Abstract
Objective
Families and other surrogate decision-makers for chronically critically ill patients often lack information about patient prognosis or options for care. This study describes an approach to develop and validate a printed information brochure about chronic critical illness aimed at improving comprehension of the disease process and outcomes for patients’ families and other surrogate decision-makers.
Design
Investigators reviewed existing literature to identify key domains of informational needs. Content of these domains was incorporated in a draft brochure that included graphics and a glossary of terms. Clinical sensibility, balance, and emotional sensitivity of the draft brochure were tested in a series of evaluations by cohorts of experienced clinicians (n=49) and clinical content experts (n=8), with revisions after each review. Cognitive testing of the brochure was performed through interviews of 10 representative family members of chronically critically ill patients with quantitative and qualitative analysis of responses.
Measurements and Main Results
Clinical sensibility and balance were rated in the two most favorable categories on a 5-point scale by more than two thirds of clinicians and content experts. After review, family members described the brochure as clear and readable and recommended that the brochure be delivered to family members by clinicians, followed by a discussion of its contents. They indicated that the glossary was useful and recommended supplementation by additional lists of local resources. After reading the brochure, their prognostic estimates became more consistent with actual outcomes.
Conclusions
We have developed and validated a printed information brochure that may improve family comprehension of chronic critical illness and its outcomes. The structured process that is described can serve as a template for the development of other information aids for use with seriously ill populations.
Keywords: critically ill, mechanical ventilation, communication, information sharing, tracheostomies, validation studies
Introduction
Chronic critical illness is a devastating syndrome of prolonged dependence on mechanical ventilation and other intensive care therapies [1]. The chronically critically ill are a large and growing population that is estimated to exceed 100,000 at any given time in the US [2, 3]. Due to the patients’ prolonged institutional care needs and high mortality rates, families face especially difficult decisions and shoulder heavy emotional, financial, and practical burdens. Previous research has documented opportunities to improve quality of communication and informed decision-making experienced by these families [4]. For example, 80% and 93% of families in one study reported receiving no information about expected functional status at hospital discharge and prognosis for 1-year survival, respectively [5]. Over 80% had not discussed any care options other than continuing intensive care therapies. Another recent study found that surrogates’ expectations of outcomes for patients on prolonged mechanical ventilation were high, inaccurate, and discordant with those of the physicians, who rarely discussed these outcomes with the surrogates [6].
High-quality evidence has established the effectiveness of printed informational materials for educating families about critical illness and intensive care therapies. Such materials can improve knowledge relevant to treatment decisions, align expectations more closely with medical realities, encourage direct communication with the clinical team, reduce decisional conflict, and help families participate in care planning [7-9]. In one study, a proactive communication strategy including a protocol-guided family meeting with the physician and a brochure on bereavement for relatives of patients dying in the ICU resulted in significant benefits for family psychological adjustment [10]. Although professional societies, collaborative groups, and individual institutions or ICUs have developed printed materials for families on a range of ICU topics, none addressed the needs of patients and families facing chronic critical illness.
To address this need, we used a structured process to develop, validate, and test a novel informational brochure about chronic critical illness for families and other surrogate decision-makers of patients.
Materials and Methods
Content
We initially defined the content for the chronic critical illness brochure based on review of literature relating to informational needs of families of patients with acute and chronic critical illness, including qualitative research by our group. Chronically critically ill patients, families of patients, and professional caregivers for these patients (n=25) who participated in preliminary focus group meetings and structured in-depth interviews agreed on the importance of information in the following domains: nature of the patient’s illness and treatments; prognosis for outcomes including ventilator independence, function and life quality; impact of treatment on patient experience, including symptom burden; potential complications of treatment; expected care needs after hospitalization; and alternatives to continuation of treatment. A subsequent structured interview study of 100 family decision-makers for chronically critically ill patients confirmed the importance of information on items within these domains and showed that this information was not consistently communicated by clinicians [5].
