Abstract
Context
The extent to which better spending produces higher-quality care and better patient outcomes in a universal health care system with selective access to medical technology is unknown.
Objective
To assess whether acute care patients admitted to higher-spending hospitals have lower mortality and readmissions.
Design, Setting, and Patients
The study population comprised adults (> 18 years) in Ontario, Canada, with a first admission for acute myocardial infarction (AMI) (n=179 139), congestive heart failure (CHF) (n=92 377), hip fracture (n=90 046), or colon cancer (n=26 195) during 1998–2008, with follow-up to 1 year. The exposure measure was the index hospital’s end-of-life expenditure index for hospital, physician, and emergency department services.
Main Outcome Measures
The primary outcomes were 30-day and 1-year mortality and readmissions and major cardiac events (readmissions for AMI, angina, CHF, or death) for AMI and CHF.
Results
Patients’ baseline health status was similar across hospital expenditure groups. Patients admitted to hospitals in the highest- vs lowest-spending intensity terciles had lower rates of all adverse outcomes. In the highest- vs lowest-spending hospitals, respectively, the age- and sex-adjusted 30-day mortality rate was 12.7% vs 12.8% for AMI, 10.2% vs 12.4% for CHF, 7.7% vs 9.7% for hip fracture, and 3.3% vs 3.9% for CHF; fully adjusted relative 30-day mortality rates were 0.93 (95% CI, 0.89–0.98) for AMI, 0.81 (95% CI, 0.76–0.86) for CHF, 0.74 (95% CI, 0.68–0.80) for hip fracture, and 0.78 (95% CI, 0.66–0.91) for colon cancer. Results for 1-year mortality, readmissions, and major cardiac events were similar. Higher-spending hospitals had higher nursing staff ratios, and their patients received more inpatient medical specialist visits, interventional (AMI cohort) and medical (AMI and CHF cohorts) cardiac therapies, preoperative specialty care (colon cancer cohort), and postdischarge collaborative care with a cardiologist and primary care physician (AMI and CHF cohorts).
Conclusion
Among Ontario hospitals, higher spending intensity was associated with lower mortality, readmissions, and cardiac event rates.
Numerous studies have investigated whether higher health care spending produces better patient outcomes and higher quality of care. Evidence from the United States and other countries has been conflicting.1–12 Several studies focusing on short-term outcomes within a given state found that being treated in higher-spending hospitals was associated with better in-hospital3 or 30-day4,5 mortality. In contrast, a national study found that regional differences in spending intensity were largely attributable to use of the hospital as a site of care and greater overall use of specialists, imaging, and diagnostic testing but that patients treated in regions with higher spending intensity did not have better survival or quality of care.1,2 Whether these findings would hold true in a country with universal access to health care but a far lower supply of specialists and more selective access to medical technology is unknown.
Our objective was to assess whether acute care patients admitted to Canadian hospitals that treat patients more intensively (and at higher cost) have lower mortality and readmissions and higher quality of care.
METHODS
Design Overview
We undertook a longitudinal cohort study of patients hospitalized with selected acute clinical conditions in Ontario, Canada, and assessed the content, quality, and outcomes with respect to “exposure” to the index hospital’s medical spending intensity. Medical intensity is defined as the quantity of medical care provided overall to similarly ill patients and is a marker of a hospital’s propensity to treat similarly ill patients more (or less) intensively. It reflects the component of spending variation attributable to practice style rather than to differences in illness or price.
Because sicker patients use more services, higher-spending hospitals may appear to have worse outcomes, in part because patients are more severely ill. We used several techniques to remove this potential “reverse causality,” as in previous work.1–4 First, we studied patients with selected acute conditions who were likely to present with similar mean illness severity, rather than all admissions, to remove differences in case mix across hospitals.1,2 Second, the exposure of interest was spending at the hospital level rather than the patient level to study the effects of exposure to a system of care; this also removed potential survival bias resulting from analyzing patient-level spending.13 Last, estimates of a hospital’s spending intensity, the exposure variable, were based on individuals in their last year of life, a different group of patients, to further remove potential reverse causality between study cohort illness and spending1–4; hospital spending intensity for study patients was used as an exposure in a secondary analysis. The study was approved by the research ethics board of Sunnybrook Health Sciences Centre
Study Cohorts
We studied 4 common conditions that have moderate to high incidence and mortality, that can be validly ascertained using health administrative data, and for which treatment follows relatively standard protocols.
Study patients comprised Ontario residents hospitalized with first (index) admission for acute myocardial infarction (AMI) (n=179 139), congestive heart-failure (CHF) (n=92 377), hip fracture (n=90 046), or colon cancer with surgical resection (n=26 195)1,2,14 to Ontario acute care hospitals between April 1, 1998, and March 31, 2008, restricting to adults aged 18 to 105 years. To capture incident admissions, we excluded patients with AMI and hip fracture admitted for these conditions during the previous year and patients with CHF having a CHF admission in the previous 3 years. We included patients with a first diagnosis of colon cancer undergoing potentially curative resection within 6 months, excluding those who presented with metastatic cancer or who were diagnosed with any other cancer within the previous 5 years. We excluded patients with AMI having a stay of less than 3 days.
Patients were assigned to the cohort corresponding to their earliest admission and underwent follow-up for 1 year after the index admission date. We created an index episode of care beginning at initial admission and ending at the final discharge, incorporating transfers. To ensure stability of the hospital-specific measures, we restricted to 129 hospitals with more than 10 study condition admissions per year, resulting in exclusion of 27% of hospitals but only 3% of patients.
Hospital Spending Intensity Index
The primary exposure measure was the hospital end-of-life expenditure index (EOL-EI), calculated as the mean adjusted spending on hospital, emergency department (ED), and physician services provided to decedents in their last year of life, similar to previous work.1,2 Costs for hospital admissions and ED visits were based on standardized provincial prices and reflected resources used. Costs for physician services for inpatient and outpatient visits as well as diagnostic tests and procedures were based on the fees paid on the physician claims. Details on Ontario costing algorithms are provided in the eAppendix available at http://www.jama.com.
We first assigned all Ontario decedents during 1998–2008 to the study hospital where they had the most admissions during the last 2 years of life, as in previous work.1,2 Those who were not hospitalized or were primarily hospitalized to nonstudy hospitals were not assigned. Costs were computed for individuals and aggregated to the hospital level across all decedents assigned to the hospital. A hospital’s EOL-EI was estimated as adjusted spending per capita for decedents assigned to that hospital and was indirectly adjusted for age and sex using the entire cohort as the standard. All spending was attributed to the assigned hospital even if the patient received services elsewhere, because this hospital and its associated medical staff was deemed to represent the “system” within which the patient received care.15
We also calculated each hospital’s acute care expenditure index (AC-EI) as the mean adjusted spending for study patients admitted to that hospital for hospital, ED, and physician services during 1 year following date of admission. Costs were determined similarly to the above and reported as adjusted spending per capita for study patients admitted to each hospital.
