Abstract
Objectives
The study was conducted to examine the relative effectiveness of two psychosocial treatments (cognitive behavior therapy with cultural tailoring intervention versus brief medication management).
Methods
The study used a two-arm randomized controlled trial of individual therapy in which participant assignment was stratified by gender. Data were collected at baseline and at four follow-up points: one and four weeks and three and six months from the quit date. The intervention condition received eight 40-minute weekly sessions of individualized counseling using cognitive behavior therapy and cultural tailoring intervention, while the control condition received eight 10-minute weekly sessions of individualized counseling focusing on medication management. Both conditions received 8-week nicotine patches.
Results
Thirty Korean immigrants participated in the study. By intention-to-treat analysis, 57.1% of participants in the intervention and 18.8% of participants in the control had 7-day point prevalence abstinence at the 6-month follow-up (odds ratio = 5.8, 95% confidence interval = 1.12–26.04, p = 0.04). Participants’ self-reported abstinence was biochemically validated with breath carbon monoxide and salivary cotinine tests.
Conclusions
The combination of cognitive behavior therapy and cultural tailoring intervention had a better treatment outcome compared to brief medication management. The promising result suggests the need to further test the intervention in a larger sample and longer follow-ups before it can be adapted in clinical settings.
Keywords: smoking, smoking cessation, theory of planned behavior, cultural tailoring, Asian Americans
INTRODUCTION
Korean American men smoke at much higher rates ranging from 26.9% to 38.7% than the general U.S. population whose smoking rates hover around 20% [1–5]. They have the highest smoking-attributable cancer death rate within the Asian American population [6, 7]. In contrast, smoking rates among Korean American women have been modest although those who are acculturated to American culture smoke at a rate similar to that of the general U.S. female population [8]. Stigma associated with woman smokers still prevails in most Asian countries including Korea [9, 10]. Thus, women of Asian descent tend to underreport current use [11] and their smoking rates are likely to be underestimates. The fear of disclosure was indeed found as one of the major barriers to seeking help for smoking cessation among Asian American women [12, paper in submission].
There is a paucity of studies on the efficacy of tobacco dependence treatment in Korean Americans. To date, only three studies [13–15] have been published. The study by Fang and others [13] was the first published literature on tobacco dependence treatment for Korean Americans. However, the study did not explicate the process of cultural tailoring for Korean Americans. The second study [14] was not a clinical trial of tobacco dependence treatment. It was conducted as part of community-based health promotion activities. No information was available regarding the characteristics of the participants in terms of demographics and smoking behavior. Some cultural intervention components described in this article, such as using smoking-related health statistics in Korea, were adapted for use in the present study. The third study [15] was a randomized controlled trial of an Internet-based smoking cessation program in comparison with a similar program delivered via booklet. There was no significant difference in 30-day abstinence between the two intervention approaches. In all the three studies [13–15], abstinence rates were based on self-report without biochemical verification.
To our knowledge, no research study has been conducted to date to examine the relative effectiveness of a culturally tailored cognitive behavioral intervention compared to brief medication management in Korean Americans. The present study was guided by the Theory of Planned Behavior (TPB) [16, 17], targeting attitudes and perceived social norms through education and family involvement, and self-efficacy through the use of education, behavioral skill training, and nicotine replacement therapy (NRT).
To be successful, clinicians and researchers suggest that smoking cessation programs be anchored in the norms, values, and experiences of a particular population [18, 19]. From a very young age, children in East Asian countries are typically educated to be sensitive to how others would perceive their behavior. Their sensitivity to social cues is largely related to the cultural value of conformity and collectivism [20–22]. In line with this notion, perceived social norms favoring quitting have been found as the strongest predictor of intentions to quit smoking and actual quit attempts in Korean male immigrants [23]. Given this, perceived social norms may have a specific cultural implication that motivates Korean immigrant smokers to quit smoking.
Perceived social norm is one of the three antecedents to behavioral intentions proposed in the TPB [16, 17]; attitudes and perceived behavioral control are the other two. According to Ajzen [17], (a) attitudes are the degree to which a person has a favorable or unfavorable evaluation or appraisal of the behavior in question, (b) perceived social norms are defined as the individual’s perception of social pressures to perform the behavior, and (c) perceived behavioral control refers to the perceived ease or difficulty of performing the behavior. The theory posits that the more favorable attitudes and perceived social norms are with respect to the behavior, and the greater the individual’s perceived behavioral control, the stronger the behavioral intentions to perform the behavior should be. The construct perceived behavioral control was adapted from Bandura’s [24] self-efficacy. Researchers [25–27] using the TPB often use self-efficacy instead of perceived behavioral control. Findings from a meta-analysis [28] revealed that self-efficacy had greater predictive power in regard to behavioral intention and actual behavior than perceived behavioral control.
In addition to the TPB variables, religion (being Christian) [29–31], alcohol use, [29, 32], and depression [33, 34] were included in baseline assessment because these variables have been identified as correlates of smoking and quit attempts in Korean Americans. The following two hypotheses were postulated:
Korean Americans who received cognitive behavior therapy and cultural tailoring intervention in conjunction with NRT (the intervention condition) would have a significantly higher smoking abstinence rate than Korean Americans who received brief medication management with NRT (the control condition).
There would be significant differences in positive and negative attitudes, perceived social norms, and self-efficacy between pre- and post-treatment assessments, and the differences would be significantly greater in the intervention condition than in the control condition.
Research Method
Study Design
The study employed a two-arm randomized controlled trial with baseline and four follow-up assessments (1/4 weeks and 3/6 months). The study was approved by the Institutional Review Board of a medical university. All the participants signed the informed consent form and were provided with a gift certificate worth $20 as an incentive at each assessment: baseline and three follow-ups (four weeks, and 3/6 months).
