascade’.[23,24] Other suboptimal prescribing associated with polypharmacy includes prescription of more than one drug in the same class or prescription of a drug that interacts with or is contraindicated in combination with another of the patient's medicines.[25]
Polypharmacy in of itself is not problematic. Consider, for instance, a patient with type 2 diabetes and existing coronary heart disease who has received a resent coronary sent for myocardial infarction. It is not unreasonable or uncommon for this patient to be on 6-9 medications to reduce his or her long-term risk for diabetes complications and secondary coronary events.[26–28]
Polypharmacy can, however, become problematic when negative outcomes occur. Polypharmacy has been shown to result in:
Unnecessary and/or inappropriate medication prescribing.
Increased risk for drug interactions and ADRs.[29]
Nonadherence.
Increased overall drug expenditures.
Polypharmacy is sometimes overlooked because the symptoms it causes can be confused with symptoms of normal aging or another disease. Sometime resulting in still more drugs being prescribed to tract the new symptoms. Some signs that are caused by interactions between drugs or side-effects of drugs can include:[30,31]
Tiredness, sleepiness or decreased alertness
Constipation, diarrhea or incontinence
Loss of appetite
Confusion (all time or some time)
Falls
Depression or lack of interest in usual activities
Weakness
Tremor
Hallucinations - Seeing or hearing things
Anxiety or excitability
Feeling dizzy
Decreased sexual behavior
Skin rashes
METHODOLOGY
A retrospective study was carried out in Bhopal district by collecting prescriptions of consultants at various levels of health care. Patients attending the clinics of consultants were approached at pharmacy shops and requested to show their prescriptions and by taking prior consent of the patients prescriptions were copied. This was a descriptive study that involved the administration of a bilingual (English/Hindi) questionnaire.
The bilingual questionnaire was specifically designed for this project in order to assessing polypharmacy among patients in the Bhopal region. Prior to use, the questionnaire was reviewed by a consultant with expertise in development of survey instruments. Information collected by the questionnaire included the following:
-
Patient's demography information
Name of the patient, age, sex
Name of physician, qualifications and specialization of physician.
Date of prescription
-
Current medical conditions
Medical history of patient
Signs and symptoms
Current prescription medications (drug, dose, frequency, indication)
Current drug products or nutritional supplements
Dosage regimen
Questionnaires were completed through semi-structured interviews with patients at their respective health care centers and medical shops. Patients agreeing to participate in the study were asked to bring to the interview a list of all medications, or nutritional supplements that they were currently taking. They were also allowed to bring in the actual products if no list was available. Administration of the questionnaire was performed with the assistance of bilingual interviewers (B. Pharm students).
RESULT AND DISCUSSION
Based on the information obtained from the questionnaire, the tendency of polypharmacy was studied and analyzed under the following heads in the survey:
Over prescribing, unnecessary use of drugs (to prescribe excessive or unnecessary medication that is not beneficial for patients).
Repetitive drugs (drug prescribed in same prescription leading to the duplication), inappropriate drug combinations (medication is one that has greater potential to harm than to benefit the patient. or does not agree with accepted medical standards).
Drug-drug interactions (the action of one drug upon the effectiveness of another), food-drug interaction [Table 1 and Figure 1].
Table 1.
Data analysis and results
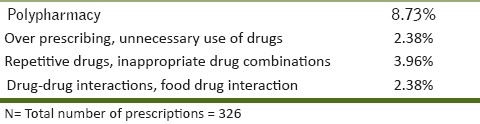
Figure 1.
Graph showing data analysis and result of survey
Over prescribing, unnecessary use of drugs
Of all prescriptions 2.38% (N=326) showed over prescribing. There was unnecessary (60%) use of tonics for the patients, multivitamin and tonics formed an integral part of all most all the prescriptions.
Metronidazole + Albendazole + Mebendazole were prescribed together for diarrhea infection indicating the misuse of antiamoebics.
Cotrimoxazole + Chloramphenicol + Ampicillin + Furoxone were prescribed for case of typhoid fever. Such multitherapy has resulted in the emergence of Salmonella typhi-resistant to many drugs in a number of Indian cities.