Although EOL-EI measures hospital practice intensity at the end of life whereas AC-EI measures hospital practice intensity during acute illness, they were highly correlated (r=0.81), implying that medical intensity, however measured, is a hospital “signature” and reflects the intensity of care provided to sick patients. EOL-EI was used as the primary exposure because it was considered a more exogenous measure of hospital intensity for several reasons. First, it was measured on a different group than the actual study cohort. Second, it was less related to underlying illness severity, because decedents were similarly ill in one respect: their life expectancy was identical. It would thus be more reflective of hospital resource capacity and physician practice style to all patients admitted to that hospital. We used EOL-EI as a “look-back” hospital intensity measure to look forward to assess outcomes in the study cohorts.
Study patients were assigned the EOL-EI and AC-EI expenditure indexes of their hospital of admission and categorized into approximate terciles of low, medium, and high intensity.
Outcomes
The primary outcomes were 30-day and 1-year mortality as well as 30-day and 1-year readmissions, a marker of general complications.16 For cardiac cohorts, we assessed major cardiac events, defined as readmission for AMI, CHF, or angina.17–19 Readmissions were analyzed as a combined outcome with mortality, because the factors causing mortality were likely an exacerbation of those causing readmission so that these events were not independent, making it inappropriate to censor for mortality.
Quality of Care
The following quality measures were examined: preoperative visit with a surgeon and anesthetist (colon cancer cohort); surgery within 2 days of admission (hip fracture cohort),20 inpatient rehabilitation (hip fracture cohort), same-day percutaneous coronary intervention (PCI) (AMI cohort),18,19 and number of medical specialist visits during the index episode.21
The following procedures were examined among patients in the AMI and CHF cohorts who survived 30 days after admission: cardiac catheterization, coronary revascularization (coronary artery bypass graft surgery or PCI), prescriptions of angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers and statins (patients 65 years or older in the AMI and CHF cohorts),17–19 and for CHF, prescription of β-blockers and contraindicated medications (nonsteroidal anti-inflammatory drugs or class I antiarrhythmics). We examined collaborative care, defined as an ambulatory visit with a primary care physician and a cardiologist within 4 weeks of discharge, and ambulatory visits with a cardiologist (AMI and CHF cohorts).22,23
Hospital volume was computed as mean number of cases admitted to the hospital per year over the study period, specific to each study condition.24–26 Attending physician volume was computed as mean number of cases per year based on claims for services rendered on the admission date, by condition.24
Data Sources
Patient records were linked using unique, anonymized, encrypted identifiers across multiple Ontario health administrative databases containing information on all publicly insured, medically necessary hospital and physician services. These databases included the Discharge Abstract Database for hospital admissions, intensive care unit admissions (after 2002), procedures, and transfers, which includes the most responsible diagnosis for length of stay, secondary diagnosis codes, comorbidities present at admission, complications occurring during the hospital stay, and attending physician identifier; the National Ambulatory Care Reporting System for ED visits; the Ontario Health Insurance Plan for physician billings, which includes diagnosis codes and procedures and location of visit; the Ontario Drug Benefits for outpatient drug prescriptions for patients 65 years or older; and the Registered Persons Database for patient demographic information and deaths. Nursing inpatient hours per weighted patient day and per acute care bed were obtained from the Canadian Management Information System27; we could not distinguish registered nurses from other nursing staff.
Cohort membership for AMI, CHF, and hip fracture was determined using the most responsible diagnosis. The colon cancer cohort was derived using the Ontario Cancer Registry and linked to Discharge Abstract Database records to determine colectomy. Comorbidities were identified using secondary Discharge Abstract Database diagnosis fields, excluding complications. Studies have confirmed the validity and reliability of Ontario’s health administrative data.28,29 International Classification of Diseases, Ninth Revision (before April 1, 2002) and International Classification of Diseases, 10th Revision–Canada (after April 1, 2002) diagnosis codes and the Canadian Classification of Procedures (before April 1, 2002) and Canadian Classification of Interventions (after April 1, 2002) procedure codes used in the study are reported in the eAppendix. Neighborhood income was derived from Statistics Canada census estimates from 2001 (1999–2003 cohorts) and 2006 (2004–2008 cohorts).
Statistical Analyses
Models used patient as the unit of analysis and EOL-EI hospital expenditure categories as the primary exposure variable. This allowed us to control for individual risk factors and permitted inferences to individual patients, although exposures were measured at the hospital level. For each condition, we developed a baseline patient severity score by using logistic regression models to predict 30-day mortality, incorporating all baseline patient characteristics and comorbidities (C statistics, 0.74–0.79).2,14
