Abstract
Objectives
To assess differences in sexual health behaviors, outcomes, and potential sociocultural determinants among male college students in the United States and the Netherlands.
Methods
Survey data were collected from random samples of students from both national cultures.
Results
American men were more likely to report inadequate contraception, HIV/STD infection, and unintended pregnancy than were Dutch men. Religiosity and sexuality education were able to explain national differences in these sexual health outcomes.
Conclusions
Findings suggest that sexuality education seems to decrease, rather than increase, sexual risk in heterosexually active male college students.
Keywords: sexual health, men’s health, United States, Netherlands, sexuality education
Sexual pleasure and risk are influenced by a variety of contextual factors. Sexual behaviors, whether they are risky or safer, are behaviors that are at least in part influenced by an individual’s larger sociocultural context. Research on factors affecting sexual health outcomes has demonstrated that human sexual behavior involves a complex sociocultural component. 1,2 Traditional models and theories of health behavior are often limited as they focus solely on the individual and not the broader social and cultural setting within which the individual operates.
Differences in sexual health outcomes across national cultures have been observed. For instance, recent epidemiological data highlight significant differences in unintended pregnancies, human immunodeficiency virus (HIV) and sexually transmitted disease (STD) infections, and induced abortions between young adults in the United States and Western European nations.3,4 Researchers and health officials have noted that young adults in the United States account for “epidemic” proportions of such adverse sexual health outcomes.5–7 In comparison, young adults in Western European nations, in general, and the Netherlands, in particular, have been noted as “most successful” in delaying the onset of first intercourse, preventing high prevalence of unintended pregnancies and induced abortions, and maintaining low prevalence of STD and HIV infections.8–15
Table 1 highlights dramatic differences in reported rates of several sexual health outcomes of young people in the Netherlands and the United States. These data provided the basis for our exploratory study of potential determinants of differences in sexual health outcomes within these 2 national cultures. Throughout our paper, we employ the term national cultures, rather than nationality or geographic location, based on Hofstede,16–18 who suggests that using this terminology captures “the complex societies of today’s nations by identifying key issues relevant to both the individual and the social system on which these nations differ in empirically verifiable ways” (p. 6).16
Table 1.
Annual Rates of Reported Sexual Health Outcomes for Young Adults (age 15–19) in the Netherlands and the United States (Berne & Huberman, 1999;a Panchaud, et al, 2000b)
| Sexual Health Outcome | Netherlands | United States |
|---|---|---|
| Pregnancy (per 1000 women)a | 12.2 | 83.6 |
| Live births (per 1000 women)a | 8.2 | 54.4 |
| Abortion (per 1000 women)a | 4.0 | 29.2 |
| AIDS cases (per 100,000)b | 0.2 | 2.3 |
| Syphilis cases (per 100,000)b | 1.0 | 6.4 |
| Gonorrhea cases (per 100,000)b | 7.7 | 571.8 |
| Chlamydia cases (per 100,000)b | 55.1 | 1131.6 |
The United States and the Netherlands, both nations that can be labeled as “developed” and “industrialized,” differ from one another in fundamental ways in terms of sociocultural sexual norms. Delbanco and colleagues19 have argued that “while subgroups within each country may differ in their views about sexuality and contraception, the Dutch tend to have a more open, liberal attitude; as a result, sexual health topics may be discussed more freely and pragmatically and in a less moralistic manner in the Netherlands than they are in the United States” (p. 71). Since the 1960s, the Dutch have been consistently noted for their predominantly liberal views on sexuality,11 including their general support for comprehensive sexuality education, openness in the family surrounding sexuality issues, and government-sponsored sexual health mass-media campaigns.8,12,20
The nature of national cultural differences in sexual norms is complex and has only recently been scientifically investigated. Hofstede,16 in an extensive review of comparative research, theorized that sexual norms within the United States and the Netherlands are uniquely socially constructed and are primarily related to differences between the national cultures on the dimension of masculinity/femininity. This construct represents differential levels of emotion found within a given culture. In relation to sexual norms, more “masculine” cultures, such as the United States, tend to be less positive and open about sexuality-related issues than do more “feminine” cultures, such as the Netherlands. Reiss6 and other social scientists have argued that high rates of adverse sexual health outcomes among young adults in the United States are a direct result of this general negative affect toward sexuality (or “erotophobia”) that is heavily based on conservative perspectives and fundamentalist religion.12,22 Such religious and political factors have been thought to impact societal attitudes toward sexuality and shape policies that restrict young peoples’ access to information and education on sexual health.6,8