Most cases of common cold are self-limiting and need management with symptomatic therapy. There is no therapeutic utility of routine administration of antibiotics because common cold is caused by virus. The antibiotics erythromycin and amoxicillin may be administered only if there is occurrence of fever.
Repetitive drugs, inappropriate drug combinations
Of all the prescriptions 3.96% (N=326) of the prescriptions showed repetition. One of the striking features of the study was the duplication of drugs in the prescription, which lead to inadequate dosage or quantities of drugs prescribed.
Anti-inflammatory drugs were repeated in the prescription e.g., Acetaminophen + Chlorpheriramine + pseudoephedrine combination was prescribed twice as sinarest and rhinoset thrice a day for 3 days.
In the study carried, it was observed that two to three multivitamin preparations were prescribed in same prescription leading to the duplication.
It indicates adoption of polypharmacy promoting unnecessary use of tonics, overlooking drug interaction and increasing the cost of therapy and occurrence of side effects. In case of respiratory disorders there is an excessive use of cough mixtures which add to the cost of therapy.
Repetitive use of anti-allergic drugs was encountered in prescription of respiratory disorders e.g., Betamethasone was prescribed twice in the same prescription in case of respiratory infections.
A preparation containing Bromhexine + Dextromethorphan was prescribed for the same patient leading to over dosage of Bromhexine.
Drug-drug interactions, food drug interaction
Of all the prescriptions 2.39% (N=326) of the prescription showed drug-drug interactions.
Iron salts were prescribed with norfloxacin irrespective of the fact that iron salt decreases the absorption of norfloxacin.
Levofloxacin and Gatifloxacin were prescribed with NSAIDS like Paracetamol and Nimesulide without any notification to take precautionary measure against convulsive seizures.
Multivitamin preparation containing Iron may decrease the absorption of levofloxacin when coadministered.
Approaches to reducing polypharmacy
Maintain an accurate medication and medical history: Identify all medications, including any over the counter (OTC) therapies. Having a complete list of medications can deter a provider from adding on an additional therapy. Further, knowledge of a specific medication being used may explain a patient-specific symptom or complaint. For example, knowing a patient is on an opiod analgesic may explain why he or she has constipation. A complete history of the patient's medical condition also is important. Identifying the patient medical history allows the pharmacist to identify inappropriately prescribed medications. For instance, metformin is not appropriate for patients with end-stage kidney disease.
Link each prescribed medication to a disease state: Each medication should match a patient's diagnosis. Any medication that does not match a diagnosis is potentially unnecessary, and an attempt to discontinue the medication should be made.
Identify medications that are treating side effects: The use of multiple medications leads to a higher risk of side effects. When side effects occur, additional medications can be initiated to treat the side effect. A common example includes the use of laxatives to treat the medication side effect of constipation. Other examples include, Aricept (donepezil) to treat cognitive impairment caused by obybutynin, tolterodine, antihistamines, opiods and benzodiazepines. Discontinuing one drug that is causing a side effect can often lead to the discontinuation of several drugs.
Reconcile medications upon discharge from hospital or skilled nursing facility: As mentioned above, a risk factor for polypharmacy includes recent hospitalization. The transfer of a patient from a hospital to his or her home is associated with adverse events and negative outcomes, most of which are related to changes in the patients drug therapy during treatment in these facilities. Evaluating a patients medications regimen and educating a patient upon discharge from a facility is likely to reduce duplicate therapy, inappropriate prescribing, and reduce unnecessary medication.
Taking preventions during prescription: The appropriateness of the medication for the patient and the potential for side effects must be considered. Any drug that is unnecessary, inappropriate, or has a high likelihood for causing side effects that would require additional therapy should be avoided.
CONCLUSIONS
The prevalence of polypharmacy among patients in the Bhopal region taking inappropriate prescription medications is 8.73% (N=29).
Of all prescriptions 2.38% (N=326) showed over prescribing drugs, 3.96% (N=326) showed repetition of drugs, 2.39% (N=326) showed drug-drug interactions.