Cox proportional hazards models were used to compare rates of mortality and readmissions across hospital expenditure categories. Models controlled for baseline patient characteristics, including age group (20–45, 46–64, 65–74, 75–84, ≥85 years), sex, and their interactions; neighborhood income quintiles; individual Charlson comorbidities at admission and during the previous 5 years; condition-specific hospital volume and teaching status; and year of admission. Cardiac models also controlled for condition-specific comorbidities at admission; history of AMI, coronary artery bypass graft surgery, or PCI in the previous 5 years (AMI cohort); and receipt of an implantable cardioverter-defibrillator or permanent pacemaker in the previous 5 years (CHF cohort).23,30 Each cohort was analyzed separately. To determine whether specific components of spending intensity explained the relationships, we added several hospital-level structural and process measures to the models, including attending physician volume, regional cancer center (colon cancer cohort), intensity of interventional (30-day cardiac catheterization rate) and medical (discharge statin prescribing rate) therapies (AMI and CHF cohorts),14 inpatient specialist visit rate, and nursing staff ratios.31
Patients admitted to the same hospital are likely to be treated similarly and have correlated outcomes. We used survival models that account for clustering of patients within hospitals by including a working correlation matrix to adjust the standard errors.32
Statistical tests were 2-sided and performed at the 5% level of significance. Analyses were performed using the STATA procedure STCOX.33
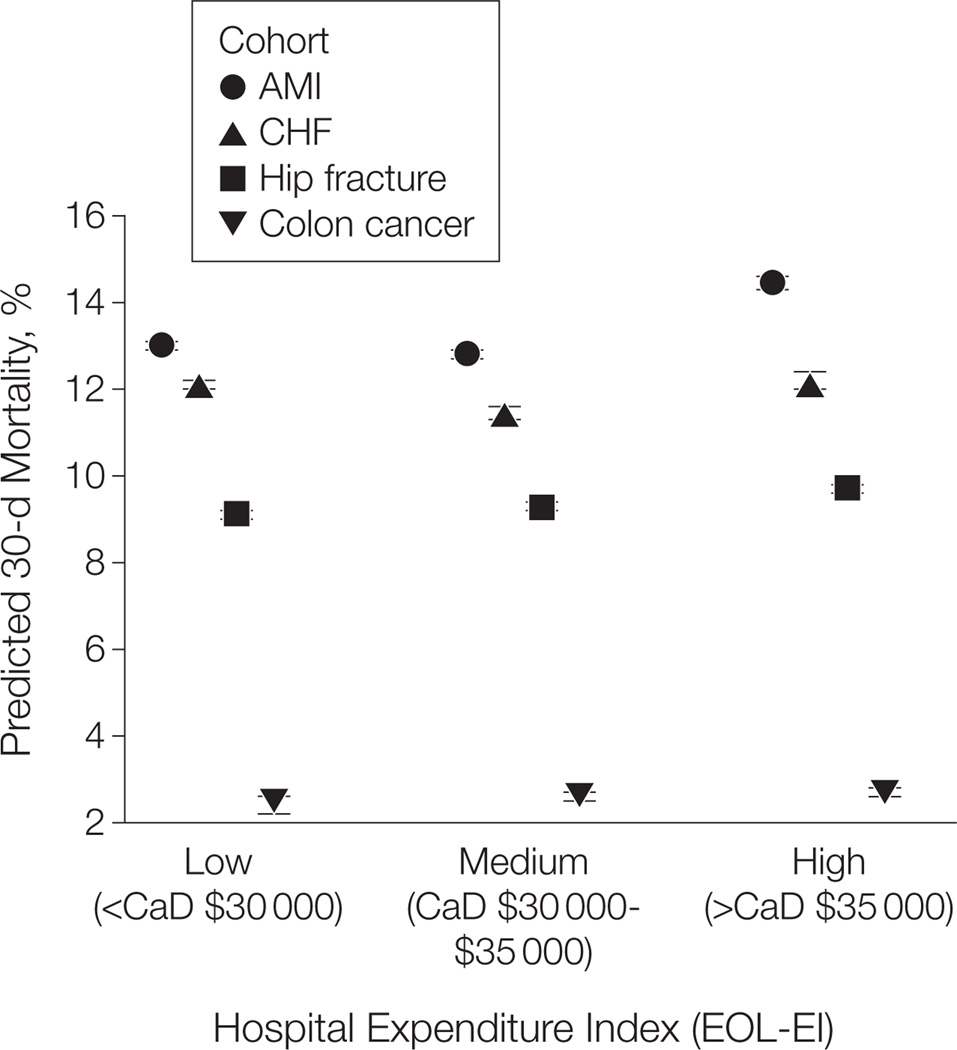
RESULTS
Adjusted spending intensity varied about 2-fold across hospitals. In Canadian dollars, EOL-EI ranged from $22 000 to $45 000 (US $21 978–$44 955) and AC-EI from $19 300 to $32 580 (US $19 281–$32 548) per capita per year. Although there were small differences in some risk factors, mean predicted 30-day mortality, the summary measure of baseline illness severity, was similar across hospital spending groups (Figure 1). The majority of the 1-year costs were incurred during the index hospital episode, varying from 42% for CHF to 64% to 72% for other conditions.
Figure 1.
Baseline Patient Severity, Measured as Predicted 30-Day Mortality Rate, Against Hospital Expenditure Index Group for the 4 Cohorts
End-of-life expenditure index (EOL-EI) ranges, in US dollars, are <$29 970 for the low EOL-EI category, $29 970–$34 965 for the medium EOL-EI category, and >$34 965 for the high EOL-EI category. AMI indicates acute myocardial infarction; CHF, congestive heart failure. Error bars indicate 95% confidence intervals.
Higher-spending hospitals tended to be higher-volume teaching or community hospitals; be located in urban areas; be associated with regional cancer centers; have on-site computed tomography and magnetic resonance imaging scanners, cardiac catheterization laboratories, and cardiac surgery capability; and be early adopters of critical care response teams (Table 1). Attending physicians in these hospitals were more likely to be specialists or to care for a higher volume of patients with that condition. These hospitals provided 30% more inpatient nursing hours per weighted patient day and per acute care bed.
Table 1.
Selected Hospital and Physician Characteristics, According to Hospital Expenditure Index
| Cohort Characteristics | EOL-EI, % | ||
|---|---|---|---|
| Low | Medium | High | |
| Acute myocardial infarction | n = 55 814 | n = 56 777 | n = 66 548 |
| Hospital characteristics High-volume hospital (>200 patients with AMI per y) Teaching |
0.0 | 5.2 | 32.8 |
| Community | 35.9 | 64.8 | 53.1 |
| On-site catheterization laboratory | 3.9 | 31.9 | 39.8 |
| On-site CABG capacity | 2.5 | 12.7 | 34.8 |
| Attending physician characteristics Cardiology |
9.4 | 29.5 | 59.5 |
| Annual AMI volume >24 patients | 28.8 | 52.1 | 44.9 |
| Congestive heart failure | n = 31 160 | n = 26 743 | n = 34 474 |
| Hospital characteristics High-volume hospital (>200 patients with CHF per y) Teaching |
0.0 | 4.2 | 29.9 |
| Community | 20.9 | 50.4 | 49.9 |
| Attending physician characteristics Cardiology |
4.5 | 15.4 | 32.6 |
| General internal medicine | 28.5 | 34.3 | 42.8 |
| Annual CHF volume >13 patients | 27.4 | 39.4 | 45.9 |
| Hip fracture | n = 26 151 | n = 27 896 | n = 35 999 |
| Hospital characteristics High-volume hospital (>150 patients with hip fracture per y) Teaching |
0.0 | 7.1 | 35.4 |
| Community | 19.3 | 39.0 | 37.2 |
| Operating surgeon characteristics Orthopedic surgeon |
82.2 | 85.0 | 89.6 |
| Annual hip fracture repair volume >18 patients | 78.2 | 75.8 | 70.8 |
| Colon cancer | n = 7184 | n = 8285 | n = 10 726 |
| Hospital characteristics High-volume hospital (>135 patients with colon cancer per y) Teaching |
0.0 | 6.2 | 49.3 |
| Community | 26.1 | 59.0 | 41.9 |
| Associated with regional cancer center | 9.2 | 29.9 | 44.5 |
| Operating surgeon characteristics Annual colon cancer resection volume >35 patients |
30.5 | 44.2 | 56.6 |
| Hospital characteristics among combined cohorts | n = 120 309 | n = 119 701 | n = 147 747 |
| On-site CT scanner | 59.2 | 90.1 | 92.2 |
| On-site MRI scanner | 6.0 | 50.8 | 79.4 |
| On-site critical care response team (2007 forward) | 4.8 | 29.1 | 79.3 |
| Inpatient nursing hours, mean (SD) Per weighted patient day |
7.7 (1.4) | 8.8 (1.2) | 10.1 (2.1) |
| Per acute care bed | 2405 (557) | 2849 (544) | 3268 (813) |
Abbreviations: AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery; CHF, congestive heart failure; CT, computed tomography; EOL-EI, end-of-life expenditure index; MRI, magnetic resonance imaging.
