Abstract
Background
Extreme prolongation or reduction of the QT interval predisposes patients to malignant ventricular arrhythmias and sudden cardiac death, but the association of variations in the QT interval within a reference range with mortality end points in the general population is unclear.
Methods
We included 7828 men and women from the Third National Health and Nutrition Examination Survey. Baseline QT interval was measured via standard 12-lead electrocardiographic readings. Mortality end points were assessed through December 31, 2006 (2291 deaths).
Results
After an average follow-up of 13.7 years, the association between QT interval and mortality end points was U-shaped. The multivariate-adjusted hazard ratios comparing participants at or above the 95th percentile of age-, sex-, race-, and R-R interval–corrected QT interval (≥439 milliseconds) with participants in the middle quintile (401 to <410 milliseconds) were 2.03 (95% confidence interval, 1.46-2.81) for total mortality, 2.55 (1.59-4.09) for mortality due to cardiovascular disease (CVD), 1.63 (0.96-2.75) for mortality due to coronary heart disease, and 1.65 (1.16-2.35) for non-CVD mortality. The corresponding hazard ratios comparing participants with a corrected QT interval below the fifth percentile (<377 milliseconds) with those in the middle quintile were 1.39 (95% confidence interval, 1.02-1.88) for total mortality, 1.35 (0.77-2.36) for CVD mortality, 1.02 (0.44-2.38) for coronary heart disease mortality, and 1.42 (0.97-2.08) for non-CVD mortality. Increased mortality also was observed with less extreme deviations of QT-interval duration. Similar, albeit weaker, associations also were observed with Bazett-corrected QT intervals.
Conclusion
Shortened and prolonged QT-interval durations, even within a reference range, are associated with increased mortality risk in the general population.
Abnormal prolongation and shortening of the electrocardiographic QT-interval duration, similar to those seen in hereditary forms of long and short QT syndromes, are associated with increased risk for ventricular arrhythmias and sudden cardiac death.1-5 The effect of less extreme variations in QT-interval duration on mortality, however, is
See Invited Commentary at end of article
controversial. Some studies have shown associations between smaller increases in QT-interval duration and total mortality, cardiovascular mortality, and sudden cardiac death,6-17 but these associations have not been replicated consistently in all studies.18-20 Furthermore, although a short duration of the QT interval also may be associated with increased mortality, most studies have used broad categorizations of QT-interval durations that make it difficult to estimate precisely the dose-response relationships between QT interval and mortality. The purpose of this analysis was to investigate the association between QT-interval duration and total mortality and mortality due to cardiovascular disease (CVD), coronary heart disease (CHD), and non-CVD causes in a representative sample of the general US population using flexible methods to identify potential variations in mortality risks along the full spectrum of QT-interval durations.
CME available online at www.jamaarchivescme.com and questions on page 1699
METHODS
STUDY POPULATION
We used data from the Third National Health and Nutrition Examination Survey (NHANES III), a cross-sectional study conducted from 1988 through 1994 that used a multistage, stratified, clustered probability design to select a representative sample of the civilian noninstitutionalized US population aged 2 months and older.21 Children, older adults, non-Hispanic black subjects, and Mexican American subjects were oversampled to produce more precise estimates for these groups. The present study was restricted to participants 40 years and older because 12-lead electrocardiograpic readings were performed only in this age group. Of the 8561 participants 40 years or older who had available electrocardiographic measurements, we excluded 122 participants with missing QT-interval duration or heart rate, 535 participants with QRS duration of at least 120 milliseconds, and 76 participants with missing mortality status. The final analysis was based on data from 7828 participants (3703 men and 4125 women).
DATA COLLECTION
The NHANES III included a standardized questionnaire administered in the home by a trained interviewer and a detailed physical examination at a mobile examination center. Demographics, educational level, smoking status, alcohol consumption, medical history, and medication use were assessed by interview. We defined QT-prolonging medications according to the Arizona Center for Education and Research on Therapeutics database.22 Height and weight were measured, and body mass index was calculated as weight in kilograms divided by height in meters squared. Blood pressure was measured 3 times during the in-home interview and 3 additional times during the participant’s visit to the mobile examination center. Laboratory test results included measurement of total and high-density lipoprotein cholesterol, plasma glucose, serum potassium, and serum calcium concentrations. Diabetes mellitus was defined as a fasting plasma glucose level of at least 126 mg/dL, a nonfasting plasma glucose level of at least 200 mg/dL, and/or current use of oral hypoglycemic agents or insulin (to convert glucose levels to millimoles per liter, multiply by 0.0555).