Others have suggested that lower rates of adverse sexual health outcomes are related to a more positive affect toward sexuality (or “erotophilia”) in Western European nations.8,12,20 Ketting and Visser11 state that the Netherlands is unique, even within the European context, because the gravity of adverse sexual health outcomes was quickly recognized and accepted on an official level by the Dutch, who tend to be pragmatic in their approach to political and social issues. As a result of this early response, there has been a constant and additive flow over the past half-century of Dutch government-sponsored and research-based “reports, documents, discussions, debates, proposals, and activities” as well as “public information campaigns, school sex education programs, and information centers to help teach young people about reproduction and contraceptive options” (p. 162).11
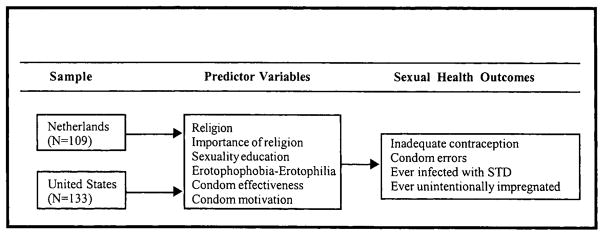
Few studies have directly tested the role of sociocultural factors in relation to sexual health outcomes. The purpose of this study was to determine if there are differences in sexual health outcomes among samples of male college students in the United States and the Netherlands who report recent sexual activity with a female partner and, if so, whether these differences are associated with selected factors related to sociocultural climates toward sexuality. Figure 1 gives a graphic representation of our study framework.
Figure 1.
Theoretical Framework of Our Study
Specifically, we focused on participants’ reported experiences with 4 adverse sexual health outcomes: using inadequate contraception, experiencing errors with condom use, ever being infected with an STD, and ever unintentionally impregnating a partner. We determined whether these outcomes were related to the sociocultural factors of religion, importance of religion, previous experiences with sexuality education, “erotophobia-erotophilia” or “the learned disposition to respond to sexual stimuli with negative-to-positive affect and evaluations” (p. 123),”perceived condom effectiveness, and condom motivation. In our analyses, we explored whether national cultural differences could be explained by those factors that were related to sexual health outcomes. We chose to investigate religiosity, sexuality education, and sexuality-related attitudes based on previous theoretical work that suggests these factors may be strongly associated with sexual health outcomes.
METHODS
Sampling
One large public university in the Midwestern United States and 1 large public university in the center of the Netherlands were selected for data collection. Similar to other international and comparative studies of sexual health, our 2 universities could both be classified as “public universities that are large in size but not located in a metropolis nor considered to be socially or politically atypical” (p. 47).24 The universities were chosen based on practical circumstances.
Arrangements were made with administrative offices at each university to confidentially acquire the contact information of potential participants for the purpose of mail-based data collection. The participants were chosen a priori on the basis of their declared major or school at each university. In the United States, students enrolled in programs of study in the departments of General Studies, Anthropology, Economics, Education, Psychology, or Sociology were selected. In the Netherlands, students enrolled in the Faculty of Social Sciences, with majors parallel to those of the American students, were chosen for selection. After receiving human subjects’ clearance from the appropriate institutional review boards, simple random sampling was employed in order to draw representative samples of male college students from the selected universities. Following each university’s approval, computers generated electronic lists of all eligible male students and, through the use of a software package, each student was randomly assigned a unique number and randomly selected according to this number. We chose to focus on college men as a first step in understanding sexual health outcomes among more diverse samples.
Potential participants were mailed a letter of introduction, a study information sheet, and a copy of the questionnaire. Within 2 weeks of mailing the questionnaire, a postcard was sent reminding participants to return the questionnaire if they had not done so already. Participation in the study was voluntary and anonymous. No identifying information, with the exception of broad demographic characteristics, was elicited. For Dutch participants, all materials were translated into Dutch, and translated back into English for reliability, in collaboration with a faculty member from the Department of Germanic Studies at Indiana University. The first author traveled to the Netherlands in early 2002 to assist in the data collection process. Identical data collection began simultaneously in the United States. From the total of 1800 students to whom we mailed recruitment materials, 369 men (or 21%) completed and returned the survey. Because of the nature of the recruitment procedure, it is not possible to determine the representativeness of the final samples.
Instrumentation
A comprehensive questionnaire assessing male sexual health and male condom use,25 used in previous college samples,26,27 was adapted and utilized in our study samples.
Demographics
The questionnaire solicited basic demographic information including age, ethnicity, sexual identity, and relationship status. Based on participants’ responses, we created a sexual relationship status variable as either exclusive (individuals in a steady relationship who engage in sexual activity exclusively with one another within the past 3 months) or nonexclusive (individuals who currently have multiple intimate relationships with several different sexual partners or engage in sexual activity with multiple partners without being involved in an ongoing intimate relationship within the past 3 months).