Table 2 reports selected therapies and procedures for each cohort, according to EOL-EI group, averaged over the 10-year period. Patients admitted to higher-spending hospitals had longer lengths of stay, were less likely to be admitted to an intensive care unit, and had more medical specialist visits during the index episode. Cardiac patients admitted to higher-spending hospitals were more likely to receive cardiac interventions and evidence-based discharge medications. They were also more likely to experience collaborative ambulatory care within 4 weeks and to visit a cardiologist within 1 year. Patients with CHF were less likely to receive contraindicated medications; those with hip fracture were more likely to receive inpatient rehabilitation; and those with colon cancer were more likely to have a preoperative consultation with a surgeon and anesthetist and to undergo computed tomography for preoperative staging.
Table 2.
Selected Therapies and Procedures, According to Hospital Expenditure Index, Averaged Over the 10-Year Period
| Cohort Characteristics | EOL-EI, % | ||
|---|---|---|---|
| Low | Medium | High | |
| Acute myocardial infarction | n = 55 814 | n = 56 777 | n = 66 548 |
| Selected inpatient care during index episode Index episode length of stay, median (IQR), d |
7 (5–11) | 7 (5–12) | 8 (5–13) |
| Inpatient medical specialist consults, median (IQR) | 3 (1–6) | 4 (2–7) | 6 (3–10) |
| ICU admission during index episode (2002 forward) | 75.7 | 70.0 | 65.1 |
| Interventional cardiac therapies Cardiac catheterization within 30 d |
33.0 | 43.6 | 45.8 |
| CABG surgery or PCI within 30 d | 21.6 | 28.8 | 31.2 |
| PCI same day | 1.3 | 4.1 | 8.4 |
| Discharge drug prescriptions within 30 d Patients ≥65 y, alive 4 weeks post discharge, No. |
29 288 | 28 054 | 34 482 |
| ACE inhibitor/ARB | 62.6 | 64.8 | 66.7 |
| Statins | 48.3 | 53.5 | 57.3 |
| Postdischarge ambulatory care Patients alive 30 d post discharge, No. |
48 022 | 49 211 | 57 073 |
| Visit to PCP within 4 weeks | 74.3 | 72.5 | 71.8 |
| Visit to cardiologist within 4 weeks | 8.7 | 14.9 | 17.2 |
| Visit to PCP and cardiologist within 4 weeks | 6.7 | 11.5 | 12.5 |
| Visit to cardiologist within 1 y | 35.3 | 50.9 | 58.6 |
| Congestive heart failure | n = 31 160 | n = 26 743 | n = 34 474 |
| Selected inpatient care during index episode Index episode length of stay, median (IQR), d |
7 (4–11) | 7 (4–11) | 7 (4–12) |
| Inpatient medical specialist consults, median (IQR) | 2 (0–4) | 3 (0–6) | 5 (2–11) |
| ICU admission during index episode (2002 forward) | 28.6 | 23.2 | 18.1 |
| Inpatient echocardiogram | 9.3 | 10.2 | 11.6 |
| Discharge drug prescriptions within 30 d Patients ≥65 y, alive 4 weeks post discharge, No. |
22 432 | 19 108 | 24 685 |
| ACE inhibitor/ARB | 62.2 | 62.5 | 61.3 |
| β-Blockers | 31.5 | 35.6 | 39.6 |
| Statins | 17.9 | 23.2 | 26.4 |
| NSAIDs/class I AAD within 1 y (contraindicated) | 19.2 | 18.2 | 15.5 |
| Postdischarge ambulatory care Patients alive 30 d post discharge, No. |
26 696 | 23 392 | 30 182 |
| Visit to PCP within 4 weeks | 68.8 | 67.3 | 65.5 |
| Visit to cardiologist within 4 weeks | 5.1 | 12.4 | 15.9 |
| Visit to PCP and cardiologist within 4 weeks | 3.6 | 9.5 | 11.2 |
| Visit to cardiologist within 1 y | 17.8 | 34.4 | 42.1 |
| Hip fracture | n = 26 151 | n = 27 896 | n = 35 999 |
| Selected inpatient care during index episode Surgery ≤2 d after admission |
77.7 | 84.1 | 81.9 |
| Index episode length of stay, median (IQR), d | 11 (8–18) | 11 (7–19) | 12 (8–21) |
| Inpatient medical specialist consults, median (IQR) | 1 (0–3) | 1 (0–4) | 2 (0–7) |
| ICU admission during index episode (2002 forward) | 9.0 | 8.2 | 8.5 |
| Inpatient rehabilitation | 17.4 | 27.5 | 39.8 |
| Colon cancer | n = 7184 | n = 8285 | n = 10 726 |
| Selected preoperative specialty care Preoperative consult with anesthetist, within 4 weeks |
18.3 | 27.4 | 35.8 |
| Preoperative consult with surgeon, within 6 weeks | 44.8 | 43.0 | 48.8 |
| CT scan prior to surgery for preoperative staging | 31.6 | 33.0 | 45.0 |
| Selected inpatient care during index episode Index episode length of stay, median (IQR), d |
10 (8–14) | 9 (7–14) | 9 (7–14) |
| Inpatient medical specialist consults, median (IQR) | 0 (0–2) | 0 (0–2) | 0 (0–3) |
| ICU admission during index episode (2002 forward) | 38.3 | 30.8 | 19.5 |
Abbreviations: AAD, antiarrhythmic drug; ACE, angiotensin-converting enzyme; ARB, angiotensin II receptor blocker; CABG, coronary artery bypass graft; CT, computed tomography; EOL-EI, end-of-life expenditure index; ICU, intensive care unit; IQR, interquartile range; NSAIDs, nonsteroidal anti-inflammatory drugs; PCI, percutaneous coronary intervention; PCP, primary care physician.