Presentation
Three investigators (JN, SC, MD), as members of the SCCM Patient and Family Support Committee, incorporated content from these domains in an initial draft of the brochure. To choose an appropriate format, we reviewed ICU family brochures about acute critical illness that were shown to be effective in previous research and others prepared by professional societies and large-scale ICU collaboratives that were not formally evaluated. We also referred to recommendations and references addressing appropriate presentation of health-related information for lay readers including those with limited health literacy [11, 12]. We selected a question-and-answer format for the brochure, covering the topics listed in Table 1. To promote ease of reading and retention, we limited the text on each topic to a single paragraph and targeted active rather than passive sentences of less than or equal to 20 words. The brochure explicitly encourages families to discuss issues directly with the ICU clinicians. We included a professionally-drawn graphic showing a patient receiving mechanical ventilation via tracheotomy and a glossary explaining terms that families of critically ill patients might hear, such as “endotracheal tube,” “ventilator/respirator,” and “weaning.”
Table 1.
Topics Addressed in Informational Brochure on Chronic Critical Illness
| What is chronic critical illness? |
| What treatment is available for chronic critical illness? |
| Do chronically critically ill patients regain the ability to breathe on their own, without a breathing machine? |
| What does it feel like to be chronically critically ill? |
| Can patients with chronic critical illness live on their own? |
| What is the experience like for families? |
| Is chronic critical illness a serious condition? |
| What is a tracheotomy? |
| What are the options? |
Expert Evaluation of Clinical Sensibility, Balance, and Emotional Sensitivity
Utilizing cohorts of clinicians and clinical experts, we tested the draft brochure for clinical sensibility (material is appropriate for the condition of chronic critical illness and adapted to typical settings: clarity, face validity, content validity, and utility) [13, 14]; balance (in presentation of outcomes and options) [8]; and emotional sensitivity (material is sensitive to distress of family, compassionate). The clinician cohort (n=49) included physicians and professionals from other disciplines who care for chronically critically ill patients in long-term acute care hospitals. We distributed a 7-item questionnaire addressing clinical sensibility and emotional sensitivity along with the draft brochure to clinicians attending an educational conference sponsored by the National Association of Long-Term Hospitals. They provided ratings on a 5-point scale (not at all, a little bit, somewhat, quite a bit, very much) for each of the items, and they also provided written feedback to open-ended questions about the brochure. We used the results of this evaluation to revise the brochure and then sought input from the Patient/Family Support Committee of the SCCM, which has developed a series of brochures to educate patients and families about critical care. After incorporating that feedback in further revisions, we distributed the brochure to a national panel of 6 physicians and 2 doctorally-prepared nurses with research and clinical expertise in chronic critical illness and communication, along with the same clinical sensibility questionnaire completed by the clinicians and additional questions focusing specifically on balance in presentation of treatment options.
Cognitive Testing with Target Audience
We performed cognitive testing of the revised brochure to ensure that it communicated information in a way that is accessible to persons with a range of education, and sensitive to cultural concerns. Subjects were adult (>21 years old), English-speaking, primary surrogate decision-makers for adult chronically critically ill patients. We recruited subjects for the study by a process of systematic patient screening in the University of North Carolina Hospitals Medical ICU during weeks when specialized personnel were available to perform the cognitive testing. We screened consecutive patients for inclusion (adult patients receiving mechanical ventilation for at least 10 days who were being considered for a tracheostomy) and exclusion criteria (chronic neuromuscular disease, prolonged mechanical ventilation prior to ICU admission, and previous tracheotomy). We identified surrogate decision-makers for patients by speaking with the ICU physician, and permission was requested to approach for consent. Subjects were not enrolled if they were not available to attend interviews at the hospital or if they refused consent.