Sexual Health Outcomes
Participants were asked to report frequencies of specific sexual activities with male and female partners during the previous 3 months (in the questionnaire, sex was defined as “when you put your penis in your partner’s mouth, vagina, or rectum (anus, butt)”). Their use of a wide range of standard contraceptive methods during the previous 3 months was assessed including the pill, male condoms, the pill plus male condoms (colloquially referred to as “Double Dutch”), female condoms, diaphragm, and IUD. Participants were classified as using inadequate contraception if they reported either not using any of those contraceptive methods or withdrawal before ejaculation.
If participants reported using a male condom for vaginal, oral, and/or anal sex with a female partner at least once in the past 3 months, they were classified as condom users. These participants were asked to recount experiences with 34 errors and problems related to condom use.26,27 Potential condom use errors included availability errors (eg, wanting a condom but not having one available); communication errors (eg, not discussing condom use before sexual activity); and technical errors (eg, not leaving space at the tip of the condom). Total condom errors were calculated by summing participants’ scores across these 3 categories.
Participants were asked if a health care provider had ever informed them that they were infected with a sexually transmitted disease (including syphilis, gonorrhea, HIV/AIDS, genital herpes, trichomoniasis, chlamydia, and hepatitis B). Lastly, they were asked to report if they “think or know” that they had ever impregnated a partner without intending to.
Predictor Variables
The predictor variables assessed on our questionnaire included religiosity, importance of religion, erotophobia-erotophilia, sexuality education, perceptions of condom use effectiveness, and motivation to use condoms. Religiosity was determined by distinguishing between religious (those identifying as members of a variety of Christian and non-Christian religions) and nonreligious participants (those identifying as either nonpracticing or atheist). Participants described the level of importance of religion in their daily lives, measured on a scale of 1 (not important at all) to 7 (very important).
Participants were asked to report if they ever received formal sexuality education by selecting 1 or more responses to the following question: “How would you describe the type of sexuality education you received? 1. I have had no formal sex education, 2. I received sex education from my parents/guardians, 3. I received sex education in middle school, 4. I received sex education in high school.” For use with logistic regression, the 3 separate sexuality education variables (parents, middle school, and secondary school) were combined to create an overall index of the participants’ experience with sexuality education by summing the responses to the 3 individual questions.
The questionnaire employed the 7-point Likert-type erotophobia-erotophilia scale,23 designed to measure the levels of avoidance or approach responses to sexual stimuli by assessing the participants’ extent of agreement or disagreement to several statements (eg, “Almost all pornographic material is nauseating”). The scale has been used in diverse North American samples23,28 as well as in international samples in Israel, France, Finland, Germany, Japan, Norway, Portugal, Sweden, and Zimbabwe.29 The scale had not been previously reported in Dutch samples. Reliability of the erotophobia-erotophilia scale was determined to be moderate in our sample, r(242)=.63.
The questionnaire measured participants’ beliefs in the effectiveness of condoms in preventing HIV/STD infections and pregnancies on a scale from 1 (very effective) to 4 (not at all effective). Their motivation to use condoms with their sexual partners was also assessed on a scale of 1 (highly motivated) to 5 (not at all motivated).
Data Analysis
Analyses of the data included descriptive, bivariate, and multivariate statistical techniques. We first used Pearson chi-square tests and analyses of variance (ANOVA) to determine if differences were present between Dutch and American participants in terms of demographic factors, sexual health outcomes, and predictor variables. The alpha level was set at P<0.05. After finding numerous significant differences between the Dutch and American participants, we controlled for demographic variables that significantly differed between the 2 samples in our exploratory analyses (age and sexual relationship status) to assure that differences in sexual health outcomes and predictor variables were not confounded by demographic variables. We used backward multivariate logistic regression to see whether the differences in the sexual health outcomes between the 2 national cultures could be explained by differences in our hypothesized predictor variables.
We calculated exact 95% confidence intervals for the odds ratios associated with our sexual health outcomes because several cells were found to contain a small number of respondents (for example, 1 participant in the Netherlands reported experience with unintended pregnancy). Reliability of the traditional large-sample, normal theory-based 95% confidence intervals used in our statistical software may have been questionable. In using exact 95% confidence intervals, we were able to avoid the issue of accuracy of large-sample approximations because approximation is not necessary as the values are exact.30
RESULTS
Sample
A total of 369 participants completed and returned the survey (193 American and 176 Dutch). To qualify for analysis, participants had to report having had vaginal, oral, and/or anal sex with a female partner at least once during the preceding 3 months. Given our focus on currently sexually active individuals, we excluded the 91 respondents who reported that they had not engaged in any sexual activity with a partner during the previous 3 months.
