Abstract
Objective: Low-level laser therapy (LLLT) is a treatment method commonly used in physiotherapy for musculoskeletal disorders. The aim of this study was to monitor the function of temporomandibular joint (TMJ) and surrounding tissues and compare the objective measurements of the effect of LLLT. Background data: LLLT has been considered effective in reducing pain and muscular tension; thus improving the quality of patients' lives. Materials and Methods: TMJ function was evaluated by cephalometric tracing analysis, orthopantomogram, TMJ tomogram, and computer face-bow record. Interalveolar space between central incisors before and after therapy was measured. Patients evaluated pain on the Visual Analog Scale. LLLT was performed in five treatment sessions (energy density of 15.4 J/cm2) by semiconductive GaAlAs laser with an output of 280 mW, emitting radiation wavelength of 830 mm. The laser supplied a spot of∼0.2 cm2. Results: Baseline comparisons between the healthy patients and patients with low-level laser application show that TMJ pain during function is based on anatomical and function changes in TMJ areas. Significant differences were seen in the posterior and anterior face height. The results comparing healthy and impaired TMJ sagittal condyle paths showed that patients with TMJ pain during function had significantly flatter nonanatomical movement during function. After therapy, the unpleasant feeling was reduced from 27.5 to 4.16 on the pain Visual Analog Scale. The pain had reduced the ability to open the mouth from 34 to 42 mm. Conclusions: The laser therapy was effective in the improvement of the range of temporomandibular disorders (TMD) and promoted a significant reduction of pain symptoms.
Introduction
Temporomandibular disorders (TMD) occur as a result of problems with the jaw, temporomandibular joint (TMJ), and surrounding facial muscles that control chewing and moving the jaw.1 The TMJ is the hinge joint that connects the lower jaw (mandible) to the temporal bone of the skull, which is immediately in front of the ear on each side of the head. The joints are flexible, allowing the jaw to move smoothly up and down and from side to side. Symptoms of TMD include headaches, tenderness of the chewing muscles, and clicking or locking of the joints.2 More than 40% of the general population has at least one sign of TMD; however, only one in four of such people is actually aware of, or reports any symptoms, with only 10–20 % seeking treatment.3 One of the most popular areas of TMD research is developing clear guidelines for diagnosing these disorders. Automatic measurement and classification of TMDs before and during the treatment can assist in early diagnosis and accurate monitoring of treatment, and can enhance the efficacy of the treatment.
Current methods for TMD detection involve a physical examination by an expert in the TMJ area.2 A dentist or clinician almost always diagnoses a TMD, based solely on a person's medical history and on a physical examination. A typical clinical finding of patients with TMD is a lateral and posterior tenderness of the TMJ on palpation, and pain in the area of the TMJ during maximum opening and during lateral excursion. A TMD patient has pain/ discomfort in the jaw, mainly in the region of the TMJ and/or muscles of mastication, and limitation of mandibular function.4–7
These patients can be managed with nonsurgical therapies, but some end-stage TMJ patients require surgical TMJ repair or reconstruction. A multifactor etiology for TMD is proposed. The possible suggested causal factors include many different structural parameters such as psychological variables, acute trauma, degenerative articular illness, and functional mandibular overload variables. The patient can develop end-stage TMJ as a result of trauma, osteoarthritis, reactive arthritis, ankylosis, idiopathic condylar resorption, connective tissue/autoimmune diseases (e.g., rheumatoid arthritis, psoriatic arthritis, lupus, scleroderma, Sjogren's syndrome, ankylosing spondylitis) or other TMJ pathologies.4
Unclear etiology of TMD, the same clinical findings resulting from various causes and the proven relation between TMD and psychological factors, are the main reasons why there is still no consensus in classification of TMD.1,8 One of the most commonly used diagnostic schemes intended for research purposes is the Research Diagnostic Criteria for TMD (RDC/TMD). It standardizes clinical examination of patients with TMD, improves reproducibility among clinicians, and facilitates comparison of results among researchers.1 TMD is considered to be a subgroup of musculoskeletal disorders.8–10 This may explain reports of successful use of physical therapy in the treatment of TMD.