A trained research assistant met with each subject to obtain demographic information and to assess the subject’s understanding of the patient’s prognosis for ventilator liberation, short-term survival, long-term survival, and functional recovery. For this assessment, we used four visual analogue scales, one for each outcome. On each scale, the left pole of a 100 mm line corresponded to certainty of a poor prognosis for the specified outcome and the right pole to certainty of a good prognosis, and the subject was asked to mark the point on this line that best reflected the subject’s expectation of the prognosis. Subjects also completed questionnaires including the Hospital Anxiety and Depression Scale (HADS) [15] to measure symptoms of anxiety and depression, and the Quality of Communication scale. The HADS consists of 2 subscales (anxiety and depression), each containing 7 items scored from 0 (lowest symptom) to 3 (highest level); a subscale score ≥ 11 is suggestive of anxiety or depressive disorders [15]. The Quality of Communication scale is a validated instrument that consists of a series of questions evaluating the quality of communication between clinician teams and family surrogates [16]. Our subjects rated 10 items describing aspects of clinician communication on a scale from 0 (“the very worst I could imagine”) to 10 (“the very best I can imagine”).
Following the baseline interviews, a trained investigator (MV) met with each subject in an interview that was digitally recorded. A copy of the brochure was given to the subject who was given time to read and review it. During this review, the investigator used cognitive response and “think-aloud” techniques [17-19] to test content and language for comprehensibility and clarity. Probing questions relating to how well the brochure held the subject’s attention were included. Each subject was then asked to explain content of the brochure in his or her own words, and respond to questions about specific aspects of content. Some of the questions were in a true-false format, and others were open ended. After interviewing half of the cohort, information from the interviews was incorporated in a revised brochure, which was then retested using the same technique with the remaining subjects.
These research protocols were reviewed and approved by the Institutional Review Boards at Mount Sinai School of Medicine and the University of North Carolina and by the Office of Human Subjects Research at the NIH Clinical Center. A waiver of consent was granted for clinician testing as the research presented minimal risk to subjects, and informed written consent was obtained for participation by surrogate decision-makers in the cognitive testing.
Analysis
Descriptive statistics were used to summarize patient and surrogate characteristics and quantitative aspects of the evaluative process. Results are expressed as mean ± SD or median (IQR) for continuous variables and n (%) for categorical variables. Analyses were performed using Stata 11.0.
Qualitative Analysis
For qualitative analysis of the cognitive response interviews, a deductive and inductive process was used to develop a coding scheme. Before data collection, a provisional coding scheme was created from the conceptual framework, the list of research questions, and key variables. This scheme was revised and expanded based upon review and coding of the interview records. The cognitive response interviews were transcribed verbatim and coded by an investigator (MV). Beside the coded responses, categories or labels were generated and a list of themes developed. The themes were then reviewed and slightly more abstract categories were attributed to several responses or observations. The responses were then put into the appropriate designated qualitative category.
Results
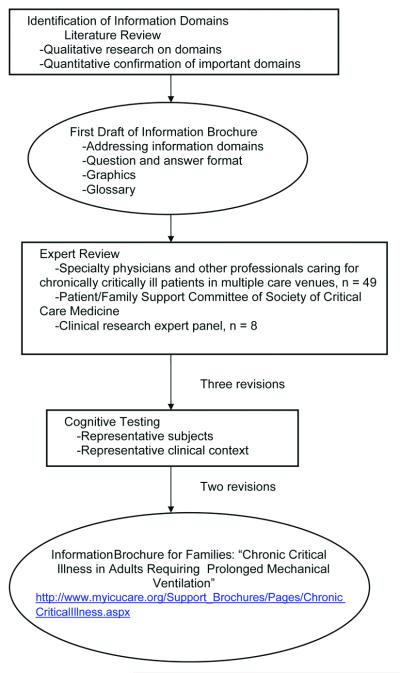
The steps in the iterative process for the development and evaluation of the brochure about chronic critical illness are summarized in Figure 1.
Figure 1.
Iterative process for development of an informational brochure for families of chronically critically ill patients.
Evaluation of Brochure by Clinicians and Clinical Experts
Results of testing with the clinicians and clinical expert panel are shown in Table 2. The response rate for the clinician cohort (n=49) was 100%. More than two-thirds of respondents rated all items in the brochure in the two most favorable categories on the 5-point clinical sensibility scale. Proportions of such ratings exceeded 80% for 5 of 7 items. Across all sensibility and balance items, the expert panel (n=8) reviewing the revised brochure gave high ratings.