QT INTERVAL
Standard 12-lead resting electrocardiographic recordings were performed using a commercially available device (Marquette MAC 12; Marquette Medical Systems, Inc, Milwaukee, Wisconsin) with signals sampled at 250 samples per second per channel when participants visited the mobile examination centers. All electrocardiographic readings were reviewed at the Central ECG [Electrocardiogram] Laboratory, Epidemiological Cardiology Research Center, Wake Forest University, Winston-Salem, North Carolina. Recordings with technical errors, missing leads, or inadequate quality per visual inspection were excluded. Then, a representative P-QRS-T cycle was derived automatically by selective averaging using the Dalhousie ECG Analysis Program.23 The program measured the QT interval as a global interval by selective averaging of all normally conducted complexes. The global QT interval derived in this manner reduces measurement uncertainties due to small T-wave amplitudes in any individual lead. Resting heart rates and QT intervals were obtained from electrocardiographic readings.
As the primary metric for QT analysis, we used age-, race-, sex-, and R-R interval–adjusted QT-interval (QTrras) duration by means of the residual method. More specifically, we first regressed QT interval on age (continuous), race or ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, and other), sex (female or male), and R-R interval (restricted quadratic splines with knots at the 5th, 50th, and 95th percentiles to allow a more flexible and nonlinear relationship between QT and R-R intervals) as the independent covariates in the linear regression model. Then, we obtained the model residuals for each participant. Residuals represent, for each participant, the component of QT interval not explained by model regressors. Residuals are uncorrelated with the regressors and thus adjusted for them. Because the average of the residuals is 0, we rescaled the residuals by adding the mean QT interval of the overall study population to calculate the final QTrras. Parallel analyses also were performed with the Bazett heart rate–corrected QT-interval (QTb) duration.
MORTALITY END POINTS
Participants in the NHANES III were followed up for mortality through December 31, 2006.24 Vital status and cause of death assignment were based on probabilistic matching of NHANES III with the National Death Index death certificate records. Cause of death was determined based on the underlying cause listed on the death certificates. We used the International Classification of Diseases, Ninth Revision (ICD-9) for classifying deaths occurring from 1988 through 1998 and the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) for deaths occurring from 1999 through 2006. Cardiovascular disease mortality was defined as ICD-9 codes 390 to 434 and 436 to 459 or ICD-10 codes I00 to I99. Coronary heart disease mortality was defined as ICD-9 codes 410 to 414 and 429.2 or ICD-10 codes I20 to I25. Non-CVD mortality was defined as all other deaths that were not classified as CVD mortality. In addition, we excluded cases of “sudden death, unknown causes” (ICD-9 code 798 or ICD-10 code R96) from non-CVD mortality in a sensitivity analysis and found similar results (not shown).
STATISTICAL ANALYSIS
We used electrocardiographic sampling weights to account for the complex survey design of the NHANES III.21 We used Cox proportional hazards models to estimate multivariate-adjusted hazard ratios for mortality end points associated with QTrras. To provide detailed analyses of the dose-response relationship of the QTrras with mortality rate, we used 2 alternative approaches. First, we categorized QTrras into 7 categories with cutoffs at the 5th, 20th, 40th, 60th, 80th, and 95th percentiles of the weighted population QTrras distribution. In these analyses, we used the middle category as the reference category (participants between the 40th and 60th QTrras percentiles, corresponding to the middle quintile). Second, we modeled QTrras with restricted quadratic splines with knots at the 5th, 50th, and 95th percentiles of the QTrras distribution to provide a smooth yet flexible description of the dose-response relationship. In spline analyses, we used the 50th percentile of the QTrras distribution as the reference value (median).
We censored follow-up at age 90 years because mortality was high after this age and few participants contributed person-time in this age category. Models were adjusted for age; race or ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, and other); sex; R-R interval (restricted quadratic splines with knots at the 5th, 50th, and 95th percentiles); body mass index; smoking status (current, former, or never); alcohol consumption (<12 or ≥12 drinks in the past year); high school education (<12 years or ≥12 years); annual household income (<$20 000 or ≥$20 000); total and high-density lipoprotein cholesterol, serum potassium, and serum calcium levels; systolic blood pressure; use of blood pressure– lowering medication; diabetes mellitus; history of myocardial infarction; history of congestive heart failure; use of QT-prolonging medications; and use of β-blockers.
Also, we performed stratified analyses in men and women separately and sensitivity analyses excluding individuals with diabetes mellitus, myocardial infarction, or heart failure or those taking QT-prolonging medications (final sample size, 5475). All analyses were conducted using commercially available software (SUDAAN, version 10.0; Research Triangle Institute, Research Triangle Park, North Carolina).
RESULTS
The average age of study participants was 56.5 years; 45.1% of participants were male (Table 1). The mean (SD) duration was 406.1 (18.8) milliseconds for the QTrras and 429.3 (23.3) milliseconds for the QTb. The numbers of all-cause, CVD, CHD, and non-CVD deaths during follow-up were 2291, 911, 515, and 1380, respectively (Table 2).