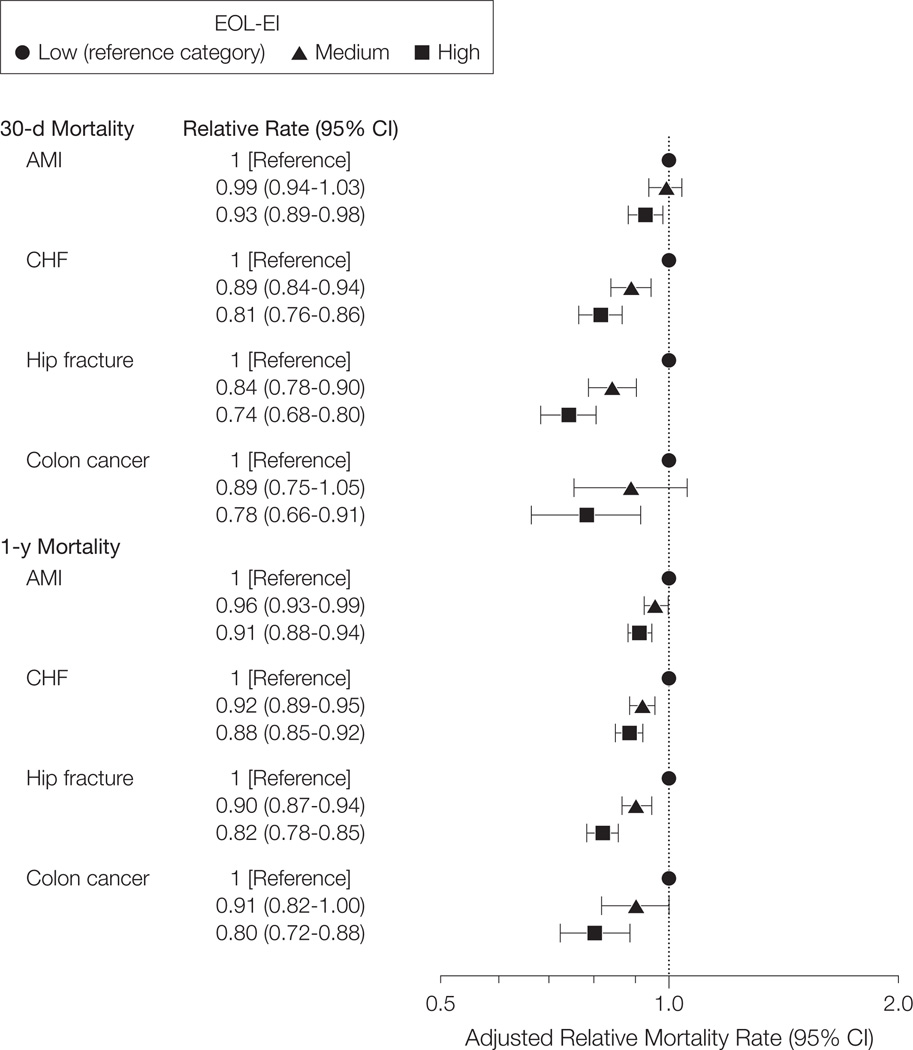
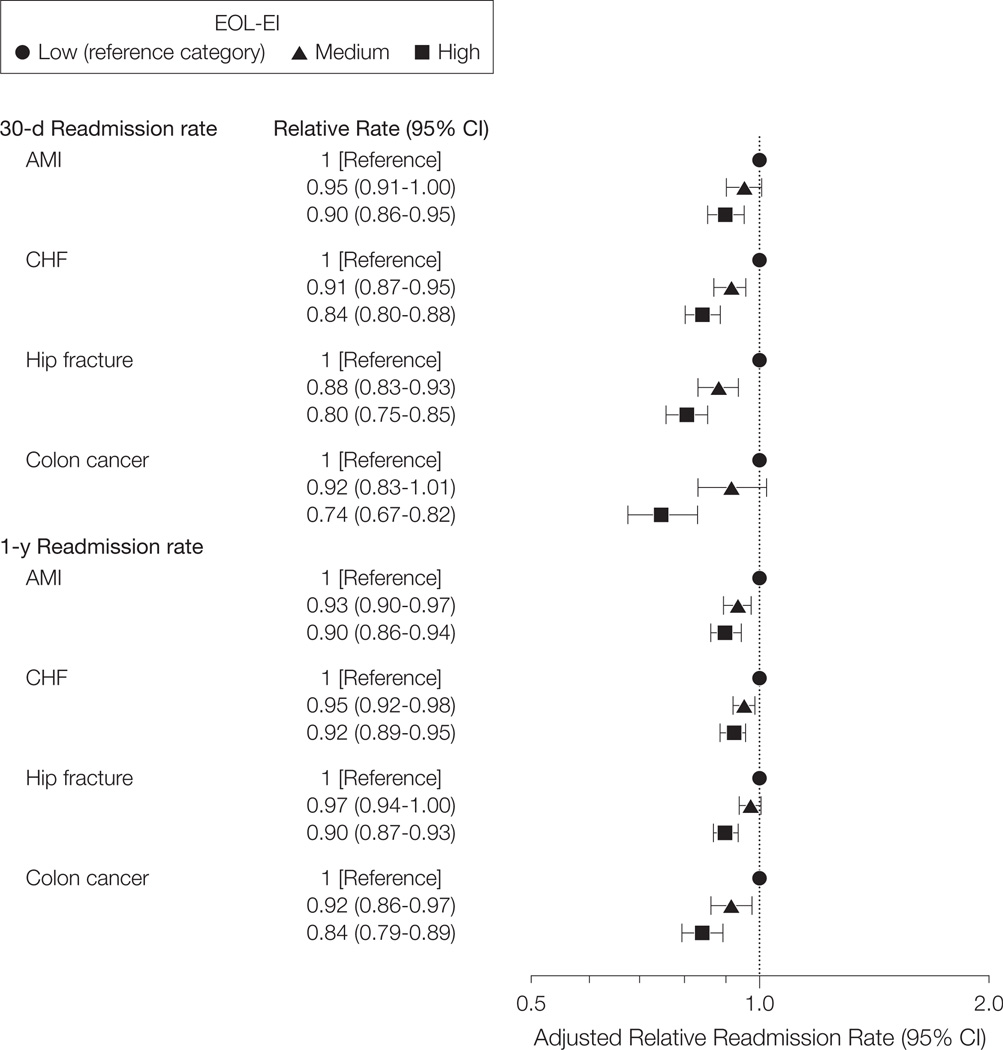
In the highest- vs lowest-spending hospitals, respectively, the age- and sex-adjusted 30-day mortality rate was 12.7% vs 12.8% for AMI, 10.2% vs 12.4% for CHF, 7.7% vs 9.7% for hip fracture, and 3.3% vs 3.9% for colon cancer. The age-and sex-adjusted 30-day major cardiac event rate was 17.4% vs 18.7% for patients with AMI and 15.0% vs 17.6% for those with CHF. The age- and sex-adjusted 30-day readmission rate was 23.1% vs 25.8% for patients with hip fracture and 10.3% vs 13.1% for those with colon cancer. In higher-spending hospitals, age- and sex-adjusted mortality and readmission rates were lower for all cohorts (Table 3). After full adjustment, mortality and readmission rates were lower in higher-spending hospitals for all cohorts (Figure 2 and Figure 3). Although some of the hospital-level structural and process measures were significantly related to the outcomes, results were similar when adding these variables to the models. Findings were also similar using the “look-forward” hospital expenditure index (AC-EI) as the exposure measure (eAppendix). Results did not change when stratified by age group (younger than 65 years and 65 years or older), sex, and neighborhood income quintile or after excluding remote northern hospitals.
Table 3.