Table 2.
Clinical Sensibility of Informational Brochure on Chronic Critical Illness
| Item | Mean ± [scap]sd[r] Scorea | |
|---|---|---|
| NALTHb | Expert Panelc | |
| Clear | 4.3 ± 0.7 | 4.4 ± 0.5 |
| Understandable to families | 3.8 ± 0.9 | 4.1 ± 0.4 |
| Sensitive and compassionate | 4.4 ± 0.8 | 4.6 ± 0.5 |
| Includes important information | 4.4 ± 0.7 | 4.9 ± 0.4 |
| Does not omit important information | 3.5 ± 1.2 | 4.1 ± 0.4 |
| Does not include unimportant information |
4.4 ± 1.0 | 4.9 ± 0.4 |
| Helps prepare families for decisions | 4.2 ± 0.9 | 4.2 ± 0.7 |
Likert scale from 1 to 5 with 5 being the optimal rating for the item
NALTH = 49 long-term hospital health professionals attending an educational conference of the National Association for Long-Term Hospitals
Expert Panel = 8 clinical researchers (physicians or doctorally-prepared nurses) with expertise in chronic critical illness and/or communication in the ICU. This panel reviewed a version of the brochure that incorporated results of review by the NALTH professionals.
Responses from Family Members
Ten surrogate decision-makers for 9 chronically critically patients participated in the cognitive testing. All participants were family members of the patients, and two shared decision-making responsibilities for one patient. Characteristics of patient and family subjects are shown in Table 3. The cohort represented a range of family relationships and sociodemographic characteristics. Symptoms of anxiety and depression were prevalent in this group, with 38% having HADS subscale scores suggestive of anxiety and 25% having subscale scores suggestive of depression.
Table 3.
Characteristics of Patients and Surrogate Decision-Makers
| Patient Characteristics (n = 9) | Mean ± [scap]sd[r] or n (%) |
|---|---|
| Age | 56 ± 21 |
| Male | 4 (44) |
| Race | |
| White | 4 (44) |
| African American | 5 (56) |
| Ventilator days | |
| At study enrollment | 19 ± 7 |
| Total during hospitalization | 31 ± 30 |
| Advance care planning at enrollment | |
| Any advance directive (including CPR preference) | |
| No documentation of advance directive | 9 (100) |
| Family Meeting with ICU team before enrollment | 2 (22) |
| Alive at ICU discharge | 5 (56) |
| Receiving mechanical ventilation at hospital discharge | |
| Complete ventilator dependence | 2 |
| Nocturnal ventilation | 3 |
| Total | 5 (56) |
| Hospital Disposition | |
| Died | 4 (44) |
| Home | 1(20) |
| Rehabilitation Hospital | 1 (20) |
| Long-term Acute Care Hospital | 3 (40) |
| Surrogate characteristics (n = 8)a | |
| Relationship of surrogate to patient | |
| Spouse | 4 (50) |
| Parent | 1 (12) |
| Child | 1 (12) |
| Other | 2 (25) |
| Female | 6 (75) |
| Race | |
| White | 4 (50) |
| African-American | 4 (50) |
| Occupation | |
| Employed | 6 (75) |
| Retired | 1 (12) |
| Unable to work due to health problems | 1 (12) |
| Income | |
| <15,000 | 0 |
| 15-34,000 | 1 (12) |
| 34-50,000 | 0 |
| >50,000 | 3 (38) |
| Prefer not to answer | 4 (50) |
| Religion | |
| Catholic | 1 (12) |
| Protestant | 5 (63) |
| Other | 2 (25) |
| Education | |
| High school graduate | 4 (50) |
| Some college | 1 (12) |
| College graduate | 3 (38) |
Two family participants did not provide demographic information.