Polypharmacy is a widespread problem, and physician, clinical pharmacists, and patients are all responsible. Physicians are more ignorant to pharmacological interactions of the drugs rather indulged in the malpractices. Therefore, more number of orientation programs, continuing medical educations, etc. should be attended by the medical practitioners as a routine practice. Physicians need to be aware of the frequency of dosing and the total number of medications a patient has to take, and their bearing on compliance. Attention has to be given to the mechanism of action of the drugs, to avoid prescribing drugs with duplicate actions.
Patients may contribute to the problem by self-medicating, failing to follow prescribed directions, failing to report all medications or OTC products used, and borrowing or trading medication with other persons. Awareness of other therapies to which the patient subscribes is also essential. It is important to remember that the consequences of inappropriate polypharmacy can be particularly significant to an elderly patient's well-being, financial security and ability to adhere to prescribed therapy.
A statement of polypharmacy is needed at this time in order to:
Promote periodic evaluation of drugs for efficacy
Reduce ADRs
Heighten awareness of health professionals regarding principles of geriatric prescription.
Prevention of unnecessary drug therapy problem can be conducted through reduction of drug use. It is recommended to eliminate all medications without therapeutic benefit, goal or indication.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Zarowitz BJ, Stebelsky LA, Muma BK, Romain TM, Peterson EL. Reduction of high-risk polypharmacy drug combinations in patients in a managed care setting. Pharmacotherapy. 2005;25:636–45. doi: 10.1592/phco.2005.25.11.1636. [DOI] [PubMed] [Google Scholar]
- 2.Goh CR. Minimising Polypharmacy - a challenge in palliative care. Singapore Med J. 2002;43:273–5. [PubMed] [Google Scholar]
- 3.Nisly NL, Gryzlak BM, Zimmerman MB, Wallace RB. Dietary Supplement Polypharmacy: An Unrecognized Public Health Problem? Evid Based Complement Alternat Med. 2010;7:107–13. doi: 10.1093/ecam/nem150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States.The Slone Survey. JAMA. 2002;287:337–44. doi: 10.1001/jama.287.3.337. [DOI] [PubMed] [Google Scholar]
- 5.Nolan L, O’Malley K. Prescribing for the elderly: Part 1.Sensitivity of the elderly to adverse drug reactions. J Am Geriatr Soc. 1998;36:142–9. doi: 10.1111/j.1532-5415.1988.tb01785.x. [DOI] [PubMed] [Google Scholar]
- 6.Lamy PP. adverse drug effects. Clin Geriatr Med. 1990;6:293–307. [PubMed] [Google Scholar]
- 7.Montamat SC, Cusack B. Overcoming problems with polypharmacy and drug misuse in the elderly. Clin Geriatr Med. 1992;8:143–58. [PubMed] [Google Scholar]
- 8.Williams P, Rush DR. Geriatric polypharmacy. Hosp Pract. 1986;21:9–20. doi: 10.1080/21548331.1986.11706572. [DOI] [PubMed] [Google Scholar]
- 9.Roenke KL, Pinholt EM. Reducing polypharmacy in the elderly. J Am Geriatr Soc. 1990;38:31–6. doi: 10.1111/j.1532-5415.1990.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 10.Kroenke KL. Polypharmacy. Am J Med. 1985;79:149–52. doi: 10.1016/0002-9343(85)90001-4. [DOI] [PubMed] [Google Scholar]
- 11.Stewart RB, Cooper JW. Polypharmacy in the aged. Practical solutions. Drugs Aging. 1994;4:449–61. doi: 10.2165/00002512-199404060-00002. [DOI] [PubMed] [Google Scholar]
- 12.Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–16. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]