Subjects
Participants were all Korean immigrants residing in the northeast region of the nation where a large number of Korean immigrants had settled. They were self-identified Korean Americans who (1) were able to speak and read Korean or English, (2) aged 18 years or more, (3) had been smoking at least 10 cigarettes per day for the past six months, (4) were willing to use nicotine patches as directed, and (5) were expected to live in the study geographical area for at least one year. During the single-arm pilot study (N = 22, data unpublished), participants were restricted to those who were able to speak and read Korean. Yet, due to difficulty recruiting female smokers, any self-identified Korean adults were invited to the study regardless of their preferred language (Korean versus English). People were excluded if they (1) were currently involved in other treatments for smoking cessation, (2) were pregnant or lactating, or had a plan to become pregnant in the next 12 months, (3) had a history of serious cardiac diseases or presence of skin diseases, or (4) earned a score of 20 or higher on the Alcohol Use Disorders Identification Test (AUDIT) [35]. Criterion two and three were related to contraindications to nicotine patches [36]. The decision to exclude those with drinking problems was based on the outcomes of the pilot study. In the pilot study, eight of the participants (36.4%) earned scores of 8 or higher on the AUDIT, including two whose scores were 20 or higher. Three dropped out of the program, and the other four also relapsed to smoking shortly after the program (within the 3-month follow-up). Only one (1/8, 12.5%) continued to be abstinent at the 6-month follow-up. In contrast, among those without drinking problems (n = 14), two dropped out and four relapsed to smoking shortly after the program. Five (5/14, 35.7%) continued to be abstinent at 6-month follow-up. If we had adopted the cutoff score of 8, more than one-third of the potential participants would have been ineligible. Instead, we used the cutoff score of 20 in order to exclude smokers who might have a serious alcohol problem [35].
Procedures
Most participants were recruited via advertisements in Korean newspapers calling for smokers who were willing to participate in a research project for smoking cessation. All the advertisements were written in Korean and posted for about three months. Forty people contacted the research team and were screened briefly via telephone interviews. All the interviews were conducted in Korean. Of these, 34 people met the inclusion criteria and 31 participated in baseline assessment. Those who were excluded were mostly light smokers with 5–8 cigarettes a day. One person who earned a score of 20 on the AUDIT [35] was excluded. The person denied having a problem with alcohol use and refused to refrain from drinking alcohol.
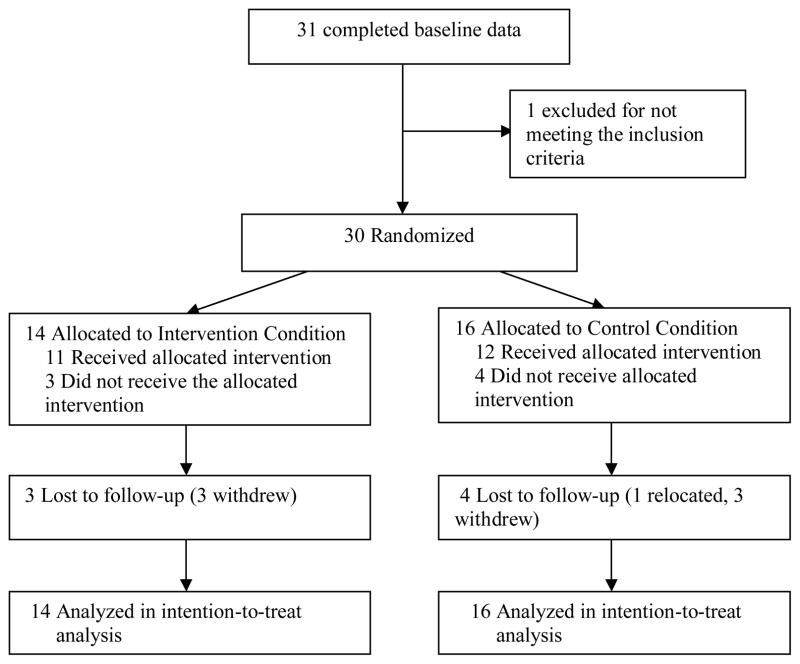
The remaining 30 were randomized into one of two conditions (intervention versus control) by a computer-generated number, and the randomization was stratified by gender. Fourteen people were assigned to the intervention and 16 to the control (Figure 1). The decision to stratify random allocation by gender was based on the following two reasons. First, gender differences in smoking cessation outcomes have been consistently reported [37–39]. Secondly, we were not sure how many Korean women would participate in a person-to-person smoking cessation study, given that smoking is still socially proscribed behavior against women in the Korean American community [4, 22].
Figure 1.
Flow diagram of a parallel randomized trial of smoking cessation interventions with Korean Americans
Intervention
All the intervention was delivered in an individual format by a Korean clinician. Approximately 90% of the interventions were delivered by a female clinician who was certified in mental health counseling. Upon request from several Korean women who voiced concerns about the possibility of meeting someone whom they knew, the study site was moved from a Korean community center to an office of a private company. These women had their therapy sessions during off-business hours.
Cultural tailoring of the treatment entailed three elements: (1) explanation of the effects of carbon monoxide (CO) in an analogy of briquette gas poisoning in Korea (see below for the explanation), (2) information on smoking-related death rates in Korea, including recent smoking-related deaths among celebrities in Korea, and (3) utilization of family support. All these components were developed from previous studies [14, 22, 23] and pilot-tested with 22 Korean American smokers (data unpublished). All intervention materials were prepared and delivered in Korean.
Explanation of the effects of CO in an analogy of briquette gas poisoning in Korea
The traditional Korean heating system, called “Ondol,” is one in which direct heat is transferred from a burning coal briquette to the thick masonry floor. The burning briquette often produces a great amount of CO, which used to account for about 50% of all death tolls during winter in Korea [40, 41]. In 2001, approximately 1.5% of households in Korea reported using briquettes [41]. The most watched and talked about Korean drama of 2010 was “Giant,” in which the main male character had lost his mother by the briquette gas poisoning [42]. Many Korean immigrants in the US continue to watch Korean dramas. Thus, participants in this study clearly understood when the harmful effects of CO from smoking were explained with the analogy of the briquette gas poisoning.
Information on smoking-related deaths in Korea
We provided health education, using Korean videotapes showing a variety of smoking-related diseases and compared morbidity and mortality rates of the diseases between smokers and non-smokers in Korea. We also provided information about the highest rate of smoking-attributable cancer deaths found among Korean men in California [6, 7]. Many were very receptive to the information, particularly when they were informed about celebrities [43] in Korea who recently died from lung cancer or other smoking-related diseases.