We chose to analyze data from respondents who engaged in other-sex activity due to a small number of men who reported engaging in recent sexual activity exclusively with other men (N=15) and the resulting lack of statistical power. Men were not excluded based on their self-reported sexual identity. A small number of men reported at least 1 sexual experience with a man during the previous 3 months (2.5%, N=6) in addition to recent sexual involvement with women; however, only their sexual behaviors with female partners were included in the analyses.
In order to maintain a focus on “traditional” college-age students, 21 participants over the age of 30 years old were also excluded. Thus, data were analyzed from 242 male participants who engaged in recent sex with a female partner (133 American and 109 Dutch, ages 18–30 years old).
Table 2 presents an overview of our sample, including the multivariate analyses exploring the relationships between selected sociocultural factors and selected sexual health outcomes while controlling for demographic factors.
Table 2.
Means (SD), Proportions, and Comparisons of Demographic Variables With Relationships Between National Cultures and Sexual Health Outcomes Controlling for Demographic Variables (N=242)
| Variable | Netherlands (N=109, 45%) | United States (N=133, 55%) | Total (N=242) | F/χ2 | Odds-Ratio (95% CI) |
|---|---|---|---|---|---|
| Demographies | |||||
| Age (years) | 23.30(2.13) | 21.27(2.67) | 22.19(2.59) | 43.42**** | |
| Sexual relationship status | 17.50**** | ||||
| Exclusive (%) | 54.3 | 25.6 | 67.8 | ||
| Nonexclusive (%) | 45.7 | 74.4 | 32.2 | ||
| Predictors (controlling for demographics) | |||||
| Religion | 9.31 (5.11–16.95)**** | ||||
| Religious (%) | 33.9 | 82.7 | 60.7 | ||
| Nonreligious (%) | 66.1 | 17.3 | 39.3 | ||
| Importance of religion | 2.04(1.65) | 3.55(1.87) | 2.87(1.92) | 38.56**** | |
| Sexuality education | |||||
| Parents (%) | 51.4 | 23.3 | 36.0 | 0.29(0.17–0.50)**** | |
| Middle school (%) | 73.4 | 35.3 | 52.5 | 0.20(0.11–0.35)**** | |
| Secondary school (%) | 83.5 | 67.7 | 74.8 | 0.41 (0.22–0.77)*** | |
| Total | 2.08 (0.73) | 1.26(0.84) | 1.63(089) | 57.31**** | |
| Sexual attitudes, beliefs, and intentions | |||||
| Erotophobia-Erotophilia | 2.61 (1.00) | 3.07 (1.03) | 2.86(1.04) | 16.80**** | |
| Condom effectiveness | 3.90(0.31) | 3.65 (0.48) | 1.32(0.45) | 21.58**** | |
| Condom motivation | 3.34(1.28) | 2.71 (1.54) | 2.99(1.46) | 1.83, ns | |
| Outcomes (controlling for demographics) | |||||
| Inadequate contraception (%) | 6.4 | 33.1 | 21.1 | 7.20(2.97–17.49)****† | |
| Total Condom Errors | 1.78(0.82) | 2.11 (0.67) | 1.98(0.75) | 2.85* | |
| Ever had STD (%) | 3.7 | 16.5 | 10.7 | 5.20 (1.78–16.88)****† | |
| Ever unintentionally impregnated (%) | 0.9 | 14.3 | 8.3 | 18.00(2.75–734.67)****† | |
P<1.0,
P<0 .05,
P<0.01,
P<0.001,
Exact 95% Confidence Interval
Demographics
The mean age of the participants was 22 years (SD=2.59). A significant difference in age was found between American and Dutch participants, F(1, 241)=43.42, P<0.001. American participants (M=21.27, SD=2.13) were significantly younger than Dutch participants (M=23.30, SD=2.67).
Dutch participants were significantly more likely to report being in exclusive sexual relationships (82%, N=89) than Americans (56%, N=75), χ2 (1. N=242)= 17.50, P<0.01.
In terms of ethnicity, 93% of the sample identified as white (N=225) and the remaining 7% as other ethnicities (N=17). The majority of the men self-identified as heterosexual (97%, N=234), with the remainder as bisexual (2.5%, N=6) and homosexual (0.8%, N=2). Most participants grew up in either small (32%, N=78) or medium-sized (25%, N=68) sized cities. Significant differences were not found between the 2 samples in relation to these variables.
