Abstract
Objective
The current study investigated whether emotion dysregulation (ED; difficulties in the self-regulation of affective states) mediated relations between anxiety sensitivity (AS; fear of anxiety and related sensations) and cognitive-based smoking processes.
Method
Participants (n = 197; 57.5% male; Mage = 38.0) were daily smokers recruited as part of a randomized control trial for smoking cessation.
Results
AS was uniquely associated with all smoking processes. Moreover, ED significantly mediated relations between AS and the smoking processes.
Conclusions
Findings suggest that ED is an important construct to consider in relations between AS and cognitive-based smoking processes among adult treatment-seeking smokers.
Keywords: Anxiety Sensitivity, Smoking, Emotion Dysregulation, Expectancies
Anxiety sensitivity (AS), defined as the extent to which individuals believe anxiety and anxiety-related sensations have harmful consequences1,2 is a relatively stable, yet malleable, cognitive characteristic that predisposes individuals to the development and maintenance of anxiety psychopathology3. Historically, AS has been studied in relation to better understanding the etiology and maintenance of anxiety and its disorders, particularly panic and posttraumatic stress disorder4–11. More recent work has suggested that AS also may play a role in certain substance use disorders12–15.
One emerging and promising line of inquiry within this substance use domain has focused on the relation between AS and cigarette smoking. For example, AS is significantly associated with less success during smoking cessation attempts16. Specifically, higher levels of AS are related to significantly greater odds of early lapse and relapse during quit attempts17,18. In terms of cognitive-based smoking processes, AS is positively correlated with smoking to reduce negative affect, but often not other smoking motives (e.g., pleasure, handling, taste19–22. Other studies have found that AS is related to expectancies for negative affect reduction23,24. Additionally, smokers high in AS perceive the prospect of quitting as a more difficult and personally threatening experience25, endorsing overall greater perceived barriers to smoking cessation.
Despite the documented association between AS and cognitive-based smoking processes (i.e., beliefs about and reasons underlying smoking behavior; perceived barriers to cessation), there is little understanding of possible mediators of this relation. The identification of potential mediating variables is notable for at least two key reasons. First, by developing an understanding of mediating processes, we can gain a clearer understanding of the pathway(s) through which AS affects smoking-based processes; an important next step in further refining current theoretical models of AS-smoking relations16. Second, explicating these explanatory mechanisms is essential to translating basic research knowledge about AS and smoking to advances in specialized behavioral and pharmacologic smoking cessation interventions for smokers with anxiety and mood-related vulnerability (e.g., elevated anxiety and depressive symptoms16). Thus, there is a need to elucidate the explanatory mediating mechanisms underlying the relations between AS and cognitive-based smoking processes.
Emotion dysregulation represents a promising integrative construct of increasing scholarly interest in anxiety psychopathology and substance use disorder comorbidity research26–29. Previous empirical work has conceptualized healthy emotion regulatory processes as involving the (a) awareness of emotional states, (b) acceptance of emotional states, (c) ability to behave in accordance with personal goals even in the face of experiencing negative emotional states (e.g., anxiety), and (d) ability to use adaptive emotion regulation strategies in a flexible manner in order to meet personal goals and situational demands30. However, demonstrating a deficit in any one of these skills suggests the presence of emotion dysregulation (i.e., difficulties in emotion regulation30). Past non-smoking oriented work has indicated that AS and emotion dysregulation represent theoretically and empirically distinct explanatory constructs31. Yet, related work suggests that the way in which individuals monitor and manage the various manifestations of anxiety (e.g., cognitive or physical) may have an exacerbating or modulating effect32,33. That is, responding to anxiety-related symptoms with less acceptance and fewer emotion regulatory strategies results in greater distress33, whereas responding to anxiety-related symptoms with observation and acceptance results in less distress32. Although there has historically been limited work on emotion dysregulation and smoking, available studies have found that higher levels of emotion dysregulation are related to greater endorsement of certain beliefs about the effects of smoking (i.e., negative reinforcement/negative affect reduction outcome expectancies34) as well as perceived barriers to cessation35. Collectively, such data highlight empirically and clinically significant relations between AS, emotion dysregulation, and cognitive-based smoking processes.
As informed by integrative theoretical models of anxiety and smoking comorbidity16, individuals who fear the negative consequences of anxiety-related sensations may be more likely to respond to such sensations with overall less awareness and acceptance, thereby producing greater levels of distress. Further, in the absence of adaptive emotion regulatory strategies, such persons may learn to rely on smoking to manage negative mood states in the short-term, resulting in certain beliefs about the negatively reinforcing effects of smoking (i.e., negative effect reduction), making the prospect of quitting smoking an overall more threatening experience. Thus, from this perspective, a formative next research step is to evaluate whether emotion dysregulation mediates (explains) the association between AS and cognitive-based smoking processes among adult treatment-seeking daily smokers. Consistent with contemporary models of mediation36, this hypothesized association is tested by the examination of emotion dysregulation as a mediator of the relation between AS and cognitive-based smoking processes (i.e., beliefs about and motives underlying smoking behavior; perceived barriers to cessation). Here, a significant relation between the predictor (i.e., AS) and the criterion (i.e., cognitive-based smoking processes) is said to be mediated when the introduction of a third variable (i.e., emotion dysregulation) results in the non-significance of the initial relation37.
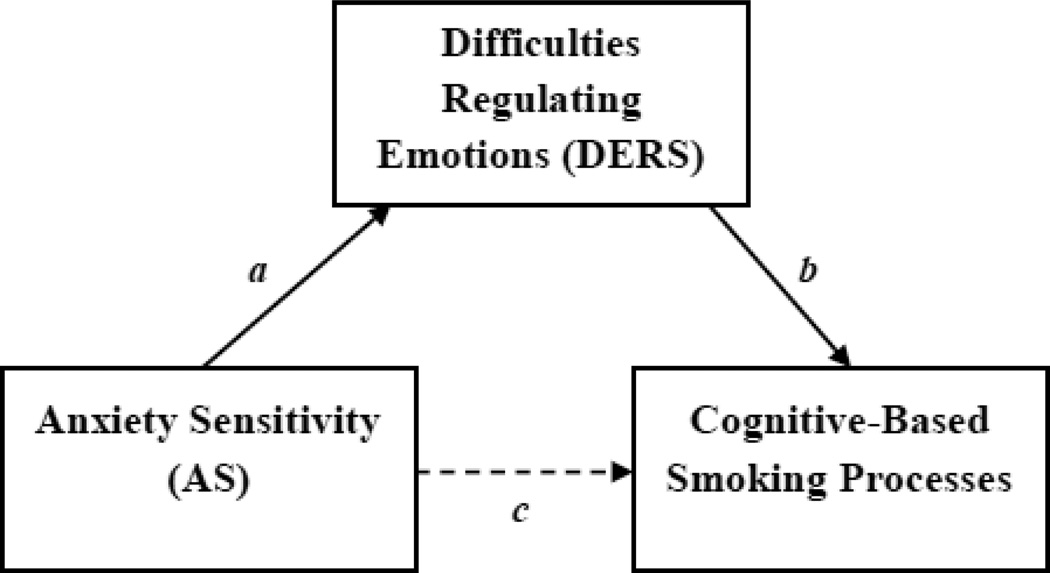
Together, the current study tested the hypotheses that, among adult treatment-seeking daily smokers, greater levels of AS would significantly predict greater endorsement of a) negative reinforcement/negative affect reduction smoking outcome expectancies; b) negative affect reduction smoking motives; and c) perceived barriers for smoking cessation. All effects were expected to be evident above and beyond the variance accounted for by average number of cigarettes smoked per day, marijuana use in the past 30 days, alcohol consumption, number of current Axis I diagnoses, panic attack history, and participant sex; factors known to covary with AS, emotion dysregulation, and smoking35,21. Moreover, it was further hypothesized that emotion dysregulation would mediate (explain) the relation between AS and the studied smoking processes (see Figure 1).