Utilization of family support in smoking cessation
Korean smokers who perceived strong social norms (family and friends) favoring quitting were more likely to make a serious quit attempt by complying with the norms than those who perceived weak social norms [22, 23]. With the participant’ permission, family members were contacted at least two times (once before and after the quit date) to facilitate their support. Most expressed their strong wish for the participant to quit smoking. They were informed about symptoms of nicotine withdrawal and how to help if the smoker manifested the symptoms. Participants without family members were encouraged to seek support from friends and co-workers.
Intervention condition
Each of the participants in this condition received eight 40-minute weekly sessions of individualized counseling targeting the three TPB variables: attitudes, perceived social norms, and self-efficacy. Each therapy session was structured in a combination of cognitive behavior therapy and cultural tailoring intervention. They also used nicotine patches for eight weeks as recommended by the Public Health Services Guideline [36]. Medication adherence was monitored by counting patches that were returned after use. During the first two sessions, the participant talked about pros and cons of smoking and quitting (decisional balance). In addition, the deleterious effects of smoking, particularly the harmful effects of CO, the addictive nature of nicotine, and immediate health benefits of quitting were addressed. The quit date was set between the second and fourth sessions. The participant and therapist discussed the choice of the date based on the person’s readiness for quitting (self-efficacy in quitting) that was assessed at baseline. Using cognitive behavior therapy, the participant was trained in a variety of skills to help deal with nicotine craving and other withdrawal symptoms. The person was also educated about how to use the nicotine patch correctly and manage its side effects. Interventions during the remaining fifth through seventh sessions were tailored to individual’s needs, as indicated by his or her experience with withdrawal symptoms and progress in abstinence or relapse to smoking. Many talked about their feelings toward the death of a very popular figure in Korea who recently died of lung cancer [43, 44]. In the eighth session, a graduation ceremony was held after the review of the overall process.
Control condition
All the participants in this condition received eight 10-minute weekly sessions of individualized counseling focusing on medication management. Participants could choose any quit date between the second and fourth sessions. They were briefly informed about the deleterious effects of smoking and cognitive behavioral skills that are useful in dealing with smoking craving and withdrawal symptoms. Participants also received nicotine patches for eight weeks. The initial dosage and tapering schedule were based on the U.S. Public Health Services Guideline [36]. Adherence to the medication was monitored by counting used patches.
Assessment
The primary outcome was the 7-day point prevalence abstinence at the 6-month follow-up. Abstinence was defined as having not smoked a single puff for the past seven days. Continuous abstinence, having not smoked a single puff since the quit date, was also assessed at each weekly meeting and follow-up. In addition, breath CO and salivary cotinine tests were analyzed to verify self-reported abstinence.
The CO level was measured by Micro+ Smokerlyzer CO Monitor (Bedfont Scientific, NJ). The salivary cotinine level was assessed by NicAlert® test, which is a semi-quantitative measure of cotinine based on colorimetric immunoassay reaction. The test strip displays seven zones that represent a range of cotinine levels from 0 (0–10 ng/ml) to 6 (≥ 2000 ng/ml). It has been suggested that the two tests are more effective together than either measure alone [45]. More recent findings indicated that CO with a cutoff level of 6 parts per million (ppm) would predict smoking with 100% sensitivity and 100% specificity [46]. The company producing the NicAlert® test recommends the cutoff level of 3 (≥ 100 ng/ml) for the determination of smoking. In contrast, Marrone and colleagues [46] suggested that results ≥ 1 (10–30 ng/ml) indicate tobacco use. In this study, we used results ≤ 1 as not smoking if self-reports and CO levels (lower than 6 ppm) indicated abstinence. The adjustment was made because most participants in the study reported exposure to secondhand smoke at work areas. Similar to our findings, Ma and colleagues [47] found that Korean Americans reported the highest exposure to secondhand smoke and the lowest proportion of employer’s smoking restriction policy at work compared with Chinese, Vietnamese, and Cambodian Americans (p < 0.001).
Measures
All the questionnaires were self-administered in paper and pencil. Prior to their use in the present study, all the measures that were developed in English had been translated and back-translated through a rigorous process and pilot-tested for cross-cultural validation [23, 48–50]. Participants filled out the questionnaire at each follow-up point. Exhaled breath was tested for CO level to assess its correlation with the number of cigarettes smoked per day on average.
Data collection including biochemical tests were done primarily by a research assistant (RA) who was not blinded to study condition. Due to limited resources, only one part-time RA was hired; she entered most of the data and transcribed the audiotaped counseling sessions in both conditions. Thus, it was difficult to conceal the condition to her. When the RA was not available, a clinician who did not deliver the intervention collected data.
Demographic data were gathered with respect to gender, age, marital status, education, annual family income, and religion. Participants were also asked about the presence of other smokers in the household. Smoking and quitting behaviors were gathered in the following areas: age at which participant began smoking regularly, use of other tobacco products, history of past-year quit attempts, and any serious quit attempts that lasted at least 24 hours in the past year.
Acculturation was assessed using the Suinn-Lew Asian Self-Identify Acculturation Scale [51]. The questionnaire consists of 21 items (one’s familiarity with spoken and written languages, and preference for ethnic identity, friends, food, movie, and music). The score of each item ranges from 1, “Korean-culture oriented,” to 5, “American-culture oriented.” The scale score is the mean of the 21-item scores. Cronbach’s alpha was .88 for this study.
Nicotine dependence was assessed using the Fagerström Test for Nicotine Dependence [52]. The total score is the sum of the scores of six items and ranges from 0 to 10. A higher score indicates more dependence on nicotine, and scores of 7 to 10 indicate high dependence. Cronbach’s alpha of a Korean-version FTND was .72 [53], and this Korean-version was used in the present study. Cronbach’s alpha was .51 in the present study.
Alcohol use was assessed using the AUDIT [35]. The measure consists of 10 items and each item scores from 0 to 4. A Cronbach’s alpha of .80 was obtained in the present study.
Depression was assessed using the Center for Epidemiologic Studies-Depression Scale [54], which consists of 20 items. Participants rate how often they experience each symptom over the past week on a 4-point (0–3) scale from “rarely (i.e., once per day) to “most of the time” (i.e., 5–7 days). The total score is the sum of the 20 item scores. Instead of the cutoff score of 16 recommended by Radloff, a cutoff score of 20 was suggested as a better predictor of depression among Koreans [55]. In the present study, Cronbach’s alpha was .93.