Sexual Health Outcomes
American participants were more likely (33%, N=44) to use inadequate contraception than were Dutch participants (6%, N=7), (OR=7.20, 95% CI =2.97–17.49). We excluded 2 Dutch men and 1 American man who reported that they were trying to impregnate their partners during the previous 3 months.
Condom use errors were assessed from 74 American and 49 Dutch condom users. American participants had a marginally significantly higher mean score (M=2.11, SD=.67) of condom errors than did Dutch participants (M=1.98, SD = .75), F(1, 122)=2.85, P<0.09. Controlling for demographic variables, the differences were no longer significant. Thus, condom use errors were not explored further in relation to predictor variables
American participants were more likely (17%, N=22) to report having been diagnosed with a sexually transmitted disease than were Dutch participants (4%, N=4), (OR=5.20, 95% CI=.78–16.88). American participants were also more likely (14%, N=19) to report ever having unintentionally impregnated a partner than were Dutch participants (1%, N=1), (OR=18.00, 95% CI=.75–754.67).
Predictor Variables
American participants were more likely to identify as religious (83%, N=110) than were Dutch participants (34%, N=37), (OR=9.31, 95% CI=5.11–16.95). A significant relationship was also found between national culture and importance of religion, F(1, 241)=38.56, P<0.001. American participants (M=3.55, SD=1.87) were more likely to report religion as important in their daily lives than were Dutch participants (M=2.04, SD=1.65).
American participants were less likely to report having received sexuality education from their parents (23%, N=31) than were their Dutch counterparts (51%, N=56), (OR=0.29, 95% CI = 0.17–0.50). American participants were less likely to report having received sexuality education in middle school (35%, N=47) than were their Dutch counterparts (73%, N=80), (OR=0.20, 95% CI=0.11–0.35). In addition, American participants were less likely to report having received sexuality education in secondary school (68%, N=90) than were Dutch participants (84%, N=91), (OR=0.41, 95% CI=0.22–0.77). Overall, Dutch participants’ mean total sexuality education score (2.08, SD=0.73) was significantly higher than Americans’ mean score (1.26, SD=0.84), F(1, 241) = 57.31, P<0.001.
A significant relationship was found between national culture and erotophobia-erotophilia, F(1, 241)=16.80, P<0.001. Dutch participants (M=2.61, SD=1.00) were significantly more erotophilic, or had a more positive affect toward sexuality, than American participants (M=3.07, SD=1.03).
Dutch participants’ mean scores (M=3.90, SD=.31) suggested that they were also more likely than American participants (M=3.65, SD=.48) to view condoms as effective in preventing STD and pregnancy, F(1, 241)=21.58, P<0.001.
Dutch participants’ mean scores (M=3.34, SD=1.28) did not suggest that they were more likely than American participants (M=2.71, SD= 1.54) to be highly motivated to use condom with their sexual partners.
Logistic Regression
As shown in Table 3, several of our hypothesized predictor variables were successful in predicting sexual health outcomes. Using inadequate contraception was significantly predicted by importance of religion (OR=0.77, 95% CI=0.61–0.96) and sexuality education (OR=1.67, 95% CI= 1.04–2.67). Individuals with a higher importance of religion and less overall sexuality education were less likely to use adequate contraception. When analyzed with the predictor variables, national culture was no longer significant in predicting inadequate contraception.
Table 3.
Backward Logistic Regression Analyses Including National Culture for Sexual Health Outcomes and National Culture and Predictor Variables for Sexual Health Outcomes (N=242)
| Dependent Variable | Predictor Variable | B | Odds Ratio | B | Odds Ratio |
|---|---|---|---|---|---|
| Inadequate Contraception | National culture | −1.71 | 7.20 (2.97–17.49)****† | ns | ns |
| Importance of religion | −0.27 | 0.77 (0.61–0.96)*** | |||
| Sexuality education | 0.51 | 1.67 (1.04–2.67)*** | |||
| Ever had STD | National culture | 1.65 | 5.20 (1.78–16.88)***† | ns | ns |
| Sexuality education | −1.22 | 0.30 (0.11–0.79)*** | |||
| Ever Unintentionally Impregnated | National culture | 2.89 | 18.00 (2.75–754.67)***† | ns | ns |
| Importance of religion | −0.25 | 0.78 (0.59–1.04)* | |||
| Sexuality education | −2.70 | 0.07 (0.01–0.43)**** |
P<1.0,
P<0.05,
P<0.01,
P<0.001,
Exact 95% Confidence Interval
Ever having been infected with a sexually transmitted disease was significantly predicted by sexuality education (OR=0.30, 95% CI=0.11–0.79). Individuals with less overall sexuality education were more likely to report having been infected with an STD. Ever having unintentionally impregnated a partner was significantly predicted by sexuality education (OR=0.07, 95% CI=0.01–0.43). Individuals with less sexuality education were more likely to report having unintentionally impregnated a partner. A marginally significant relationship was also present with importance of religion (OR=0.78, 95% CI=0.59–1.04). Individuals who reported a higher importance of religion were more likely to report having unintentionally impregnated a partner. Again, when analyzed with the predictor variables, national culture was no longer significant in predicting ever having been infected with an STD or ever having unintentionally impregnated a partner.