Figure 1.
Proposed mediational model of emotion dysregulation mediating anxiety sensitivity and cognitive-based smoking processes
Method
Participants
Participants included 197 adult daily smokers (57.5% male; Mage = 38.0; SD = 12.8), whom were recruited to participate in a randomized control trial examining the efficacy of a 4-session smoking-based behavioral intervention program focused on emotional vulnerability in comparison to standard pharmacological and psychosocial care. In terms of ethnic background, 170 participants identified as Caucasion, 17 identified as African-American, 4 identified as Hispanic, 2 identified as Asian, and 4 identified as “other.” Participants reported smoking an average of 20.5 cigarettes per day (SD = 12.6), smoking their first cigarette at 14.6 years of age (SD = 3.8), and smoking regularly at 17.4 years of age (SD = 4.1). Moreover, participants endorsed moderate levels of nicotine dependence, as indexed by a score of 5.7 (SD = 2.1) on the Fagerstrom Test for Nicotine Dependence (FTND38). Nearly all participants (93.1%) reported making at least one previous attempt to quit smoking, endorsing an average of 3.4 (SD = 2.5) ‘serious’ lifetime quit attempts.
As assessed by the Structured Clinical Interview for DSM-IV Axis I Disorders-Non-Patient Version (SCID-I-N/P39), 38.7% of the sample met criteria for current (past month) Axis I psychopathology. Participants endorsing current psychopathology met criteria for an average of 1.94 (SD = 1.18) diagnoses. Specifically, 12.7% of the total sample met criteria for major depressive disorder, 6.4% met criteria for dysthymia, 1.9% met criteria for other depression-related disorder(s) (e.g., bipolar disorder, depressive disorder NOS), 21.7% met criteria for social anxiety disorder, 13.4% met criteria for a specific phobia, 3.8% met criteria for obsessive-compulsive disorder, 9.6% met criteria for generalized anxiety disorder, 8.3% met criteria for panic disorder with or without agoraphobia, 8.3% met criteria for posttraumatic stress disorder, 3.2% met criteria for anxiety disorder NOS, .6% met criteria for an eating disorder, 12.7% met criteria for alcohol abuse or dependence, 9.6% met criteria for marijuana abuse or dependence, and 3.8% met criteria for other substance abuse or dependence (e.g., opiate). Additionally, 44.1% of the sample met criteria for past 2-year, unexpected panic attacks.
Participants were deemed eligible for participation if they were 18 years or older, reported smoking an average of 10 or more cigarettes per day for at least one year, and provided a confirmatory Carbon Monoxide breath sample of at least 10 ppm at the baseline session. Exclusion criteria included: endorsement of current or past psychotic-spectrum symptoms via structured interview screening; current suicidality or homicidality; and limited mental competency or inability to provide informed, voluntary, written consent.
Measures
Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-I-N/P39)
Diagnostic assessments were conducted using the SCID-I-N/P (Non-Patient Version39) SCID-I-N/P interviews were administered by trained research assistants or doctoral level staff and supervised by independent doctoral-level professionals. Interviews were audio-taped and the reliability of a random selection of 12.5% of interviews were checked (MJZ) for accuracy; no cases of (diagnostic coding) disagreement were noted. The SCID-N/P follows the DSM-IV-TR diagnosis guidelines and demonstrates good psychometric properties40,41. In the current study, the SCID-N/P was employed to document psychopathology for the inclusionary/exclusionary criteria and history of panic attacks. In addition, the present investigation utilized a composite score, which was generated by summing the number of current Axis I diagnoses, to account for the severity of psychopathology.
Smoking History Questionnaire (SHQ42)
The SHQ is a self-report measure used to collect descriptive information regarding smoking history and pattern. The SHQ has been used in previous studies as a measure of smoking history (e.g., onset of regular smoking), pattern (e.g., number of cigarettes consumed per day), past quit attempts (e.g., how many times in your life have you made a serious quit attempt [rated on 0–9 scale where if more than 9 attempts were made, participants indicate 9], and problematic symptoms experienced during quitting (e.g., weight gain, nausea, irritability, and anxiety42,43. The current study used the SHQ to measure descriptive smoking history variables (e.g., current smoking rate and age of smoking onset; see Participants section).
Fagerstrom Test for Nicotine Dependence (FTND38)
The FTND is a well-established six-item measure designed to assess varying levels of tobacco dependence. This measure has demonstrated good psychometric properties, including internal consistency, positive associations with relevant smoking variables (e.g. salivary cotinine38,44), and high test-retest reliability45. Internal consistency in the present sample was in the range that is typical for the FTND (Cronbach’s α = .57).
Carbon Monoxide
Biochemical verification of smoking status was completed by Carbon Monoxide (CO) analysis of breath samples (10 ppm cutoff46). Expired air CO levels were assessed using a CMD/CO Carbon Monoxide Monitor (Model 3110; Spirometrics, Inc.).
Alcohol Use Disorders Identification Test (AUDIT47)
The AUDIT is a ten-item self-report measure developed by the World Health Organization to identify individuals with alcohol problems47. There is a large body of literature attesting to the reliability and validity of the AUDIT48. In the present investigation, the frequency and quantity items from the AUDIT were used to index current alcohol consumption (an average frequency-by-quantity composite score49. Internal consistency was very good within the current sample (Cronbach’s α = .85).
Marijuana Smoking History Questionnaire (MSHQ50)
The MSHQ is a self-report measure designed to collect descriptive information regarding marijuana use history and pattern (e.g., rate of use, age of first use). Consistent with past research51,17, the current study utilized the single item assessing past 30-day marijuana use.