Attitudes were assessed using an indirect measure of attitudes the Perceived Risks and Benefits of Quitting Questionnaire [56]. It consists of two subscales: 18 items on perceived risks (e.g., “I will be less able to concentrate,” and “I will miss the taste of cigarettes”) and 22 items on perceived benefit (e.g., “I will smell cleaner,” and “I will feel proud that I was able to quit”). Participants are asked to assess the likelihood of each item would be on a 7-point scale (1 = no chance at all, 7 = certain to happen) if they were to stop smoking. Scores of the items are averaged to estimate the score of each subscale. In this study, Cronbach’s alphas of the Risk and Benefit subscales were .86 and .91, respectively.
Perceived social norms were assessed using a measure consisting of two items regarding normative beliefs (i.e., “I believe that my family [my friends] wants me to quit smoking”) and motivation to comply (i.e., “I am willing to comply with the belief”). My friends included anyone to whom the participant felt very close, regardless of their race and ethnicity. Findings from the previous study [24] indicated that smokers are often conflicted by the discrepancy between the social norms for family and the social norms for friends. Scores for each item ranged from −3 “strongly disagree” to +3 “strongly agree”. The total score was obtained by adding the normative belief and motivation to comply scores. The perceived social norms were not submitted to internal reliability testing, because smokers tend to hold contradictory beliefs [57].
Self-efficacy in quitting was assessed using the Situational Temptation Scale [58]. The measure consists of 17 situational items, and participants can rate, on a 5-point (1–5) scale, their confidence in resisting smoking temptation at each given situation. In the present study, a short version of 10 items adapted for Korean Americans [49] was used and the total score could range from 10 to 50. Cronbach’s alpha was .85 for the present study. In addition, overall quitting self-efficacy was assessed on a 10-point ladder scale ranging from 1 “no confidence at all” to 10 “the highest possible confidence”.
Nicotine withdrawal symptoms were assessed using the Minnesota Nicotine Withdrawal Scale [59]. The scale was later modified to include smoking urges or craving as one of the nine symptoms [60]. Participants rate, on a 4-point (0–3) scale, their experience with the symptoms, yielding the total score between 0 and 36. The scale was administered only after the quit date. A Cronbach’s alpha of .83 was obtained in the present study.
At the end of the program, which was about four weeks after the quit date (six to eight weeks from the baseline assessment), participants were re-assessed on the measures of the TPB variables (attitudes, perceived social norms, and self-efficacy).
Data analysis
Data were analyzed with SPSS for Windows version 18.0. Descriptive statistics were computed for demographics and key study variables. Chi-square test and independent t-test were used to assess differences in demographics, smoking and quitting behavior, and psychosocial variables between treatment conditions and between those who completed the program and those who dropped out. For hypothesis one, a bivariate logistic regression analysis was performed to compare abstinence rates for each study condition at each follow-up. For hypothesis two, a paired t-test was performed to assess any changes in the TPB variables before and after the program. All tests were two-tailed at a 0.05 significance level.
Results
A total of 30 participants (23 men and seven women) were randomized into intervention and control conditions (see Table 1). Participants aged 28 to 70 with a mean age of 46.5 (SD = 10.5). One-third of the participants (33.3%) reported smoking more than 20 cigarettes a day on average. Nine participants (30%) had a score of 7 or more on the FTND, indicating high or very high nicotine dependence. Baseline data showed no differences in demographics, smoking behaviors, and psychosocial variables including the three TPB variables between the two treatment conditions. The only difference was found in the number of serious quit attempts made in the past year; the control condition made more attempts than the intervention condition (t = 2.58, p = 0.02).
Table 1.
Demographic characteristics, smoking behaviors and psychosocial variables by treatment condition (N = 30)
| Variable (possible score range) | Intervention (n = 14) | Control (n = 16) | Total (N = 30) |
|---|---|---|---|
| Mean (SD), N (%) | Mean (SD), N (%) | Mean (SD), N (%) | |
| Age | 46.7 (9.8) | 46.3 (11.4) | 46.5 (10.5) |
| Gender | |||
| Male | 12 (85.7%) | 11 (68.8%) | 23 (76.7%) |
| Female | 2 (14.3%) | 5 (31.3%) | 7 (23.3%) |
| Marital Status | |||
| Married | 11 (78.6%) | 12 (75.0%) | 23 (76.7%) |
| All others | 3 (21.4%) | 4 (25.0%) | 7 (23.3%) |
| Years in Education | 15.1 (3.1) | 14.5 (1.9) | 14.8 (2.5) |
| Years in the US | 16.5 (7.9) | 16.1 (10.9) | 16.3 (9.5) |
| Acculturation (1–5) | 1.8 (0.3) | 1.9 (0.4) | 1.8 (0.4) |
| Age at Smoking Onset | 20.0 (2.8) | 21.6 (5.5) | 20.9 (4.4) |
| Number of Cigarettes Smoked | 19.6 (6.4) | 18.6 (6.6) | 19.0 (6.5) |
| Nicotine Dependence (0–10) | 4.9 (1.7) | 4.9 (2.3) | 4.9 (2.0) |
| Carbon Monoxide level | 27.1 (12.8) | 28.0 (16.8) | 27.6(14.7) |
| Number of Serious Quit Attempts* in the Past Year | 0.8 (0.8) | 1.8 (1.3) | 1.3 (1.2) |
| Alcohol Use (0–40) | 6.8 (5.8) | 5.1 (4.7) | 5.9 (5.2) |
| Depression (0–60) | 11.5 (12.5) | 14.2 (13.3) | 12.9 (12.7) |
| Positive Attitudes (1–7) | 5.9 (0.7) | 5.8 (0.9) | 5.9 (0.8) |
| Negative Attitudes (1–7) | 4.1 (0.9) | 4.4(1.1) | 4.2 (1.0) |
| Perceived Family Norm (−6–+6) | 5.1 (1.2) | 5.3 (1.3) | 5.2 (1.2) |
| Perceived Peer Norm (−6–+6) | 2.8 (2.8) | 3.1 (3.0) | 3.0 (2.9) |
| Self-efficacy (10–50) | 29.2 (7.9) | 30.9 (8.2) | 30.1 (8.0) |
Note,
p = 0.02
Twenty three (76.7%) completed the program and seven (23.3%, three from the intervention and four from the control condition) dropped out. The completion of the program was defined as having attended at least six sessions of the eight weekly session program and having completed the 8-week nicotine patch schedule. Including those who dropped out of the program, the mean number of sessions attended was 5.4 (SD = 1.9) for the intervention condition and 4.8 (SD = 2.3) for the control condition. The difference was not statistically significant. Compared to those who completed the program, those who dropped out had less positive attitudes toward quitting (t = −2.44, p = 0.02), less perceived peer norm favoring quitting (t = −2.61, p = 0.01), and more depressed feelings (t = 2.14, p = 0.04) at baseline. Twenty-three participants (76.7%) were followed-up over six months, and those who were lost were treated as smoking similar to the amount they smoked before the treatment.