Across all questions in the Quality of Communication Scale, communication by the ICU team was rated on average as 7.4 ± 1.2, with a score of 10 representing the best quality. Communication of prognosis was rated 7.6 ± 3.3, with one subject indicating that there had been no communication of prognosis. Before reading the brochure, 88% (7 of 9) family subjects responded on visual analog scales that the patient was likely to survive for one year, and 63% (5 of 7) expected the patient would return to prior levels of function. After reading the brochure, no subject marked as “true” the statement that “most patients with chronic critical illness will survive more than six months” and 89% recognized that most chronically critically ill patients would not recover their baseline function (Table 4).
Table 4.
Surrogate Decision-Makers Responses to “True” or “False” Questions about Brochure Information Following Review (n = 9)a
| N (%) | True | False |
|---|---|---|
| In time, all patients with chronic critical illness are able to regain the ability to breathe on their own without the help of a ventilator |
1 (11) | 8 (89)b |
| Some patients with chronic critical illness feel distressed by pain. | 8 (89)b | -- |
| Some patients with chronic critical illness feel frustrated about being unable to talk. | 8 (89)b | 1 (11) |
| In time, most patients with chronic critical illness are able to function as well as before their illness | 1 (11) | 8 (89)b |
| In time, most patients with chronic critical illness will be able to live on their own | 2 (23) | 6 (67)b |
| Most patients with chronic critical illness will survive more than six months | -- | 6 (67)b |
| When a patient has chronic critical illness and is dependent on a breathing machine, they have the option to refuse further support from the breathing machine. |
6 (67)b | -- |
One participant did not answer these items.
Correct responses
Qualitative Results
Families of patients in our interviews identified four primary themes that they considered important in their evaluation of the information brochure for chronic critical illness: value of information, delivery of the brochure, medical glossary, and available resources.
Value of Information
In all of the interviews, respondents found the information in the brochure to be educational and detail oriented. Several commented on the usefulness of reading candid information reflective of their situation. As one family member said, “I think it is very enlightening. It gives you everything you need to know about the person in chronic critical illness. And my husband is that stage.” Others agreed and thought the information would be helpful in dealing with the health care team. This was particularly true for those who had not been in an ICU situation before. According to one family member, “It would have helped me make decisions that I didn’t think were up to me. It helped me learn about chronic critical illness, what to expect when he gets off the vent[ilator]…[and] who can help you. I didn’t know we had a social worker until another family member told me….this is the first time I’ve been through this.”
Respondents reported that the information was written at a level that was clear for a range of educational backgrounds. Several families were relieved to have the information, but one respondent was distressed by the information on poor outcomes. She talked about the need to balance scientific language with some compassion: “I do [think it is coming off too strong]. I mean it is good. I guess it makes me wonder if something else is going on….I mean it’s good, it just makes me wonder if she is not going to be here much longer.”
Delivery of Brochure
Of particular importance was the timing and method of delivery of the information brochure. Respondents were divided on whether or not it made a difference if a doctor or nurse handed them the brochure. Both were viewed as credible and involved in patient care. However, respondents felt strongly that the brochure should be hand delivered to the family before meeting with the health care team. What was important was giving families the information so they could have a framework for talking to doctors. One respondent explained, “[The brochures] should be given... I think for any family that is going through this… it should be automatic….whatever doctor who is in charge of that particular situation should say, ‘Mrs. X, we understand your husband is going through, is going to be in the ICU with us. He is on a ventilator. I would like for you, if you are comfortable, and when you are comfortable, here’s a brochure explaining what he is undergoing and some steps we may have moving [him] towards and give it to him.’ I mean if you are going to the trouble to make this, it shouldn’t be something just sitting around in the waiting room.”
Respondents also talked about the importance of having a small, portable reference document. They liked being able to have the information at their fingertips. It was also mentioned that the smaller size made the information appear more accessible than a larger, denser, “overwhelming” document.
Medical Glossary
During the interviews, respondents received a medical glossary as an addition to the informational brochure. Overwhelmingly, respondents talked about the glossary as a useful reference and a helpful resource for family members. As one respondent said, “Now, this gives the definitions of all these words? When you have something that gives you the definitions like in school, you have a real sense of what it is. So if this gives you the definitions…this would be very helpful.” Others talked about the importance of making the glossary a supplement to the brochure and keeping the two documents together in order to increase the likelihood families would receive both documents. It would also assure that the information in each reinforced the other: “If those words are going to help you with whatever, I would keep them all together.”