Anxiety Sensitivity Index-III (ASI-III52)
The ASI-III is an 18-item self-report measure in which respondents indicate, on a 5-point Likert-type scale (0 = very little to 4 = very much), the degree to which they are concerned about possible negative consequences of anxiety-related symptoms (e.g., “It scares me when my heart beats rapidly”). ASI-III items were derived from the Anxiety Sensitivity Index (ASI53) and the Anxiety Sensitivity Index – Revised (ASI-R54). ASI-III and its subscales demonstrated strong and improved reliability and factorial validity relative to previous measures of the construct; as well as convergent, discriminant, and criterion-related (known-group) validity52. In the present study, the total (global) score was used as the primary independent variable. Internal consistancy was found to be excellent within the current sample (Cronbach’s α = .93).
Difficulties in Emotion Regulation Scale (DERS30)
The DERS is a 36-item self-report measure that assesses, on a 5-point Likert-type scale (1 = Almost never to 5 = Almost always), the degree to which respondents experience dysregulated emotional states (“I experience my emotions as overwhelming and out of control”). Items on the DERS yield a total score as well as six subscale scores: Non-Acceptance of Emotional Responses, Difficulties Engaging in Goal-Directed Behavior, Impulse Control Difficulties, Lack of Emotional Awareness, Access to Emotion Regulation Strategies, and Lack of Emotional Clarity. The DERS demonstrates strong psychometric properties, including internal consistency, test–retest reliability, as well as construct and predictive validity30,55. In the current study, the total score was used as the proposed mediator variable (Cronbach’s α = .83 in the present sample).
Smoking Consequences Questionnaire (SCQ56)
The SCQ is a 50-item self-report measure that assesses smoking expectancies on a 10-point Likert-type scale on likelihood of occurrence (0 = completely unlikely to 9 = completely likely). The SCQ yields four factors (i.e., Positive Reinforcement, Negative Reinforcement/Negative Affect Reduction, Negative Consequences, and Appetite Control); however, the current study only utilized the Negative Reinforcement/Negative Affect Reduction subscale (SCQ-NR; e.g., “If I’m feeling irritable, a smoke will help me relax”), owing to its theoretical relevance to the study objectives. This measure has strong psychometric properties56–58, and the SCQ-NR subscale demonstrated excellent internal consistency in the present sample (Cronbach’s α = .93).
Reasons for Smoking (RFS59)
The RFS is a self-report measure consisting of 23 items, rated on a 5-point Likert-type scale (1 = Never to 5 = Always), used to assess smoking motives. The RFS yields a total score, along with six subscale scores (i.e., Habitual, Addictive, Negative Affect Reduction, Relaxation, Sensorimotor, and Stimulation). In the current study, only the Negative Affect Reduction subscales (RFS-NA; e.g., “When I feel uncomfortable or upset about something, I light up a cigarette”) was utilized. The psychometric properties of this scale, including measures of factor structure, internal consistency, and test-retest reliability, have been well established60. In addition, the RFS-NA subscale demonstrated very good internal consistency within the present sample (Cronbach’s α = .88).
Barriers to Cessation Scale (BCS61)
The BCS is a 19-item measure on which respondents indicate, on a 4-point Likert-type scale (0 = not a barrier or not applicable to 3 = large barrier), the extent to which they identify with each of the listed barriers to cessation (e.g., “Fear of failing to quit”). This measure yields a total score as well as three subscale scores (i.e., Addictive Barriers, External Barriers, and Internal Barriers61). As with past research62, the current study utilized the total score. This measure has good content and predictive validity, and internal consistency62. Internal consistency in the current sample was very good (Cronbach’s α = .88).
Procedure
Participants were recruited at two sites (University of Vermont, Burlington, VT, USA and Florida State University, Tallahassee, Florida, USA) via newspaper, radio, and internet advertisements to participate in a larger study examining the efficacy of a novel 4-session smoking cessation behavioral intervention that focused on vulnerability to panic (Panic-Smoking Program; PSP) in comparison to a standard smoking cessation program (SP). Identical procedures were executed at both sites. The collection of outcome data is currently ongoing as of September 2011. The current report is based on analyses of data collected during the study’s baseline assessment session, which took place prior to randomization and the commencement of the intervention. These analyses have not been published or presented previously. At this session, participants were administered the measures described above, and later compensated for their time. All participants provided informed consent and the study protocol was approved by both universities’ IRBs.
Data Analytic Strategy
Zero-order (or bi-variate as applicable) correlations were first obtained to examine associations between the predictor and criterion variables. Subsequently, the incremental validity of AS was examined in relation to the criterion variables using hierarchical multiple regression63. Separate models were constructed for each of the smoking-based criterion variables (i.e., SCQ-NR, RFS-NA, and BCS-total score). Average number of cigarettes smoked per day, marijuana use in the past 30 days, alcohol consumption (an average frequency-by-quantity composite score), number of Axis I current diagnoses, panic attack history (dummy coded: 1 = no; 2 = yes), and participant sex (dummy coded: 1 = male; 2 = female) were entered as a block at step 1. These covariates were chosen on an a priori basis as factors that could theoretically affect relations between the studied predictor and criterion variables. At step 2 of the model, the ASI-total score was entered. These hierarchical models test the incremental main effect of the predictor variable, independent of the covariates, in relation to the criterion variables64. In addition, a series of hierarchical multiple regressions were conducted to test whether emotion dysregulation (as indexed by the DERS-total score) mediated the relations between AS and the studied smoking-based criterion variables (please see below for a detailed description of the analytic rationale and approach). Overall, this analytic approach is consistent with general recommendations for mediational analysis65.
Results
Zero-order (or Bi-variate) Correlations
Zero-order (or bi-variate as applicable) correlations were first obtained to examine relations between the studied variables (see Table 1). As expected, AS was significantly correlated with emotion dysregulation (r = .66, p < .01), and all criterion variables, including: SCQ-NR (r = .30), RFS-NA (r = .30), and BCS-total score (r = .31); all p’s < .01. Additionally, emotion dysregulation was significantly related to all criterion variables: SCQ-NR (r = .33), RFS-NA (r = .37), and BCS-total score (r = .35); all p’s < .01.
Table 1.