Difference in Nicotine Abstinence between the Two Treatment Conditions
Abstinence rates at 4-time points were compared between the treatment conditions (see Table 2). In general, those who received the combination treatment (the intervention condition) were twice as likely to be abstinent compared to those who received brief medication management (the control condition). At the 6-month follow-up, 57.1% of the intervention condition and 18.8% of the control condition were abstinent in the last seven days and the difference was statistically significant (odds ratio [OR] = 5.40, 95% confidence interval [CI] = 1.12–26.04, p = 0.04). The two treatment conditions also differed in continuous abstinence, which showed a large effect size (OR = 4.33, 95% CI = 0.85–22.23, p = 0.08).
Table 2.
Abstinence rates over time by treatment condition (N = 30)
| Time-points | Intervention group (n = 14) | Control group (n = 16) | OR (95% CI)a | ||
|---|---|---|---|---|---|
| 7-days point prevalence | Continuous | 7-days point prevalence | Continuous | ||
| 1 week | 64.3 | 64.3 | 31.3 | 31.3 | 3.96 (0.87, 18.12) |
| 4 weeks | 78.6 | 64.3 | 56.3 | 31.3 | 2.85 (0.57, 14.33) |
| 3 months | 64.3 | 57.1 | 31.3 | 31.3 | 3.96 (0.87, 18.12) |
| 6 months | 57.1 | 50.0 | 18.8 | 18.8 | 5.40 (1.12, 26.04)* |
Note, OR = odds ratio, CI = confidence interval,
= differences in 7-day point prevalence abstinence between the two treatment conditions,
p = 0.036.
There was no discrepancy in abstinence rates between self-reports and biochemical measures (both breath CO and salivary cotinine tests) except for one participant whose cotinine level was above the cutoff point. The cotinine test was repeated in a week but yielded the same result. Thus, he was classified as smoking although his breath CO levels were 3–5ppm. The participant stated that secondhand smoke at work might be a possible cause for the high cotinine level. According to him, a coworker who used the desk next to his was a heavy smoker. Those who reported abstinence when called but did not participate in biochemical testing were treated as smoking except for one participant who was relocated in Texas. The person had been continuously abstinent from the quit date and thus he was treated as not smoking.
Changes in the TPB Variables after the Intervention
Compared to baseline, negative attitudes (perceived risks of quitting) showed a significant decrease (t = − 4.97, p = 0.00) and self-efficacy showed a significant increase (t = 5.03, p = 0.00) at the end of the program. Although the changes were more pronounced in the intervention than in the control, the difference was not statistically significant. On the other hand, positive attitudes (perceived benefits of quitting) and perceived social norms (both family and peer) showed no changes from the baseline. The odds of being abstinent were high for those with high levels of self-efficacy (OR = 1.46, 95% CI = 1.09–1.96, p = 0.02) and low scores of depression (OR = 0.91, 95% CI = 0.85–0.98, p = 0.01) at baseline.
Discussion
Half of the participants who received the cognitive behavior and cultural tailoring intervention were able to quit smoking and maintain abstinence over time. Those who received the intervention had more than five times the odds of being abstinent at the 6-month follow-up compared to those who received the brief medication management. The difference between the two treatment conditions seemed to be larger than those found in other studies comparing groups with similar treatment intensity. For example, biochemically confirmed abstinence rates at 9-, 26-, and 52-week follow-ups were 45%, 37%, and 35% respectively in a study of 12-week individualized cognitive behavior therapy sessions along with 8-week NRT [61]. A meta-analysis of 18 studies providing four to eight sessions of counseling in combination with medication yielded an odds ratio of 1.3 (95% CI = 1.1–1.5) compared to medication only intervention [36]. Given this, the relatively large effect size might suggest practical significance of the combination treatment over the brief medical management [62].
Participants in both conditions showed a decrease in negative attitudes (perceived risks of quitting) and an increase in self-efficacy after the treatment. In contrast, there were no significant changes in positive attitudes (perceived benefits of quitting) and perceived social norms. Most participants expressed that they experienced less withdrawal symptoms or less severity of the symptoms even if they had compared to their experiences in previous quit attempts, which might have affected the change in negative attitudes and self-efficacy. These findings are consistent with the result that participants treated with nicotine patches reported fewer withdrawal symptoms and increased self-efficacy than those who did not use the patches [63]. In accordance with the high level of education, participants in this study appeared to be cognizant of the health benefits associated with quitting even prior to their participation in the program. Thus, it is not surprising that there was no significant change in positive attitudes toward quitting. Smokers who perceived strong social norms favoring quitting were more likely to come for the treatment [23, 24]. Thus, the perceived social norms might be less likely to change after the treatment due to the ceiling effect. Another possible reason might be related to the small sample size of the present study.
The analogy of the briquette gas poisoning seemed to facilitate the participants’ understanding of the detrimental effect of CO on the body. The use of data from people in Korea and Korean Americans also might have affected, to some extent, the participants’ decision to maintain abstinence. Most participants had been aware of the smoking-attributable deaths of popular stars in Korea. They talked about how surprising was the recent death of a singer who died from lung cancer in January 2010 [43, 44].