Age- and Sex-Adjusted Outcomes According to Hospital Expenditure Index, Averaged Over the 10-Year Period
| Cohort Outcomes | EOL-EI, % | ||
|---|---|---|---|
| Low | Medium | High | |
| Acute myocardial infarction | n = 55 814 | n = 56 777 | n = 66 548 |
| Death Within 30 d of admission |
12.8 | 12.7 | 12.7 |
| Within 1 y of admission | 22.5 | 21.9 | 22.4 |
| Major cardiac event Within 30 d of admission |
18.7 | 17.8 | 17.4 |
| Within 1 y of admission | 37.8 | 35.7 | 35.9 |
| Congestive heart failure | n = 31 160 | n = 26 743 | n = 34 474 |
| Death Within 30 d of admission |
12.4 | 10.8 | 10.2 |
| Within 1 y of admission | 32.3 | 29.9 | 29.8 |
| Major cardiac event Within 30 d of admission |
17.6 | 15.8 | 15.0 |
| Within 1 y of admission | 47.0 | 45.1 | 44.8 |
| Hip fracture | n = 26 151 | n = 27 896 | n = 35 999 |
| Death Within 30 d of admission |
9.7 | 8.5 | 7.7 |
| Within 1 y of admission | 25.8 | 24.5 | 23.1 |
| Readmission or death Within 30 d of admission |
14.8 | 13.4 | 12.3 |
| Within 1 y of admission | 47.6 | 46.5 | 44.1 |
| Colon cancer | n = 7184 | n = 8285 | n = 10 726 |
| Death Within 30 d of admission |
3.9 | 3.6 | 3.3 |
| Within 1 y of admission | 10.9 | 10.4 | 9.7 |
| Readmission or death Within 30 d of admission |
13.1 | 12.2 | 10.3 |
| Within 1 y of admission | 40.4 | 38.6 | 36.9 |
Abbreviation: EOL-EI, end-of-life expenditure index.
Figure 2.
Multivariate Adjusted Relative 30-Day and 1-Year Mortality Rates for Medium and High vs Low Hospital Expenditure Groups for the 4 Cohorts
End-of-life expenditure index (EOL-EI) ranges, in Canadian dollars, are <$30 000 (US $29 970) for the low EOL-EI category, $30 000 to $35 000 (US $29 970–$34 965) for the medium EOL-EI category, and >$35 000 (US $34 965) for the high EOL-EI category. AMI indicates acute myocardial infarction; CHF, congestive heart failure.
Figure 3.
Multivariate Adjusted Relative 30-Day and 1-Year Cardiac (AMI, CHF) and All-Cause (Hip Fracture, Colon Cancer) Readmission Rates for Medium and High vs Low Hospital Expenditure Groups for the 4 Cohorts
End-of-life expenditure index (EOL-EI) ranges, in Canadian dollars, are <$30 000 (US $29 970) for the low EOL-EI category, $30 000 to $35 000 (US $29 970–$34 965) for the medium EOL-EI category, and >$35 000 (US $34 965) for the high EOL-EI category. AMI indicates acute myocardial infarction; CHF, congestive heart failure.
COMMENT
We found that higher hospital spending intensity was associated with better survival, lower readmission rates, and better quality of care for seriously ill, hospitalized patients in Ontario in a universal health care system with more selective access to medical technology. Higher-spending hospitals were higher-volume teaching or community hospitals with high-volume or specialist attending physicians and having specialized programs, such as regional cancer centers, and specialized services, such as on-site cardiac catheterization, cardiac surgery, and diagnostic imaging facilities. The study also points to plausible mechanisms through which higher spending may be associated with better outcomes.
Benefits appeared early, suggesting an acute-phase hospital effect. For acute conditions, timely access to preoperative and in-hospital specialist care, skilled nursing staff, rapid response teams, cardiac high-technology services, and regional cancer centers, all found in the higher-spending systems, are related to better outcomes.21,27,34–39 These systems also provided consistently, but not strikingly, higher levels of evidence-based care and collaborative ambulatory care, both shown to improve care.22,23,40 Higher spending on evidence-based services delivered in the acute phase of care for severely ill hospitalized patients—by far the largest component of spending for our cohorts—is indeed likely to be beneficial.
It would be facile to interpret this study as demonstrating that higher spending is causally related to better outcomes and that providing more money to lower-spending hospitals would necessarily improve their outcomes. Higher-spending hospitals differed in many ways, such as greater use of evidence-based care, skilled nursing and critical care staff, more intensive inpatient specialist services, and high technology, all of which are more expensive.
To place the study in context, the United States has a 3- to 4-times higher per capita supply of specialized technology, such as computed tomography and magnetic resonance imaging scanners, but a similar supply of acute care beds and nurses.41 Ontario 2001 population rates of cardiac testing and revascularization lagged behind corresponding 1992 US rates and paralleled the supply of cardiologists and catheterization facilities. 42–44 It is therefore possible that Canadian hospitals, with fewer specialized resources, selective access to medical technology, and global budgets, are using these resources more efficiently, especially during the inpatient episode for care-sensitive conditions.45,46 Canada’s health care expenditures per capita are about57%of those in the United States.47 At this spending level, there might still be a positive association between spending and outcomes. For example, the same-day PCI rate for patients with AMI in low-intensity hospitals in 2008 was 3.5%, leaving room for improvement. This pattern is consistent with studies in the United States showing a positive association between spending and outcomes among low-intensity hospitals or regions but no association at average or higher intensity levels.5,6
Strengths of the study include the population-based, longitudinal cohort design; the consistency of findings across cardiac, cancer, medical, and surgical patients; the examination of plausible clinical mechanisms whereby higher intensity maybe associated with better outcomes; and the examination of readmissions. The “look-back” (EOL-EI) and “look-forward” (AC-EI) measures of spending intensity were highly correlated and produced similar findings, as in US studies.2
Several limitations should be considered. Because the design precludes strong inferences about causation, we cannot know which components of care may have led to better outcomes. In observational studies, comparisons of exposure groups may be biased because of unobserved selection bias.13 It is unlikely that the findings are the result of unmeasured case mix, because patients in higher-spending hospitals had similar or higher illness severity at admission, which would, if anything, bias toward finding worse outcomes. We cannot rule out the possibility that higher-intensity hospitals coded more aggressively, but there is less incentive to do so in a system with global hospital budgets. Although admission severity would be determined more accurately using clinical detail from medical charts, previous work has shown high concordance between risk-adjusted hospital outcomes using chart and administrative data.48,49 Canadian data distinguish between comorbidities present at admission and complications, leading to improved admission severity coding. The EOL-EI has been critiqued for the purpose of estimating hospital efficiency50,51 but is used here simply to distinguish high- and low-intensity hospitals, as in other US studies. 1–4 The findings may not generalize to chronic conditions, for which avoiding exacerbations of disease that lead to hospitalization through coordinated ambulatory care is key. The findings also may not generalize to jurisdictions in which hospital resources are more abundant and are used in cost-effective as well as cost-ineffective ways, leading to inefficiency. 45,46
This study shows that in Ontario, a province with global hospital budgets and fewer specialized health care resources than the United States, outcomes following an acute hospitalization are positively associated with higher hospital spending intensity. Higher spending intensity, in turn, is associated with greater use of specialists, better patient care, and more use of advanced procedures. These results suggest that it is critical to understand not simply how much money is spent but whether it is spent on effective procedures and services.