Zero-Order (or Bi-variate) Correlations among Theoretically-Relevant Variables
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | Mean or % (SD) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CPD | 1 | .05 | −.02 | .06 | −.08 | −.01 | .22** | .11 | .16** | .22** | .08 | 20.49 (12.57) |
| 2. MJ Use | 1 | .32** | .20** | −.06 | .02 | .10 | .17** | .18** | .10 | .14* | 1.90 (2.91) | |
| 3. Alcohol | 1 | .19** | −.28** | .06 | .15* | .26** | .05 | −.01 | .08 | 4.23 (3.90) | ||
| 4. Diagnosis | 1 | .07 | .19** | .48** | .55** | .14* | .18** | .10 | .75 (1.19) | |||
| 5. Sex | 1 | .16* | .05 | .01 | .16** | .26** | .26** | 57.5% Male | ||||
| 6. PA Hx | 1 | .31** | .27** | .10 | .10 | .12 | 44.1% Yes | |||||
| 7. ASI | 1 | .66** | .30** | .30** | .31** | 15.54 (12.61) | ||||||
| 8. DERS | 1 | .33** | .37** | .35** | 75.23 (22.13) | |||||||
| 9. SCQ-NR | 1 | .71** | .55** | 5.71 (1.74) | ||||||||
| 10. RFS-NA | 1 | .60** | 3.50 (.79) | |||||||||
| 11. BCS | 1 | 25.28 (10.99) |
Note:
p < .05;
p < .01;
CPD = Average cigarettes smoked per day - Smoking History Questionnaire; MJ Use = Marijuana use in the past 30 days – Marijuana Smoking History Questionnaire; Alcohol = Alcohol consumption (average frequency-by-quantity composite score) – Alcohol Use Disorders Identification Test; Diagnosis = Number of current Axis-I diagnoses, per Structured Clinical Interview-Non-Patient Version for DSM-IV; Sex = Dummy coded (1 = males; 2 = females); PA Hx = Two-year history of panic attacks, dummy-coded (no=1, yes=2), per Structured Clinical Interview-Non-Patient Version for DSM-IV; ASI = Anxiety Sensitivity Index-III-Total Score; DERS = Difficulties Regulating Emotions Scale-Total Score; SCQ-NR = Smoking Consequences Questionnaire-Negative Reinforcement/Negative Affect Reduction Subscale; RFS-NA = Reasons for Smoking-Negative Affect Subscale; BCS = Barriers to Cessation Scale-Total Score.
Negative Reinforcement/Negative Affect Reduction Smoking Outcome Expectancies
Initially, a hierarchical linear regression was conducted to examine the relation between AS (the predictor) and SCQ-NR (the criterion). Overall, the model predicted 18% of variance in SCQ-NR [F(7, 196) = 5.92, p < .001]. Step 1 of the model predicted 11.5% of variance, with participant sex being the only significant predictor. Step 2 accounted for an additional 6.5% of variance. As hypothesized, AS was a significant predictor of SCQ-NR above and beyond the covariates at Step 1 of the model (see Table 2).
Table 2.
Regression analyses examining emotion dysregulation as a mediator of anxiety sensitivity and negative reinforcement/negative affect reduction smoking outcome expectancies
| DV | Predictors | B | β | |
|---|---|---|---|---|
| SCQ-NR | 1. | CPD | .02 | .13 |
| MJ Use | .08 | .14 | ||
| Alcohol | .01 | .03 | ||
| Diagnosis | .13 | .09 | ||
| Sex | .82 | .23** | ||
| PA Hx | .14 | .04 | ||
| 2. | ASI | .04 | .30** | |
| DERS | 1. | CPD | .14 | .08 |
| MJ Use | .15 | .02 | ||
| Alcohol | .85 | .15* | ||
| Diagnosis | 9.03 | .49** | ||
| Sex | −2.99 | −.07 | ||
| PA Hx | 6.03 | −.13* | ||
| 2. | ASI | .96 | .53** | |
| SCQ-NR | 1. | CPD | .02 | .13 |
| MJ Use | .08 | .14 | ||
| Alcohol | .01 | .03 | ||
| Diagnosis | .13 | .09 | ||
| Sex | .82 | .23** | ||
| PA Hx | .14 | .04 | ||
| 2. | ASI | .04 | .30** | |
| 3. | DERS | .03 | .34** | |
| SCQ-NR | 1. | CPD | .02 | .13 |
| MJ Use | .08 | .14 | ||
| Alcohol | .01 | .03 | ||
| Diagnosis | .13 | .09 | ||
| Sex | .82 | .23** | ||
| PA Hx | .14 | .04 | ||
| 2. | DERS | .03 | .41** | |
| 3. | ASI | .02 | .12 | |
Note: β = Standardized beta weight provided for hierarchical multiple regression; CPD = Average cigarettes smoked per day - Smoking History Questionnaire; MJ Use = Marijuana use in the past 30 days – Marijuana Smoking History Questionnaire; Alcohol = Alcohol consumption (average frequency-by-quantity composite score) – Alcohol Use Disorders Identification Test; Diagnosis = Number of current Axis-I diagnoses, per Structured Clinical Interview-Non-Patient Version for DSM-IV; Sex = Dummy coded (1 = males; 2 = females); PA Hx = Two-year history of panic attacks, dummy-coded (no=1, yes=2), per Structured Clinical Interview-Non-Patient Version for DSM-IV; ASI = Anxiety Sensitivity Index-III-Total Score; DERS = Difficulties Regulating Emotions Scale-Total Score; SCQ-NR = Smoking Consequences Questionnaire-Negative Reinforcement/Negative Affect Reduction Subscale.
A second hierarchical linear regression was conducted to examine the relation between AS (the predictor) and emotion dysregulation (the mediator). The model predicted 55.5% of variance in emotion dysregulation [F(7, 196) = 34.6, p < .001]. Step 1 of the model predicted 35.2% of variance, with participant sex, alcohol consumption, and number of current Axis I diagnoses each being a significant predictor. Step 2 accounted for an additional 20.3% of variance. Here, AS was a significant predictor above and beyond the variance accounted for at Step 1 of the model (see Table 2).
As described in Table 2, the mediational role of emotion dysregulation in the relation between AS and SCQ-NR was examined by employing the strategy proposed by Baron and Kenny (1986). The first requirement of this statistical test of mediation rests with an association between the predictor variable (AS) and criterion variable (SCQ-NR). This association was found to be statistically significant (see analysis 1 in Table 2). The second requirement for mediation involves establishing a relation between the predictor variable and the proposed mediating variable (emotion dysregulation). Again, this association was found to be statistically significant (see analysis 2 in Table 2). The third requirement states that a relation between the proposed mediating variable and the criterion variable must exist after controlling for the effects of the predictor. After controlling for AS, emotion dysregulation was significantly associated with SCQ-NR (see analysis 3 in Table 2). The final requirement for mediation involves evaluating the relation between the predictor and the criterion when the variance accounted for by the proposed mediator has been removed. When this equation yields a non-significant effect for the predictor, the controlling variable is said to fully mediate the relation. In these analyses, emotion dysregulation mediated the relation between AS and SCQ-NR, as AS was no longer a significant predictor of SCQ-NR (see analysis 4 in Table 2). Indeed, post-hoc analyses using the Sobel Test for mediation66 revealed that emotion dysregulation significantly mediated the relation between AS and SCQ-NR (z = 3.45, SE = .007, p < .01).
As mediational analyses are often conducted using longitudinal data, one powerful method of strengthening the interpretation of mediational analyses conducted with cross-sectional data is to conduct an additional analysis reversing the proposed mediator and criterion variable65,67,68. Here, we evaluated whether SCQ-NR mediated the relation between AS and emotion dysregulation. Results were not consistent with mediation in this direction as AS remained a significant predictor of emotion dysregulation after controlling for SCQ-NR [F(8, 196) = 32.7, p < .001].