- 13.Gomez ER, Demoly P. Epidemiology of hypersensitivity drug reactions. Curr Opin Allergy Clin Immunol. 2005;5:309–16. doi: 10.1097/01.all.0000173785.81024.33. [DOI] [PubMed] [Google Scholar]
- 14.Chumney EC, Robinson LC. The effects of pharmacist interventions on patients with polypharmacy. Pharm Pract. 2006;4:103–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Aminzadeh F, Dalziel WB. Older adults in the emergency department: A systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39:238–47. doi: 10.1067/mem.2002.121523. [DOI] [PubMed] [Google Scholar]
- 16.Carlson JE. Perils of polypharmacy: 10 steps to prudent prescribing. Geriatrics. 1996;51:26–35. Hanlon JT. Drug-related problems update. Am J Geriatr Pharmacother 2004;2:88-90. [PubMed] [Google Scholar]
- 17.Steinman MA, Rosenthal GE, Landefeld CS, Bertenthal D, Sen S, Kaboli PJ. Conflicts and concordance between measures of medication prescribing quality. Med Care. 2007;45:95–9. doi: 10.1097/01.mlr.0000241111.11991.62. [DOI] [PubMed] [Google Scholar]
- 18.Veehof L, Stewart R, Haaijer-Ruskamp F, Jong BM. The development of polypharmacy. A Longitudinal study. Fam Pract. 2000;17:261–7. doi: 10.1093/fampra/17.3.261. [DOI] [PubMed] [Google Scholar]
- 19.Schaefer K, Maerkedahl H, Birk HO, Henriksen LO. Polypharmacy in general practice. Dan Med Bull. 2010;57:A4165. [PubMed] [Google Scholar]
- 20.Gallagher P, Barry P, O’Mahony Review Article Inappropriate prescribing in the elderly. J Clin Pharm Ther. 2007;27:113–21. doi: 10.1111/j.1365-2710.2007.00793.x. [DOI] [PubMed] [Google Scholar]
- 21.Wilcox SM, Himmelstein DU, Wollhander S. Inappropriate drug prescribing for the community-dwelling elderly. JAMA. 1994;272:292–6. [PubMed] [Google Scholar]
- 22.Rozenfeld S, Fonseca MJ, Acurcio FA. Drug utilization and polypharmacy among the elderly: A survey in Rio de Janeiro City, Brazil. Rev Panam Salud Publica. 2008;23:34–43. doi: 10.1590/s1020-49892008000100005. [DOI] [PubMed] [Google Scholar]
- 23.Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. Arch Intern Med. 1991;151:1825–32. [PubMed] [Google Scholar]
- 24.Hawkins C, Hanks GW. The gastroduodenal toxicity of nonsteroidal anti-inflammatory drugs.A review of the literature. J Pain Symptom Manage. 2000;20:140–51. doi: 10.1016/s0885-3924(00)00175-5. [DOI] [PubMed] [Google Scholar]
- 25.Ahmad A, Hugtenburg J, Welschen LM, Dekker JM, Nijpels G. Effect of medication review and cognitive behavior treatment by community pharmacists of patients discharged from the hospital on drug related problems and compliance: Design of a randomized controlled trial. BMC Public Health. 2010;10:133. doi: 10.1186/1471-2458-10-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent Patterns of Medication Use in the Ambulatory Adult Population of the United States: The Slone Survey. JAMA. 2002;287:337–44. doi: 10.1001/jama.287.3.337. [DOI] [PubMed] [Google Scholar]
- 27.Hilmer Sarah N. The dilemma of polypharmacy. Aust Prescr. 2008;31:2–3. [Google Scholar]
- 28.Dutch Working party on infection prevention (WIP): guideline for primary care. [Last accessed on 2009 May 6]. available from: http://www.wip.nl/free_content/Richtlijnen/1Huisartsen.pdf .
- 29.Pau AK. Polypharmacy problem: Drug interactions in the multidrug therapy of HIV infection, Publish in New York City by The Physician's Research Network, Inc. 2002;7:4–9. Available online www.PRN.org . [Google Scholar]
- 30.Lin P. The Canadian Alzheimer Disease Review. 2003 Sep;:10–14. [Google Scholar]
- 31.Bista D, Palaian S, Shankar PR, Prabhu MM, Paudel R, Mishra P. Understanding the essentials of drug interactions: A potential need for safe and effective use of drugs. Kathmandu Univ Med J (KUMJ) 2006;4:421–30. [PubMed] [Google Scholar]