Table 1.
Baseline Characteristics of the 7828 Study Participants
| Characteristic | Patients, %a |
|---|---|
| Age, mean (SD), y | 56.5 (12.4) |
| Male sex | 45.1 |
| Race | |
| Non-Hispanic white | 80.6 |
| Non-Hispanic black | 9.0 |
| Mexican American | 3.6 |
| High school education | 70.7 |
| Annual household income <$20 000 | 31.1 |
| Systolic blood pressure, mean (SD), mm Hg | 128.7 (18.2) |
| Total cholesterol level, mean (SD), mg/dL | 218.0 (42.1) |
| HDL cholesterol level, mean (SD), mg/dL | 51.0 (16.1) |
| BMI, mean (SD) | 27.3 (5.5) |
| Serum potassium level, mean (SD), mEq/L | 4.1 (0.3) |
| Serum calcium level, mean (SD), mg/dL | 9.2 (0.4) |
| Diabetes mellitus | 8.6 |
| Myocardial infarction | 5.2 |
| Congestive heart failure | 2.9 |
| Smoking status | |
| Current | 22.9 |
| Former | 34.7 |
| Never | 42.4 |
| Consume alcohol | 45.8 |
| Use QT-prolonging medication | 12.0 |
| Use a β-blocker | 7.9 |
| Heart rate, mean (SD), beat/min | 68.1 (11.5) |
| QT interval, mean (SD), ms | 406.1 (30.8) |
| QTrras, mean (SD), ms | 406.1 (18.8) |
| QTb, mean (SD), ms | 429.3 (23.3) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HDL, high-density lipoprotein; QTb, Bazett heart rate–corrected QT interval; QTrras, age-, race-, sex-, and R-R interval–adjusted QT interval.
SI conversion factors: To convert calcium to millimoles per liter, multiply by 0.25; cholesterol to millimoles per liter, multiply by 0.0555; and potassium to millimoles per liter, multiply by 1.
Data are expressed as percentage of patients unless otherwise indicated.
Table 2.
Number of Deaths by QTrras and QTb Percentiles
| No. of Deathsa |
|||||
|---|---|---|---|---|---|
| Percentile | Cutoff, ms | Totalb | CVD | CHD | Non-CVD |
| QTrras | |||||
| <5th | <377 | 143 | 62 | 36 | 81 |
| 5th to <20th | 377 to <391 | 323 | 129 | 74 | 194 |
| 20th to <40th | 391 to <401 | 420 | 154 | 89 | 266 |
| 40th to <60th | 401 to <410 | 429 | 170 | 99 | 259 |
| 60th to <80th | 410 to <421 | 409 | 154 | 83 | 255 |
| 80th to <95th | 421 to <439 | 373 | 149 | 80 | 224 |
| ≥95th | ≥439 | 194 | 93 | 54 | 101 |
| Total | 2291 | 911 | 515 | 1380 | |
| QTb | |||||
| <5th | <393 | 85 | 38 | 22 | 47 |
| 5th to <20th | 393 to <409 | 258 | 101 | 60 | 157 |
| 20th to <40th | 409 to <423 | 378 | 151 | 89 | 227 |
| 40th to <60th | 423 to <434 | 401 | 142 | 90 | 259 |
| 60th to <80th | 434 to <448 | 490 | 196 | 104 | 294 |
| 80th to <95th | 448 to <470 | 469 | 191 | 100 | 278 |
| ≥95th | ≥470 | 210 | 92 | 50 | 118 |
| Total | 2291 | 911 | 515 | 1380 | |
Abbreviations: CHD, coronary heart disease; CVD; cardiovascular disease; QTb, Bazett heart rate–corrected QT interval; QTrras, age-, race-, sex-, and R-R interval–corrected QT interval.
Includes follow-up though the end of the study.
Determined by summing CVD and non-CVD values.