Acknowledgments
Funding/Support: Funding was provided by an Emerging Team Grant (ETG92248) in Applied Health Services and Policy Research from the Canadian Institutes of Health Research, by a grant from the US National Institute on Aging (1PO1-AG19783-01), and by the Institute for Clinical Evaluative Sciences, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care.
Role of the Sponsors: The funding agencies had no role in design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Stukel had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Stukel, Fisher, Alter, Guttmann, Fung.
Acquisition of data: Stukel.
Analysis and interpretation of data: Stukel, Fisher, Alter, Guttmann, Ko, Fung, Wodchis, Baxter, Earle, Lee.
Drafting of the manuscript: Stukel.
Critical revision of the manuscript for important intellectual content: Stukel, Fisher, Alter, Guttmann, Ko, Fung, Wodchis, Baxter, Earle, Lee.
Statistical analysis: Stukel, Fung, Wodchis.
Obtained funding: Stukel.
Study supervision: Stukel.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Online-Only Material: The eAppendix and Author Video Interview are available at http://www.jama.com.
Additional Contributions: We thank Nancy Mac-Callum, MLIS, and Ashley Corallo, MPH, Institute for Clinical Evaluative Sciences, Toronto, for assistance with manuscript preparation. These individuals received no compensation beyond salary for their contributions.
REFERENCES
- 1.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending, 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 2.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending-2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 3.Romley JA, Jena AB, Goldman DP. Hospital spending and inpatient mortality: evidence from California: an observational study. Ann Intern Med. 2011;154(3):160–167. doi: 10.7326/0003-4819-154-3-201102010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silber JH, Kaestner R, Even-Shoshan O, Wang Y, Bressler LJ. Aggressive treatment style and surgical outcomes. Health Serv Res. 2010;45(6, pt 2):1872–1892. doi: 10.1111/j.1475-6773.2010.01180.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnato AE, Chang CC, Farrell MH, Lave JR, Roberts MS, Angus DC. Is survival better at hospitals with higher “end-of-life” treatment intensity? Med Care. 2010;48(2):125–132. doi: 10.1097/MLR.0b013e3181c161e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goodman DC, Fisher ES, Little GA, Stukel TA, Chang CH, Schoendorf KS. The relation between the availability of neonatal intensive care and neonatal mortality. N Engl J Med. 2002;346(20):1538–1544. doi: 10.1056/NEJMoa011921. [DOI] [PubMed] [Google Scholar]
- 7.Skinner JS, Staiger DO, Fisher ES. Is technological change in medicine always worth it? the case of acute myocardial infarction. Health Aff (Millwood) 2006;25(2):w34–w47. doi: 10.1377/hlthaff.25.w34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin S, Rice N, Smith PC. Does health care spending improve health outcomes? evidence from English programme budgeting data. J Health Econ. 2008;27(4):826–842. doi: 10.1016/j.jhealeco.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Chen LM, Jha AK, Guterman S, Ridgway AB, Orav EJ, Epstein AM. Hospital cost of care, quality of care, and readmission rates: pennywise and pound foolish? Arch Intern Med. 2010;170(4):340–346. doi: 10.1001/archinternmed.2009.511. [DOI] [PubMed] [Google Scholar]
- 10.Landrum MB, Meara ER, Chandra A, Guadagnoli E, Keating NL. Is spending more always wasteful? the appropriateness of care and outcomes among colorectal cancer patients. Health Aff (Millwood) 2008;27(1):159–168. doi: 10.1377/hlthaff.27.1.159. [DOI] [PubMed] [Google Scholar]
- 11.Yasaitis L, Fisher ES, Skinner JS, Chandra A. Hospital quality and intensity of spending: is there an association? Health Aff (Millwood) 2009;28(4):w566–w572. doi: 10.1377/hlthaff.28.4.w566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rothberg MB, Cohen J, Lindenauer P, Maselli J, Auerbach A. Little evidence of correlation between growth in health care spending and reduced mortality. Health Aff (Millwood) 2010;29(8):1523–1531. doi: 10.1377/hlthaff.2009.0287. [DOI] [PubMed] [Google Scholar]
- 13.Stukel TA, Fisher ES, Wennberg DE, Alter DA, Gottlieb DJ, Vermeulen MJ. Analysis of observational studies in the presence of treatment selection bias: effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. JAMA. 2007;297(3):278–285. doi: 10.1001/jama.297.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stukel TA, Alter DA, Schull MJ, Ko DT, Li P. Association between hospital cardiac management and outcomes for acute myocardial infarction patients. Med Care. 2010;48(2):157–165. doi: 10.1097/MLR.0b013e3181bd4da7. [DOI] [PubMed] [Google Scholar]
- 15.Shortell SM, Casalino LP. Health care reform requires accountable care systems. JAMA. 2008;300(1):95–97. doi: 10.1001/jama.300.1.95. [DOI] [PubMed] [Google Scholar]
- 16.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 17.Lee DS, Tran C, Flintoft V, Grant FC, Liu PP, Tu JV. Canadian Cardiovascular Outcomes Research Team/Canadian Cardiovascular Society Heart Failure Quality Indicator Panel. CCORT/CCS quality indicators for congestive heart failure care. Can J Cardiol. 2003;19(4):357–364. [PubMed] [Google Scholar]
- 18.Tu JV, Khalid L, Donovan LR, Ko DT. Canadian Cardiovascular Outcomes Research Team/Canadian Cardiovascular Society Acute Myocardial Infarction Quality Indicator Panel. Indicators of quality of care for patients with acute myocardial infarction. CMAJ. 2008;179(9):909–915. doi: 10.1503/cmaj.080749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krumholz HM, Anderson JL, Bachelder BL, et al. American College of Cardiology/American Heart Association Task Force on Performance Measures; American Academy of Family Physicians; American College of Emergency Physicians; American Association of Cardiovascular and Pulmonary Rehabilitation; Society for Cardiovascular Angiography and Interventions; Society of Hospital Medicine. ACC/AHA 2008 performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Performance Measures for ST-Elevation and Non-ST-Elevation Myocardial Infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine. Circulation. 2008;118(24):2596–2648. doi: 10.1161/CIRCULATIONAHA.108.191099. [DOI] [PubMed] [Google Scholar]