Many wives of male smokers participated in the study and attended the treatment session with husbands at least once. The wives were very supportive and vigilant in monitoring husband’s adherence to nicotine patches. However, utilization of family support was not practical for female smokers. Most married women had husbands who smoked but were not interested in quitting. Pollak et al. [64] found that women’s smoking cessation was predicted only when both women’s and male partners’ supports were taken into consideration. The utilization of family support was not successful for single women, either. They refused seeking the support, stating that none in the family knew of their smoking.
Interestingly, CO levels (mean = 28, SD = 14.7) measured were relatively high compared to the mean number of cigarettes smoked per day (mean = 19, SD = 6.5). For example, the mean level of breath CO was 17 ppm (SD = 9.7) among African Americans and 25 ppm (SD = 12.8) among European Americans who reported smoking 16 and 22 cigarettes a day on average, respectively [46]. The CO yield per cigarette was 1.45 for Korean Americans in this study, whereas it was 1.06 for African Americans and 1.14 for European Americans. More studies are needed to examine whether there are any racial or ethnic differences in smoking topography. The difference also might be related to other factors such as exposure to secondhand smoke at work. Many in the present study reported that they had been exposed to secondhand smoke at work (i.e., offices or stores), which is similar to findings from the study by Ma and colleagues [65].
The present study has several limitations. The sample size is too small to determine the efficacy of the cognitive behavior therapy and cultural tailoring intervention in Korean Americans over the brief medication management. The differing length of treatment between the two conditions might have affected the large effect size. The findings are also limited in its applicability to Korean Americans who were born in the US given that all the participants were immigrants. Nevertheless, several findings were noteworthy. First, the effect of the culturally tailored cognitive behavior therapy intervention yielded a large effect size over the control condition and the treatment effect lasted over the 6-month follow-up. More studies are needed to determine whether the effect is related to the cultural tailoring or the longer time allotted for counseling sessions in the intervention condition. Similar to findings for other racial and ethnic groups, it seems that family support, particularly the partner’s support, is important for Korean Americans’ successful smoking cessation and abstinence. Third, the findings also support the use of both CO and saliva cotinine tests for the verification of self-reported abstinence. These findings need to be further tested with a larger sample size and longer follow-ups for possible implications in clinical settings.
Contributor Information
Sun S Kim, Email: sun.kim@umassmed.edu, University of Massachusetts Medical School, Department of Psychiatry.
Seong-Ho Kim, Email: seonghony@yahoo.co.kr, Fordham University, Graduate School of Social Service.
Douglas Ziedonis, Email: Douglas.ziedonis@umassmemorial.org, University of Massachusetts Medical School, Department of Psychiatry.
References
- 1.An N, Cochran SD, Mays VM, McCarthy WJ. Influence of American acculturation on cigarette smoking behaviors among Asian American subpopulations in California. Nicotine & Tobacco Research. 2008;10(4):579–87. doi: 10.1080/14622200801979126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baluja KF, Park J, Myers D. Inclusion of immigrant status in smoking prevalence statistics. Research and Practice. 2003;93:642–6. doi: 10.2105/ajph.93.4.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SS, Ziedonis D, Chen KW. Tobacco use and dependence in Asian Americans: a review of the literature. Nicotine & Tobacco Research. 2007;9(2):169–84. doi: 10.1080/14622200601080323. [DOI] [PubMed] [Google Scholar]
- 4.Ma GX, Shive S, Tan Y, Toubbeh J. Prevalence and predictors of tobacco use among Asian Americans in the Delaware Valley region. American Journal of Public Health. 2002;92(6):1013–20. doi: 10.2105/ajph.92.6.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Vital signs: current cigarette smoking among adults aged > or = 18 years --- United States, 2009. Morbidity and Mortality Weekly Report. 2010;59(35):1135–40. [PubMed] [Google Scholar]
- 6.Kwong SL, Chen MS, JR, Snipes KP, Bal DG, Wright WE. Asian subgroups and cancer incidence and mortality rates in California. Cancer. 2005;104(12 Suppl):2975–81. doi: 10.1002/cncr.21511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leistikow BN, Chen M, Tsodikov A. Tobacco smoke overload and ethnic, state, gender, and temporal cancer mortality disparities in Asian Americans and Pacific Islander-Americans. Preventive Medicine. 2006;42:430–34. doi: 10.1016/j.ypmed.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 8.Song YJ, Hofstetter CR, Hovell MF, Paik HY, Park HR, Lee J, Irvin V. Acculturation and health risk behaviors among Californians of Korean descent. Preventive Medicine. 2004;39:147–56. doi: 10.1016/j.ypmed.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Cho HJ, Khang YH, Jun HJ, Kawachi I. Marital status and smoking in Korea: the influence of gender and age. Social Science & Medicine. 2008;66(3):609–19. doi: 10.1016/j.socscimed.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Khang YH, Yun SC, Cho HJ, Jung-Choi K. The impact of governmental antismoking policy on socioeconomic disparities in cigarette smoking in South Korea. Nicotine & Tobacco Research. 2009;11:262–9. doi: 10.1093/ntr/ntn036. [DOI] [PubMed] [Google Scholar]
- 11.Wewers ME, Ahijevych KL, Dhatt RK, Guthrie RM, Kuun P, Mitchell L, Moeschberger ML, Chen MS., Jr Cotinine levels in Southeast Asian smokers. Nicotine & Tobacco Research. 2000;2(1):85–91. doi: 10.1080/14622200050011349. [DOI] [PubMed] [Google Scholar]
- 12.Burgess D, Fu SS, Joseph AM, Hatsukami DK, Solomon J, van Ryn M. Understanding smoking and cessation among Hmong smokers. Journal of Health Care for the Poor and Underserved. 2008;19(2):442–51. doi: 10.1353/hpu.0.0022. [DOI] [PubMed] [Google Scholar]
