Abstract
Hormonal influences during pregnancy can compromise otherwise controlled lipid levels in women with familial hypertriglyceridemia and predispose to pancreatitis leading to increased morbidity in both mother and fetus. Both cholesterol and triglyceride levels in serum increase progressively during pregnancy. The mainstay of treatment includes dietary restriction of fatty meal and lipid-lowering medications. Experiences with plasmapheresis are limited. We report two cases of hypertriglyceridemia-induced acute pancreatitis during pregnancy, which were successfully treated by plasmapheresis.
Keywords: Acute pancreatitis, plasmapheresis, pregnancy
Introduction
Hypertriglyceridemia is a known cause of acute pancreatitis (AP).[1] Hypertriglyceridemia may be primary, such as in chylomicronemia syndrome, or secondary to alcohol abuse, diabetes mellitus, estrogen use, as well as pregnancy. It is one of the important causes of acute nonbiliary pancreatitis in pregnancy.[2,3] AP rarely complicates pregnancy. It is estimated to occur in 1 in 1,000 to 1 in 12,000 pregnancies.[4] Older reviews of AP in pregnancy reported maternal and fetal mortality rates as high as 20% and 50%, respectively.[4,5] Contemporary reports documented a much improved outcome of AP in pregnancy, when the management of AP secondary to gallstones has undergone substantial changes like endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic cholecystectomy.[6,7] A single centre cohort study over 10 years has described no maternal death with fetal loss of 4.7% in 34 parturients who had AP.[7]
Cholesterol and triglyceride (TG) plasma levels physiologically increase during pregnancy. AP is the main consequence of hyperlipidemia and it can occur either during pregnancy, in the third trimester, or in the puerperium. AP might be seen in cases with familial hypertriglyceridemia at pregnancy and cases resistant to medical therapy can be treated with plasmapheresis successfully.[8,9]
We report (with the informed consent of the patients) the successful treatment of plasmapheresis in two pregnant women that had familial hypertriglyceridemia causing AP during pregnancy.
Case Reports
Case 1
A 27-year-old primipara woman, in the 5th week of gestation, was referred to the obstetrical emergency for an acute abdominal pain with vomiting and fever. The epigastric pain was continuous and radiating to the back, with aggravation in supine position and relief on crouching forward. Her sister had a history of gestational AP due to familial hypertriglyceridemia. Her physical examination was unremarkable. The TG and amylase levels were high and there was leucocytosis [Table 1]. Other biochemical parameters and the coagulation tests were normal. Magnetic resonance imaging (MRI) findings were consistent with AP. Despite medical therapy as there was no reduction in TG and on the sixth day of admission to the hospital, she was shifted to intensive care unit (ICU) for plasmapheresis. We used fresh frozen plasma (FFP) for therapeutic plasma exchange with a volume of 40 ml per kg body weight (BW) along with heparin infusion 10 U/kg/h for anticoagulation. The plasmapheresis treatment was ceased as there was a significant drop of TG after three sessions [Figure 1]. In the second week, because of the fetal loss, pregnancy was terminated. In 8 days time, with the levels of TG 278 mg/dL and cholesterol 181 mg/dL, she was discharged from the hospital. After discharge, she regularly visited the outpatient department without any complications.
Table 1.
Initial laboratory data of patients prior to the plasmapheresis treatment

Figure 1.