DISCUSSION
The results from our analyses are striking and show many significant differences in sexual health exist between our samples of American and Dutch male college students reporting recent sex with a female partner. Significant differences were found on every variable in the directions we expected, demonstrating that male college students in the Netherlands report fewer adverse sexual health outcomes when compared to male college students in the United States.
We hypothesized that differences in sexual health outcomes found between participants in the United States and the Netherlands would be explained by factors such as religiosity, sexuality education, and sexuality-related attitudes. The results of our multivariate analyses suggest that religiosity and sexuality education were, indeed, predictive of differences in sexual health outcomes between our samples. Participants who reported higher importance of religion and less sexuality education were less likely to report using adequate contraception. Participants who were less likely to report having received sexuality education were more likely to report ever having been infected with a sexually transmitted disease. Participants who were less likely to report having sexuality education were also more likely to report ever having unintentionally impregnated a partner. Those who reported higher importance of religion were also marginally more likely to report unintentionally impregnating a partner. These results are consistent with previous theoretical explanations for differential sexual health outcomes between the United States and the Netherlands.8,12,19 Furthermore, the fact that national culture as a predictor disappears in multivariate analyses shows that the predictor variables of religiosity and sexuality education function in similar ways within both the United States and the Netherlands.
It is noteworthy for health educators that sexuality education, in particular, was predictive of fewer reports of all 3 negative sexual health outcomes in our sample. An intense debate continues in the United States in regard to sexuality education, including those who favor comprehensive approaches, those who favor abstinence-only approaches, and those who favor no sexuality education whatsoever.8 A central argument of some who oppose comprehensive sexuality education is that giving individuals information about sexuality, in and of itself, may increase sexual risk; however, the outcomes of our study clearly suggest the opposite. Sexuality education seems to decrease, rather than increase, sexual risk.
Comprehensive sexuality education that is based on young peoples’ rights, respect and responsibility has shown relative success in the Netherlands and may yield similar results in the United States.8 The Sexuality Information and Education Council of the United States (SIECUS)31 recommends comprehensive, age-appropriate, lifelong educational programs that focus on providing people with accurate information related to numerous biological, psychological, and social sexual health issues. Individuals who experience more comprehensive educational interventions may be less likely to experience adverse sexual health outcomes, as our findings suggest.
The results of our study must be interpreted while considering its limitations. It is possible that college students may respond differently to a questionnaire on human sexuality than would their counterparts who do not attend college. Fewer young people in the Netherlands attend universities than young people in the United States so the results may not be generalizable to men outside the college environment.
Although we controlled for demographic variables in our analyses, it is possible the samples are not ideally suited for comparison based on the significant differences between them in terms of age and relationship status. Additionally, although the samples were similar to one another in terms of geographical location and student characteristics, empirical evidence’ that the universities are comparable to one another does not exist.
Mail-based random sampling techniques have also proven to be problematic in previous international and comparative studies on sexual behaviors, mainly due to low response rates.19,24 Although this was certainly an issue of concern in our study, we feel nonresponse may have been amplified in our samples because, due to bureaucratic delays, mail-based sampling did not begin until the end of the spring term at both universities, a time when many students had left the campus (numerous envelopes were deemed undeliverable and subsequently returned to the investigator). Even though response rate was low, we have no reason to assume that nonresponse was different between the 2 universities.
Last, using a cross-sectional method, it is possible that a survey may not have fully assessed complex and dynamic factors that are reflective of a nation’s sociocultural climate in regard to sexuality at a given point in time. For example, the limited operationalization of concepts such as sexuality education on a brief 1-time questionnaire did not allow us to assess the content and quality of such education,32 even if previous experience was reported. Future research endeavors may benefit from a more in-depth investigation of sociocultural climates than we were able to employ in our samples through ongoing and additive research.
Although this study was exploratory in nature, it holds implications for further international and comparative studies of sexual health in different national cultures. The disparities in sexual health outcomes between our samples suggest that national cultures such as the Netherlands have a great deal to offer in terms of their successful approaches to sexual health. Future research should focus on new ways of operationalizing, measuring, and understanding the Dutch approach to sexual health. Such information could be valuable for improving sexual health in other national cultures and contexts, including the United States.