Low-level laser therapy (LLLT) is a local application of a monochromatic, narrow-band, coherent light source. LLLT is recommended as a treatment option for TMD guidelines but with limitations, because of heterogeneous laser parameters and a lack of dosage consensus in the LLLT literature. The action of LLLT is disputed, but it the analgesic, anti-inflammatory and stimulative effects have been confirmed.11–18 Although LLLT is a treatment method commonly used in physiotherapy of musculoskeletal disorders, there are few studies that deal with its utilization in the treatment of TMD.
The aim of study is monitor the function of TMJ and surrounding tissues and compare the objective results of the effect of LLLT.
Materials and Methods
Subjects
The study group consisted of 104 consecutive patients (17 men with average age 18.57 years and 87 women with average age 27.57 years) with TMJ pain, who were referred from medical practitioners and dentists to the Department of Oral and Maxillofacial Surgery at Charles University in the years 2010–2011. The clinic is the primary referral center for TMD at the institution, as both conservative and surgical treatments are offered. Patients were referred to the center for treatment with reported pain or malfunction of the temporomandibular region as the primary problem. The patients including in our study were divided into several groups according to the type of therapy used:
No treatment, 2 patients (2.08 %);
Conservative treatment and stabilization splint, 48 patients (49.92 %);
Conservative treatment, stabilization splint and physical therapy including GaAlAs laser, 27 patients (28.08 %);
Conservative treatment, stabilization splint and arthrocentesis, 12 patients (12.48 %);
Conservative treatment, stabilization splint and wisdom teeth extraction, 8 patients (8.32 %); and
Surgical therapy; TMJ prosthesis, 7 patients (7.28 %).
The criteria of inclusion/exclusion for different groups were presence of pain, tenderness over the TMJ, swelling of the TMJ, and abnormal motion of the TMJ.
Average length of treatment was 11.58 months for men and 9.45 months for women.
Of the total of 104 TMJ pain patients referred for the first assessment, 77 did not meet the inclusion criteria; 27 subjects were included in this study. All had failed to obtain satisfactory pain relief after an initial treatment protocol, including self-care (soft diet, cold/hot packs) and occlusal appliance (hard acrylic, full-arch maxillary stabilization–type splint). Patients were instructed to adhere to this treatment protocol for a period of 6 weeks; they were not subjected to treatment within the last 2 weeks before the trial.
The prospective study was conducted according to American Dental Association (ADA) recommendations. Patients were requested to provide informed consent to the clinical examination and regular follow-ups, including photographic records by means of the informed consent form in accordance with the Declaration of Helsinki.
Clinical examination
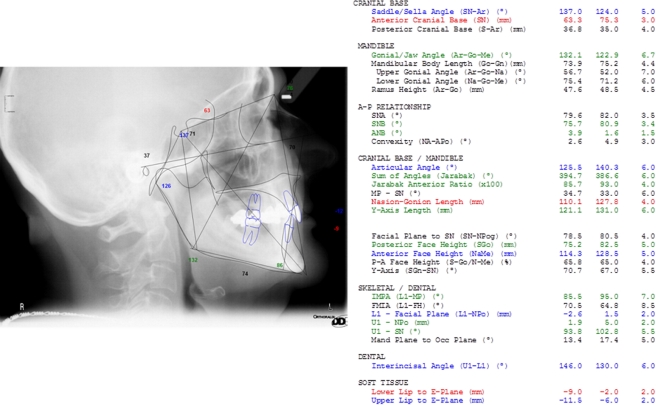
Treatment was initiated in the incorrect jaw alignment evaluation. A gradual analysis of TMJ was evaluated by cephalometric radiography, orthopantomogram, TMJ tomogram (Gendex, Oralix 9200, Milan, Italy), and computer face-bow record (Arcus Digma, KAVO Dental, Biberach, Germany). Twenty-four different measurements (22 skull points; computer-assisted analysis) were used as determinates of the skeletal sagittal jaw relationship (Fig. 1). Dolphin Imaging 11.0 – Cephalometric Tracing Analysis (CephX Inc. Las Vegas, NV) evaluated the planes: SNA,sella-nasion point A; SNB, sella-nasion point B; SGo NMe, sella-gonion nasion-menton; Ar-Go-Me, articulare gonion-menton; the results were compared with healthy orthodontic patients.19
FIG. 1.
Dolphin imaging 11.0 – cephalometric tracing analysis.