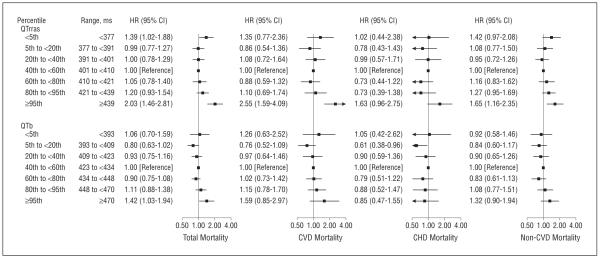
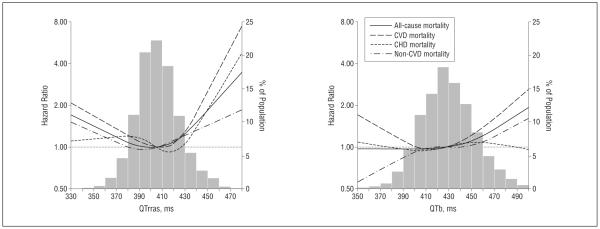
After an average follow-up of 13.7 years, the multivariate-adjusted hazard ratios comparing participants above the 95th percentile of the QTrras (≥439 milliseconds) with participants in the middle quintile (401 to <410 milliseconds) were 2.03 (95% confidence interval [CI], 1.46-2.81) for total mortality, 2.55 (1.59-4.09) for CVD mortality, 1.63 (0.96-2.75) for CHD mortality, and 1.65 (1.16-2.35) for non-CVD mortality (Figure 1). The corresponding hazard ratios comparing participants below the 5th percentile of the QTrras (<377 milliseconds) with the middle quintile were 1.39 (95% CI, 1.02-1.88) for total mortality, 1.35 (0.77-2.36) for CVD mortality, 1.02 (0.44-2.38) for CHD mortality, and 1.42 (0.97-2.08) for non-CVD mortality. Although participants with the extreme 5% highest and lowest QTrras had the highest mortality rate, other categories also were at increased risk compared with the middle quintile (Figure 1). Consistently, in the spline regression models, the risk increased progressively from the middle of the QTrras distribution with no clear threshold of risk (Figure 2).
Figure 1.
Multivariate-adjusted hazard ratios (HRs) for total mortality rate and mortality due to cardiovascular disease (CVD), coronary heart disease (CHD), and non-CVD causes. Mortality end points were associated with age-, sex-, race-, and R-R interval–corrected QT interval (QTrras) and Bazett heart rate–corrected QT interval (QTb). Models were adjusted for age; race or ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, or other); sex; R-R interval (restricted quadratic splines with knots at the 5th, 50th, and 95th percentiles); body mass index (calculated as weight in kilograms divided by height in meters squared); smoking status (current, former, or never); alcohol consumption (<12 or ≥12 drinks in the past year); high school education (<12 years or ≥12 years); annual household income (<$20 000 or ≥$20 000); levels of total and high-density lipoprotein cholesterol, serum potassium, and serum calcium; systolic blood pressure; use of blood pressure–lowering medication; diabetes mellitus; history of myocardial infarction; history of congestive heart failure; use of QT-prolonging medications; and use of β-blockers. Wald test P values for testing the association of QTrras categories with mortality end points were less than .001 for total mortality and CVD mortality, .02 for CHD mortality, and .008 for non-CVD mortality. The corresponding P values for QTb were .08, .24, .49, and .28, respectively. CI indicates confidence interval.
Figure 2.
Multivariate-adjusted hazard ratios for total mortality rate and mortality due to cardiovascular disease (CVD), coronary heart disease (CHD), and non-CVD causes. Mortality end points were associated with age-, sex-, race-, and R-R interval–adjusted QT interval (QTrras) and Bazett heart rate–corrected QT interval (QTb) using restricted quadratic splines. The horizontal dotted line indicates a hazard ratio of 1. Adjustment factors are described in Figure 1.
The U-shaped association between QT interval and mortality end points also was evident when using the QTb, although the magnitude of the association was slightly de-creased (Figures 1 and 2). The hazard ratios comparing participants with a QTb at or above the 95th percentile with those in the middle quintile were 1.42 (95% CI, 1.03-1.94) for total mortality, 1.59 (0.85-2.97) for CVD mortality, 0.85 (0.47-1.55) for CHD mortality, and 1.32 (0.90-1.94) for non-CVD mortality (Figure 1). The corresponding hazard ratios comparing participants with a QTb below the 5th percentile with those in the middle quintile were 1.06 (95% CI, 0.70-1.59) for total mortality, 1.26 (0.63-2.52) for CVD mortality, 1.05 (0.42-2.62) for CHD mortality, and 0.92 (0.58-1.46) for non-CVD mortality.
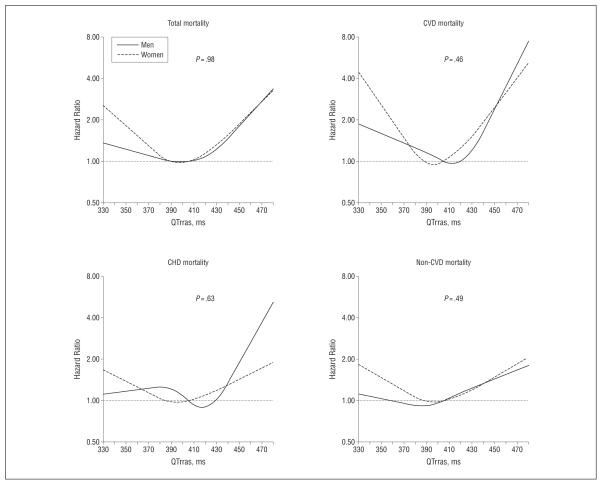
When stratified by sex, the association between the QTrras and mortality end points was similar among men and women (Figure 3). Finally, excluding participants with diabetes mellitus, myocardial infarction, or heart failure or those receiving QT-prolonging medications did not materially change the results (eFigure; http://www.archinternmed.com).
