Abstract
Background
Chitotriosidase is an accepted marker of macrophage activation. In this study, we investigated serum chitotriosidase levels in pulmonary tuberculosis (PTB).
Methods
Forth-two patients with PTB and 30 healthy subjects were enrolled in the study. The radiological extent of PTB, radiological sequela after treatment, and the degree of smear positivity were assessed. Chitotriosidase levels were measured by a fluorometric method.
Results
The serum chitotriosidase levels of the PTB patients were significantly higher than those of the control subjects (39.73±24.97 vs. 9.63±4.55 nmol/mL/h, P<0.001). After completion of the standard 6-month antituberculous treatment, chitotriosidase levels in PTB patients significantly decreased (10.47±4.54 nmol/mL/h, P<0.001). Chitotriosidase levels correlated significantly with the radiological extent of PTB, degree of smear positivity, and post-treatment radiological sequela score (r=0.439, r=0.449, and r=0.337, respectively).
Conclusions
This study demonstrated that serum chitotriosidase levels increase in PTB; therefore, chitotriosidase can be used as a marker of disease activity, severity, and response to treatment.
Keywords: Chitotriosidase, Tuberculosis, Lung
INTRODUCTION
Chitotriosidase (CHT), a member of the chitinase enzyme family, is a glycopolymer found in many living organisms such as fungi, nematodes, and insects. Although no CHT activity in human metabolism has been documented, CHT has been suggested to play a role in innate immunity and is considered to be a useful marker of macrophage activation [1]. In recent years, the clinical relevance of CHT levels in various diseases has been widely investigated. In particular, CHT was identified as a potential marker of disease activity and as a valuable tool to monitor efficacy of treatment in Gaucher's disease [2, 3]. The clinical importance of CHT was first reported in Gaucher's disease and other lysosomal storage disorders such as fucosidosis and galactosialidosis [3, 4]. In addition, CHT levels were increased in the sera of patients with sarcoidosis, atherosclerosis, acute Plasmodium falciparum malaria, visceral leishmaniasis, β-thalassemia, steatohepatitis, neurodegenerative disorders (including Alzheimer's disease and cerebrovascular dementia), and in the cerebrospinal fluid of multiple sclerosis patients [2, 4-9].
The studies regarding CHT on sarcoidosis revealed that it might be involved in the pathogenesis and could be a diagnostic tool or activity marker for the disease [5, 10-12]. Similar to sarcoidosis, tuberculosis (TB) is also a granulomatous disease that mainly affects the lungs. Activated macrophages play a significant role in the immunopathogenesis of both sarcoidosis and TB. Bacteriological confirmation by sputum smear and culture is essential for the diagnosis of pulmonary tuberculosis (PTB). However, the sensitivity of sputum smears is low, and the prevalence of smear-negative active PTB has been increasing among patients co-infected with HIV. Thus, new efforts have been made to evaluate disease activity with biochemical markers while waiting for conventional culture results to be obtained [13-15].
Currently available information on CHT activity in PTB is limited and has been obtained from studies involving small study populations [11, 16]. We aimed to investigate serum CHT activity in PTB, its alteration in response to treatment, and its relationship with microbiological and radiological parameters.
METHODS
1. Study population
The study was conducted in Department of Pulmonary Medicine of Gulhane Military Medical Academy, in Ankara, Turkey. The study population consisted of patients with PTB. A total of 54 patients with PTB were evaluated. Patients with extrapulmonary involvement of TB, any other associated pulmonary or extrapulmonary diseases and those with active PTB without culture positivity were excluded. Finally, we enrolled 42 patients with PTB as the study group and 30 healthy subjects as the control group in the study. Chest x-ray radiography, routine biochemical analyses (including complete blood count), and erythrocyte sedimentation rate analyses were performed for both the groups. The study was approved by the local ethics committee, and informed consent was obtained from all subjects.
2. Chitotriosidase activity
Blood samples (5 mL) were obtained by venipuncture in an EDTA-containing tube. Plasma and packed cells were separated by centrifugation at 1,500×g for 10 min and stored at -80℃ until they were processed. CHT activity was measured as previously described by Hollak et al. [3]. Briefly, 5 µL of plasma was incubated with 100 µL of 22 µmol/L 4-methylumbelliferryl-β-D-N-N'-N"-triacetylchitotriosidase (Sigma M-5639; Sigma-Aldrich ChemieGmBH, Taufkirchen, Germany) in McIlvain's phosphate-citrate buffer; pH=5.2, for 1 hr at 37.0℃ in darkness. The reaction was terminated by the addition of 120 µL 0.5 mol/L Na2CO3-NaHCO3 buffer (pH=10.7). In the quantitative method, the fluorescence of 4-methylumbelliferone was measured in a Microfluor 2 plate by a fluorometer (BIO-TEK SynergyHT; Biotek Instruments Inc., Winooski, VT, USA) at excitation and emission wavelengths of 360 nm and 450 nm, respectively. CHT activity was expressed as nanomoles of substrate hydrolyzed per milliliter per hour (nmol/mL/h).