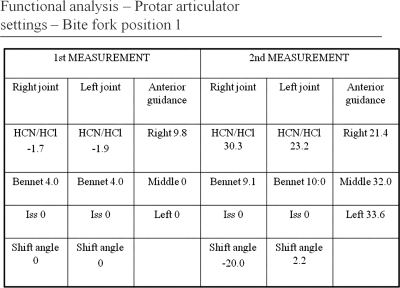
Computer face-bow record (Arcus Digma, KAVO Dental, Biberach, Germany) and functional analysis with Protar articulator settings (KAVO Dental, Biberach, Germany) monitored the TMJ movement before and after treatment (Fig. 2).
FIG. 2.
Computer face-bow record and functional analysis with Protar articulator settings monitor the TMJ movement before and after treatment.
Interalveolar space between central incisors before and after therapy was measured.
Subjective observations
Patients evaluated pain on the Visual Analog Scale (VAS); where 0 indicates “no pain” and 100 indicates “the worst possible pain.” The reported pain by patients on VAS was determined.
Treatment
Patients were recommended not to open the mouth maximally; to avoid biting hard food, and not to chew gum. Stabilization with hard acrylic splint was made to cover all the teeth in the upper jaw. The splint surface was smooth to provide centric relation occlusion, eliminating posterior interferences and anterior guidance on frontal teeth and reducing neuromuscular activity. When the pain was not reduced the low-level laser was applied.
Statistical analysis
Statistical Student t test (at the significance level p=0.01) including standard deviation was implemented to monitor objective measurements and subjective pain evaluation.
Laser system treatment
LLLT was performed in five treatment sessions by semiconductive GaAlAs laser (BTL Beauty-line Technology Laser, Brno, Czech Republic) with an output operating power of 280 mW, emitting radiation wavelength of 830 mm. The laser supplied a spot of ∼0.2 cm.2
Patients were treated with an energy density of 15, 4 J/cm2 in five sessions (five weekly treatments)15 (Table 1). The laser probe with collimation tip was placed over the spots that were tender to palpation on the masticatory muscles, which were detected during the clinical examination in front of the tragus, when the mouth was open, through the meatus acusticus externus, when the mouth was open, and 2 cm in front of tragus, under the zygomatic arch, when the mouth was closed. The total treatment dose was 46.2 J/cm2; total energy was 9.24 J.
Table 1.
Laser Experimental Arrangement
| Laser medium | GaAlAs laser diode |
|---|---|
| Wavelength | 830 nm |
| Output power - maximum | 400 mW |
| Output power - operating | 280 mW |
| Probe aperture | 0.2 cm2 |
| Energy density | 15.4 J/cm2 |
| Time | 11 sec |
| Frequency | Continuous |
| Kind of application | Contact |
| Number of treatment sessions | 5 |
| Number of treated points | 3 |
| Total treatment dose | 46.2 J/cm2 |
| Total energy | 9.24 J |
Results
Baseline comparisons between the healthy patients and patients with low-level laser application show that TMJ pain during function is based on anatomical and function changes in TMJ areas. Significant differences were seen in the posterior face height and anterior face height. Relationships SNA, SNB, and SGo:Nme were significantly lower and the Ar-Go–Me –area was significantly higher (Table 2) when the values were compared with the healthy patients.
Table 2.
Cephalometric Analysis
| Analysis20 | SNA | SNB | Sgo:Nme | Ar-Go-Me |
|---|---|---|---|---|
| Bjork | 82.0 SD:3.5 |
80.9 SD:3.4 |
120.8 SD:6.7 |
|
| Roth-Jarabak | 82.0 | 80.9 | 65.0 SD:4.0 |
120.8 SD:6.7 |
| Jarabak | 82.0 | 80.9 | 65.0 | 120.8 SD:6.7 |
| McLaughlin | 82.0 | 80.0 SD:3.0 |
||
| Czech standard population | 80.82 SD: 4.20 |
78.66 SD: 3.94 |
70.83 SD:5.49 |
|
| Czech TMJ diseases | ↓ 80.08a SD: 3.16 |
↓ 76.56a SD: 3.88 |
↓ 64.84a SD:5.65 |
↑ 125.32a SD: 7.07 |
SNA, sella-nasion Point A; SNB, sella-nasion Point B; SGo:Nme, sella-gonion nasion-menton; Ar-Go–Me, articulare gonion-menton.