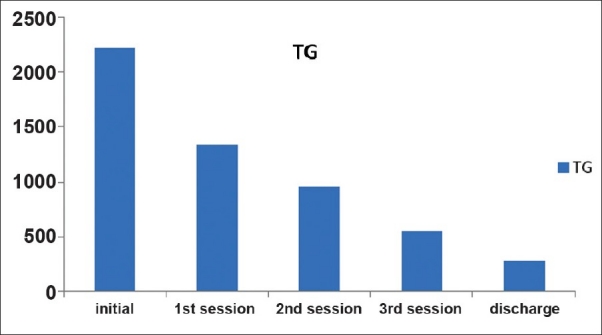
The time-course of plasmapheresis therapy of Case 1. After the first session of plasmapheresis triglycerides reduced to 1336 mg/dL, after second, to 956 mg/dL and third to 550 mg/dl. She was taken to the ward following the three sessions – plasmaphresis therapy to continue with supportive treatment. After a week on the ward, she was discharged from the hospital with the levels of TG: 278 mg/dL and cholesterol: 181 mg/dL
Case 2
A 24-year-old primigravida patient, in the 27th week of gestation, was admitted to the obstetrics and gynecology department with acute onset of nausea, vomiting, and aggravated epigastric pain. Laboratory findings, except the lipid profile, were normal [Table 1]. She was admitted to the ICU for treatment of pancreatitis. She had familial history of hypertriglyceridemia. MRI findings were consistent with AP. As there was no reduction in TG levels despite medical therapy, the treating multidisciplinary team decided to initiate plasmapheresis and eight sessions with 3 days intervals were planned. After completion of plasmapheresis sessions, the patient was sent to the ward for the continuation of supportive treatment. Within 10 days, despite to the dietary restriction of fat and administration of lipid-lowering agents, the level of TGs again increased (TG 2483 mg/dL and cholesterol 351 mg/dL) and six more sessions of plasmapheresis were planned. In all the sessions, FFP (40 ml/kg BW) and heparin (10 U/kg/h) were used. The lipid values slowly returned toward normal during the following days [Figure 2]. On the 21st day of her second admission, the patient was sent back to the obstetrics ward. She was kept on lipid-lowering dietary and drug therapy until the 34th week of gestation. Cesarean delivery was performed under spinal anesthesia in the 34th week, and the patient delivered a healthy 3100 g female infant. Her lipids became normal thereafter and she was followed up in the outpatient clinic.
Figure 2.
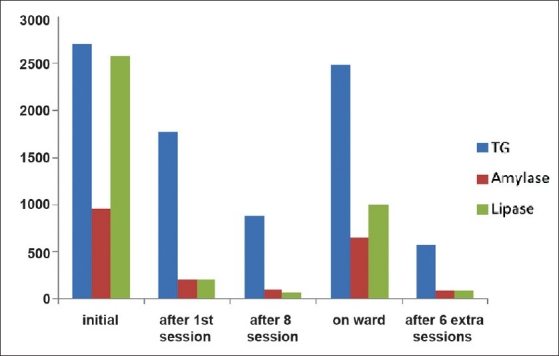
The change of lipid profile of Case 2 with plasmapheresis therapies. After the first session of plasmapheresis, triglycerides reduced to 1774 mg/dL, amylase to 208 U/L, and lipase to 208 U/L. After the 8th session, triglycerides were 880 mg/dL and she was taken to the ward with continuation of lipidlowering medical therapy. But as TG levels rose again up to 2483 mg/dL under this treatment, six more lasmapheresis sessions were arranged. After the last session, the TG decreased to 570 mg/dL and she needed no more sessions until the delivery of child on 34th gestational week
Discussion
Hypertriglyceridemia-induced pancreatitis is a serious complication of familial dyslipidemias. Hormonal influences during pregnancy can compromise otherwise controlled lipid levels in women with familial hypertriglyceridemia and predispose to pancreatitis.[10] Plasma TG increase two-fold to four-fold in pregnancy, principally in the third trimester, because of increased TG-rich lipoprotein production and decreased lipoprotein lipase activity.[11] In women with abnormal lipoprotein metabolism, this can lead to severe hypertriglyceridemia, precipitating pancreatitis.[12] General and specific therapy is available to reduce TG levels during the acute phase of pancreatitis, which may improve the outcome. Nutrition and pharmacologic therapy may be essential in preventing further attacks. Plasmapheresis is an alternative, safe, and successful treatment for the cases resistant to the medical treatment. We successfully used plasmapheresis to manage hypertriglyceridemia-induced pancreatitis during pregnancy.