3. Microbiological examination
Three sputum samples were collected from all patients, who were able to expectorate spontaneously, on 3 consecutive days. Sputum smears for acid-fast bacilli (AFB) were prepared and stained according to the Ziehl-Neelsen method [15]. M. tuberculosis cultures were carried out using Lowenstein-Jensen media (Salubris Inc., Istanbul, Turkey) and a radiometric BACTEC TB 460 system (Becton Dickinson, Sparks, MD, USA). When sputum smears were negative or insufficient, bronchoalveolar lavage via fiber optic bronchoscopy was performed for smear preparation and M. tuberculosis cultures. Diagnosis of active PTB was confirmed by a positive M. tuberculosis culture. The severity of the sputum smears was graded as follows:
Score 0: no AFB (i.e. smear negative),
Score 1: less than 10 AFB per 100 fields,
Score 2: 10-99 AFB per 100 fields,
Score 3: 1-9 AFB per field, and
Score 4: 10 or more AFB per field.
4. Radiological extent of active and sequela TB
The radiological extent of active TB was determined separately and blindly by 2 chest physicians (S.G. and E.T.). In cases of disagreement between the physicians, the final decision was made by a consensus of them after evaluating the chest x rays together. A modified form of a previously described scoring system was used [17, 18]. Briefly, in every chest x-ray radiograph, each lung was divided into 3 zones: the upper zone was above the level of the second rib at the costosternal junction, the middle zone was between the levels of the second and fourth ribs at the costosternal junction, and the lower zone was below the middle zone. A chest x-ray score was determined by visually estimating the extent of the opacities attributable to PTB (nodular infiltration, consolidation, atelectasis, linear densities, etc.) and separately evaluating the existence of cavitation. The score was based on the percentage of opacities in each lung zone and the total diameter of the cavities, by the following system:
Score 1: involvement of less than 25% of a lung zone without any demonstrable cavitation,
Score 2: involvement of between 25-50% of a lung zone without any demonstrable cavitation, or involvement of less than 25% of a lung zone and a total cavity diameter <2 cm,
Score 3: involvement of between 50-75% of a lung zone without any demonstrable cavitation, or involvement of less than 50% of a lung zone and a total cavity diameter between 2-4 cm,
Score 4: involvement of more than 75% of a lung zone, or any cavitary disease with a total cavity diameter >4 cm. The scores of the 6 zones were summed, with 24 as the worst possible score.
The radiological extent of the TB sequela after treatment was assessed by the following scoring system:
0 point: no sequel;
1 point (mild): involving less than 1/4 of a lung zone or tuberculomas smaller than 1 cm,
2 points (moderate): involving between 1/4 and a whole lung zone or tuberculomas between 1 and 3 cm,
3 points (severe): involving more than 1 lung zone, tuberculomas greater than 3 cm, cavitary sequel independent from the diameter, or radiological findings of restriction or lung volume loss.
5. Statistical analysis
The SSPS software was used for statistical analysis. Descriptive statistics are shown as mean±standard deviation. Mean CHT levels between the groups and those of pre- and post-treatment periods were compared by t-test. Correlations between CHT, the radiological extent of active PTB, sequela of PTB, and degree of the sputum smears were calculated by means of the Spearman rank correlation test. The correlation coefficient was symbolized by "r," and P value less than 0.05 was considered significant.
RESULTS
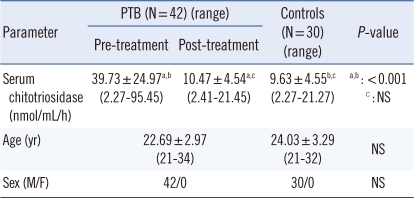
Demographic characteristics and mean CHT levels were given in Table 1. The mean ages of the groups were not significantly different. Since the study was conducted in a military hospital, all subjects in both the groups were men. Serum CHT levels were significantly higher in the PTB group (39.73±24.97 nmol/mL/h) than those in control subjects (9.63±4.55, nmol/mL/h, P<0.001). After 6-month antituberculous treatment, CHT levels significantly decreased to levels near those of healthy controls (10.47±4.54 nmol/mL/h, P<0.001; Table 1 and Fig. 1). Post-treatment CHT levels of PTB patients did not differ significantly from those of controls (P =0.441).