Negative Affect Reduction Smoking Motives
Initially, a hierarchical linear regression was conducted to examine the relation between AS (the predictor) and RFS-NA (the criterion). Overall, the model predicted 22.3% of variance in RFS-NA [F(7, 196) = 7.7, p < .001]. Step 1 of the model predicted 17.4% of variance, with participant sex and average number of cigarettes per day each being a significant predictor. Step 2 accounted for an additional 4.9% of variance; as hypothesized, AS was a significant predictor of RFS-NA above and beyond the covariates at Step 1 of the model (see Table 3).
Table 3.
Regression analyses examining emotion dysregulation as a mediator of anxiety sensitivity and negative affect reduction smoking motives
| DV | Predictors | B | β | |
|---|---|---|---|---|
| RFS-NA | 1. | CPD | .01 | .19** |
| MJ Use | .02 | .09 | ||
| Alcohol | .01 | .06 | ||
| Diagnosis | .06 | .09 | ||
| Sex | .55 | .35** | ||
| PA Hx | −.01 | −.01 | ||
| 2. | ASI | .02 | .26** | |
| DERS | 1. | CPD | .14 | .08 |
| MJ Use | .15 | .02 | ||
| Alcohol | .85 | .15* | ||
| Diagnosis | 9.03 | .49** | ||
| Sex | −2.99 | −.07 | ||
| PA Hx | 6.03 | −.13* | ||
| 2. | ASI | .96 | .53** | |
| RFS-NA | 1. | CPD | .01 | .19** |
| MJ Use | .02 | .09 | ||
| Alcohol | .01 | .06 | ||
| Diagnosis | .06 | .09 | ||
| Sex | .55 | .35** | ||
| PA Hx | −.01 | −.01 | ||
| 2. | ASI | .02 | .26** | |
| 3. | DERS | .01 | .41** | |
| RFS-NA | 1. | CPD | .01 | .15 |
| MJ Use | .02 | .08 | ||
| Alcohol | .01 | .01 | ||
| Diagnosis | −.08 | −.13 | ||
| Sex | .60 | .38 | ||
| PA Hx | −.11 | −.08 | ||
| 2. | DERS | .02 | .44** | |
| 3. | ASI | .00 | .04 | |
Note: β = Standardized beta weight provided for hierarchical multiple regression; CPD = Average cigarettes smoked per day - Smoking History Questionnaire; MJ Use = Marijuana use in the past 30 days – Marijuana Smoking History Questionnaire; Alcohol = Alcohol consumption (average frequency-by-quantity composite score) – Alcohol Use Disorders Identification Test; Diagnosis = Number of current Axis-I diagnoses, per Structured Clinical Interview-Non-Patient Version for DSM-IV; Sex = Dummy coded (1 = males; 2 = females); PA Hx = Two-year history of panic attacks, dummy-coded (no=1, yes=2), per Structured Clinical Interview-Non-Patient Version for DSM-IV; ASI = Anxiety Sensitivity Index-III-Total Score; DERS = Difficulties Regulating Emotions Scale-Total Score; RFS-NA = Reasons for Smoking-Negative Affect Subscale.
A second hierarchical linear regression was conducted to examine the relation between AS (the predictor) and emotion dysregulation (the mediator). Please see analysis 2 in the “Negative Reinforcement/Negative Affect Reduction Smoking Outcome Expectancies” section for an expanded presentation of these findings.
The mediational role of emotion dysregulation in the relation between AS and RFS-NA was then examined. After controlling for AS, emotion dysregulation was significantly associated with RFS-NA (see analysis 3 in Table 3). Additionally, emotion dysregulation mediated the relation between AS and RFS-NA, as AS was no longer a significant predictor of RFS-NA (see analysis 4 in Table 3). Post-hoc analyses using the Sobel Test for mediation66 confirmed that emotion dysregulation significantly mediated the relation between AS and RFS-NA (z = 4.17, SE = .003, p < .01. Furthermore, as described above, we employed a more rigorous test of mediation by evaluating whether RFS-NA mediated the relation between AS and emotion dysregulation. Results were not consistent with mediation in this direction as AS remained a significant predictor of emotion dysregulation after controlling for RFS-NA [F(8, 196) = 34.8, p < .001].
Barriers to Smoking Cessation
Initially, a hierarchical linear regression was conducted to examine the relation between AS (the predictor) and the BCS-total score (the criterion). Overall, the model predicted 19.3% of variance in the BCS-total score [F(7, 196) = 6.4, p < .001]. Step 1 of the model predicted 11.3% of variance, with participant sex and marijuana use in the past 30 days each being a significant predictor. Step 2 accounted for an additional 8.0% of variance; as hypothesized, AS was a significant predictor of the BCS-total score above and beyond the covariates at Step 1 of the model (see Table 4).
Table 4.
Regression analyses examining emotion dysregulation as a mediator of anxiety sensitivity and barriers to smoking cessation
| DV | Predictors | B | β | |
|---|---|---|---|---|
| BCS | 1. | CPD | .03 | .04 |
| MJ Use | .67 | .19* | ||
| Alcohol | .27 | .10 | ||
| Diagnosis | −.06 | −.01 | ||
| Sex | 5.32 | .24** | ||
| PA Hx | 1.63 | .08 | ||
| 2. | ASI | .30 | .33** | |
| DERS | 1. | CPD | .14 | .08 |
| MJ Use | .15 | .02 | ||
| Alcohol | .85 | .15* | ||
| Diagnosis | 9.03 | .49** | ||
| Sex | −2.99 | −.07 | ||
| PA Hx | 6.03 | −.13* | ||
| 2. | ASI | .96 | .53** | |
| BCS | 1. | CPD | .03 | .04 |
| MJ Use | .67 | .19* | ||
| Alcohol | .27 | .10 | ||
| Diagnosis | −.06 | −.01 | ||
| Sex | 5.32 | .24** | ||
| PA Hx | 1.63 | .08 | ||
| 2. | ASI | .30 | .33** | |
| 3. | DERS | .18 | .38** | |
| BCS | 1. | CPD | .03 | .04 |
| MJ Use | .67 | .19* | ||
| Alcohol | .27 | .10 | ||
| Diagnosis | −.06 | −.01 | ||
| Sex | 5.32 | .24** | ||
| PA Hx | 1.63 | .08 | ||
| 2. | DERS | .22 | .46** | |
| 3. | ASI | .12 | .13 | |
Note: β = Standardized beta weight provided for hierarchical multiple regression; CPD = Average cigarettes smoked per day - Smoking History Questionnaire; MJ Use = Marijuana use in the past 30 days – Marijuana Smoking History Questionnaire; Alcohol = Alcohol consumption (average frequency-by-quantity composite score) – Alcohol Use Disorders Identification Test; Diagnosis = Number of current Axis-I diagnoses, per Structured Clinical Interview-Non-Patient Version for DSM-IV; Sex = Dummy coded (1 = males; 2 = females); PA Hx = Two-year history of panic attacks, dummy-coded (no=1, yes=2), per Structured Clinical Interview-Non-Patient Version for DSM-IV; ASI = Anxiety Sensitivity Index-III-Total Score; DERS = Difficulties Regulating Emotions Scale-Total Score; BCS = Barriers to Cessation Scale-Total Score.