Significant value; SD. standard deviation.
Also, the results comparing healthy and impaired TMJ sagittal condyle paths showed that patients with TMJ pain during function had flatter nonanatomical movement during function. Those differences between left and right TMJ were also significant (Table 3).
Table 3.
Arcus Digma Analysis
| TMD | Average value | SD | Sig. (two-tailed) | ||
|---|---|---|---|---|---|
| Right joint | HCN/HCI | l. sin. | 32.60 | 7.70 | * 0.013 |
| l. dx. | 11.56 | 17.56 | |||
| Bennett angle | l. sin. | 8.17 | 4.90 | 0.96 | |
| l. dx. | 7.99 | 8.91 | |||
| ISS | l. sin. | 0.06 | 0.15 | 0.34 | |
| l. dx. | 0.00 | ||||
| Shift angle | l. sin. | -4.84 | 15.20 | 0.64 | |
| l. dx. | -0.49 | 18.16 | |||
| Left joint | HCN/HCI | l. sin. | 31.47 | 13.65 | * 0.11 |
| l. dx. | 10.74 | 24.52 | |||
| Bennett | l. sin. | 10.67 | 7.67 | 0.74 | |
| l. dx. | 9.04 | 8.10 | |||
| ISS | l. sin. | 0.12 | 0.12 | 0.21 | |
| l. dx. | 0.04 | 0.05 | |||
| Shift angle | l. sin. | 3.80 | 15.97 | 0.97 | |
| l. dx. | 3.44 | 20.04 | |||
| Anterior guidance | Right | l. sin. | 22.08 | 16.55 | 0.21 |
| l. dx. | 38.88 | 24.52 | |||
| Middle | l. sin. | 31.13 | 25.32 | 0.67 | |
| l. dx. | 37.48 | 21.31 | |||
| Left | l. sin. | 34.68 | 13.01 | 0.19 | |
| l. dx. | 21.66 | 17.15 |
HCN, joint path angle; HCI, horizontal condylar inclination; ISS, immediate side shift; l. sin., lateris sinistri (laterotrusion left); l. dx., lateris dextri (laterotrusion right).
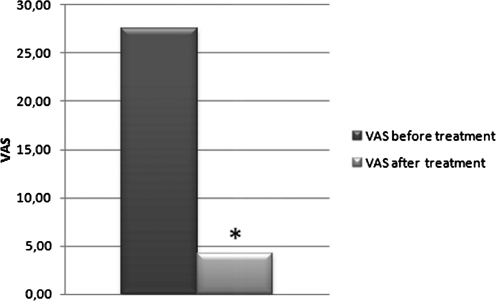
The running evaluation of the treatment results showed that decrease in pain occurred in the majority of TMD patients between the second and fourth therapeutic sessions. The unpleasant feeling was reduced on the pain VAS after therapy from 27.5 (variability±9.89) to 4.16 (variability±5.84) (Fig. 3).
FIG. 3.
Visual Analog Scale (VAS).
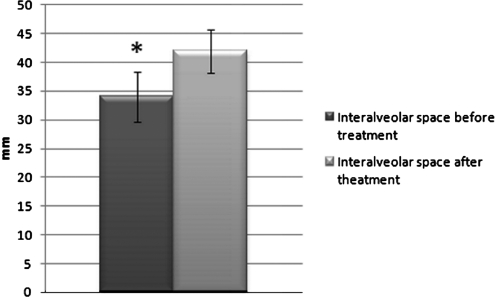
The pain had reduced the ability to open the mouth. After application of laser, the ability to open the mouth increased from 34 (variability±4.32) to 42 mm (variability±3.77) (23.53 %) (Fig. 4).
FIG. 4.
Interalveolar space between central incisors before and after therapy.
Paired Student t test at the significance level p=0.01 objectively verified interalveolar space increase and confirmed VAS pain decrease.
Discussion and Conclusions
The initial treatment of TMD frequently focuses on the use of placebo control methods.15 LLLT was applied in our study as a noninvasive auxiliary therapy for pain decrease in patients with TMD. It has been employed as element that has biomodulatory, anti-inflammatory and analgesic effects on physiological, cellular, and systemic responses. LLLT has been considered effective in reducing pain and muscular tension, thus improving the quality of patients' lives.20 Dose and beam parameters are critical for successful laser, LED, and other light therapy treatment.21 In our study, it was confirmed that patients not only had anatomical changes in the TMJ but also had reduced anterior and posterior face height. Deformities were the cause the TMJ pain, and analgesic effects helped to reduce the chronic pain.