Acknowledgments
The first author would like to express his appreciation to Linda Berne, EdD, Barbara Huberman, MEd, and the participants of the 1999 Advocates for Youth European Study Tour for the original inspiration to conduct this study. We would also like to acknowledge Drs Erick Janssen, Cynthia Graham, Stephanie Sanders, Mohammad Torabi, and Richard Crosby, as well as Inge van der Cruyssevan Antwerpen, JD, and Eriko Tomiyama Dodge, BGS, for their support during the formative phase of the project. During the production of this manuscript, we would like to thank Drs. Rita Melendez, Susie Hoffman, Raymond Smith, Sharlene Beckford, Sheri Kirshenbaum, Peter Lin, David Lounsbury, Ouzama Nicholson, Rogerio Pinto, and Michael Stirratt, for their invaluable feedback on earlier drafts of this paper. Lastly, we appreciate the time and statistical expertise of Drs Bruce Levin and Theresa Exner.
Support for this project was provided by funds from the Friends of The Kinsey Institute Grant-In-Aid Award and the William L. Yarber Professorship Fellow Award, both to the first author. During the production of this manuscript, the first author acknowledges support in the form of center grant P30 MH43520 from the National Institute of Mental Health to the HIV Center for Clinical and Behavioral Studies, Anke A. Ehrhardt, PhD, Principal Investigator, and NRSA T32 MH19139, Behavioral Sciences Research in HIV Infection, Anke A. Ehrhardt, PhD, Program Director.
Contributor Information
Brian Dodge, Behavioral Sciences Research in HIV Infection Fellow, Columbia University/New York State Psychiatric Institute, HIV Center for Clinical and Behavioral Studies.
Theo G. M. Sandfort, Associate Professor, Clinical Sociomedical Sciences (in Psychiatry), Research Scientist, Columbia University/New York State Psychiatric Institute, HIV Center for Clinical and Behavioral Studies, New York, NY.
William L. Yarber, Professor, Indiana University, Department of Applied Health Science, Bloomington, IN.
John de Wit, Associate Professor, Department of Social and Organizational Psychology, Utrecht University, Utrecht, Netherlands.
References
- 1.Parker R, Herdt G, Carballo M. Sexual culture, HIV transmission, and AIDS research. J Sex Res. 1991;28:77–98. [Google Scholar]
- 2.Vanwesenbeeck I, van Zessen G, Ingham R, et al. Factors and processes in heterosexual competence and risk: an integrated review of the evidence. Psychol Health. 1997;14:25–50. [Google Scholar]
- 3.Darroch J, Singh S, Frost J, et al. Differences in teenage pregnancy rates among 5 developed countries: the roles of sexual activity and contraceptive use. Fam Plann Perspect. 2001;33:244–250. [PubMed] [Google Scholar]
- 4.Panchaud C, Singh S, Feivelson D, et al. Sexually transmitted diseases among adolescents in developed countries. Fam Plann Perspect. 2000;32:24–32,45. [PubMed] [Google Scholar]
- 5.Eng TR, Butler WT. The Hidden Epidemic: Confronting Sexually Transmitted Diseases. Washington, D.C: National Academic Press; 1997. pp. 1–432. [PubMed] [Google Scholar]
- 6.Reiss IL. An End to Shame: Shaping Our Next Sexual Revolution. Buffalo, NY: Prometheus Books; 1990. pp. 1–287. [Google Scholar]
- 7.Satcher D. The Surgeon General’s Call to Action to Promote Sexual Health and Responsible Sexual Behavior. Rockville, MD: Office of the Surgeon General; 2001. pp. 1–29. [PubMed] [Google Scholar]
- 8.Berne L, Huberman B. European Approaches to Adolescent Sexual Behavior and Responsibility. Washington, DC: Advocates for Youth; 1999. pp. 1–85. [Google Scholar]
- 9.Ketting E. The effect of oral contraception on society. Nederlands TijdschriftvoorGeneeskunde. 2000;144(6):283–286. [PubMed] [Google Scholar]
- 10.Ketting E. Forum for Family Planning: Can We Learn from the Dutch? London: FPA; 1994. Teenage pregnancy: A problem that can be reduced; pp. 1–12. [Google Scholar]
- 11.Ketting E, Visser A. Contraception in the Netherlands: The low abortion rate explained. Patient Educ Couns. 1994;23:161–171. doi: 10.1016/0738-3991(94)90032-9. [DOI] [PubMed] [Google Scholar]