A second hierarchical linear regression was conducted to examine the relation between AS (the predictor) and emotion dysregulation (the mediator). Please see analysis 2 in the “Negative Reinforcement/Negative Affect Reduction Smoking Outcome Expectancies” section for an expanded presentation of these findings.
The mediational role of emotion dysregulation in the relation between AS and the BCS-total score was then examined. After controlling for AS, emotion dysregulation was significantly associated with the BCS-total score (see analysis 3 in Table 4). Additionally, emotion dysregulation mediated the relation between AS and the BCS-total score, as AS was no longer a significant predictor of the BCS-total score (see analysis 4 in Table 4). Post-hoc analyses using the Sobel Test for mediation66 confirmed that emotion dysregulation significantly mediated the relation between AS and the BCS-total score (z = 3.74, SE = .048, p < .01). Furthermore, as described above, we employed a more rigorous test of mediation by evaluating whether the BCS-total score mediated the relation between AS and emotion dysregulation. Findings were not consistent with mediation in this direction as AS remained a significant predictor of emotion dysregulation after controlling for the BCS-total score [F(8, 196) = 33.8, p < .001].
Discussion
The present study examined AS in terms of predicting cognitive-based smoking processes among adult treatment-seeking daily smokers. As hypothesized, there was consistent evidence that AS was significantly and uniquely associated with the cognitive-based smoking processes of negative affect reduction smoking motives, negative reinforcement smoking expectancies, and perceived barriers for quitting. The size of the observed effects were generally medium to large69 (see Table 2), with higher levels of AS being incrementally associated with greater endorsement of the studied criterion variables. Importantly, the effects for AS were apparent over and above the significant variance accounted for by smoking rate, marijuana use in the past 30 days, alcohol consumption, number of current Axis I diagnoses, panic attack history and participant sex. Thus, the results cannot be attributed to these co-occurring risk factors.
Also consistent with prediction, emotion dysregulation significantly mediated the relations between AS and each of the studied cognitive-based smoking processes. Although the cross-sectional nature of the research design does not allow us to disentangle whether emotion dysregulation occurs after AS37, the present findings suggest that the inability to self-regulate certain affective states (e.g., anxiety, depression) may, at least partially, explain the previously observed relations between AS and cognitive-based smoking processes. Specifically, high AS individuals, who also lack the ability to effectively manage affective states, may be more likely to a) develop specific beliefs about the negatively reinforcing effects of smoking, b) be motivated to smoke for affect regulation purposes, and c) endorse greater barriers to cessation. We attempted to strengthen confidence in this observation by evaluating an alternative model, wherein each of the cognitive-based smoking processes mediated the relation between AS and emotion dysregulation. No support was found for such a model. That is, AS, emotion dysregulation, and the studied cognitive-based smoking processes were not simply interrelated; rather, the present findings suggest specificity in terms of the potential mediating role of emotion dysregulation. Thus, the current findings highlight that emotion dysregulation is an important construct to consider in the relations between AS and cognitive-based smoking processes among adult treatment-seeking smokers.
A number of limitations of the present investigation and points for future direction should be considered. First, the present sample is limited in that it is comprised of a relatively homogenous (e.g., primarily Caucasian) group of adult smokers who volunteered to participate in smoking cessation treatment. Given that the vast majority of cigarette smokers attempt to quit on their own (70% of smokers70), it will be important for researchers to draw from populations other than those included in the present study to rule out potential self-selection bias among persons with these characteristics and increase the generalizability of these findings. For example, future studies might benefit from recruiting a more ethnically/racially diverse sample of smokers who are interested in undergoing a self-guided quit attempt (i.e., absent of a treatment intervention). Second, we sampled community-recruited daily smokers. Inspection of the level of nicotine dependence among this sample was relatively low. To enhance the generalizability of the results, it may therefore be useful to replicate and extend the present findings to heavier smoking samples and evaluate if similar patterns emerge. Third, the present study utilized a self-report measure of nicotine dependence (i.e., FTND38). Given that past research has suggested that the FTND may function differently among various ethnic groups (e.g., African-Americans71,72), it might be beneficial for future research to employ multiple assessment approaches in order to more comprehensively measure nicotine dependence. Fourth, even though we employed a more rigorous analytic approach, the present study was nonetheless correlational in nature. It is therefore necessarily limited because it cannot shed light on processes over time or isolate causal relations between variables. Finally, in the present study we modeled a wide range, but naturally only a select number, of cognitive-based smoking processes. Thus, it is advisable for future work to explore the potential mediating role of emotion dysregulation in terms of other smoking processes, such as smoking cessation outcomes (i.e., lapse and relapse) and the course of nicotine withdrawal symptoms during and after treatment.
Overall, the results of the current study broadly highlight the importance of emotion dysregulation in terms of better understanding the link between AS and cognitive-based smoking processes. Such findings serve to conceptually inform the development of specialized intervention strategies for smokers with elevated risk for anxiety psychopathology. Specifically, the present findings suggest that it may be necessary to understand and clinically address emotion dysregulation, among anxiety vulnerable, daily tobacco users, in order to facilitate more successful cessation attempts. That is, smokers with elevated levels of AS may benefit from intensive cognitive-behavioral strategies, aimed at increasing self-efficacy over the ability to regulate affective states as well as gain control over affect-driven behaviors (distress tolerance- and/or mindfulness-based skills), in an effort to promote greater degrees of smoking abstinence.
Acknowledgments
Disclosures
This work was supported by a National Institute on Health grant awarded to Dr. Michael J. Zvolensky and Dr. Norman B. Schmidt (R01 MH076629-01A1). This work was also supported by a National Institute on Drug Abuse National Research Service Award (5 F31 DA026634-03) awarded to Kirsten A. Johnson. Please note that the funding source had no other role other than financial support.