Table 1.
Serum chitotriosidase levels in pulmonary tuberculosis (PTB) patients and healthy controls
Abbreviations: PTB, pulmonary tuberculosis; NS, not significant.
Fig. 1.
Serum chitotriosidase levels in control subjects and pulmonary tuberculosis (PTB) patients before and after treatment.
Abbreviation: TB, tuberculosis.
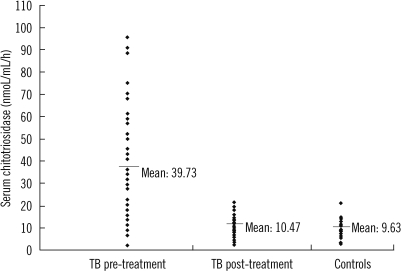
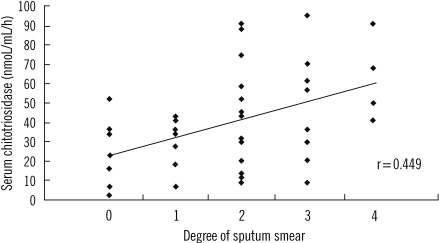
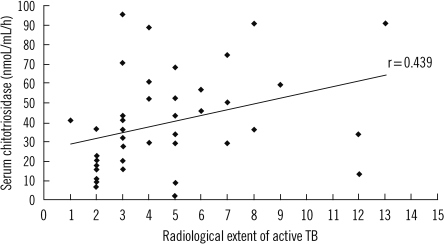
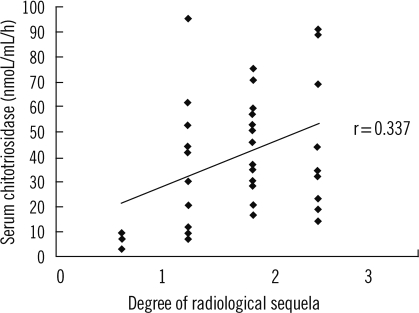
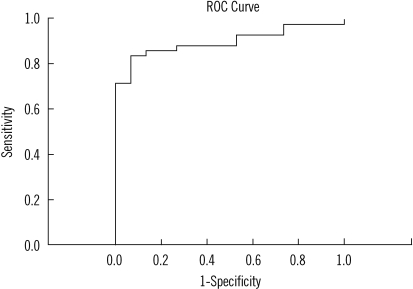
Serum CHT levels showed moderately significant correlations with the microbiological and radiological scores of active PTB patients (r=0.449, P=0.003 and r=0.439, P=0.004, respectively; Figs. 2 and 3), whereas CHT levels showed a weak correlation with radiological sequela scores at the end of the treatment (r=0.337, P=0.029; Fig. 4). The correlations between CHT and other biochemical parameters were not significant. The discriminative diagnostic parameters between PTB patients and healthy subjects were calculated by using ROC curve analysis (Fig. 5). Area under curve (AUC) in ROC analysis describes discriminative diagnostic power of the test that means the closer to 1 is the more powerful test and it was 0.898 in the current study. At the cut-off level of 15.45 nmol/mL/h for distinguishing active PTB patients from healthy subjects, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated as 83.3%, 93.3%, 94.6%, and 80%, respectively.
Fig. 2.
Correlation between serum chitotriosidase level and the degree of sputum smear for acid-fast bacilli (AFB).
Fig. 3.
Correlation between serum chitotriosidase level and radiological extent of active tuberculosis (TB).
Fig. 4.
Correlation between serum chitotriosidase level and the degree of post-treatment radiological sequela score after antituberculous treatment.
Fig. 5.
ROC analysis to distinguish active pulmonary tuberculosis (PTB) patients from healthy subjects. Area under curve: 0.898.