Figure 3.
Multivariate-adjusted hazard ratios of total mortality rate and mortality due to cardiovascular disease (CVD), coronary heart disease (CHD), and non-CVD causes. Mortality end points were associated with age-, sex-, race-, and R-R interval–adjusted QT interval (QTrras) using restricted quadratic splines, stratified by sex. The horizontal dotted line indicates a hazard ratio of 1. Adjustment factors are described in Figure 1. P values are for interaction.
COMMENT
In a large sample representative of the general US population, the association between QT-interval duration and all-cause, CVD, and CHD mortality was U-shaped, with increased risks at the lower and upper tails of the QT-interval distribution. Although the increase in risk was highest at the extremes of the distribution, the risk of mortality progressively increased with longer and shorter QT-interval duration compared with the population average with no clear threshold for risk change.
Population-based studies reporting associations between prolonged QT-interval duration and mortality rate have been inconsistent. Some studies7-17 have shown progressive associations of QT-interval duration with mortality rate, but other studies have shown U-shaped associations6,25 or nonsignificant associations.18-20 The categories used for evaluating the association of QT-interval duration with mortality rate in previous studies generally were wide and inconsistent across studies, making it difficult to evaluate dose-response relationships and to compare findings. Our results suggest that analyses of QT-interval duration and mortality rate need to carefully select the cut points and the reference category to avoid masking nonlinear dose-response relationships.
In experimental models, prolongation of the QT interval is associated with the occurrence of early after-depolarizations.26 Early after-depolarizations of sufficient amplitude can generate premature action potentials that lead to cardiac arrhythmias that may progress to ventricular fibrillation and sudden cardiac death.27,28 In general, longer QT intervals reflect longer ventricular action potentials, a reduction in repolarizing reserve29 that is associated with exaggerated spatial and temporal heterogeneity of electrical recovery of the ventricle. This would allow for the development of functional reentry, in which still-activated regions of ventricular myocardium reenter and reactivate regions with shorter action potentials, producing polymorphic ventricular tachycardias. The progressive association of QT-interval duration with mortality at the high end of the distribution then would reflect an increased likelihood of ventricular arrhythmias associated with increasing heterogeneity in ventricular action potential duration.
Although the literature regarding prolonged QT intervals is substantial, less is known regarding shortened QT intervals, especially at the population level. Short QT syndrome is a rare disease associated with hastened ventricular repolarization (QT intervals typically ≤320 milliseconds) and an increased risk of sudden cardiac death,3,4,18,30-32 although more recent studies33,34 have shown that genetically confirmed cases of short QT syndromemay have QT-interval durations of 320 to 360 milliseconds. Data from population-based studies regarding the risk associated with a QT interval at the low end of the distribution are limited. A small study in the Netherlands6 found no association for sudden cardiac death when comparing participants with a QTb of less than 400 vs 400 to 440 milliseconds. Similarly, a Finnish study of 10 822 participants found no association of all-cause mortality comparing participants with a QTb of less than 340 vs 360 to 449 milliseconds,18 and a study of 3596 participants in England reported no association for all-cause or cardiovascular mortality comparing participants with a QTb of less than 397 vs 410 to 422 milliseconds.25 None of these studies presented a more detailed dose-response analysis. Our findings indicate that the results of these analyses could depend on the cutoff points used to define the lower tail of the QT-interval distribution and on the QT-interval values used to define the reference category.
Similar to QT prolongation, shortening of the QT interval is not uniform in time and space in the ventricle. Thus, shortening of the QT interval is associated with exaggerated heterogeneity of repolarization in time and space. The exaggerated heterogeneity of action potential duration creates a substrate for functional reentry similar to that of long QT syndrome but with hastened recovery and reduced refractoriness in the ventricle, and arrhythmias are likely to be even more malignant in short compared with long QT syndromes.35
Traditionally, reference ranges for QT-interval duration in the general population were expressed in terms of QTb.18,30,31,36,37 The Bazett correction, however, has a strong residual correlation with heart rate and results in wider distributions compared with other adjustment methods with better control for heart rate.38 Indeed, the 2009 recommendations for the standardization and interpretation of the QT interval from the American Heart Association Electrocardiography and Arrhythmias Committee Council on Clinical Cardiology, the American College of Cardiology Foundation, and the Heart Rhythm Society recommended that linear regression functions rather than the Bazett formula be used for QT correction.39 The report further recommended that, in addition to rate, sex and age should be incorporated into QT adjustment because women and elderly individuals tend to have longer QT intervals. The report proposed a reference range for linear function–adjusted QT-interval duration from 390 to 450 milliseconds in men or 460 milliseconds in women. In the NHANES III, these values correspond to the 17th and 98th percentiles of the QTrras distribution in men and the 18th and 99th percentiles of that distribution in women. Our analysis thus indicates that QT-interval duration is associated with variations in mortality rate even within reference ranges calculated using the most recent normative standards. Moreover, our study showed that the observed associations were stronger when using the QTrras compared with the QTb, which might be explained partly by the imperfection of the Bazett correction formula.