Available Resources
One of the themes that emerged was the need for more information about local resources and support. Respondents talked about their desire to get as much information as possible, particularly about additional resources for the patient in the ICU and for the family. What emerged from the interviews was a tendency for family members to neglect themselves during this process. Respondents talked about the importance of providing support for the families, from a resource list of places for overnight accommodations to rehabilitation options and facilities.
The finished brochure is available through the Society of Critical Care Medicine at http://www.myicucare.org/Support_Brochures/Pages/ChronicCriticalIllness.aspx.
Discussion
The use of printed materials (e.g., brochures, booklet, leaflets) is an evidence-based strategy to help meet the informational needs of ICU families, improve their psychological well-being, and assist them in surrogate decision-making for critically ill patients. This strategy is both practical and relatively inexpensive to implement. However, studies establishing the value of these materials have not provided a detailed description of methods used to develop the materials under study. In this report we set forth each step of a structured process for developing a brochure for families of patients with chronic critical illness. We summarize the criteria and sources used to define the brochure’s content, considerations that guided drafting and formatting, and testing we conducted to confirm the clinical sensibility, sensitivity, and balance of our brochure as well as its accessibility for readers who are representative of the target audience. This description is intended to contribute methodological guidance to development of printed informational materials that are valid and effective for educating ICU families about a range of topics related to critical illness and intensive care treatment.
Several prior reports described preparation of ICU discharge materials for patients and families. The process involved literature review, patient and family interviews [20], and meetings with local experts in focus groups or panels [21]. We used a comprehensive, iterative process in which these methods were supplemented by review by national groups of clinical and research experts from multiple treatment venues, and formal cognitive testing in subjects who were members of the target audience and who reviewed and evaluated the brochure during the time of their loved one’s critical illness. By involving both clinicians and families, we include the key stakeholders in the care and outcomes of the patients. This approach supports a shared decision-making model in that the information is accurate from a medical standpoint yet comprehensible for surrogate decision-makers and other family members. We believe these additional steps enhanced the validity and potential effectiveness of our brochure.
The goals of sharing information with families, in print and in family meetings, include helping families anticipate and plan for the financial and supportive caregiving needs of the patient, helping families cope emotionally and spiritually with adverse outcomes, and enhancing informed decision-making about important treatment choices. After reading the brochure we developed on chronic critical illness, families appeared to have better comprehension of this syndrome and typical outcomes including poor long-term survival and functional dependence. Disagreement about prognosis among clinicians increases as critical illness becomes prolonged [22], and uncertainty regarding long-term outcomes may be even greater since ICU clinicians do not usually follow chronically critically ill patients beyond hospitalization. Therefore chronic critical illness presents informational needs that can be greater than in the acute phase of critical illness [4-6, 9].
Families indicated that an informational brochure can be valuable but is not a substitute for personal communication with the care team. In fact, it may be that the main value of printed materials in past studies was the encouragement they provided to families to seek opportunities to meet with the ICU team for mutual exchange of information. An independent advantage of such materials is that they can be reviewed at a time when the family feels best able to concentrate on the information, and can be re-read if the information is forgotten, as commonly occurs with families experiencing depression and anxiety when a loved one is critically ill. Written information and the comprehension it promotes may actually assist families to cope with psychological distress [9]. Effective printed materials may also help to focus families on key issues so that they are better prepared for a face-to-face meeting with ICU clinicians; this preparation, in turn, can save time for busy clinicians and assist them to achieve the meeting’s goals in the most efficient way.