DISCUSSION
In this study, we showed that compared to healthy individuals, patients with PTB had elevated serum CHT levels. Of note, the elevated CHT levels returned to normal after completion of the standard 6-month antituberculous treatment. Moreover, serum CHT levels were positively correlated with the microbiological and radiological scores of active TB, suggesting that the higher the bacillus load and the worse the radiologically extended disease, the higher the serum CHT levels. However, the correlation coefficients between CHT levels, and radiological and microbiological scores were in moderate degree, and these data need to be confirmed by studies on large populations. On the other hand, a statistically significant, but weak, correlation was observed between CHT levels and radiological sequela after treatment in patients with PTB. Our main aim was to investigate the potential of serum CHT as a marker of disease activity (not a diagnostic tool) in PTB, and ROC analysis revealed that CHT was a good activity marker in PTB. A cut-off level of 15.45 nmol/mL/h can be used to determine the activity of PTB, at which the PPV and NPV were calculated as 94.6% and 80%, respectively.
TB is a granulomatous disease caused by M. tuberculosis complex in which the innate immune response is regulated by natural killer cells, T lymphocytes, macrophages, interferon-γ, and other type-1 cytokines [19]. Activated macrophages play a major role in the formation of tuberculous granulomas. Therefore, the elevated CHT levels in PTB, and its correlation with radiological extent and degree of bacillus load suggests that CHT might have a role in the immunopathogenesis of TB.
Although its physiological role in the human organism is not completely understood, CHT is widely accepted as a marker of activated macrophages and is thought to participate in innate immunity, particularly in defense mechanisms against chitin-containing pathogens. It is mainly excreted by macrophages and polymorphonuclear neutrophils under specific stimuli. Van Eijk et al. demonstrated that granulocyte macrophage-colony stimulating factor stimulates the synthesis of CHT in macrophages and promotes exocytosis of specific CHT-containing granules from polymorphonuclear neutrophils [20]. The same study revealed that CHT inhibits the growth of Candida neoformans in vitro and recombinant human CHT improves survival in neutropenic mouse models with systemic candidiasis and aspergillosis in vivo. In support of these data, neonates with systemic candidiasis have been reported to have elevated plasma CHT levels, and genetic variations in CHT alleles result in increased susceptibility to Gram-negative bacterial infection in children undergoing therapy for acute myeloid leukemia [21, 22]. Another study revealed that Wuchereria bancrofti infection, which causes filariasis, is associated with an increased frequency of CHT deficiency [23]. In a recent study supporting the idea that CHT is involved in innate immunity, Malaguarnera et al. demonstrated that interferon-γ, tumor necrosis factor-α, and lipopolysaccharide promoted CHT gene expression in human macrophages [24]. According to a recent report, serum CHT activity was elevated in Crimean-Congo hemorrhagic fever, and decreased serum CHT activity might be associated with increased mortality [25].
Little data on CHT activity and active TB is available in the current literature [11, 16]. Bargagli et al. demonstrated that serum CHT activity in 15 patients with PTB was almost 2 times higher than that of 30 healthy subjects (20.53±4.125 vs. 10.39±0.5184 nmol/mL/h), although these differences were not statistically significant [11]. However, as stated in their study, the number of patients with PTB was low (N=15), and the results need to be validated with further studies using a larger number of patients. The differences in the study populations might explain the discrepancy between their results and the results of the present study. Pleural fluid CHT activity was also investigated in TB and non-TB pleural effusions [16]. Bouzas et al. demonstrated that pleural fluid CHT levels in 12 patients with TB pleurisy were significantly higher than those in lymphocytic non-TB pleural effusions, whereas there was no significant difference between TB pleural effusions and neutrophilic pleural effusions. They also observed a positive correlation between pleural fluid CHT and adenosine deaminase, which is used as a diagnostic tool for TB pleurisy in some circumstances due to its high sensitivity and specificity. Iyer et al. conducted a study among patients with leprosy, which is another mycobacterial disease [26]. Serum CHT activity in 78 leprosy patients was significantly higher than that in 36 healthy controls, and a significant decrease was detected after treatment; furthermore, serum CHT activity was significantly correlated with serum neopterin levels, which is another marker of activated macrophages.
In recent years, several studies have reported elevated CHT activity in sarcoidosis, which is another granulomatous disease that primarily involves the lungs [5, 10-12, 27]. Serum CHT activity in patients with sarcoidosis was first investigated by Grosso et al. [10]. The authors reported that compared to healthy controls, sarcoidosis patients, especially those in the active phase, had increased levels of CHT, and serum CHT correlated with the radiological stage of the disease. Bargagli et al. reported that serum CHT levels in sarcoidosis patients were nearly 10-fold more than that in healthy controls [5, 11]. Furthermore, CHT levels in sarcoidosis patients were approximately 6-fold higher than those of PTB patients, although the number of PTB patients was relatively low (N=15), suggesting that the different magnitudes of CHT activity observed in these different granulomatous diseases may depend on separate mechanisms of macrophage activation or different cytokine profiles. This finding might have special clinical value, since differential diagnosis of TB and sarcoidosis presents a problem for physicians in daily medical practice when they confronted with a lung biopsy revealing granulomatous inflammation.