Contributor Information
Kirsten A. Johnson, University of Vermont, 2 Colchester Avenue, Burlington, VT 05405
Samantha G. Farris, University of Houston, 126 Heyne Building, Houston, Texas 77204
Norman B. Schmidt, Florida State University, 1107 W. Call Street, Tallahassee, FL 32306
Michael J. Zvolensky, University of Houston, 126 Heyne Building, Houston, Texas 77204
References
- 1.McNally RJ. Anxiety sensitivity and panic disorder. Biol Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- 2.Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. San Diego: Academic Press; pp. 107–121. [Google Scholar]
- 3.Reiss S, Havercamp SH. The sensitivity theory of motivation: Implications for psychopathology. Beh Res Ther. 1996;34:621–632. doi: 10.1016/0005-7967(96)00041-1. [DOI] [PubMed] [Google Scholar]
- 4.Hayward C, Killen JD, Kraemer HC, Taylor CB. Predictors of panic attacks in adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39:207–214. doi: 10.1097/00004583-200002000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Li W, Zinbarg RE. Anxiety sensitivity and panic attacks: A 1-year longitudinal study. Behav Modif. 2007;31:145–161. doi: 10.1177/0145445506296969. [DOI] [PubMed] [Google Scholar]
- 6.Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. J Anxiety Disord. 1992;6:241–247. [Google Scholar]
- 7.Marshall GN, Miles JNV, Stewart SH. Anxiety sensitivity and PTSD symptom severity are reciprocally related: Evidence from a longitudinal study of physical trauma survivors. J Abnorm Psychol. 2010;119:143–150. doi: 10.1037/a0018009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt NB, Keough ME, Mitchell MA, Reynolds EK, MacPherson L, Zvolensky MJ, Lejuez CW. Anxiety sensitivity: Prospective prediction of anxiety among early adolescents. J Anxiety Disord. 2010;24:503–508. doi: 10.1016/j.janxdis.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. J Abnorm Psychol. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt NB, Lerew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. J Abnorm Psychol. 1999;108:532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. J Psychiatr Res. 2006;40:691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Lejuez CW, Paulson A, Daughters SB, Bornovalova MA, Zvolensky MJ. The association between heroin use and anxiety sensitivity among inner-city individuals in residential drug use treatment. Beh Res Ther. 2006;44:667–677. doi: 10.1016/j.brat.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Norton GR, Rockman GE, Luy B, Marion T. Suicide, chemical abuse, and panic attacks: A preliminary report. Behav Res Ther. 1993;31:37–40. doi: 10.1016/0005-7967(93)90040-2. [DOI] [PubMed] [Google Scholar]
- 14.Stewart SH, Karp J, Pihl RO, Peterson RA. Anxiety sensitivity and self-reported reasons for drug use. Journal of Substance Abuse. 1997;9:223–224. doi: 10.1016/s0899-3289(97)90018-3. [DOI] [PubMed] [Google Scholar]
- 15.Stewart SH, Kushner MG. Introduction to the special issue on “Anxiety Sensitivity and Addictive Behaviors”. Addict Behav. 2001;26:775–785. doi: 10.1016/s0306-4603(01)00236-2. [DOI] [PubMed] [Google Scholar]
- 16.Zvolensky MJ, Bernstein A. Cigarette smoking and panic psychopathology. Current Directions in Psychological Science. 2005;14:301–305. [Google Scholar]
- 17.Zvolensky MJ, Bonn-Miller MO, Bernstein A, Marshall E. Anxiety sensitivity and abstinence duration to smoking. Journal of Mental Health. 2006;15:659–670. [Google Scholar]
- 18.Zvolensky MJ, Stewart SH, Vujanovic AA, Gavric D, Steeves D. Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine Tob Res. 2009;11:323–331. doi: 10.1093/ntr/ntn037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Battista SR, Stewart SH, Fulton HG, Steeves D, Darredeau C, Gavric D. A further investigation of the relations of anxiety sensitivity to smoking motives. Addict Behav. 2008;22:1402–1408. doi: 10.1016/j.addbeh.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 20.Comeau N, Stewart SH, Loba P. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addict Behav. 2001;26:803–825. doi: 10.1016/s0306-4603(01)00238-6. [DOI] [PubMed] [Google Scholar]
- 21.Leyro TM, Zvolensky MJ, Vujanovic A, Bernstein A. Anxiety sensitivity and smoking motives and outcome expectancies among adult daily smokers: Replication and extension. Nicotine Tob Res. 2008;10:985–994. doi: 10.1080/14622200802097555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Novak A, Burgess ES, Clark M, Zvolensky MJ, Brown RA. Anxiety sensitivity, self-reported motives for alcohol and nicotine use and level of consumption. J Anxiety Disord. 2003;17:165–180. doi: 10.1016/s0887-6185(02)00175-5. [DOI] [PubMed] [Google Scholar]
- 23.Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: Relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addict Behav. 2001;26:887–99. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- 24.Gregor KL, Zvolensky MJ, McLeish AC, Bernstein A, Morissette S. Anxiety sensitivity and perceived control over anxiety-related events: Associations with smoking outcome expectancies and perceived cessation barriers among daily smokers. Nicotine Tob Res. 2008;10:627–635. doi: 10.1080/14622200801978706. [DOI] [PubMed] [Google Scholar]
- 25.Zvolensky MJ, Bernstein A, Cardenas SJ, Colotla VA, Marshall EC, Feldner MT. Anxiety sensitivity and early relapse to smoking: A test among Mexican daily, low-level smokers. Nicotine Tob Res. 2007;9:483–491. doi: 10.1080/14622200701239621. [DOI] [PubMed] [Google Scholar]
- 26.Barlow DH, Allen LB, Choate ML. Toward unified treatment for emotional disorders. Behav Ther. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 27.Bonn-Miller MO, Vujanovic AA, Zvolensky MJ. Emotional dysregulation: Association with coping-oriented marijuana use motives among current marijuana users. Subst Use Misuse. 2008;43:1656–1668. doi: 10.1080/10826080802241292. [DOI] [PubMed] [Google Scholar]
- 28.Kashdan TB, Steger M. Expanding the topography of social anxiety: An experience sampling assessment of positive emotions and events, and emotion suppression. Psychol Sci. 2006;17:120–128. doi: 10.1111/j.1467-9280.2006.01674.x. [DOI] [PubMed] [Google Scholar]
- 29.Orsillo SM, Roemer L. Acceptance and mindfulness-based approaches to anxiety: Conceptualization and Treatment. New York: Springer; [Google Scholar]
- 30.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;36:41–54. [Google Scholar]
- 31.Vujanovic AA, Zvolensky MJ, Bernstein A. The interactive effects of anxiety sensitivity and emotion dysregulation in predicting anxiety-related cognitive and affective symptoms. Cognitive Therapy and Research. 2008;32:803–817. [Google Scholar]