Limitations of the cognitive testing of our brochure are that family subjects were related to patients receiving care in a single intensive care unit. All were Christian and none was Hispanic. However, these subjects did represent diverse educational and economic backgrounds. They also exhibited a high degree of symptoms of anxiety and depression, typical of families of critically ill patients [10, 23]. In addition, development of the brochure involved review and feedback from national groups of clinical and research experts. Although the sample of family subjects was small, no new themes emerged in 3 successive interviews before we completed that phase of the research. We acknowledge that the brochure itself can only describe general outcomes for chronically critically ill patients. Patient- and family-specific information must be shared in a knowledgeable, skillful and compassionate way by the responsible clinicians. Such communication should involve not only delivery of information but listening and discussion about the patient’s values, goals, and preferences, and the family’s needs for support [5, 6]. This brochure is an information resource, but not a decision aid designed to support or inform a specific set of treatment choices.
Conclusion
Existing evidence is clear that many ICU families lack information that could assist them in making appropriate decisions as surrogates and in coping with their own psychological distress when a loved one is critically ill. Brochures, booklets, leaflets and other printed materials are practical and relatively inexpensive tools to help meet the informational needs of patients and families in the ICU. Their value as an adjunctive strategy for communication has been demonstrated in well-conducted randomized, controlled trials. Information aids should, however, be rigorously developed to ensure that content is sufficient and appropriate and that format is clear and accessible. We have developed and validated an informational brochure for family and other surrogate decision-makers of patients with chronic critical illness. For teams wishing to develop new materials, our methodologic framework can provide guidance on approaches to maximize the effectiveness of the validation effort and its product.
Acknowledgements
The authors would like to acknowledge the Patient and Family Support Committee of the Society of Critical Care Medicine as well as Meg Hassenpflug, MS, RD, FCCM and members of National Association for Long Term Hospitals for their thorough review and contributions to the information brochure. This work was funded by the Department of Bioethics, NIH Clinical Center.
Funding: Department of Bioethics, NIH Clinical Center
Footnotes
The authors have not disclosed any potential conflicts of interest.
Disclaimer: The views expressed here are those of the authors and do not necessarily reflect the policies of the US Department of Health and Human Services or the National Institutes of Health.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Shannon S. Carson, University of North Carolina.
Maihan Vu, University of North Carolina.
Marion Danis, Department of Bioethics, NIH Clinical Center.
Sharon L. Camhi, University of Pittsburgh and Pittsburgh VA Healthcare System.
Leslie P. Scheunemann, University of North Carolina.
Christopher E. Cox, Duke University.
Laura C. Hanson, University of North Carolina.
Judith E. Nelson, Mount Sinai School of Medicine.
References
- 1.Nelson J, Cox C, Hope A, Carson S. Chronic Critical Illness. Am J Resp Crit Care Med. 2010;182(4):446. doi: 10.1164/rccm.201002-0210CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cox C, Carson S, Holmes G, Howard A, Carey T. Increase in tracheostomy for prolonged mechanical ventilation in North Carolina, 1993-2002. Crit Care Med. 2004;32(11):2219. doi: 10.1097/01.ccm.0000145232.46143.40. [DOI] [PubMed] [Google Scholar]
- 3.Zilberberg MD, de Wit M, Pirone JR, Shorr AF. Growth in adult prolonged acute mechanical ventilation: implications for healthcare delivery. Crit Care Med. 2008;36(5):1451–1455. doi: 10.1097/CCM.0b013e3181691a49. [DOI] [PubMed] [Google Scholar]