- 20.Weller I, Wai EK, Jaglal S, Kreder HJ. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005;87(3):361–366. doi: 10.1302/0301-620x.87b3.15300. [DOI] [PubMed] [Google Scholar]
- 21.Morrison RS, Chassin MR, Siu AL. The medical consultant’s role in caring for patients with hip fracture. Ann Intern Med. 1998;128(12, pt 1):1010–1020. doi: 10.7326/0003-4819-128-12_part_1-199806150-00010. [DOI] [PubMed] [Google Scholar]
- 22.Ayanian JZ, Landrum MB, Guadagnoli E, Gaccione P. Specialty of ambulatory care physicians and mortality among elderly patients after myocardial infarction. N Engl J Med. 2002;347(21):1678–1686. doi: 10.1056/NEJMsa020080. [DOI] [PubMed] [Google Scholar]
- 23.Lee DS, Stukel TA, Austin PC, et al. Improved outcomes with early collaborative care of ambulatory heart failure patients discharged from the emergency department. Circulation. 2010;122(18):1806–1814. doi: 10.1161/CIRCULATIONAHA.110.940262. [DOI] [PubMed] [Google Scholar]
- 24.Tu JV, Austin PC, Chan BT. Relationship between annual volume of patients treated by admitting physician and mortality after acute myocardial infarction. JAMA. 2001;285(24):3116–3122. doi: 10.1001/jama.285.24.3116. [DOI] [PubMed] [Google Scholar]
- 25.Meyerhardt JA, Catalano PJ, Schrag D, et al. Association of hospital procedure volume and outcomes in patients with colon cancer at high risk for recurrence. Ann Intern Med. 2003;139(8):649–657. doi: 10.7326/0003-4819-139-8-200310210-00008. [DOI] [PubMed] [Google Scholar]
- 26.Ross JS, Normand SL, Wang Y, et al. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med. 2010;362(12):1110–1118. doi: 10.1056/NEJMsa0907130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tourangeau AE, Doran DM, McGillis Hall L, et al. Impact of hospital nursing care on 30-day mortality for acute medical patients. J Adv Nurs. 2007;57(1):32–44. doi: 10.1111/j.1365-2648.2006.04084.x. [DOI] [PubMed] [Google Scholar]
- 28.Richards J, Brown A, Homan C. The Data Quality Study of the Canadian Discharge Abstract Database. Statistics Canada website. [Accessed February 8, 2012];2001 http://www.statcan.gc.ca/bsolc/olc-cel/olc-cel?catno=11-522-X20010016282&lang=eng.
- 29.Juurlink D, Preyra C, Croxford R, et al. Canadian Institute for Health Information Discharge Abstract Database: A Validation Study. Toronto, Ontario, Canada: Institute for Clinical Evaluative Sciences; 2006. [Google Scholar]
- 30.Tu JV, Austin PC, Walld R, Roos L, Agras J, McDonald KM. Development and validation of the Ontario Acute Myocardial Infarction Mortality Prediction Rules. J Am Coll Cardiol. 2001;37(4):992–997. doi: 10.1016/s0735-1097(01)01109-3. [DOI] [PubMed] [Google Scholar]
- 31.Skinner J. Causes and consequences of regional variations in health care. In: Pauly MV, McGuire TG, Pita Barros B, editors. Handbook of Health Economics. Vol 2. New York, NY: Elsevier; 2012. pp. 45–93. [Google Scholar]
- 32.Lin DY. Cox regression analysis of multivariate failure time data: the marginal approach. Stat Med. 1994;13(21):2233–2247. doi: 10.1002/sim.4780132105. [DOI] [PubMed] [Google Scholar]
- 33.StataCorp. Stata Statistical Software/SE: Release 11. College Station, TX: StataCorp; 2009. [Google Scholar]
- 34.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361(14):1368–1375. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 35.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346(22):1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 36.Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364(11):1037–1045. doi: 10.1056/NEJMsa1001025. [DOI] [PubMed] [Google Scholar]
- 37.Birkmeyer NJ, Goodney PP, Stukel TA, Hillner BE, Birkmeyer JD. Do cancer centers designated by the National Cancer Institute have better surgical outcomes? Cancer. 2005;103(3):435–441. doi: 10.1002/cncr.20785. [DOI] [PubMed] [Google Scholar]
- 38.Neuman MD, Archan S, Karlawish JH, Schwartz JS, Fleisher LA. The relationship between short-term mortality and quality of care for hip fracture: a meta-analysis of clinical pathways for hip fracture. J Am Geriatr Soc. 2009;57(11):2046–2054. doi: 10.1111/j.1532-5415.2009.02492.x. [DOI] [PubMed] [Google Scholar]
- 39.Joynt KE, Orav EJ, Jha AK. The association between hospital volume and processes, outcomes, and costs of care for congestive heart failure. Ann Intern Med. 2011;154(2):94–102. doi: 10.1059/0003-4819-154-2-201101180-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291(11):1358–1367. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 41.Organisation for Economic Co-operation and Development (OECD) OECD Health Data 2011. OECD website. [Accessed January 3, 2012];2011 Jun; http://www.oecd.org/document/30/0,3746,en_2649_37407_12968734_1_1_1_37407,00.html.
- 42.Alter DA, Stukel TA, Newman A. Proliferation of cardiac technology in Canada: a challenge to the sustainability of Medicare. Circulation. 2006;113(3):380–387. doi: 10.1161/CIRCULATIONAHA.105.560466. [DOI] [PubMed] [Google Scholar]
- 43.Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113(3):374–379. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ayanian JZ. Rising rates of cardiac procedures in the United States and Canada: too much of a good thing? Circulation. 2006;113(3):333–335. doi: 10.1161/CIRCULATIONAHA.105.598789. [DOI] [PubMed] [Google Scholar]
- 45.Weinstein MC, Skinner JA. Comparative effectiveness and health care spending—implications for reform. N Engl J Med. 2010;362(5):460–465. doi: 10.1056/NEJMsb0911104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fisher E, Skinner J. Comment on Silber et al.: Aggressive treatment styles and surgical outcomes. Health Serv Res. 2010;45(6, pt 2):1893–1902. 1908–1911. doi: 10.1111/j.1475-6773.2010.01186.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Countries. World Health Organization website. [Accessed February 15, 2012]; http://www.who.int/countries/en/.
- 48.Austin PC, Tu JV. Comparing clinical data with administrative data for producing acute myocardial infarction report cards. J Royal Stat Soc A. 2006;169(1):115–126. [Google Scholar]
- 49.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113(13):1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 50.Skinner J, Staiger D, Fisher ES. Looking back, moving forward. N Engl J Med. 2010;362(7):569–574. doi: 10.1056/NEJMp1000448. [DOI] [PubMed] [Google Scholar]
- 51.Bach PB. A map to bad policy—hospital efficiency measures in the Dartmouth Atlas. N Engl J Med. 2010;362(7):569–574. doi: 10.1056/NEJMp0909947. [DOI] [PMC free article] [PubMed] [Google Scholar]