Several limitations of this study need to be considered. The QT-interval duration was measured at a single baseline time, which may result in nondifferential measurement error because there is substantial within-individual variability. Repeated measurements of QT-interval duration are needed to reduce measurement error and to better characterize the association between QT interval and mortality rate in future studies. Causes of death were ascertained based on death certificates, and we did not have detailed adjudications of arrhythmic sudden cardiac deaths, an end point that more specifically may reflect the effect of QT-interval duration on mortality rate. Although potential misclassifications may occur by using death certificate data and by the limited adjudication of arrhythmic deaths, these inaccuracies were likely to be unrelated to baseline QT-interval data and therefore would tend to result in an underestimation of the association between QT-interval duration and specific causes of death in our study.
In conclusion, data from the NHANES III, a large sample representative of the general US population, showed a U-shaped relationship between QT interval and mortality end points. Shortened and prolonged QT-interval durations, even within reference ranges, were associated with increased risks of total, CVD, CHD, and non-CVD death. Detailed analyses of the dose-relationship between QT-interval duration and mortality in other populations should be conducted to confirm these findings, especially the mortality implications of a shortened QT interval, and to elucidate the mechanisms underlying these associations.
Supplementary Material
Acknowledgments
Funding/Support: The study was supported in part by Translational Cardiology grant 2008-03 from the National Center for Cardiovascular Research; grants ES015597 and HL091062 from the National Institutes of Health; the Donald W. Reynolds Cardiovascular Clinical Research Center at The Johns Hopkins University; and the Fondation Leducq.
Footnotes
Author Contributions: Study concept and design: Zhang, Post, Blasco-Colmenares, Tomaselli, and Guallar. Acquisition of data: Zhang, Blasco-Colmenares, and Guallar. Analysis and interpretation of data: Zhang, Post, Dalal, Blasco-Colmenares, and Guallar. Drafting of the manuscript: Zhang and Guallar. Critical revision of the manuscript for important intellectual content: Post, Blasco-Colmenares, and Guallar. Statistical analysis: Zhang, Dalal, Blasco-Colmenares, and Guallar. Obtained funding: Guallar. Study supervision: Guallar.
Financial Disclosure: None reported.
Online-Only Material: The eFigure is available at http://www.archinternmed.com.
REFERENCES
- 1.Priori SG, Schwartz PJ, Napolitano C, et al. Risk stratification in the long-QT syndrome. N Engl J Med. 2003;348(19):1866–1874. doi: 10.1056/NEJMoa022147. [DOI] [PubMed] [Google Scholar]
- 2.Sauer AJ, Moss AJ, McNitt S, et al. Long QT syndrome in adults. J Am Coll Cardiol. 2007;49(3):329–337. doi: 10.1016/j.jacc.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 3.fGaita F, Giustetto C, Bianchi F, et al. Short QT syndrome: a familial cause of sudden death. Circulation. 2003;108(8):965–970. doi: 10.1161/01.CIR.0000085071.28695.C4. [DOI] [PubMed] [Google Scholar]
- 4.Gussak I, Brugada P, Brugada J, et al. Idiopathic short QT interval: a new clinical syndrome. Cardiology. 2000;94(2):99–102. doi: 10.1159/000047299. [DOI] [PubMed] [Google Scholar]
- 5.Schimpf R, Borggrefe M, Wolpert C. Clinical and molecular genetics of the short QT syndrome. Curr Opin Cardiol. 2008;23(3):192–198. doi: 10.1097/HCO.0b013e3282fbf756. [DOI] [PubMed] [Google Scholar]
- 6.Algra A, Tijssen JGP, Roelandt JRTC, Pool J, Lubsen J. QT interval variables from 24 hour electrocardiography and the two year risk of sudden death. Br Heart J. 1993;70(1):43–48. doi: 10.1136/hrt.70.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dekker JM, Schouten EG, Klootwijk P, Pool J, Kromhout D. Association between QT interval and coronary heart disease in middle-aged and elderly men: the Zutphen Study. Circulation. 1994;90(2):779–785. doi: 10.1161/01.cir.90.2.779. [DOI] [PubMed] [Google Scholar]