In conclusion, we suggest that elevated serum CHT activity in PTB might be a marker of disease extent, severity, and response to antituberculous treatment. However, further studies in larger populations are needed to validate these data and to reveal the clinical usefulness of the enzyme, including in differential diagnosis between other lung diseases.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Di Rosa M, Musumeci M, Scuto A, Musumeci S, Malaguarnera L. Effect of interferon-γ, interleukin-10, lipopolysaccharide and tumor necrosis factor-α on chitotriosidase synthesis in human macrophages. Clin Chem Lab Med. 2005;43:499–502. doi: 10.1515/CCLM.2005.088. [DOI] [PubMed] [Google Scholar]
- 2.Malaguarnera L. Chitotriosidase: the yin and yang. Cell Mol Life Sci. 2006;63:3018–3029. doi: 10.1007/s00018-006-6269-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollak CE, van Weely S, van Oers MH, Aerts JM. Marked elevation of plasma chitotriosidase activity. A novel hallmark of Gaucher disease. J Clin Invest. 1994;93:1288–1292. doi: 10.1172/JCI117084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Michelakakis H, Dimitriou E, Labadaridis I. The expanding spectrum of disorders with elevated plasma chitotriosidase activity: an update. J Inherit Metab Dis. 2004;27:705–706. doi: 10.1023/b:boli.0000043025.17721.fc. [DOI] [PubMed] [Google Scholar]
- 5.Bargagli E, Maggiorelli C, Rottoli P. Human chitotriosidase: a potential new marker of sarcoidosis severity. Respiration. 2008;76:234–238. doi: 10.1159/000134009. [DOI] [PubMed] [Google Scholar]
- 6.Artieda M, Cenarro A, Gañán A, Jericó I, Gonzalvo C, Casado JM, et al. Serum chitotriosidase activity is increased in subjects with atherosclerosis disease. Arterioscler Thromb Vasc Biol. 2003;23:1645–1652. doi: 10.1161/01.ATV.0000089329.09061.07. [DOI] [PubMed] [Google Scholar]
- 7.Malaguarnera L, Rosa MD, Zambito AM, dell'Ombra N, Marco RD, Malaguarnera M. Potential role of chitotriosidase gene in nonalcoholic fatty liver disease evolution. Am J Gastroenterol. 2006;101:2060–2069. doi: 10.1111/j.1572-0241.2006.00680.x. [DOI] [PubMed] [Google Scholar]
- 8.Altarescu G, Rudensky B, Abrahamov A, Goldfarb A, Rund D, Zimran A, et al. Plasma chitotriosidase activity in patients with beta-thalassemia. Am J Hematol. 2002;71:7–10. doi: 10.1002/ajh.10151. [DOI] [PubMed] [Google Scholar]
- 9.Comabella M, Domínguez C, Rio J, Martín-Gallán P, Vilches A, Vilarrasa N, et al. Plasma chitotriosidase activity in multiple sclerosis. Clin Immunol. 2009;131:216–222. doi: 10.1016/j.clim.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Grosso S, Margollicci MA, Bargagli E, Buccoliero R, Perrone A, Galimberti D, et al. Serum levels of chitotriosidase as a marker of disease activity and clinical stage in sarcoidosis. Scand J Clin Lab Invest. 2004;64:57–62. doi: 10.1080/00365510410004092. [DOI] [PubMed] [Google Scholar]
- 11.Bargagli E, Margollicci M, Nikiforakis N, Luddi A, Perrone A, Grosso S, et al. Chitotriosidase activity in the serum of patients with sarcoidosis and pulmonary tuberculosis. Respiration. 2007;74:548–552. doi: 10.1159/000100555. [DOI] [PubMed] [Google Scholar]
- 12.Bargagli E, Margollicci M, Luddi A, Nikiforakis N, Perari MG, Grosso S, et al. Chitotriosidase activity in patients with interstitial lung diseases. Respir Med. 2007;101:2176–2181. doi: 10.1016/j.rmed.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Gray JW. Childhood tuberculosis and its early diagnosis. Clin Biochem. 2004;37:450–455. doi: 10.1016/j.clinbiochem.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Segura RM, Pascual C, Ocaña I, Martínez-Vázquez JM, Ribera E, Ruiz I, et al. Adenosine deaminase in body fluids: a useful diagnostic tool in tuberculosis. Clin Biochem. 1989;22:141–148. doi: 10.1016/s0009-9120(89)80013-x. [DOI] [PubMed] [Google Scholar]