Hypertriglyceridemia-induced pancreatitis during pregnancy has been reported previously.[13–15] The clinical course and treatment of pancreatitis due to hypertriglyceridemia are similar to those of pancreatitis of other causes. Family history of lipid abnormalities should be elicited, and an attempt to identify secondary causes made. A serum TG level >1,000 mg/dL is an identifiable risk factor. Reduction of TG levels to well below 1,000 mg/dL effectively prevents further episodes of pancreatitis.[16,17] The mainstay of treatment for the hypertriglyceridemia associated with pancreatitis includes dietary restriction of fat and administration of lipid-lowering agents.[1,2] To prevent AP, hospitalization for intravenous fluid therapy and plasma exchange may be required. Plasmapheresis and extracorporeal lipid elimination are therapeutic alternatives.[3,8] Plasma exchange can dramatically reduce excessive lipid levels,[18,19] as was seen in our two cases. Our second patient presented with triglyceridemia-induced pancreatitis in the 27th week of pregnancy. There was no previous history of lipid abnormality, diabetes mellitus, alcohol ingestion, or any other precipitating factor apart from family history. Plasma TG level was 2699 mg/dL at admission.
Pancreatitis in pregnancy is associated with a high maternal death and fetal loss rate. These rates are declining with earlier diagnosis of the disease.[20] Treatment in early phase is important both for the fetus and the mother's health. The commonest reasons for maternal and fetal mortality are AP itself and, very rarely, AP is associated with preeclampsia–eclampsia or HELLP syndrome.[15,21] In our first case, pregnancy had to be terminated, but in the second case the patient delivered a healthy infant. The incidence of preterm delivery and perinatal death in these patients is higher than that in the general obstetric population.[22–24] Ramin et al. demonstrated that, of pregnancies complicated with pancreatitis, 19% had AP in the first trimester, 26% in the second, 53% at more than 28 weeks gestation, and 2% postpartum.[4] One of our patients was at 5th gestational week and the other was at 27th gestational week.
The incidence of pancreatitis during pregnancy is low, but related morbidity and mortality are high. Early and prompt treatment is the key factor to successful outcome. Plasmapheresis is an alternative and safe treatment for the cases resistant to the medical therapy. The early application of plasmapheresis in parturients with hypertriglyceridemia-induced AP may improve the clinical course.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Yadav D, Pitchumoni CS. Issues in hyperlipidemic pancreatitis. J Clin Gastroenterol. 2003;36:54–62. doi: 10.1097/00004836-200301000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Neill AM, Hackett GA, Overton C, Byrne CD. Active management of acute hyperlipidaemic pancreatitis in pregnancy. J Obstet Gynaecol. 1998;18:174–5. doi: 10.1080/01443619867975. [DOI] [PubMed] [Google Scholar]
- 3.Exbrayat V, Morel J, De Filippis J, Tourne G, Jospe R, Auboyer C. Hypertriglyceridemia-induced pancreatitis in pregnancy. A case report. Ann Fr Anesth Reanim. 2007;26:677–9. doi: 10.1016/j.annfar.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Ramin KD, Ramin SM, Richey SD, Cunningham FG. Acute pancreatitis in pregnancy. Am J Obstet Gynecol. 1995;173:187–91. doi: 10.1016/0002-9378(95)90188-4. [DOI] [PubMed] [Google Scholar]
- 5.Ramin KD, Ramsey PS. Disease of the gallbladder and pancreas in pregnancy. Obstet Gynecol Clin North Am. 2001;28:571–80. doi: 10.1016/s0889-8545(05)70218-7. [DOI] [PubMed] [Google Scholar]
- 6.Swisher SG, Hunt KK, Schmit PJ, Hiyama DT, Bennion RS, Thompson JE. Management of pancreatitis complicating pregnancy. Am Surg. 1994;60:759–2. [PubMed] [Google Scholar]