- 8.Dekker JM, Crow RS, Hannan PJ, Schouten EG, Folsom AR, ARIC Study Heart rate-corrected QT interval prolongation predicts risk of coronary heart disease in black and white middle-aged men and women: the ARIC study. J Am Coll Cardiol. 2004;43(4):565–571. doi: 10.1016/j.jacc.2003.09.040. [DOI] [PubMed] [Google Scholar]
- 9.Okin PM, Devereux RB, Howard BV, Fabsitz RR, Lee ET, Welty TK. Assessment of QT interval and QT dispersion for prediction of all-cause and cardiovascular mortality in American Indians: the Strong Heart Study. Circulation. 2000;101(1):61–66. doi: 10.1161/01.cir.101.1.61. [DOI] [PubMed] [Google Scholar]
- 10.Pytlak A, Piotrowski W. Prognostic significance of QTc interval for predicting total, cardiac, and ischemic heart disease mortality in community-based cohort from Warsaw Pol-MONICA population. Ann Noninvasive Electrocardiol. 2000;5(4):322–329. [Google Scholar]
- 11.Perkiömäki JS, Sourander LB, Levomäki L, Räihä IJ, Puukka P, Huikuri HV. QT dispersion and mortality in the elderly. Ann Noninvasive Electrocardiol. 2001;6(3):183–192. doi: 10.1111/j.1542-474x.2001.tb00106.x. [DOI] [PubMed] [Google Scholar]
- 12.Robbins J, Nelson JC, Rautaharju PM, Gottdiener JS. The association between the length of the QT interval and mortality in the Cardiovascular Health Study. Am J Med. 2003;115(9):689–694. doi: 10.1016/j.amjmed.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Sheehan J, Perry IJ, Reilly M, et al. QT dispersion, QT maximum and risk of cardiac death in the Caerphilly Heart Study. Eur J Cardiovasc Prev Rehabil. 2004;11(1):63–68. doi: 10.1097/01.hjr.0000114970.39211.9e. [DOI] [PubMed] [Google Scholar]
- 14.Nilsson G, Hedberg P, Jonasson T, Lönnberg I, Öhrvik J. QTc interval and survival in 75-year-old men and women from the general population. Europace. 2006;8(4):233–240. doi: 10.1093/europace/euj040. [DOI] [PubMed] [Google Scholar]
- 15.Rautaharju PM, Kooperberg C, Larson JC, LaCroix A. Electrocardiographic abnormalities that predict coronary heart disease events and mortality in post-menopausal women: the Women’s Health Initiative. Circulation. 2006;113(4):473–480. doi: 10.1161/CIRCULATIONAHA.104.496091. [DOI] [PubMed] [Google Scholar]
- 16.Straus SMJM, Kors JA, De Bruin ML, et al. Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J Am Coll Cardiol. 2006;47(2):362–367. doi: 10.1016/j.jacc.2005.08.067. [DOI] [PubMed] [Google Scholar]
- 17.Kao WHL, Arking DE, Post W, et al. Genetic variations in NOS1AP are associated with sudden cardiac death in US white community-based populations. Circulation. 2009;119(7):940–951. doi: 10.1161/CIRCULATIONAHA.108.791723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anttonen O, Junttila MJ, Rissanen H, Reunanen A, Viitasalo M, Huikuri HV. Prevalence and prognostic significance of short QT interval in a middle-aged Finnish population. Circulation. 2007;116(7):714–720. doi: 10.1161/CIRCULATIONAHA.106.676551. [DOI] [PubMed] [Google Scholar]
- 19.Bernstein JM, Frishman WH, Chang CJ. Value of ECG P-R and QT-c interval prolongation and heart rate variability for predicting cardiovascular morbidity and mortality in the elderly: the Bronx Aging Study. Cardiol Elderly. 1997;5:31–41. [Google Scholar]
- 20.Elming H, Holm E, Jun L, et al. The prognostic value of the QT interval and QT interval dispersion in all-cause and cardiac mortality and morbidity in a population of Danish citizens. Eur Heart J. 1998;19(9):1391–1400. doi: 10.1053/euhj.1998.1094. [DOI] [PubMed] [Google Scholar]
- 21.Plan and operation of the Third National Health and Nutrition Examination Survey, 1988-94, series 1: programs and collection procedures. Vital Health Stat 1. 1994 Jul;(32):1–407. [PubMed] [Google Scholar]
- 22.Arizona Center for Education and Research on Therapeutics [Accessed September 15, 2009];Drugs that prolong the QT interval and/or induce torsades de pointes ventricular arrhythmia. http: //www.azcert.org/medical-pros/drug-lists/drug-lists.cfm.
