Abstract
Hair dye poisoning is not rare but is an emerging poisoning in India. The main component of hair dye causing toxicity is paraphenylenediamine (PPD). Acute poisoning by PPD causes characteristic severe angioedema of the upper airway accompanied by a swollen, dry, hard, and protruding tongue. Systemic intoxication results in multisystem involvement and can cause rhabdomyolysis, acute renal failure (ARF). PPD consumption is an uncommon cause of ARF. There is no specific antidote for PPD and treatment is mainly supportive. We report a case of suicidal ingestion of hair dye that presented with cervicofascial edema and later developed rhabdomyolysis and ARF. Our patient improved with dialysis and symptomatic management.
Keywords: Acute renal failure, hair dye, paraphenylenediamine, rhabdomyolysis
INTRODUCTION
Super Vasmol 33™ is an emulsion based hair dye commonly used in India. The main ingredients of the dye are paraphenylene diamine, resorcinol, propylene glycol, sodium ethylene diamine tetra acetic acid (EDTA), preservatives, and perfumes. The main compound responsible for the toxicity is paraphenylenediamine (PPD).[1] Common clinical manifestations of PPD are cervicofacial edema, chocolate brown colored urine, oliguria, muscular edema, and shock.[1] Hypocalcaemia may occur in the setting of severe rhabdomyolysis[2] or due to sodium EDTA. Patients can develop seizures, which may be due to toxins in dye or as a result of hypocalcaemia. Treatment in mainly supportive as there is no specific antidote for PPD.
CASE REPORT
A 23-year-old married female presented with history of suicidal consumption of hair dye (Super Vasomol 33™) approximately about 60 ml one day prior to our emergency medical services department. She had facial swelling with edema of lips, stridor, and difficulty in breathing. There was no history of dark colored urine or decreased urine output at presentation. Clinical examination revealed facial swelling with edematous lips, swollen neck, and tongue. The pulse rate was 100/min, blood pressure was 110/80 mmHg, and SpO2 was 98% with oxygen by mask. The cardiovascular system and respiratory system examinations were normal. On day 2 of hospital admission, the patient developed dark colored urine with a decreased urine output and pedal edema. The laboratory investigations revealed blood urea of 180 mg/dl and creatinine of 5.6 mg/dl [Table 1]. The serum creatine phosphokinase (CPK) levels were 1750 U/L, serum calcium 10 mg/dl, and urine myoglobin was positive. The liver function tests were normal and peripheral smear did not reveal evidence of hemolysis. The chest x-ray and electrocardiogram were normal.
Table 1.
Renal function tests and other investigations
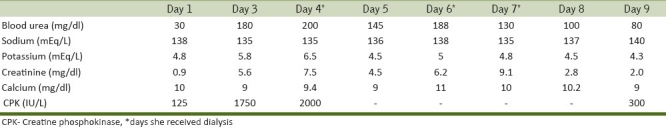
The patient was treated with injection hydrocortisone and antihistamines in view of stridor and respiratory distress, which resolved after 2 days of treatment. On day 3 of poisoning (second hospital admission day), she developed rhabdomyolysis and ARF. Her blood urea, creatinine levels were elevated [Table 1] and arterial blood gas analysis showed severe metabolic acidosis. She was managed initially with forced alkaline diuresis and in view of severe metabolic acidosis and hyperkalemia she received three sittings of hemodialysis. Acute renal failure (ARF) resolved over 6 days with dialysis and patient was discharged on day 9 of hospital admission.
DISCUSSION
The toxicity of PPD was first described in a hairdresser in 1924 following exposure due to occupational handling.[3] PPD is a key ingredient of hair dyes, used for color enhancement. It is widely used in industrial products such as textile or fur dyes, dark colored cosmetics, temporary tattoos, photographic development, and gasoline. PPD is commonly used in its raw form for cosmetic purposes in Africa, Middle East, and Indian subcontinent. PPD is also a well-known skin irritant and may be absorbed from the skin.