- 12.Lottes I. Sexual health policies in other industrialized countries: are there lessons for the United States? J Sex Res. 2002;39:79–83. doi: 10.1080/00224490209552125. [DOI] [PubMed] [Google Scholar]
- 13.de Vroome EMM, Paalman MEM, Dingelstad AAM, et al. Increase in safe sex among the young and non-monogamous: knowledge, attitudes and behavior regarding safe sex and condom use in the Netherlands from 1987 to 1993. Patient Educ Couns. 1994;24:279–288. doi: 10.1016/0738-3991(94)90071-x. [DOI] [PubMed] [Google Scholar]
- 14.Rademakers J. Teenage pregnancy and contraceptive behavior in the Netherlands. In: Correa H, editor. Unwanted Pregnancies and Public Policy: An International Perspective. Commack, NY: Nova Science Publishing; 1994. pp. 59–68. [Google Scholar]
- 15.Vogels T, van der Vliet R, Danz M, et al. Young people and sex: Behaviour and health risks in Dutch school students. Int J Adol Med Health. 1993;6(2):137–147. doi: 10.1515/IJAMH.1993.6.2.137. [DOI] [PubMed] [Google Scholar]
- 16.Hofstede GH, editor. Masculinity and Femininity: The Taboo Dimension of National Cultures. Thousand Oaks, CA: Sage Publications; 1998. pp. 1–238. [Google Scholar]
- 17.Hofstede GH. Empirical models of cultured differences. In: Bleichordt N, Drenth PJD, editors. Contemporary Issues in Cross-Cultural Psychology. Amsterdam/Lisse: Swets & Zeitlinger; 1991. pp. 4–20. [Google Scholar]
- 18.Hofstede GH. National cultures revisited. Behav Sd Res. 1987;18:285–305. [Google Scholar]
- 19.Delbanco S, Lundy J, Hoff T, et al. Public knowledge and perceptions about unplanned pregnancy and contraception in three countries. Fam Plann Perspect. 1997;29:70–75. [PubMed] [Google Scholar]
- 20.Kok G, Kolker L, de Vroome E, et al. ‘Safe sex’ and ‘compassion’: Public campaigns on AIDS in the Netherlands. In: Sandfort TGM, editor. The Dutch Response to HIV: Pragmatism and Consensus. London: UCL Press; 1998. pp. 19–39. [Google Scholar]
- 21.Weeks J. The social construction of sexuality. In: Peiss K, editor. Major Problems in the History of American Sexuality. Boston: Houghton Mifflin Company; 2002. pp. 2–9. [Google Scholar]
- 22.Weeks J. Sex, politics and society: The regulation of sexuality since 1800. 2. London: Longman; 1989. pp. 1–326. [Google Scholar]
- 23.Fisher WA, Byrne D, White LA, et al. Erotophobia-erotophilia as a dimension of personality. J Sex Res. 1988;25:123–151. [Google Scholar]
- 24.Weinberg MS, Lottes I, Shaver F. Sociocultural correlates of permissive sexual attitudes: a test of Reiss’s hypothesis about Sweden and the United States. J Sex Res. 2000;37:44–52. [Google Scholar]
- 25.Kinsey Institute. Male Condom Use Errors Survey (MCUES) Bloomington, IN: The Kinsey Institute for Research in Sex, Gender, and Reproduction at Indiana University; 2001. pp. 1–15. [Google Scholar]
- 26.Crosby RA, Sanders S, Yarber WL, et al. Condom use errors and problems among college men. Sex Transm Dis. 2002;29:552–557. doi: 10.1097/00007435-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Sanders SA, Graham CA, Crosby RA, et al. Condom use errors and problems among young women who put condoms on their male partners. Journal of the American Women’s Medical Association. 2003;58(2):95–98. [PubMed] [Google Scholar]
- 28.Yarber WL, Fisher WA. Affective orientation to sexuality and venereal disease preventive behaviors. Health Values. 1983;7(6):19–23. [Google Scholar]
- 29.Fisher WA. The sexual opinion survey. In: Davis CM, Yarber WL, Bauserman G, et al., editors. Sexuality-Related Measures: A Compendium. 2. Thousand Oaks, CA: Sage Publications; 1998. pp. 218–222. [Google Scholar]
- 30.Fleiss JL, Levin B, Cho Paik M. Statistical Methods for Rates and Proportions. 3. Hoboken, NJ: John Wiley & Sons; 2003. p. 112. [Google Scholar]
- 31.Sexuality Information and Education Council of the United States. Developing Guidelines for Comprehensive Sexuality Education. New York: SIECUS; 2000. pp. 1–36. [Google Scholar]
- 32.Lewis J, Knijn T. A comparison of English and Dutch sex education in the classroom. Educ Health. 2001;19(4):59–64. [Google Scholar]