- 15.Deniz O, Gumus S, Yaman Y, Ciftci F, Ors F, Cakir E, et al. Serum total cholesterol, HDL-C and LDL-C concentrations significantly correlate with the radiological extent of disease and the degree of smear positivity in patients with pulmonary tuberculosis. Clin Biochem. 2007;40:162–166. doi: 10.1016/j.clinbiochem.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 16.Bouzas L, San José E, Tutor JC. Chitotriosidase activity in pleural effusions. Clin Lab. 2007;53:449–452. [PubMed] [Google Scholar]
- 17.Seaton A, Seaton D, et al., editors. Crofton and Douglas's Respiratory Diseases. 4th ed. London: Blackwell Science; 1989. [Google Scholar]
- 18.Deniz O, Gumus S, Yaman H, Ciftci F, Ors F, Cakir E, et al. Serum total cholesterol, HDL-C and LDL-C concentrations significantly correlate with the radiological extent of disease and the degree of smear positivity in patients with pulmonary tuberculosis. Clin Biochem. 2007;40:162–166. doi: 10.1016/j.clinbiochem.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 19.Poggi A, Catellani S, Musso A, Zocchi MR. Gammadelta T lymphocytes producing IFNgamma and IL-17 in response to Candida albicans or mycobacterial antigens: possible implications for acute and chronic inflammation. Curr Med Chem. 2009;16:4743–4749. doi: 10.2174/092986709789878238. [DOI] [PubMed] [Google Scholar]
- 20.van Eijk M, van Roomen CP, Renkema GH, Bussink AP, Andrews L, Blommaart EF, et al. Characterization of human phagocyte-derived chitotriosidase, a component of innate immunity. Int Immunol. 2005;17:1505–1512. doi: 10.1093/intimm/dxh328. [DOI] [PubMed] [Google Scholar]
- 21.Labadaridis I, Dimitriou E, Theodorakis M, Kafalidis G, Velegraki A, Michelakakis H. Chitotriosidase in neonates with fungal and bacterial infections. Arch Dis Child Fetal Neonatal Ed. 2005;90:F531–F532. doi: 10.1136/adc.2004.051284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lehrnbecher T, Bernig T, Hanisch M, Koehl U, Behl M, Reinhardt D, et al. Common genetic variants in the interleukin-6 and chitotriosidase genes are associated with the risk for serious infection in children undergoing therapy for acute myeloid leukemia. Leukemia. 2005;19:1745–1750. doi: 10.1038/sj.leu.2403922. [DOI] [PubMed] [Google Scholar]
- 23.Choi EH, Zimmerman PA, Foster CB, Zhu S, Kumaraswami V, Nutman TB, et al. Genetic polymorphisms in molecules of innate immunity and susceptibility to infection with Wuchereria bancrofti in South India. Genes Immun. 2001;2:248–253. doi: 10.1038/sj.gene.6363767. [DOI] [PubMed] [Google Scholar]
- 24.Malaguarnera L, Musumeci M, Di Rosa M, Scuto A, Musumeci S. Interferon-gamma, tumor necrosis factor-alpha, and lipopolysaccharide promote chitotriosidase gene expression in human macrophages. J Clin Lab Anal. 2005;19:128–132. doi: 10.1002/jcla.20063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kurt YG, Cayci T, Onguru P, Akgul EO, Yaman H, Aydin I, et al. Serum chitotriosidase enzyme activity in patients with Crimean-Congo hemorrhagic fever. Clin Chem Lab Med. 2009;47:1543–1547. doi: 10.1515/CCLM.2009.347. [DOI] [PubMed] [Google Scholar]
- 26.Iyer A, van Eijk M, Silva E, Hatta M, Faber W, Aerts JM, et al. Increased chitotriosidase activity in serum of leprosy patients: association with bacillary leprosy. Clin Immunol. 2009;131:501–509. doi: 10.1016/j.clim.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Tercelj M, Salobir B, Simcic S, Wraber B, Zupancic M, Rylander R. Chitotriosidase activity in sarcoidosis and some other pulmonary diseases. Scand J Clin Lab Invest. 2009;69:575–578. doi: 10.1080/00365510902829362. [DOI] [PubMed] [Google Scholar]