- 23.Rautaharju PM, MacInnis PJ, Warren JW, Wolf HK, Rykers PM, Calhoun HP. Methodology of ECG interpretation in the Dalhousie program: NOVACODE ECG classification procedures for clinical trials and population health surveys. Methods Inf Med. 1990;29(4):362–374. [PubMed] [Google Scholar]
- 24.National Center for Health Statistics . The Third National Nutrition and Health Survey Linked Mortality File: Matching Methodology. US Dept of Health and Human Services, Centers for Disease Control and Prevention; Hyattsville, MD: 2006. [Google Scholar]
- 25.Sohaib SMA, Papacosta O, Morris RW, Macfarlane PW, Whincup PH. Length of the QT interval: determinants and prognostic implications in a population-based prospective study of older men. J Electrocardiol. 2008;41(6):704–710. doi: 10.1016/j.jelectrocard.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 26.Zabel M, Hohnloser SH, Behrens S, Li YG, Woosley RL, Franz MR. Electrophysiologic features of torsades de pointes: insights from a new isolated rabbit heart model. J Cardiovasc Electrophysiol. 1997;8(10):1148–1158. doi: 10.1111/j.1540-8167.1997.tb01001.x. [DOI] [PubMed] [Google Scholar]
- 27.Davey P. QT interval and mortality from coronary artery disease. Prog Cardiovasc Dis. 2000;42(5):359–384. doi: 10.1053/pcad.2000.0420359. [DOI] [PubMed] [Google Scholar]
- 28.Elming H, Sonne J, Lublin HK. The importance of the QT interval: a review of the literature. Acta Psychiatr Scand. 2003;107(2):96–101. doi: 10.1034/j.1600-0447.2003.00061.x. [DOI] [PubMed] [Google Scholar]
- 29.Roden DM. Long QT syndrome: reduced repolarization reserve and the genetic link. J Intern Med. 2006;259(1):59–69. doi: 10.1111/j.1365-2796.2005.01589.x. [DOI] [PubMed] [Google Scholar]
- 30.Gallagher MM, Magliano G, Yap YG, et al. Distribution and prognostic significance of QT intervals in the lowest half centile in 12,012 apparently healthy persons. Am J Cardiol. 2006;98(7):933–935. doi: 10.1016/j.amjcard.2006.04.035. [DOI] [PubMed] [Google Scholar]
- 31.Kobza R, Roos M, Niggli B, et al. Prevalence of long and short QT in a young population of 41,767 predominantly male Swiss conscripts. Heart Rhythm. 2009;6(5):652–657. doi: 10.1016/j.hrthm.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 32.Moriya M, Seto S, Yano K, Akahoshi M. Two cases of short QT interval. Pacing Clin Electrophysiol. 2007;30(12):1522–1526. doi: 10.1111/j.1540-8159.2007.00901.x. [DOI] [PubMed] [Google Scholar]
- 33.Antzelevitch C, Pollevick GD, Cordeiro JM, et al. Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals, and sudden cardiac death. Circulation. 2007;115(4):442–449. doi: 10.1161/CIRCULATIONAHA.106.668392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Viskin S. The QT interval: too long, too short or just right. Heart Rhythm. 2009;6(5):711–715. doi: 10.1016/j.hrthm.2009.02.044. [DOI] [PubMed] [Google Scholar]
- 35.Extramiana F, Antzelevitch C. Amplified transmural dispersion of repolarization as the basis for arrhythmogenesis in a canine ventricular-wedge model of short-QT syndrome. Circulation. 2004;110(24):3661–3666. doi: 10.1161/01.CIR.0000143078.48699.0C. [DOI] [PubMed] [Google Scholar]
- 36.Funada A, Hayashi K, Ino H, et al. Assessment of QT intervals and prevalence of short QT syndrome in Japan. Clin Cardiol. 2008;31(6):270–274. doi: 10.1002/clc.20208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mason JW, Ramseth DJ, Chanter DO, Moon TE, Goodman DB, Mendzelevski B. Electrocardiographic reference ranges derived from 79,743 ambulatory subjects. J Electrocardiol. 2007;40(3):228–234. doi: 10.1016/j.jelectrocard.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 38.Luo S, Michler K, Johnston P, Macfarlane PW. A comparison of commonly used QT correction formulae: the effect of heart rate on the QTc of normal ECGs. J Electrocardiol. 2004;37(suppl):81–90. doi: 10.1016/j.jelectrocard.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 39.Rautaharju PM, Surawicz B, Gettes LS, et al. American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; American College of Cardiology Foundation; Heart Rhythm Society. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2009;119(10):e241–e250. doi: 10.1161/CIRCULATIONAHA.108.191096. doi:10.1161/CIRCULATIONAHA.108.1910096. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.