- 7.Hernandez A, Petrov MS, Brooks DC, Banks PA, Ashley SW, Tavakkolizadeh A. Acute pancreatitis and pregnancy: A 10-year single center experience. J Gastrointest Surg. 2007;11:1623–7. doi: 10.1007/s11605-007-0329-2. [DOI] [PubMed] [Google Scholar]
- 8.Iskandar SB, Olive KE. Plasmapheresis as an adjuvant therapy for hypertriglyceridemia-induced pancreatitis. Am J Med Sci. 2004;328:290–4. doi: 10.1097/00000441-200411000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Perrone G, Criel C. Severe hypertriglyceridemia in pregnancy. A clinical case report. Minerva Ginecol. 1996;48:573. [PubMed] [Google Scholar]
- 10.Salameh WA, Mastrogiannis DS. Maternal hyperlipidemia in pregnancy. Clin Obstet Gynecol. 1994;37:66–77. doi: 10.1097/00003081-199403000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Musa AA Abu, Usta IM, Rechdan JB, Nassar AH. Recurrent hypertriglyceridemia-induced pancreatitis in pregnancy: A management dilemma. Pancreas. 2006;32:227–8. doi: 10.1097/01.mpa.0000202943.70708.2d. [DOI] [PubMed] [Google Scholar]
- 12.Neill AM, Hackett GA, Overton C, Byrne CD. Active management of acute hyperlipidaemic pancreatitis in pregnancy. J Obstet Gynaecol. 1998;18:174–5. doi: 10.1080/01443619867975. [DOI] [PubMed] [Google Scholar]
- 13.De Chalain TM, Michell WL, Berger GM. Hyperlipidemia, pregnancy and pancreatitis. Surg Gynecol Obstet. 1988;167:469–73. [PubMed] [Google Scholar]
- 14.Loo CC, Tan JY. Decreasing the plasma triglyceride level in hypertnglyceridemia-induced pancreatitis in pregnancy: A case report. Am J Obstet Gynecol. 2002;187:241–2. doi: 10.1067/mob.2002.122422. [DOI] [PubMed] [Google Scholar]
- 15.Bildirici I, Esinler I, Deren O, Durukan T, Kabay B, Onderoglu L. Hyperlipidemic pancreatitis during pregnancy. Acta Obstet Gynecol Scand. 2002;81:468–70. doi: 10.1034/j.1600-0412.2002.810516.x. [DOI] [PubMed] [Google Scholar]
- 16.Okura Y, Hayashi K, Shingu T, Kajiyama G, Nakashima Y, Saku K. Diagnostic evaluation of acute pancreatitis in two patients with hypertriglyceridemia. World J Gastroenterol. 2004;10:3691–5. doi: 10.3748/wjg.v10.i24.3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Athyros VG, Giouleme O, Nikolaidis NL, Vasiliadis TV, Bouloukos VI, Kontopoulos AG, et al. Long-term follow-up of patients with acute hypertriglyceridemia-induced pancreatitis. J Clin Gastroenterol. 2002;34:472–5. doi: 10.1097/00004836-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 18.Bae JH, Baek SH, Choi HS, Cho KR, Lee HL, Lee OY, et al. Acute pancreatitis due to hypertriglyceridemia: Report of 2 cases. Korean J Gastroenterol. 2005;46:475–80. [PubMed] [Google Scholar]
- 19.Ewald N, Hardt PD, Kloer HU. Treatment of hyperlipidemic acute pancreatitis with plasma exchange: A single-center experience. Curr Opin Lipidol. 2009;20:497–504. doi: 10.1097/MOL.0b013e3283319a1d. [DOI] [PubMed] [Google Scholar]
- 20.Angelini DJ. Obstetric triage revisited: Update on non-obstetric surgical conditions in pregnancy. J Midwifery Womens Health. 2003;48:111–8. doi: 10.1016/s1526-9523(02)00417-8. [DOI] [PubMed] [Google Scholar]
- 21.Sanderson SL, Ivenus PH, Wilson DE. Successful hyperlipemic pregnancy. JAMA. 1991;265:1858–60. [PubMed] [Google Scholar]
- 22.Keilson LM, Vary CP, Sprecher DL, Renfrew R. Hyperlipidemia and pancreatitis during pregnancy in two sisters with a mutation in the lipoprotein lipase gene. Ann Intern Med. 1996;124:425–8. doi: 10.7326/0003-4819-124-4-199602150-00007. [DOI] [PubMed] [Google Scholar]
- 23.Nies BM, Dreiss RJ. Hyperlipidemic pancreatitis in pregnancy: A case report and review of the literature. Am J Perinatol. 1990;7:166–9. doi: 10.1055/s-2007-999472. [DOI] [PubMed] [Google Scholar]
- 24.Economides DL, Crook D, Nicolaides KH. Hypertriglyceridemia and hypoxemia in small-for-gestational-age fetuses. Am J Obstet Gynecol. 1990;162:382–6. doi: 10.1016/0002-9378(90)90391-j. [DOI] [PubMed] [Google Scholar]