Evaluations analyzing the painful symptoms at the right and the left sides in the treated group show that there was a significant difference between the healthy and impaired TMJ. LLLT was effective in reducing the painful symptoms following optimal mouth opening. LLLT increased pain tolerance because of changes in cellular membrane potency, vasodilatation, reduction of edema, increase in intracellular metabolism, and acceleration of wound healing. 20,22
The laser therapy was efficient in promoting an increase of mandibular movements in the patients who received the active laser dose.23 We also confirmed the fact that the analgesic effect of low-intensity lasers had a direct effect on mouth opening and decrease in the VAS scores. Those results showed significant differences among the healthy and impaired TMJ.
It is known that LLLT was applied on the selected points considering the presence of nociceptors in the periarticular tissues (discal ligaments, capsular ligaments, and retrodiscal tissues), because these structures are involved in TMJ pain.15,23,24 Our study verified that pain in TMJ is directly connected with discrepancies in TMJ paths and in the physiology and anatomy of the dental skull. The actual analgesic efficacy of LLLT stems from the fact that TMD symptoms have been treated by a wide array of methods separately, such as interocclusal splint, medication, physical therapy, and surgical procedures, and lasers can be of great value because of the increase of beta endorphin level, increase of pain discharge threshold, decrease of bradykinin and histamine release, increase of lymphatic flow, decrease of edema and algesic substances, increase of blood supply, time reduction of inflammation, and promotion of muscle relaxation.25
The results of the study confirmed that the laser therapy was effective in the improvement of the range of TMD, and promoted a significant reduction of pain symptoms.
Acknowledgment
This research has been supported by a Grant of the Czech Ministry of Education by IGA MZCR 9902-4, 9991-4 Grant, and GAUK No.: 89008.
Author Disclosure Statement
No conflicting financial interests exist.
References
- 1.McNeill C. Temporomandibular disorders: guidelines for classification, assessment and management. Chicago: Quintessence Publishing Co., Inc; 1993. [Google Scholar]
- 2.Dworkin S.F. LeResche L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, criteria. J. Craniomandib. Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 3.Okeson J.P. Guidelines for assessment, diagnosis, and management. Chicago: Quintessence Publishing Co., Inc; 1996. Orofacial pain. [Google Scholar]
- 4.Wilding R.J. Shaikh M. Muscle activity and jaw movements as predictors of chewing performance. J. Orofac. Pain. 1997;11:24–36. [PubMed] [Google Scholar]
- 5.Christensen L.V. Rassouli M.N. Experimental occlusal interferences. Part V. Mandibular rotations versus hemimandibular translations. J. Oral Rehabil. 1995;22:865–876. doi: 10.1111/j.1365-2842.1995.tb00235.x. [DOI] [PubMed] [Google Scholar]
- 6.Took C.C. Sanei S. Chambers J. Dunne S. Underdetermined blind source separation of temporomandibular joint sounds. IEEE Trans. Biomed. Eng. 2006;53:2123–2126. doi: 10.1109/TBME.2006.881789. [DOI] [PubMed] [Google Scholar]
- 7.Kuwahara T. Bessette R.W. Maruyama T. Chewing pattern analysis in TMD patients with unilateral internal and bilateral derangement. Cranio. 1995;13:167–172. doi: 10.1080/08869634.1995.11678063. [DOI] [PubMed] [Google Scholar]
- 8.McNeill C. History and evolution of TMD concepts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1997;83:51–60. doi: 10.1016/s1079-2104(97)90091-3. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein B. Temporomandibular disorders: A review of current understanding. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999;88:379–385. doi: 10.1016/s1079-2104(99)70048-x. [DOI] [PubMed] [Google Scholar]