- 13.Fang CY, Ma GX, Miller SM, Tan Y, Su X, Shives S. A brief smoking cessation intervention for Chinese and Korean American smokers. Preventive Medicine. 2006;43(4):321–4. doi: 10.1016/j.ypmed.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Kim SS, Kwon M, Klessig YC, Ziedonis D. Adapting tobacco dependence group therapy treatment for Korean Americans: A case report of a pilot treatment program. Journal of Group Therapy in Addiction and Recovery. 2008;3(2):93–108. [Google Scholar]
- 15.McDonnell DD, Kazinets G, Lee HJ, Moskowitz JM. An Internet-based smoking cessation program for Korean Americans: Results from a randomized controlled trial. Nicotine & Tobacco Research. 2011 Feb 4; doi: 10.1093/ntr/ntq260. [DOI] [PubMed] [Google Scholar]
- 16.Ajzen I. Attitudes, personality, and behavior. Chicago: Dorsey Press; 1988. [Google Scholar]
- 17.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- 18.Brugged D, Dejong W, Hyde J, Le Q, Shih CS, Wong A, Tran A. Development of targeted message concepts for recent Asian immigrants about secondhand smoke. Journal of Health Communication. 2002;7(1):25–37. doi: 10.1080/10810730252801174. [DOI] [PubMed] [Google Scholar]
- 19.Perez-Stable EJ, Marin G, Posner SF. Ethnic comparison of attitudes and beliefs about cigarette smoking. Journal of General Internal Medicine. 1998;13:167–74. doi: 10.1046/j.1525-1497.1998.00051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caudill W, Schooler C. Child behavior and child rearing in Japan and the U.S. Journal of Nervous and Mental Disease. 1973;157:323–38. doi: 10.1097/00005053-197311000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Kim SS. The experiences of young Korean immigrants: A grounded theory of negotiating social, cultural, and generational boundaries. Issues in Mental Health Nursing. 2004;25:517–38. doi: 10.1080/01612840490443464. [DOI] [PubMed] [Google Scholar]
- 22.Kim SS, Son H, Nam KA. The sociocultural context of Korean American men’s smoking behavior. Western Journal Nursing Research. 2005;27(5):604–23. doi: 10.1177/0193945905276258. [DOI] [PubMed] [Google Scholar]
- 23.Kim SS. Predictors of short-term smoking cessation among Korean American men. Public Health Nursing. 2008;25(6):516–25. doi: 10.1111/j.1525-1446.2008.00738.x. [DOI] [PubMed] [Google Scholar]
- 24.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 25.Broadhead-Fearn D, White KM. The role of self-efficacy in predicting rule-following behaviors in shelters for homeless youth: a test of the theory of planned behavior. Journal of Social Psychology. 2006;146(3):307–25. doi: 10.3200/SOCP.146.3.307-325. [DOI] [PubMed] [Google Scholar]
- 26.Tolma EL, Reininger BM, Evans A, Ureda J. Examining the theory of planned behavior and the construct of self-efficacy to predict mammography intention. Health Education Behavior. 2006;33(2):233–51. doi: 10.1177/1090198105277393. [DOI] [PubMed] [Google Scholar]
- 27.Niven A, Nevill A, Sayers F, Cullen M. Predictors of rehabilitation intention and behavior following anterior cruciate ligament surgery: an application of the Theory of Planned Behavior. Scandinavian Journal of Medicine & Science in Sports. 2010;7 doi: 10.1111/j.1600-0838.2010.01236.x. [DOI] [PubMed] [Google Scholar]
- 28.Armitage CJ, Conner M. Efficacy of the theory of planned behavior: A meta-analytic review. British Journal of Social Psychology. 2001;40:471–99. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 29.Kim KK, Yu ESH, Chen EH, Kim J, Brintnall RA, Vance S. Smoking behavior, knowledge, and beliefs among Korean Americans. Cancer Practice. 2000;8:223–30. doi: 10.1046/j.1523-5394.2000.85006.x. [DOI] [PubMed] [Google Scholar]
- 30.Lew R, Moskowitz JM, Wismer BA, Min K, Kang SH, Chen AM, Tager IB. Correlates of cigarette smoking among Korean American adults in Alameda County, California. Asian American and Pacific Islander Journal of Health. 2001;19:50–60. [PubMed] [Google Scholar]
- 31.Hofstetter CR, Ayers JW, Irvin VL, Kang SDE, Hughes SC, Reighard F, Hovell MF. Does church participation facilitate tobacco control? A report on Korean immigrants. Journal of Immigrant & Minority Health. 2010;12(2):187–97. doi: 10.1007/s10903-009-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Juon H, Kim M, Han H, Ryu JP, Han W. Acculturation and cigarette smoking among Korean American men. Yonsei Medical Journal. 2003;4:875–82. doi: 10.3349/ymj.2003.44.5.875. [DOI] [PubMed] [Google Scholar]
- 33.Kim O. The relationship of depression to health risk behaviors and health perceptions in Korean college students. Adolescence. 2002;37(147):575–83. [PubMed] [Google Scholar]
- 34.Park S. Smoking behavior and predictors of smoking initiation in childhood and early adolescence. Journal of Korean Academy Nursing. 2009;39(3):376–85. doi: 10.4040/jkan.2009.39.3.376. [DOI] [PubMed] [Google Scholar]
- 35.Saunders JB, Aasland OG, Babor TF, De La Fuente JR, MG Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 36.Fiore MC, Jaen CR, Baker TB, Bailey WC, Bennett G, Benowitz NL, et al. Clinical Practice Guideline. Rockville, MD: USDHHS, U.S. Public Health Services; 2008. Treating tobacco use and dependence: 2008 Update. [Google Scholar]
- 37.Carpenter MJ, Upadhyaya HP, LaRowe SD, Saladin ME, Brady KT. Menstrual cycle phase effects on nicotine withdrawal and cigarette craving: a review. Nicotine & Tobacco Research. 2006;8:627–38. doi: 10.1080/14622200600910793. [DOI] [PubMed] [Google Scholar]
- 38.Schnoll RA, Patterson F, Lerman C. Treating tobacco dependence in women. Journal of Women’s Health. 2007;16:1211–8. doi: 10.1089/jwh.2006.0281. [DOI] [PubMed] [Google Scholar]
- 39.Piper ME, Cook JW, Schlam TR, Jorenby DE, Smith SS, Bolt DM, Loh WY. Gender, race, and education differences in abstinence rates among participants in two randomized smoking cessation trials. Nicotine & Tobacco Research. 2010;12(6):647–57. doi: 10.1093/ntr/ntq067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim YS. Seasonal variation in carbon monoxide poisoning in urban Korea. Journal of Epidemiology and Community Health. 1985;39:79–81. doi: 10.1136/jech.39.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lankov A. Times TK, editor. At the coalface of heating. Opinion. 2007 Available from http://www.koreatimes.co.kr/www/news/opinon/2011/02/165_5149.html.