- 32.Feldner MT, Zvolensky MJ, Stickle TR, Bonn-Miller MO, Leen-Feldner EW. Anxiety sensitivity-physical concerns as a moderator of the emotional consequences of emotion suppression during biological challenge: An experimental test using individual growth curve analysis. Behav Res Ther. 2006;44:249–272. doi: 10.1016/j.brat.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Kashdan TB, Zvolensky MJ, McLeish AC. Anxiety sensitivity and affect regulatory strategies: Individual and interactive risk factors for anxiety-related symptoms. J Anxiety Disord. 2008;22:429–440. doi: 10.1016/j.janxdis.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson KA, Zvolensky MJ, Marshall EC, Gonzalez A, Abrams K, Vujanovic AA. Linkages between cigarette smoking outcome expectancies and negative emotional vulnerability. Addict Behav. 2008;33:1416–1424. doi: 10.1016/j.addbeh.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gonzalez A, Zvolensky MJ, Vujanovic AA, Leyro TM, Marshall EC. An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: Relation to smoking motives and barriers to quitting. J Psychiatr Res. 2008;43:138–147. doi: 10.1016/j.jpsychires.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 37.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychology research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 38.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 39.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Patient Edition (SCID-N/P), Version 2.0. New York: Biometrics Research, New York State Psychiatric Institute; 1994. [Google Scholar]
- 40.Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II) Clinical Psychology & Psychotherapy. 2011;18:75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- 41.Shear MK, Greeno C, Kang J, Ludewig D, Frank E, Swartz HA, Hanekamp M. Diagnosis of nonpsychotic patients in community clinics. Am J Psychiatry. 2000;157:581–587. doi: 10.1176/appi.ajp.157.4.581. [DOI] [PubMed] [Google Scholar]
- 42.Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111:180–185. [PubMed] [Google Scholar]
- 43.Zvolensky MJ, Lejuez CW, Kahler CW, Brown Panic attack history and smoking cessation: An initial examination. Addict Behav. 2004;29:825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 44.Payne TJ, Smith PO, McCracken LM, McSherry WC, et al. Assessing nicotine dependence: A comparison of the Fagerström Tolerance Questionnaire (FTQ) with the Fagerström Test for Nicotine Dependence (FTND) in a clinical sample. Addict Behav. 1994;19:307–317. doi: 10.1016/0306-4603(94)90032-9. [DOI] [PubMed] [Google Scholar]
- 45.Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addict Behav. 1994;19:33–39. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 46.Cocores J. Nicotine dependence: Diagnosis and treatment. Recent Advances in Addictive Disorders. 1993;16:49–60. [PubMed] [Google Scholar]
- 47.Babor TF, de la Fuente JR, Saunders J, Grant M. Geneva, Switzerland: World Health Organization; AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care, Revision, WHO Document No. WHO/PSA/92.4. [Google Scholar]
- 48.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons With Harmful Alcohol Consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 49.Stewart SH, Zvolensky MJ, Eifert GH. Negative -reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Personality and Individual Differences. 2001;31:157–171. [Google Scholar]
- 50.Bonn-Miller MO, Zvolensky MJ. An evaluation of the nature of marijuana use and its motives among young adult active users. Am J Addict. 2009;18:409–416. doi: 10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- 51.Bonn-Miller MO, Zvolensky MJ, Leen-Feldner EW, Feldner MT, Yartz AR. Marijuana use among daily tobacco smokers: relationship to anxiety related factors. Journal of Psychopathology and Behavioral Assessment. 2005;27:279–289. [Google Scholar]
- 52.Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR. Cardenas SJ Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- 53.Reiss S, Peterson RA, Gursky M, McNally RJ. Anxiety, sensitivity, anxiety frequency, and the prediction of fearfulness. Behav Res Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 54.Taylor S, Cox BJ. An expanded anxiety sensitivity index: Evidence for a hierarchical structure in a clinical sample. J Anxiety Disord. 1998;12:463–483. doi: 10.1016/s0887-6185(98)00028-0. [DOI] [PubMed] [Google Scholar]
- 55.Whiteside US, Chen EY, Neighbors C, Hunter DA, Lo T, Larimer ME. Binge eating and emotion regulation: Do binge eaters have fewer skills to modulate and tolerate negative affect? Eat Behav. 2007;8:162–169. doi: 10.1016/j.eatbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 56.Brandon TH, Baker TB. The smoking consequences questionnaire: The subjective expected utility of smoking in college students. Psychol Assess. 1991;3:484–491. [Google Scholar]
- 57.Buckley TC, Kamholz BW, Mozley SL, Gulliver SB, Holohan DR, Helstrom AW, Kassel JD. A psychometric evaluation of the Smoking Consequences Questionnaire--adult in smokers with psychiatric conditions. Nicotine Tob Res. 2005;7:739–745. doi: 10.1080/14622200500259788. [DOI] [PubMed] [Google Scholar]
- 58.Downey KK, Kilbey MM. Relationship between nicotine and alcohol expectancies and substance dependence. Exp Clin Psychopharmacol. 1995;3:174–182. [Google Scholar]
- 59.Ikard FF, Green DE, Horn D. A scale to differentiate between types of smoking as related to the management of affect. The International Journal of the Addictions. 1969;4:649–659. [Google Scholar]
- 60.Shiffman S. Assessing smoking patterns and motives. J Consult Clin Psychol. 1993;61:732–742. doi: 10.1037//0022-006x.61.5.732. [DOI] [PubMed] [Google Scholar]
- 61.Macnee CL, Talsma A. Development and testing of the barriers to cessation scale. Nurs Res. 1995a;44:214–219. [PubMed] [Google Scholar]
- 62.Macnee CL, Talsma A. Predictors of progress in smoking cessation. Public Health Nurs. 1995b;12:242–248. doi: 10.1111/j.1525-1446.1995.tb00143.x. [DOI] [PubMed] [Google Scholar]
- 63.Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd edition. Hillsdale, NJ: Erlbaum; [Google Scholar]
- 64.Haynes SN, Lench H. Incremental validity of new clinical assessment measures. Psychol Assess. 2003;15:456–466. doi: 10.1037/1040-3590.15.4.456. [DOI] [PubMed] [Google Scholar]
- 65.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediator models. Behavior Research Methods, Instruments, and Computers. 2004;26:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 66.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology. San Francisco: Jossey-Bass; pp. 290–312. [Google Scholar]
- 67.Sheets V, Braver SL. Organizational status and perceived sexual harassment: Detecting the mediators of a null effect. Pers Soc Psychol Bull. 1999;25:1159–1171. [Google Scholar]
- 68.Shrout PE, Bolger N. Mediation in experimental and non-experimental studies: New procedures and recommendations. Psychol Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- 69.Cohen J. Statistical Power for the Behavioral Sciences. Second ed. Hillsdale, NJ: Lawrence-Erlbaum Associates, Inc.; [Google Scholar]
- 70.Levy DT, Friend K. A simulation model of policies directed at treating tobacco use and dependence. Med Decis Making. 2002;22:6–17. doi: 10.1177/0272989X0202200101. [DOI] [PubMed] [Google Scholar]
- 71.Moolchan ET, Berlin I, Robinson ML, Cadet JL. African-American teen smokers: Issues to consider for cessation treatment. J Natl Med Assoc. 2000;92:558–562. [PMC free article] [PubMed] [Google Scholar]
- 72.Schroeder JR, Moolchan ET. Ethnic differences among adolescents seeking smoking cessation treatment: A structural analysis of responses on the Fagerström Test for Nicotine Dependence. Nicotine Tob Res. 2007;9:137–145. doi: 10.1080/14622200601078400. [DOI] [PubMed] [Google Scholar]