- 10.Bradley P. Groth E. Gursoy B. The maxillofacial region: recent research and clinical practice in low intensity level laser therapy. In: Simunovic Z., editor. Lasers in Medicine and Dentistry. Vitagrad: DTP Studio; 2000. pp. 385–400. [Google Scholar]
- 11.Beckerman H. de Bie R.A. Bouter L.M. De Cuyper H.J. Oostendrop R.A.B. The efficacy of laser for musculoskeletal and skin disorders: a criteria – based meta-analysis of randomized clinical trials. Phys. Ther. 1992;72:13–21. doi: 10.1093/ptj/72.7.483. [DOI] [PubMed] [Google Scholar]
- 12.Bertolucci L.E. Grey T. Clinical analysis of mid-laser versus placebo treatment of arthralgic TMJ degenerative joints. J. Craniomandibular Pract. 1995;13:27–29. doi: 10.1080/08869634.1995.11678038. [DOI] [PubMed] [Google Scholar]
- 13.Kulekcioglu S. Sivrioglu K. Ozcan O. Parlak M. Effectiveness of low level laser therapy in temporomandibular disorders. Scand. J. Rheumatol. 2003;32:114–118. doi: 10.1080/03009740310000139. [DOI] [PubMed] [Google Scholar]
- 14.Gray R.J.M. Davies S.J. Quayle A.A. A clinical approach to temporomandibular disorders: A clinical approach to treatment. Br. Dent. J. 1994;6:101–106. doi: 10.1038/sj.bdj.4808513. [DOI] [PubMed] [Google Scholar]
- 15.Tuner J. Hode L. Clinical practice and scientific background. Tallinn, Estonia: Prima Books; 2002. Laser therapy. [Google Scholar]
- 16.Fikackova H. Dostalova T. Navratil L. Klaschka J. Effectiveness of low–level laser therapy in temporomandibular joint disorders: a placebo-controlled study. Photomed. Laser Surg. 2007;25:297–303. doi: 10.1089/pho.2007.2053. [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi M. Kubota J. Treatment of TMJ pain with diode laser therapy. Laser Ther. 1999;1:11–18. [Google Scholar]
- 18.Bezzur N.J. Habets L.L.M. Hansson T.L. The effect of therapeutic laser in patients with craniomandibular disorders. J. Craniomandib. Disord. 1988;2:83–86. [PubMed] [Google Scholar]
- 19.Hansson T. Infrared laser in the treatment of craniomandibular disorders, arthrogenous pain. J. Prosthet. Dent. 1989;61:614–617. doi: 10.1016/0022-3913(89)90287-4. [DOI] [PubMed] [Google Scholar]
- 20.Janega M. Rehacek A. Hofmanova P. Dostalova T. Smahel Z. Veleminska J. Fendrychova J. Cephalometric analysis of cephalometric radiograms of healthy patients in prosthodontics and orthodontics. Prakt. Zubn. Lek. 2009;57:112–116. [Google Scholar]
- 21.Jenkins P. A. Carroll J. D. How to report low-level laser therapy (LLLT) / photomedicine dose and beam parameters in clinical and laboratory studies. Photomed. Laser Surg. 2011;29:785–7. doi: 10.1089/pho.2011.9895. [DOI] [PubMed] [Google Scholar]
- 22.Mazzetto M.O. Carrasco T.G. Bidinelo E.F. Pizzo R.C.A. Mazzetto R.G. Low intensity laser application in temporomandibular disorders: a phase I double-blind study. J. Craniomandib. Pract. 2007;25:186–192. doi: 10.1179/crn.2007.029. [DOI] [PubMed] [Google Scholar]
- 23.Kulekcioglu S. Sivrioglu K. Ozcan O. Parlak M. Effectiveness of low-level laser therapy in temporomandibular disorder. Scand. J. Rheumatol. 2003;32:114–118. doi: 10.1080/03009740310000139. [DOI] [PubMed] [Google Scholar]
- 24.Nunez S.H. Garcez A.S. Suzuki S.S. Ribeiro M.S. Management of mouth opening in patients with temporomandibular disorders through low-level laser therapy and transcutaneous electrical neural stimulation. Photomed. Laser Surg. 2006;24:45–49. doi: 10.1089/pho.2006.24.45. [DOI] [PubMed] [Google Scholar]
- 25.Pinheiro A.L.B. Cavalcanti E.T. Rego T. Pinheiro M. Manzi C.T. Low power laser therapy in the management of disorders of the maxillofacial region. J Clin Laser Med Surg. 1997;15:181–183. doi: 10.1089/clm.1997.15.181. [DOI] [PubMed] [Google Scholar]