- 42.Fandom K WorldPress.com Ba. SBS Giant. Cocorust Repository. 2010 Available from http://co2r.wordpress.com/2010/05/10/sbs10-giant/
- 43.Han SH. Times TK, editor. Rock singer Lee Nam-yi passed away. Special. 2010 Available from http://www.koreatimes.co.kr/www/news/special/2010/05/178_59979.html.
- 44.Lee IM DognA.Com. [The death of singer Yee Nam Yi who sang “I Want to Cry”.] Available from http://news.donga.com/Enter/3/06/20100130/25804314/1.
- 45.Acosta M, Buchhalter A, Breland A, Hamilton D, Eissenberg T. Urine cotinine as an index of smoking status in smokers during 96-hr abstinence: comparison between gas chromatography/mass spectrometry and immunoassay test strips. Nicotine & Tobacco Research. 2004;6(4):615–20. doi: 10.1080/14622200410001727867. [DOI] [PubMed] [Google Scholar]
- 46.Marrone GF, Paulpillai M, Evans RJ, Singleton EG, Heishman SJ. Breath carbon monoxide and semiquantitative saliva cotinine as biomarkers for smoking. Human Psychopharmacology. 2010;25(1):80–3. doi: 10.1002/hup.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ma GX, Tan Y, Fang CY, Toubbeh JI, Shive SE. Knowledge, attitudes and behavior regarding secondhand smoke among Asian Americans. Preventive Medicine. 2005;41(2):446–53. doi: 10.1016/j.ypmed.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 48.Kim SS, Gulick EE, Kim SH, Seo HG. Psychometric properties of the Minnesota Nicotine Withdrawal Scale: a Korean version. Journal of Nursing Measurement. 2007;15(2):121–32. doi: 10.1891/106137407782156354. [DOI] [PubMed] [Google Scholar]
- 49.Kim SS, Kim SH, Gulick EE. Cross-cultural validation of a smoking abstinence self efficacy scale in Korean American men. Issues in Mental Health Nursing. 2009;30(2):122–30. doi: 10.1080/01612840802370582. [DOI] [PubMed] [Google Scholar]
- 50.Kim SS, Gulick EE, Nam KA, Kim SH. Psychometric properties of the alcohol use disorders identification test: a Korean version. Archives of Psychiatric Nursing. 2008;22(4):190–9. doi: 10.1016/j.apnu.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 51.Suinn RM, Rickard-Figueroa K, Lew S, Vigil P. The Suinn-Lew Asian Self-Identity Acculturation Scale: An initial report. Educational and Psychological Measurement. 1987;47(2):401–7. [Google Scholar]
- 52.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1989;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 53.Park SM, Son KY, Lee YJ, Lee HC, Kang JH, Lee YJ, Chang YJ, Yun YH. A preliminary investigation of early smoking initiation and nicotine dependence in Korean adults. Drug and Alcohol Dependence. 2004;74:197–203. doi: 10.1016/j.drugalcdep.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 54.Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 55.Cho MJ, Kim KH. Use of the Center for Epidemiologic Studies Depression (CES-D) Scale in Korea. The Journal of Nervous and Mental Diseases. 1998;186:304–10. doi: 10.1097/00005053-199805000-00007. [DOI] [PubMed] [Google Scholar]
- 56.McKee SA, O’Malley SS, Salovey P, Krishan-Sarin S, Mazure CM. Perceived risks and Benefits of smoking cessation: Gender-specific predictors of motivation and treatment outcome. Addictive Behaviors. 2005;30:423–35. doi: 10.1016/j.addbeh.2004.05.027. [DOI] [PubMed] [Google Scholar]
- 57.Burkhalter JE, Warren B, Shuk E, Primavera L, Ostroff JS. Intention to quit smoking among lesbian, gay, bisexual, and transgender smokers. Nicotine & Tobacco Research. 2009;11(11):1312–20. doi: 10.1093/ntr/ntp140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Velicer WF, Diclemente CC, Rossi JS, Prochaska JO. Relapse situations and self-efficacy: an integrative model. Addictive Behaviors. 1990;15:271–83. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- 59.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43:289–94. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 60.Jorenby DE, Hatsukami DK, Smith SS, Fiore MC, Allen S, Jensen J, BAKER TB. Characterization of tobacco withdrawal symptoms: Transdermal nicotine reduces hunger and weight gain. Psychopharmacology (Berl) 1996;128:130–8. doi: 10.1007/s002130050118. [DOI] [PubMed] [Google Scholar]
- 61.Alterman AI, Gariti P, Mulvaney F. Short- and long-term smoking cessation for three levels of intensity of behavioral treatment. Psychology of Addictive Behavior. 2001;15(3):261–4. [PubMed] [Google Scholar]
- 62.Kirk RE. Practical significance: A concept whose time has come. Educational and Psychological Measurement. 1996;56(5):746. [Google Scholar]
- 63.Cinciripini PM, Cinciripini LG, Wallfisch A, Haque W, Van Vunakis H. Behavior therapy and the transdermal nicotine patch: effects on cessation outcome, affect, and coping. Journal of Consulting and Clinical Psychology. 1996;64(2):314–23. doi: 10.1037//0022-006x.64.2.314. [DOI] [PubMed] [Google Scholar]
- 64.Pollak KI, Baucom DH, Stanton S, Peterson BL, Ostbye T, Palmer CA. Couples‘ reports of support for smoking cessation predicting women’s late pregnancy cessation. American Journal of Health Promotion. 2006;21(2):90–6. doi: 10.4278/0890-1171-21.2.90. [DOI] [PubMed] [Google Scholar]
- 65.Ma GX, Shive SE, Tan Y, Toubbeh JI, Fang CY, Edwards RL. Tobacco use, secondhand smoke exposure and their related knowledge, attitudes and behaviors among Asian Americans. Addictive Behaviors. 2005;30(4):725–40. doi: 10.1016/j.addbeh.2004.08.018. [DOI] [PubMed] [Google Scholar]