- 4.Nelson J, Kinjo K, Meier D, Ahmad K, Morrison R. When critical illness becomes chronic: informational needs of patients and families. J Crit Care. 2005;20(1):79–89. doi: 10.1016/j.jcrc.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Nelson J, Mercado A, Camhi S, Tandon N, Wallenstein S, August G, Morrison R. Communication about chronic critical illness. Arch Int Med. 2007;167(22):2509. doi: 10.1001/archinte.167.22.2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cox C, Martinu T, Sathy S, Clay A, Chia J, Gray A, Olsen M, Govert J, Carson S, Tulsky J. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37(11):2888. doi: 10.1097/CCM.0b013e3181ab86ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barry M. Health decision aids to facilitate shared decision making in office practice. Ann Intern Med. 2002;136(2):127. doi: 10.7326/0003-4819-136-2-200201150-00010. [DOI] [PubMed] [Google Scholar]
- 8.O’Connor A, Stacey D, Entwistle V. Decision aids for people facing health treatment or screening decisions [update of Cochrane Database Syst Rev 2001;(3): CD001431] Cochrane Database Syst Rev. 2003;2 doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- 9.Azoulay E, Pochard F, Chevret S, Jourdain M, Bornstain C, Wernet A, Cattaneo I, Annane D, Brun F, Bollaert P. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients. A multicenter, prospective, randomized, controlled trial. Am J Resp Crit Care Med. 2002;165(4):438. doi: 10.1164/ajrccm.165.4.200108-006oc. [DOI] [PubMed] [Google Scholar]
- 10.Lautrette A, Darmon M, Megarbane B, Joly L, Chevret S, Adrie C, Barnoud D, Bleichner G, Bruel C, Choukroun G. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J of Med. 2007;356(5):469. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 11.Weiss B, Coyne C, Michielutte R, Davis T, Meade C, Doak L, Doak C, Brown P, Askow E, Mettger W. Communicating with patients who have limited literacy skills: Report of the National Work Group on Literacy and Health. J Fam Prac. 1998;46(2):168–176. [PubMed] [Google Scholar]
- 12.Organizations JCoAoHC . Accreditation manual for hospitals. Joint Commission on Accreditation of Health Care Organizations; Chicago, Ill: 1996. Patient and Family Education. [Google Scholar]
- 13.Feinstein A. Clinimetrics. Yale University Press; New Haven, Connecticut: 1987. Clinical sensibility; pp. 141–165. [Google Scholar]
- 14.Feinstein AR, Josephy BR, Wells CK. Scientific and clinical problems in indexes of functional disability. Ann Intern Med. 1986;105(3):413. doi: 10.7326/0003-4819-105-3-413. [DOI] [PubMed] [Google Scholar]
- 15.Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 16.Stapleton R, Engelberg R, Wenrich M, Goss C, Curtis J. Clinician statements and family satisfaction with family conferences in the intensive care unit. Crit Care Med. 2006;34(6):1679. doi: 10.1097/01.CCM.0000218409.58256.AA. [DOI] [PubMed] [Google Scholar]
- 17.Jobe J, Mingay D. Cognition and survey measurement: History and overview. Applied Cognitive Psychology. 1991;5(3):175–192. [Google Scholar]
- 18.Jobe J, Tourangeau R, Smith A. Contributions of survey research to the understanding of memory. Applied Cognitive Psychology. 1993;7(7):567–584. [Google Scholar]
- 19.Willis G, Royston P, Bercini D. The use of verbal report methods in the development and testing of survey questionnaires. Applied Cognitive Psychology. 1991;5(3):251–267. [Google Scholar]
- 20.Paul F, Hendry C, Cabrelli L. Meeting patient and relatives’ information needs upon transfer from an intensive care unit: the development and evaluation of an information booklet. J Clin Nursing. 2004;13(3):396–405. doi: 10.1046/j.1365-2702.2003.00876.x. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell M, Courtney M. Improving transfer from the intensive care unit: the development, implementation and evaluation of a brochure based on Knowles’ Adult Learning Theory. Inter J Nursing Prac. 2005;11(6):257–268. doi: 10.1111/j.1440-172X.2005.00533.x. [DOI] [PubMed] [Google Scholar]
- 22.Meadow W, Pohlman A, Frain L, Ren Y, Kress JP, Teuteberg W, Hall J. Power and limitations of daily prognostications of death in the medical intensive care unit. Crit Care Med. 2011;39(3):474. doi: 10.1097/CCM.0b013e318205df9b. [DOI] [PubMed] [Google Scholar]
- 23.Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, Grassin M, Zittoun R, le Gall JR, Dhainaut JF. Symptoms of anxiety and depression in family members of intensive care unit patients: Ethical hypothesis regarding decision-making capacity. Crit Care Med. 2001;29(10):1893. doi: 10.1097/00003246-200110000-00007. [DOI] [PubMed] [Google Scholar]