The PPD is an aromatic amine not found in nature and many industrial companies produce it commercially. The extent of renal involvement in poisoning varies between transient proteinuria and oliguric acute kidney injury (AKI). AKI commonly develops a few days after PPD exposure. The mechanisms of kidney injury following hair dye poisoning are many. The PPD itself has a direct toxic effect on kidney due to its aromatic structure, which makes its easy reabsorption and concentration in tubule and can cause ARF.[4] It can cause rhabdomyolysis with the deposition of myoglobin cast within the renal tubules and hemolysis with resultant hemoglobinuria causing acute tubular necrosis and ARF.[5] The propylene glycol, an ingredient of hair dye, is potentially nephrotoxic and may result in a high anion gap metabolic acidosis and ARF.[6] The hypovolemia in addition can complicate renal failure. In our case acute renal failure is mainly due to rhabdomyolysis and myoglobinuria. The development of ARF in PPD intoxication does not occur in all patients and varies from 47.3% to 100%.[7]
The treatment is mainly supportive and depends on clinical presentation. Antihistamines and steroids are commonly used in the management of airway edema because of the possibility of a hypersensitivity reaction to PPD but there is no evidence to support this mode of treatment.[8] Alkaline diuresis using isotonic saline, sodium bicarbonate, and diuretics are used in the management of myoglobinuria. There is no specific antidote for PPD, and trials of PPD removal using hemoperfusion and hemodialysis had variable results. The toxin is not dialyzable[9] and dialysis in only supportive therapy.
Our patient presented with angioedema of upper airway and on day 3 of poisoning developed rhabdomyolysis and acute renal failure with severe metabolic acidosis. She received treatment with hydrocortisone, antihistamines for cervicofacial and laryngeal edema. The acute renal failure was managed with forced alkaline diuresis and hemodialysis. The patient responded well to treatment and was discharged on day 9 of hospital admission.
In conclusion, early diagnosis of rhabdomyolysis and acute renal failure with institution of appropriate supportive management will have a better outcome in hair dye poisoning. And also the time of development of renal failure following PPD intoxication is uncertain and hence all patients should be monitored in hospital for development of renal complications.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Bhargava P, Matthew P. Hair dye poisoning. J Assoc Physicians India. 2007;55:871–2. [PubMed] [Google Scholar]
- 2.Huerta-Alardin AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis – An overview for clinicians. Crit Care. 2005;9:158–69. doi: 10.1186/cc2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Filali A, Semlali I, Ottaviano V, Furnari C, Corradini D, Soulaymani R. A retrospective study of acute systemic poisoning of paraphenylenediamine (occidental takawt in Morocco) Afr J Tradit Complement Altern Med. 2006;39:142–9. [Google Scholar]
- 4.El-Ansary EH, Ahmed ME, Clague HW. Systemic toxicity of paraphenylene diamine. Lancet. 1983;1:1341. doi: 10.1016/s0140-6736(83)92456-x. [DOI] [PubMed] [Google Scholar]
- 5.Hamdouk M. PPD Nephrotoxicity: [Sheffield] Sheffield Kidney Institute; 2001. Paraphenylenediamine (Hair Dye) Acute Systemic toxicity; pp. 34–47. [Google Scholar]
- 6.Sampathkumar K, Yesudas S. Hair dye poisoning and the developing world. J Emerg Trauma Shock. 2009;2:129–31. doi: 10.4103/0974-2700.50749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sahay M, Vani R, Vali S. Hair dye ingestion – An uncommon cause of acute kidney injury. J Assoc Physicians India. 2009;57:743–4. [PubMed] [Google Scholar]
- 8.Abdelraheem M, Hamdouk M, Zijlstra E. Paraphenylene diamine (Hair Dye) poisoning in children. Arab J Nephrol Transplant. 2010;3:39–43. [Google Scholar]
- 9.Singla S, Miglani S, Lal AK, Gupta P, Agarwal AK. Paraphenylenediamine (PPD) poisoning. J Acad Clin Care Med. 2005;6:236–8. [Google Scholar]


